Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.148
Peer-review started: February 16, 2020
First decision: September 29, 2020
Revised: October 12, 2020
Accepted: November 4, 2020
Article in press: November 4, 2020
Published online: January 6, 2021
Processing time: 319 Days and 13.9 Hours
Hemifacial microsomia (HFM) is the second most common craniofacial congenital anomaly following cleft lip and palate. Because of the various phenotypic spectra and the severity of the deformity, a wide range of treatment approaches have been proposed. Recently, the surgery-first approach (SFA) was introduced to treat mild to moderate HFM, and it yielded a balanced facial appearance. The SFA not only promotes rapid improvement in facial aesthetics but also considerably reduces the overall treatment time.
A female patient, aged 25 years old, sought orthodontic treatment with the chief complaint of dental and facial asymmetry. After a comprehensive physical examination and imaging analysis were performed, the patient was diagnosed with mild HFM that was primarily attributed to unilateral abnormal development of the maxilla-mandibular. The SFA was carried out to correct the skeletal deformity. The palatal suture was used as the midline of the maxilla in the surgical plan to center the maxilla, and the chin was also properly positioned to obtain a relatively symmetrical facial appearance. Four weeks after the surgery, the patient was referred for postsurgical orthodontics to decompensate the dentition and stabilize the occlusion. After 20 mo of treatment, all orthodontic appliances were removed. The posttreatment photographs of the patient and her smile confirmed good aesthetic and occlusal results.
Mild HFM can be corrected by SFA, which not only promotes rapid improvement in facial aesthetics but also considerably reduces the overall treatment time.
Core Tip: Hemifacial microsomia (HFM) is the second most common craniofacial congenital anomaly following cleft lip and palate. Recently, the surgery-first approach (SFA) was introduced to treat mild to moderate HFM, promote rapid improvement in facial aesthetics and reduce the overall treatment time. When presurgical orthodontics information on the underlying skeletal deformity is not available, careful treatment planning and strong collaborations between skilled orthodontists and surgeons are needed to predict accurately surgical skeletal movement and postsurgical tooth movement after SFA. This case report presents a successful SFA in a patient with mild HFM. The treatment outcome confirmed a balanced facial appearance.
- Citation: Song JY, Yang H, He X, Gao S, Wu GM, Hu M, Zhang Y. Surgery-first for a patient with mild hemifacial microsomia: A case report and review of literature. World J Clin Cases 2021; 9(1): 148-162
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/148.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.148
Hemifacial microsomia (HFM) is the second most common craniofacial congenital anomaly following cleft lip and palate. It is characterized by a developmental defect in any structure of the first and second pharyngeal arch leading to predominantly asymmetric hypoplasia of their derivatives, characterized by unilateral maxilla-mandibular hypoplasia and facial asymmetry. In addition to maxilla-mandibular anomalies, this condition also involves underdevelopment of the ear, zygoma, temporal bone and the associated musculature and soft tissues[1-4].
Kearns et al[5] hypothesized that abnormal mandibular growth is the earliest skeletal manifestation and plays a vital role in progressive deformity, which provided the rationale for treatments focused on lengthening the mandible. For adults after pubertal growth, mandibular hypoplasia and facial asymmetry can be corrected by combined orthodontic-orthognathic treatment. Conventional three-stage orthodontic-orthognathic treatment, which includes presurgical orthodontics, orthognathic surgery and postsurgical orthodontics, is well established and used in most cases to correct skeletal deformities[6]. However, one drawback of conventional orthodontic-orthognathic treatment is that long-term presurgical treatment typically worsens the facial appearance and exacerbates malocclusion, which further antagonizes HFM patients, whose abnormal facial appearance may have already influenced their psychological health and social interaction[7-9].
Recently, the surgery-first approach (SFA) has attracted a great deal of interest because it corrects skeletal deformities early and is followed by orthodontic treatments to align, level and stabilize the occlusion[10-12]. This approach promotes rapid improvement in facial aesthetics and leads to psychosocial benefits, especially for HMF patients. In addition, some scholars have demonstrated a large reduction in the total treatment time, by as much as 50%, by using the SFA[13,14]. Without presurgical orthodontic information on the true underlying skeletal deformity, positioning the jaw properly without compromising the surgical results is very challenging for surgeons to perform, especially in HMF patients with complex dentofacial deformities, which require careful treatment planning and strong collaborations between skilled orthodontists and surgeons to predict accurately the surgical skeletal movement and postsurgical tooth movement.
This case report presents a successful SFA with the combination of temporary miniscrew anchorage devices performed in a patient with mild HFM.
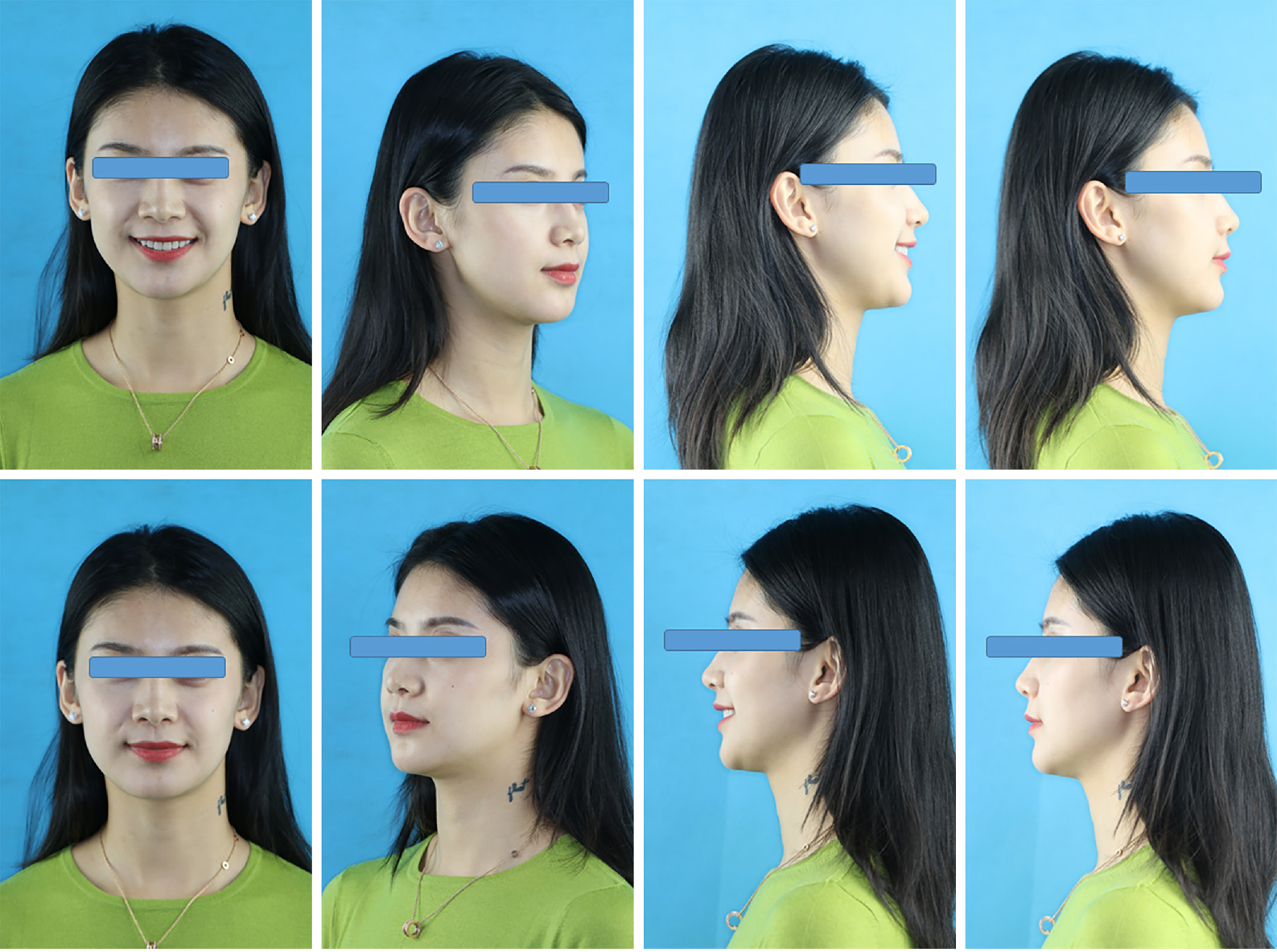
A female patient, aged 25 years old, sought orthodontic treatment with the chief complaint of dental and facial asymmetry (Figures 1 and 2).
She had no systemic diseases.
She had an aesthetic injection in her right chin and no other significant medical histories and denied a genetic history.
She had no family history.
Pretreatment frontal face evaluation showed an asymmetrical face with the right side larger than the left, the chin shifted to the left, and pronounced inclination of the occlusal plane. The two pupils were also not on the same horizontal line (Figure 1). The intraoral examination showed a more than full-cusp class III molar relationship and crossbites in the left posterior region (Figure 2). The maxillary right second molar was congenitally missing, and the right second mandibular molar had a serious defect in the dental hard tissues. The maxillary midline was diverted to the right by 4 mm, the mandibular midline was shifted to the left by 6 mm, and there was a marked inclination of the maxillary occlusal plane.
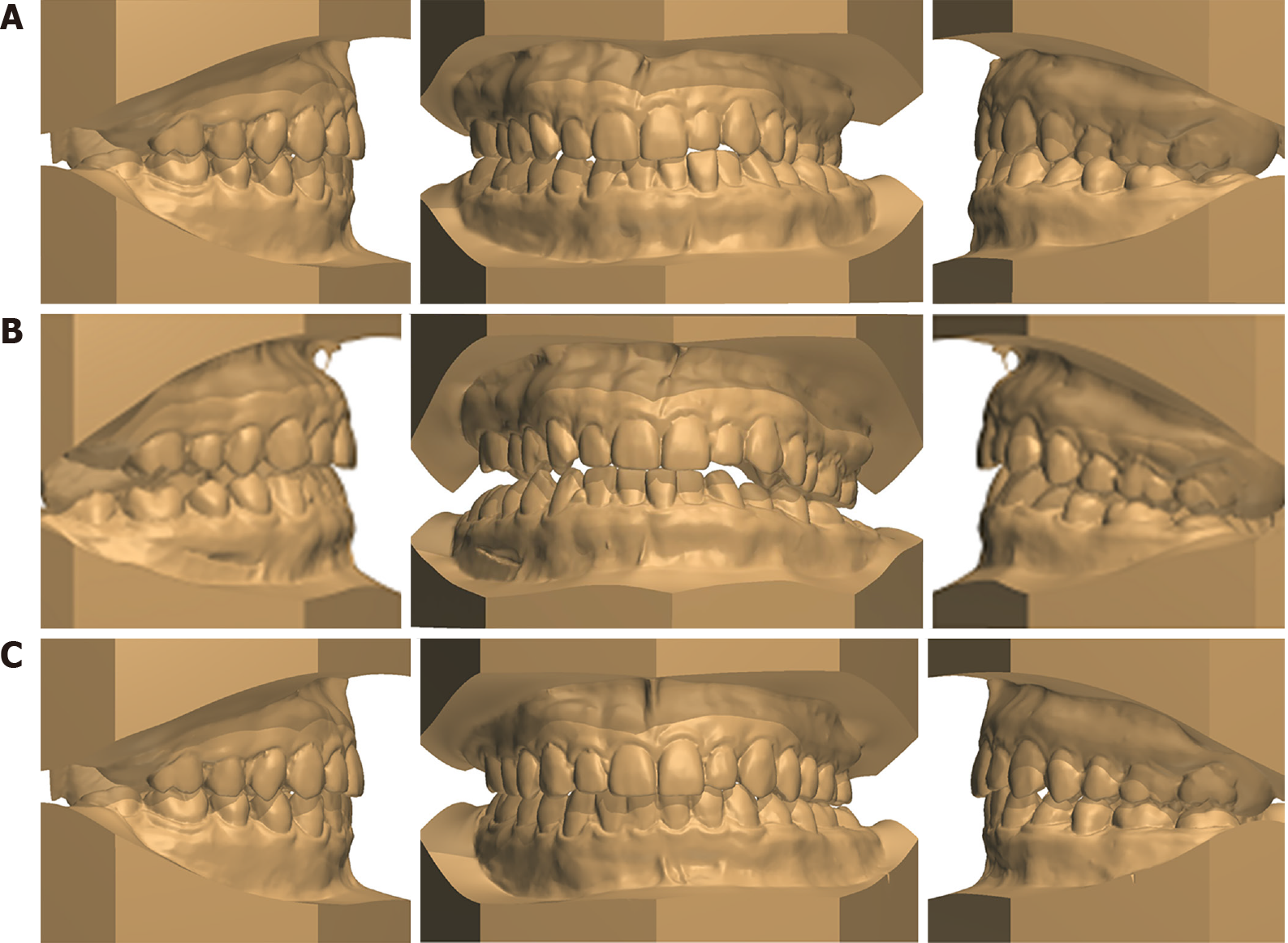
The analysis of study casts showed an overjet of -0.15 to 2.48 mm and crowding in the maxillary and mandibular anterior (Table 1, Figure 3A). The anterior Bolton index was 83%, and the overall Bolton index was 96% (17 was absent, Table 1).
| Bolton analysis | |||||
| Anterior Bolton analysis | Overall Bolton analysis | ||||
| Maxillary 6 width | 40.78 | Maxillary 12 width | 84.80 | ||
| Mandibular 6 width | 33.81 | Mandibular 12 width | 81.07 | ||
| Ratio | 0.83 | Ratio | 0.96 | ||
| Overbite/Overjet | Pretreatment | Posttreament | |||
| 21-Overjet | 1.68 | 2.27 | |||
| 11-Overjet | 2.48 | 2.47 | |||
| 12-Overjet | 1.87 | 2.25 | |||
| 22-Overjet | -0.15 | 2.01 | |||
| Arch width | Pretreatment | Posttreament | |||
| The upper arch width of 3-3 | 33.66 | 33.86 | |||
| The lower arch width of 3-3 | 24.30 | 26.44 | |||
| The upper arch width of 6-6 | 52.63 | 50.85 | |||
| The lower arch width of 6-6 | 48.78 | 47.56 | |||
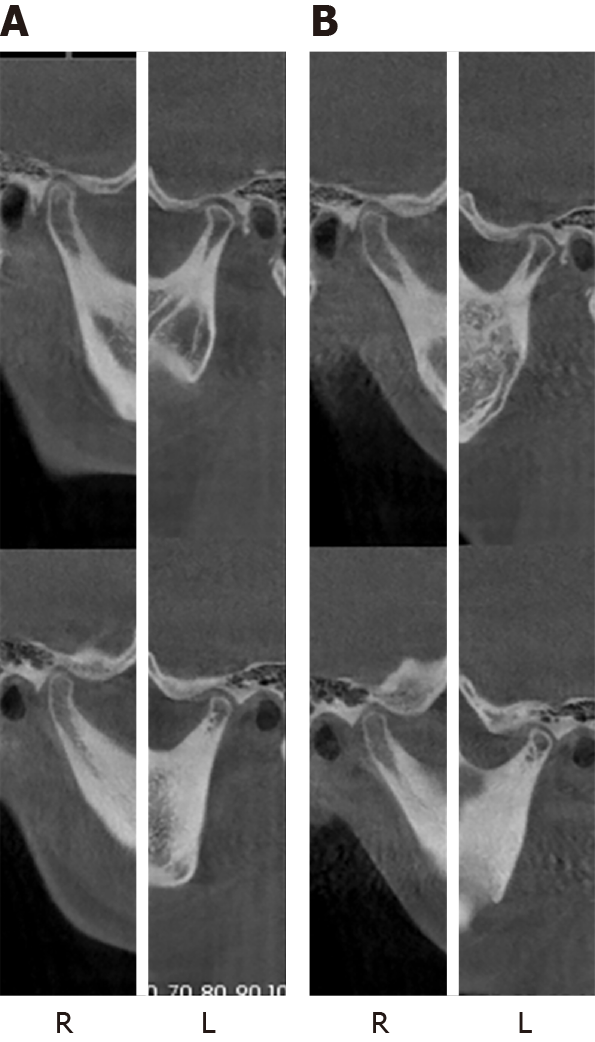
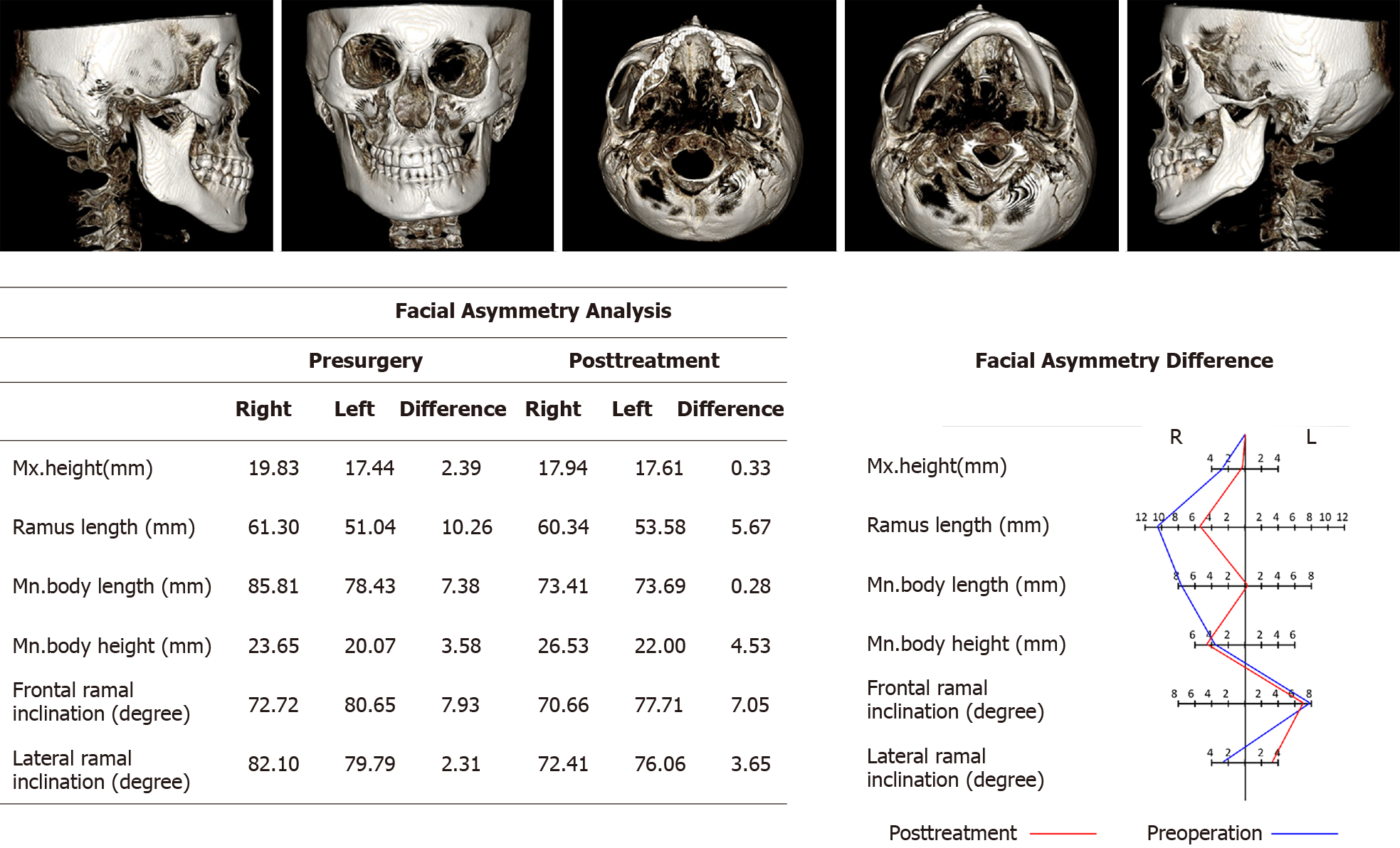
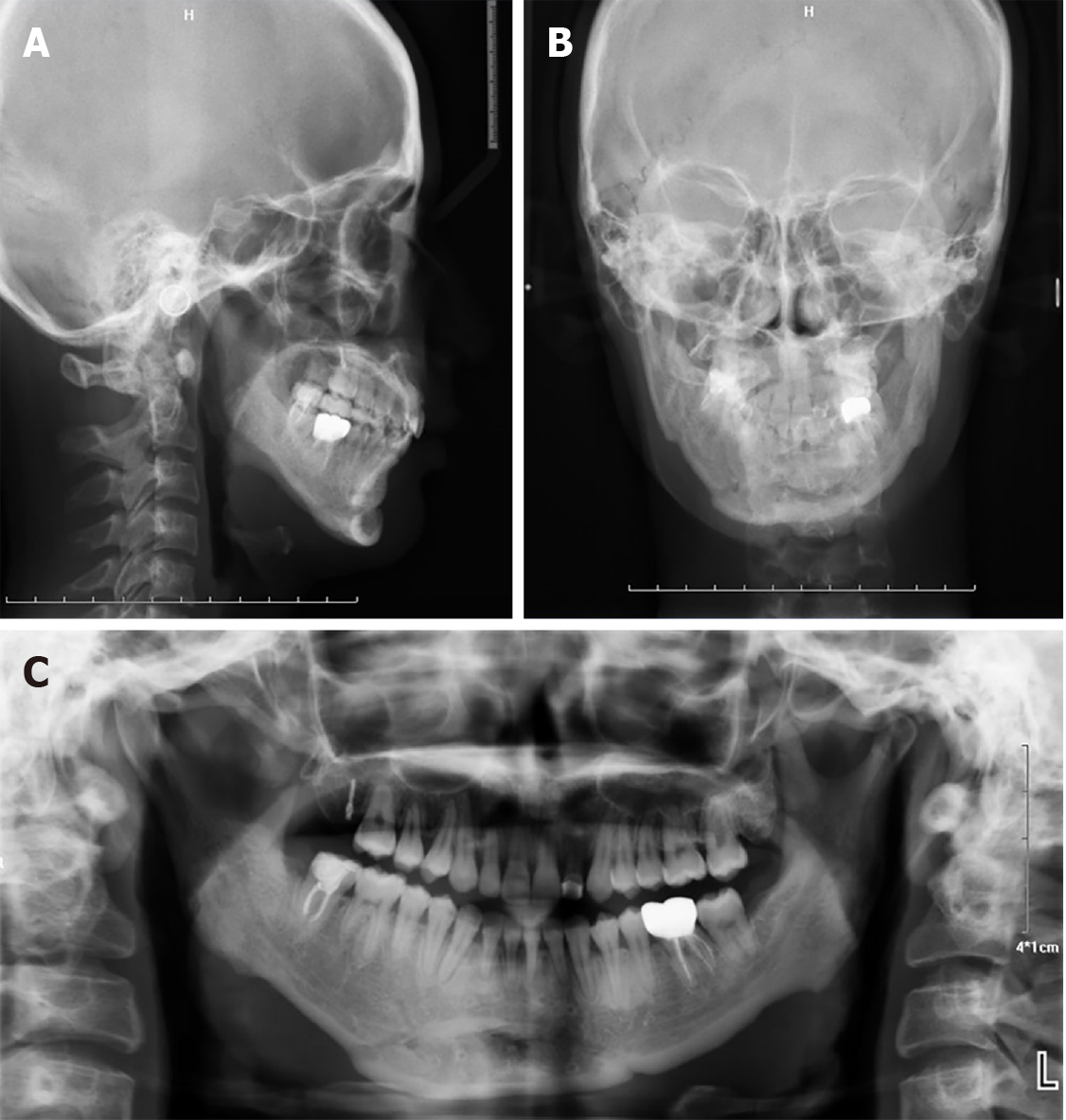
The panoramic radiograph indicated the absence of tooth 17 and mild alveolar absorption in the whole dentition (Figure 4). The lateral cephalometric analysis indicated a skeletal class III relationship (ANB, 1.9°; Wits appraisal, -5.7°) (Figure 4A, Table 2). Ricketts’ frontal cephalometric analysis (Table 3) showed skeletal asymmetry of the mandible and mandibular dental asymmetry (Figure 4B). The functional examination showed no signs of temporomandibular joint (TMJ) disorder, but the mandible deflected to the left when the jaw was opened (Figure 5). The cone beam computed tomography (CBCT) image analysis of facial asymmetry (Figure 6) showed that both the frontal and lateral ramal inclinations and the mandibular body length were larger on the right side than on the left side, which contributed to the mandibular deviation toward the left (Figure 4B). Not only was mandible asymmetry present, but the bilateral orbital, zygomatic and maxilla were also asymmetrically developed. There were no obvious symptoms in her ear.
| Pretreatment | Posttreatment | Norm ± SD | |
| Skeletal | |||
| SNA (°) | 86.6 | 86.9 | 82.0 ± 3.5 |
| SNB (°) | 84.7 | 83.0 | 80.9 ± 3.4 |
| ANB (°) | 1.9 | 3.9 | 1.6 ± 1.5 |
| Pog-NB (mm) | 0.9 | 2.0 | 3.0 ± 1.7 |
| FMA (°) | 23.0 | 35.7 | 22.9 ± 4.5 |
| Wits (°) | -5.7 | -3.8 | -1.0 ± 1.0 |
| S-Go/N-Me | 69 | 65.8 | 65.0 ± 4.0 |
| Y-Axis (°) | 65.5 | 67.1 | 67.0 ± 5.5 |
| MP-SN (°) | 30.8 | 35.7 | 33.0 ± 6.0 |
| Dental | |||
| U1-NA (mm) | 2.8 | 2.7 | 4.3 ± 2.7 |
| U1-NA (°) | 17.2 | 17.4 | 22.8 ± 5.7 |
| L1-NB (mm) | 3.8 | 5.2 | 4.0 ± 1.8 |
| L1-NB (°) | 21.7 | 35 | 25.3 ± 6.0 |
| U1-SN (°) | 103.8 | 102.4 | 103.1 ± 5.5 |
| IMPA (°) | 86.2 | 96.3 | 95.0 ± 7.0 |
| FMIA (°) | 70.8 | 56.2 | 65.7 ± 8.5 |
| Pretreatment | Posttreatment | Norm ± SD | |
| Maxillo-Mandibular relationships | |||
| Frontal convexity, left (mm) | 16.9 | 13.9 | 11.9 ± 2.5 |
| Frontal convexity, right (mm) | 11.1 | 12.0 | 11.9 ± 2.5 |
| Maxillo-Mandi Midline (mm) | -14.3 | 0.7 | 0.0 ± 2.0 |
| Skeletal/Dental | |||
| Occlusal plane tilt | -4.9 | -0.4 | 0.0 ± 2.0 |
| Molar to jaw, left (mm) | 10.3 | 11.0 | 13.1 ± 1.7 |
| Molar to jaw, right (mm) | 8.0 | 11.2 | 13.1 ± 1.7 |
| Denture to jaw midline (mm) | -1.5 | 0.2 | 0.0 ± 1.5 |
| Deep skeletal structure | |||
| Maxillary width (mm) | 62.3 | 62.4 | 64.1 ± 3.0 |
| Mandibular width (mm) | 85.6 | 81.5 | 81.3 ± 3.0 |
| Facial width (mm) | 129.0 | 128.8 | 124.7 ± 3.0 |
Considering the severely inclined occlusal plane and facial asymmetry, combined orthodontic-orthognathic treatment was a valid approach to achieve an ideal treatment outcome.
Conventional orthodontic-orthognathic treatment includes three phases: (1) Presurgical orthodontics to decompensate the dentition to increase the magnitude of surgical correction; (2) Orthognathic surgery to correct the skeletal deformity; and (3) Postsurgical orthodontics to finish and detail the occlusion. However, one drawback is that the time-consuming presurgical orthodontic treatment typically worsens the facial appearance and exacerbates the malocclusion, which does not resolve the patient’s chief complaint.
The SFA corrects the skeletal deformity early and is followed by postsurgical orthodontics to decompensate the dentition and stabilize the occlusion. This approach promotes rapid improvement in facial aesthetics and considerably reduces the overall treatment time. When presurgical orthodontics is not performed to decompensate the dentition and identify the true underlying skeletal deformity, incorporating decompensation movements of the dentition into surgical planning requires strong collaborations between skilled orthodontists and surgeons to predict accurately the surgical skeletal movement and postsurgical tooth movement.
Based on comprehensive examinations and analyses, including cephalometric analysis, dental cast predictions, and surgical simulations on profile images of the patient that were performed on imaging software (Dolphin Imaging and Management Solutions, Chatsworth, CA, United States), it was determined that the treatment plan should include a LeFort 1 osteotomy to advance and move the maxilla clockwise, a bilateral sagittal split ramus osteotomy to create a differential setback and coordination of the maxilla to correct the facial asymmetry and the skeletal deformity and postsurgical orthodontics to obtain a stable occlusion.
The patient was diagnosed with the following: (1) Mild HFM that was primarily attributed to unilateral abnormal development of the maxilla and mandible in three dimensions; (2) A congenitally missing tooth (17); (3) Two teeth with microdontia (12 and 22); and (4) Chronic periodontitis.
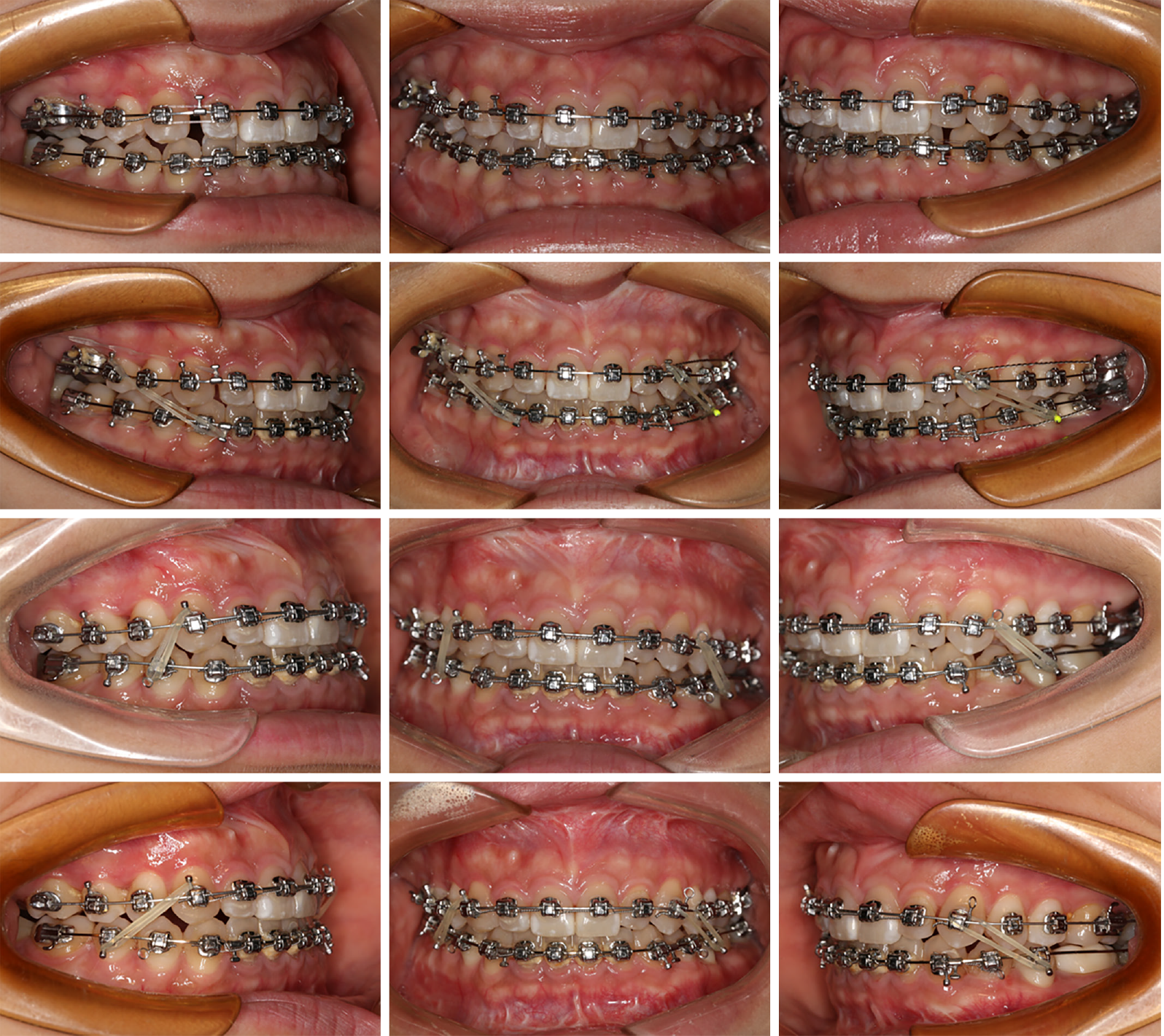
After considering the two treatment alternatives (conventional orthodontic-orthognathic treatment and the SFA), the authors and the patient decided on the SFA: Two-jaw surgery followed by postsurgical orthodontics for decompensation to achieve a proper incisor inclination and stable occlusion. After the initial phase of the periodontal treatment, preadjusted 0.022-0.028-in brackets (DamonTM Q Standardized Torque, Ormco Corporation, Orange, CA, United States) were directly bonded to all teeth (except 47) 1 wk before surgery, with initial 0.014-in nickel-titanium archwires in both arches. Both orthodontists and surgeons participated in the surgical plan to predict accurately the surgical skeletal movement and postsurgical tooth movement.
It is worth mentioning that we used the palatal suture as the midline of the maxilla to center the maxilla. Then, the maxillary movement was expected to advance by 1.5 mm and drift to the left by 2 mm, leading to 2 mm of impaction on the right side and 2 mm of extrusion on the left side. Although the postsurgery dental midline can divert to the left (without presurgical orthodontics being performed to decompensate the dentition) (Figure 3B), the maxilla was located in the center of the craniofacial area, which contributed the same nasolabial sulcus depth on both sides and a balanced facial appearance. A self-tapping miniscrew (MB105-1.6×11×7.3, Ningbo Cibei Medical Treatment Appliance Co. Ltd., Cixi, China) was placed behind the roots of the maxillary first molar on the labial side in surgery to retract with strong anchorage and to coordinate the midline in postsurgical orthodontics. The mandible was moved back by 3 mm on the left and 9 mm on the right, and the chin was placed in the middle. Considering the asymmetry of the height of the mandibular body and the mandibular angle, curved mandibular angle osteotomy and contour repair of the edge of the mandible were also carried out to correct the skeletal asymmetry. Rigid fixation was used in the maxilla and the mandible without any intermaxillary fixation.
Four weeks after the operation, the patient was referred back to the clinic to begin her postsurgery orthodontic treatment. The postsurgery face evaluation showed a symmetrical facial appearance and a straight profile. The intraoral examination showed a dental class II occlusal relationship with 6 mm of overjet (Figure 7). Orthodontic alignment and leveling of the maxillary and mandibular dental arches were performed with 0.014-in, 0.016-in, 0.016-0.022-in and 0.018-0.025-in superelastic NiTi wires. To expand the upper arch and coordinate with the lower arch, the inclinations of the posterior maxillary teeth, especially on the right side, were corrected by individual twists in the stainless-steel arches (lingual root torque) to allow the teeth to be properly positioned relative to the jaws. We used 0.019-0.025-in stainless steel wires for finishing and detailing (Figure 8). All brackets and miniscrews were debonded and removed at 20 mo, and the patient was referred to restore 36 and 47. Considering the patient’s lightly tetracycline stained teeth and the abnormal maxillary lateral incisor, she was also referred for aesthetic restoration with ceramic veneer in the maxilla and mandibular anterior region. Hawley retainers were designed to prevent the recurrence of the deformity.
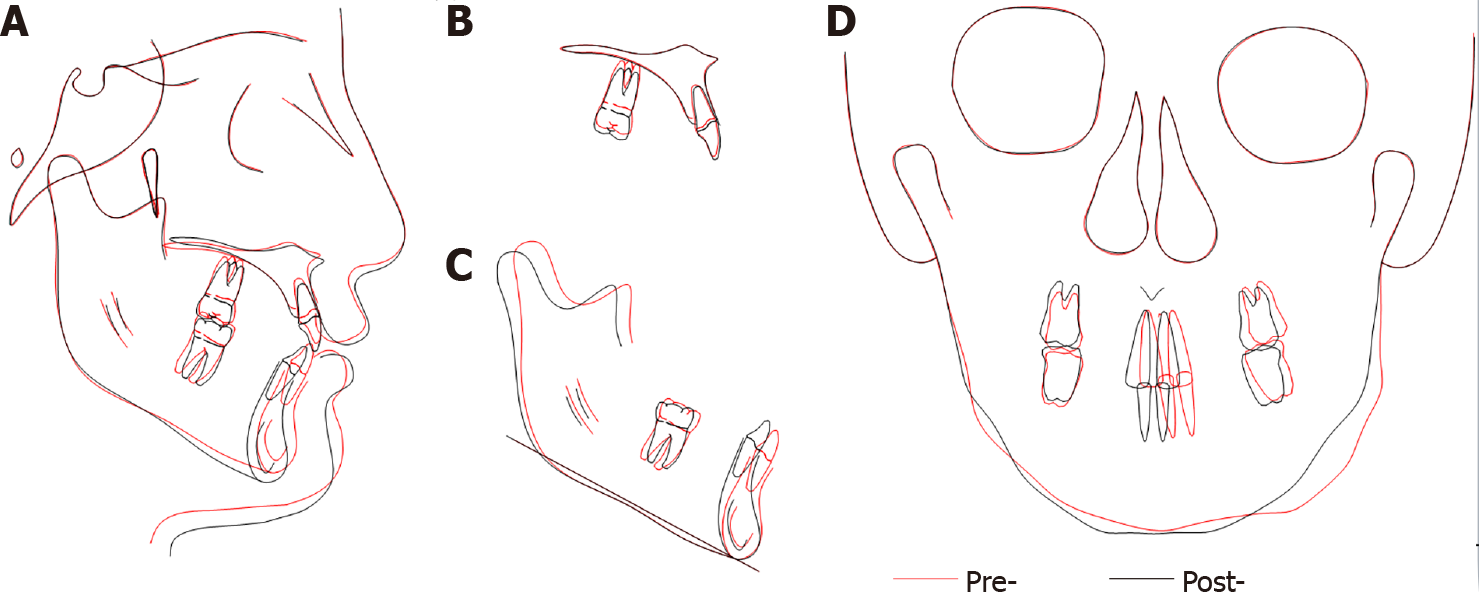
The posttreatment photographs of the patient confirmed good aesthetic and occlusal results (Figures 9 and 10). The cephalometric analysis (Figure 11, Tables 2 and 3) and the superimposition (Figure 12) showed significant improvement in the soft and hard tissues. The panoramic radiograph confirmed parallel root positioning (Figure 11C). The facial asymmetry analysis performed by CBCT showed that both the source and magnitude of the deviations were corrected (Figure 6). The CBCT image of the TMJ showed no significant change in the condylar region after treatment (Figure 5).
HFM is a complex form of dysmorphogenesis with a wide range of clinical presentations in terms of severity[4]. Although the exact etiology of HFM has not yet been determined, Kearns et al[5] hypothesized that abnormal mandibular growth is the earliest skeletal manifestation and plays a vital role in progressive deformity. When mandibular growth is restricted, vertical growth of the midface also diminishes, causing a tilted maxillary occlusal plane and asymmetry of the zygomatic and orbital regions. The Pruzansky-Kaban classification includes three mandibular types that are distinguished based on the degree of mandibular hypoplasia and the positions of the TMJ and glenoid fossa: Type I (normally shaped but small in size), type II (hypoplastic or malformed, and sometimes malpositioned) and type III (the TMJ, ramus, and glenoid fossa are absent)[15-17]. For mild and moderate HFM adult patients, the aim of treatment is to correct the asymmetries in both the maxilla and the mandible. Combined orthodontic-orthognathic treatment was the approach used to achieve the above objectives.
Recently, the SFA was introduced to overcome some of the limitations of conventional orthodontic-orthognathic treatment for mild to moderate HFM. It is well documented that HMF patients typically suffer from low confidence and even self-contempt[18,19]. Some of them are eager to improve their facial aesthetics and want to prevent the progressive deterioration of their facial appearance that can occur with presurgical orthodontics. A meta-analysis on the impact of the SFA indicated that SFA can immediately and persistently contribute to better oral health-related quality of life in patients with dentofacial deformities[20]. The SFA not only promotes rapid improvement in facial appearance but also considerably reduces the overall treatment time by eliminating the time-consuming presurgical orthodontic stage and facilitating tooth movement after surgery. The phenomenon of increased mobility of the teeth after orthognathic surgery has been attributed to the regional acceleratory phenomenon (RAP).
The RAP is a physiologic process that involves a decrease in regional bone density and accelerated bone turnover, causing fast tissue reorganization and healing[21]. Several mechanisms have been proposed for the osteopenic effect in the RAP[22-24]. Liou et al[13] demonstrated that the level of serum C-terminal telopeptide of type I collagen (a candidate marker to detect the activities of osteoclasts) significantly increased in the first week to the third month postoperatively and that the serum alkaline phosphatase (an enzyme for bone formation and associated with osteoblasts) increased in the first to fourth month postoperatively, which indicated a transient burst of bone remodeling and turnover activities after orthognathic surgery. The SFA takes advantage of this 3-4 mo golden window for the most time-consuming stage: Alignment, leveling and decompensation, thus considerably reducing the overall treatment time[13].
Although the SFA provides several positive aspects, developing accurate designs of skeletal movement and incorporating decompensation movements of the dentition into surgical planning are the keys to successful treatment. Previous studies have suggested that the correction of mandibular asymmetry is the key to the treatment of facial asymmetry[25-28]. However, maxilla asymmetry (the difference between the two sides of maxilla height and the deviation of middle palatal suture) is also related to the inclination of the occlusal plane and the difference in the nasolabial sulcus depth on both sides. Thus, the correction of the maxillary deviation is also important for patients with skeletal asymmetry, especially for HFM patients who have complex three-dimensional craniomaxillary deformities[29]. For the patient in our study, we used the palatal suture as the midline of the maxilla to center the maxilla. Considering the deviation in the palatal suture, we shifted the maxilla to the left by 2 mm to align the middle palatal suture with the midline of the craniofacial suture, which may contribute the same nasolabial sulcus depth on both sides and a balanced facial appearance. Shifting of the maxilla may make the central upper dental midline move to the left, which is due to a lack of presurgical orthodontic decompensation to align the midlines of the upper dentition and the maxilla. Then, a miniscrew was placed behind the roots of the maxillary first molar on the labial side to retract with strong anchorage and to align the midlines in postsurgical orthodontics. The CBCT image analysis of facial asymmetry showed that the height of the right maxilla is higher than that of the left maxilla. We created impaction by 2 mm on the right side and extrusion by 2 mm on the left side to correct the inclination of the occlusal plane. The movement of the mandible was also planned according to the CBCT analysis of facial asymmetry to correct the skeletal deformity and to obtain a balanced facial appearance.
In addition to correcting the skeletal deformities, obtaining a balanced soft-tissue appearance is also important in these HFM patients. Previous discussions in the literature regarding facial symmetry are associated with facial attractiveness, and the chin is the most striking feature related to facial asymmetry[30,31]. Therefore, facial asymmetry is usually defined by the extent of soft-tissue menton deviation from the midsagittal reference midline[32]. Typically, the midsagittal reference midline is defined as a line perpendicular to the pupillary line[33]. However, considering the asymmetrically developed orbital and zygomatic bones in these hemifacial hypoplasia patients, we cannot completely correct these patients' facial asymmetry. It was difficult to place the chin of this patient in the proper position to attain a symmetrical and balanced facial appearance. For this patient, we used the line between the point of nasion of soft tissue and the point of subnasale as the facial reference midline to locate her chin. Although the soft-tissue menton was not consistent with the line perpendicular to the pupillary line, the final results confirm a relatively symmetrical facial appearance.
With collaborations between skilled orthodontists and surgeons, mild HFM can be corrected by the SFA. The SFA promotes rapid improvement in facial aesthetics and considerably reduces the overall treatment time.
It is worth mentioning that we used the palatal suture as the midline of the maxilla in the surgical plan to center the maxilla and obtain a balanced facial appearance.
In these HMF patients with complex dentofacial deformities, placing the chin in the proper position is important for obtaining a relatively symmetrical facial appearance.
I would like to thank the patient for her cooperation during the treatment. Thanks to my colleagues and nursing staff in our hospital.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Chinese Stomatological Association, No. 072599; and Chinese Orthodontic Society, No. COS05572.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Galiatsatos A S-Editor: Huang P L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Werler MM, Starr JR, Cloonan YK, Speltz ML. Hemifacial microsomia: from gestation to childhood. J Craniofac Surg. 2009;20 Suppl 1:664-669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Hartsfield JK. Review of the etiologic heterogeneity of the oculo-auriculo-vertebral spectrum (Hemifacial Microsomia). Orthod Craniofac Res. 2007;10:121-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Birgfeld CB, Luquetti DV, Gougoutas AJ, Bartlett SP, Low DW, Sie KC, Evans KN, Heike CL. A phenotypic assessment tool for craniofacial microsomia. Plast Reconstr Surg. 2011;127:313-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Kaban LB. Mandibular asymmetry and the fourth dimension. J Craniofac Surg. 2009;20 Suppl 1:622-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Kearns GJ, Padwa BL, Mulliken JB, Kaban LB. Progression of facial asymmetry in hemifacial microsomia. Plast Reconstr Surg. 2000;105:492-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 82] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Proffit WR, White RP Jr. Combined surgical-orthodontic treatment: how did it evolve and what are the best practices now? Am J Orthod Dentofacial Orthop. 2015;147:S205-S215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Luther F, Morris DO, Hart C. Orthodontic preparation for orthognathic surgery: how long does it take and why? Br J Oral Maxillofac Surg. 2003;41:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 105] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | O'Brien K, Wright J, Conboy F, Appelbe P, Bearn D, Caldwell S, Harrison J, Hussain J, Lewis D, Littlewood S, Mandall N, Morris T, Murray A, Oskouei M, Rudge S, Sandler J, Thiruvenkatachari B, Walsh T, Turbill E. Prospective, multi-center study of the effectiveness of orthodontic/orthognathic surgery care in the United Kingdom. Am J Orthod Dentofacial Orthop. 2009;135:709-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Hernández-Alfaro F, Guijarro-Martínez R, Peiró-Guijarro MA. Surgery first in orthognathic surgery: what have we learned? J Oral Maxillofac Surg. 2014;72:376-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 10. | Villegas C, Uribe F, Sugawara J, Nanda R. Expedited correction of significant dentofacial asymmetry using a "surgery first" approach. J Clin Orthod. 2010;44:97-103; quiz 105. [PubMed] |
| 11. | Liao YF, Chiu YT, Huang CS, Ko EW, Chen YR. Presurgical orthodontics versus no presurgical orthodontics: treatment outcome of surgical-orthodontic correction for skeletal class III open bite. Plast Reconstr Surg. 2010;126:2074-2083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 12. | Nagasaka H, Sugawara J, Kawamura H, Nanda R. "Surgery first" skeletal Class III correction using the Skeletal Anchorage System. J Clin Orthod. 2009;43:97-105. [PubMed] |
| 13. | Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: orthodontic guidelines and setup for model surgery. J Oral Maxillofac Surg. 2011;69:771-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 14. | Baek SH, Ahn HW, Kwon YH, Choi JY. Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: evaluation of surgical movement and postoperative orthodontic treatment. J Craniofac Surg. 2010;21:332-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 15. | Horgan JE, Padwa BL, LaBrie RA, Mulliken JB. OMENS-Plus: analysis of craniofacial and extracraniofacial anomalies in hemifacial microsomia. Cleft Palate Craniofac J. 1995;32:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 82] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Kaban LB, Mulliken JB, Murray JE. Three-dimensional approach to analysis and treatment of hemifacial microsomia. Cleft Palate J. 1981;18:90-99. [PubMed] |
| 17. | Kaban LB, Moses MH, Mulliken JB. Surgical correction of hemifacial microsomia in the growing child. Plast Reconstr Surg. 1988;82:9-19. [PubMed] |
| 18. | Lee S, McGrath C, Samman N. Quality of life in patients with dentofacial deformity: a comparison of measurement approaches. Int J Oral Maxillofac Surg. 2007;36:488-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Rankin M, Borah GL. Perceived functional impact of abnormal facial appearance. Plast Reconstr Surg. 2003;111:2140-2146; discussion 2147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 123] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 20. | Huang X, Cen X, Sun W, Xia K, Yu L, Liu J, Zhao Z. The impact of surgery-first approach on the oral health-related quality of life: a systematic review and meta-analysis. BMC Oral Health. 2019;19:136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Frost HM. The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 1983;31:3-9. [PubMed] |
| 22. | Frost HM. The biology of fracture healing. An overview for clinicians. Part I. Clin Orthop Relat Res. 1989;(248):283-293. [PubMed] |
| 23. | Frost HM. The biology of fracture healing. An overview for clinicians. Part II. Clin Orthop Relat Res. 1989;(248):294-309. [PubMed] |
| 24. | Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg. 2011;69:781-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 150] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 25. | Janson GR, Metaxas A, Woodside DG, de Freitas MR, Pinzan A. Three-dimensional evaluation of skeletal and dental asymmetries in Class II subdivision malocclusions. Am J Orthod Dentofacial Orthop. 2001;119:406-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Thiesen G, Freitas MPM, Araújo EA, Gribel BF, Kim KB. Three-dimensional evaluation of craniofacial characteristics related to mandibular asymmetries in skeletal Class I patients. Am J Orthod Dentofacial Orthop. 2018;154:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Haraguchi S, Takada K, Yasuda Y. Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 2002;72:28-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 28. | Pirttiniemi PM. Associations of mandibular and facial asymmetries--a review. Am J Orthod Dentofacial Orthop. 1994;106:191-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 77] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 29. | Hwang HS, Hwang CH, Lee KH, Kang BC. Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry. Am J Orthod Dentofacial Orthop. 2006;130:779-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 153] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 30. | Staudt CB, Kiliaridis S. Association between mandibular asymmetry and occlusal asymmetry in young adult males with class III malocclusion. Acta Odontol Scand. 2010;68:131-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Hu W, Zhou Y. The compensation of dental arch and teeth in patients with skeletal protrusion and deviation of mandible. Zhonghua Kouqiang Yixue Zazhi. 2002;37:180-182. [PubMed] |
| 32. | Cavalcanti MG, Rocha SS, Vannier MW. Craniofacial measurements based on 3D-CT volume rendering: implications for clinical applications. Dentomaxillofac Radiol. 2004;33:170-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 122] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 33. | Silva BP, Jiménez-Castellanos E, Stanley K, Mahn E, Coachman C, Finkel S. Layperson's perception of axial midline angulation in asymmetric faces. J Esthet Restor Dent. 2018;30:119-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |