Published online May 6, 2020. doi: 10.12998/wjcc.v8.i9.1752
Peer-review started: February 28, 2020
First decision: April 7, 2020
Revised: April 9, 2020
Accepted: April 24, 2020
Article in press: April 24, 2020
Published online: May 6, 2020
Processing time: 61 Days and 22.4 Hours
Lymphoepithelioma-like carcinoma (LELC) is a rare, malignant epithelial tumour which can arise within the upper urinary tract. This letter adds to a previous systematic review and cumulative analysis of 28 published upper urinary tract-LELC cases which provided insight into this disease; however, the current evidence does not provide clinicians with clear guidelines due to its rarity. Therefore, the aim was to report a new case of renal pelvis LELC presented in our hospital. In this instance, we were able to report treatment experience and long-term follow-up results. This patient presented with hypertension and haemturia which initiated further investigation. While ultrasound identified an hypechoic mass, no malignant cells were detected using cytological testing. Abdominal magnetic resonance imaging identified a slightly enhanced mass in the left renal pelvis with no evidence of lymph node metastasis. Ureteroscopic tumor biopsy suggested the existence of urothelial carcinoma, hence, laparoscopic radical left nephroureterectomy with bladder cuff excision was performed. Through patient-practitioner consultations, we decided to adopt a "watch and wait" approach after radical nephroureterectomy rather than administering chemotherapy. Although, we would encourage clinicians to record and publish cases to garner insight into this type of malignant disease.
Core tip: Lymphoepithelioma-like carcinoma arising within the upper urinary tract are extremely rare, and currently only 28 cases have been published. However, the current evidence is insufficient to provide clinicians with clear guidelines due to its rarity. Sharing new case reports of renal pelvis lymphoepithelioma-like carcinoma and treatment experiences is necessary. Our treatment experience and long-term follow-up results adds to this small but growing evidence base which suggests that favorable prognosis can be achieved with radical nephroureterectomy based therapy, even for some with later stage tumors.
- Citation: Lai SC, Seery S, Diao TX, Wang JY, Liu M. Rare primary lymphoepithelioma-like carcinoma of the renal pelvis. World J Clin Cases 2020; 8(9): 1752-1755
- URL: https://www.wjgnet.com/2307-8960/full/v8/i9/1752.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i9.1752
Lymphoepithelioma-like carcinoma (LELC) is a rare, malignant epithelial tumour which can arise within the upper urinary tract (UUT)[1,2]. Due to its rarity, little is known about this malignant neoplasm. We recently published a systematic review and cumulative analysis of all the 28 previously published UUT-LELC cases in an effort to support clinicians identifying and treating this disease[3]. We found that administering a radical nephroureterectomy (RNU) treatment was associated with better disease-free survival, although our tentative recommendations were based on only a modicum of evidence. Therefore, we hope to share a new renal pelvis LELC case in our hospital with long-term follow-up, and to develop the existing evidence-base for clinicians treating this rare malignant disease.
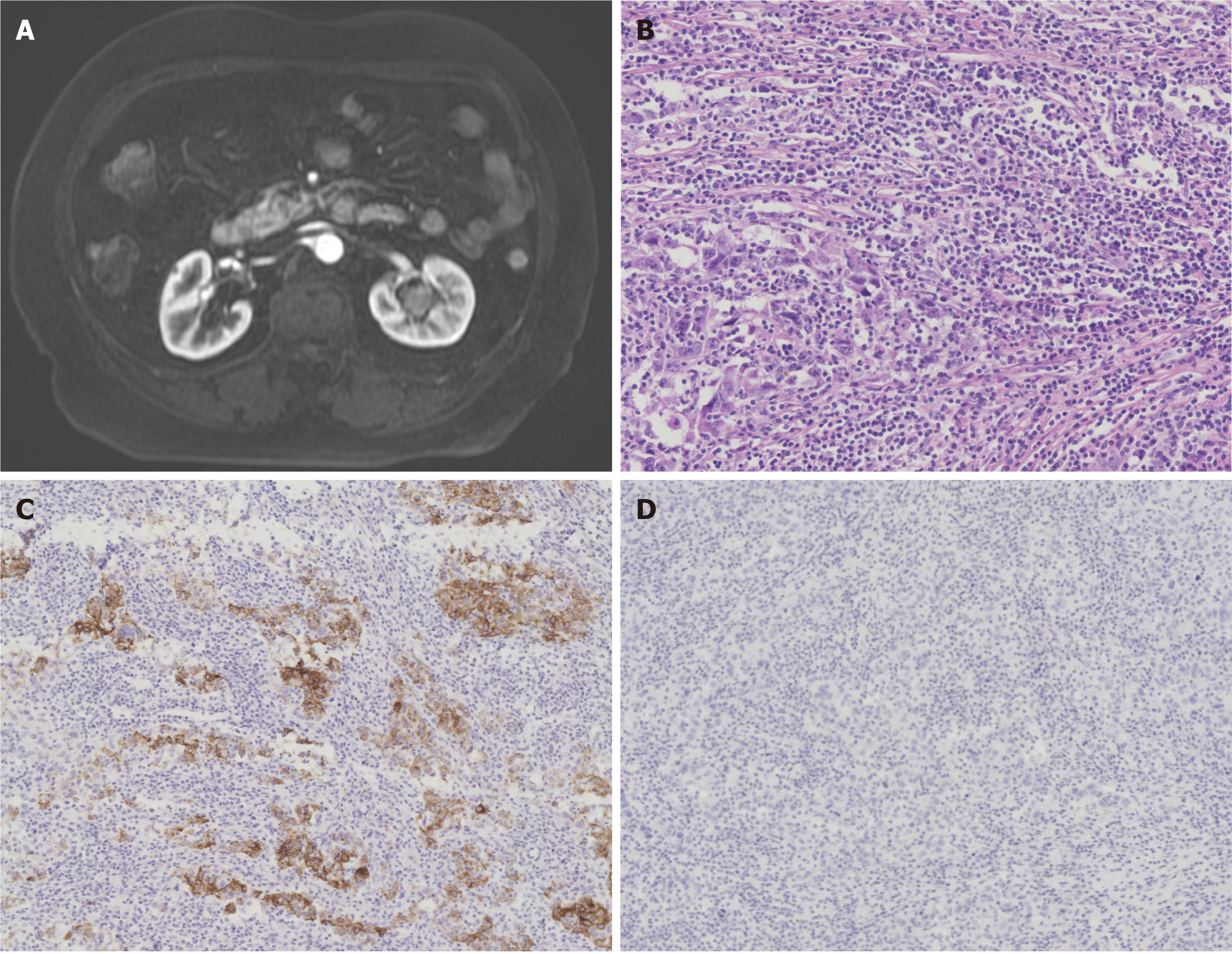
In this instance, a 75-year-old woman with an history of hypertension presented at our urology department in February 2011 having experienced two weeks of gross haematuria. A 1 cm × 1.2 cm hypoechoic mass in the left renal pelvis was found through ultrasound; however, no malignant cells were detected through cytological urine tests. The patient was sent for abdominal magnetic resonance imaging, which identified a slightly enhanced mass in the left renal pelvis although there was no evidence of lymph node metastasis (Figure 1A). Ureteroscopic tumor biopsy suggested the existence of urothelial carcinoma, hence, laparoscopic radical left nephroureterectomy with bladder cuff excision was performed.
Microscopic examination confirmed abundant lymphoid stroma surrounding the large polygonal tumour cells (Figure 1B). Immunohistochemical staining of polygonal tumour cells were returned positive for cytokeratin 7 (Figure 1C). Further, analysis of lymphoid stroma also yielded positive results for CD3 and CD20, although, Epstein-Barr virus immunostaining was negative (Figure 1D). This histological picture is compatible with the criteria for lymphoepithelial carcinoma and eventually the pathological stage was determined to be pT3N0M0. In view of this patient’s age and through a shared-decision making process which involved communicating the associated potential complications, we agreed to administer no additional therapy. Follow-up assessments including abdominal computed tomography scans and cystoscopies were taken during outpatient consultations. This lady remains in relative good health, without evidence of postoperative tumour recurrence at 93 mo.
This current case presented with similar characteristics to those previously published which commonly describe gross hematuria as the initial symptom and negative Epstein-Barr Virus testing[1,4,5]. However, pathological testing revealed two distinct histologic patterns, consisting of large predominant LELC and focal urothelial carcinoma in this case. Of note, the identified urothelial carcinoma was aggressive and may play a critical role in prognosis; although, previous literature suggests that predominant or pure subtype LELC have a relatively favorable prognosis compared to focal LELC[3,6,7]. Even though the pathological stage was pT3N0M0, which would usually require chemotherapy, through discussion with our patient we decided not to administer this intervention after RNU. Follow-up examinations provided no evidence of disease recurrence or metastasis.
This experience adds to this small but growing evidence base. Despite the sparsity of available data to guide decisions, favorable prognosis can be achieved with RNU based therapy which is evidence-based[3,8,9]. Having said that, there remains insufficient data on renal pelvis LELC to distinguish differences, therefore we encourage urologists to record and report these rare cases with longer follow-up. It remains of paramount importance to further assess the biologic behavior of these tumors and to identify the optimal management regimen and particularly disease prognostics.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Iijima S S-Editor: Wang J L-Editor: A E-Editor: Liu MY
| 1. | Fukunaga M, Ushigome S. Lymphoepithelioma-like carcinoma of the renal pelvis: a case report with immunohistochemical analysis and in situ hybridization for the Epstein-Barr viral genome. Mod Pathol. 1998;11:1252-1256. [PubMed] |
| 2. | Perez-Montiel D, Wakely PE, Hes O, Michal M, Suster S. High-grade urothelial carcinoma of the renal pelvis: clinicopathologic study of 108 cases with emphasis on unusual morphologic variants. Mod Pathol. 2006;19:494-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 138] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Lai SC, Seery S, Zhang W, Liu M, Zhang G, Wang JY. Lymphoepithelioma-like carcinoma of the upper urinary tract: A systematic review of case reports. World J Clin Cases. 2020;8:771-781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Iezzoni JC, Gaffey MJ, Weiss LM. The role of Epstein-Barr virus in lymphoepithelioma-like carcinomas. Am J Clin Pathol. 1995;103:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 257] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Wen SC, Shen JT, Jang MY, Tsai KB, Chang SF, Tsai LJ, Wu WJ. Lymphoepithelioma-like carcinoma of ureter-a rare case report and review of the literature. Kaohsiung J Med Sci. 2012;28:509-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Porcaro AB, Gilioli E, Migliorini F, Antoniolli SZ, Iannucci A, Comunale L. Primary lymphoepithelioma-like carcinoma of the urinary bladder: report of one case with review and update of the literature after a pooled analysis of 43 patients. Int Urol Nephrol. 2003;35:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Tamas EF, Nielsen ME, Schoenberg MP, Epstein JI. Lymphoepithelioma-like carcinoma of the urinary tract: a clinicopathological study of 30 pure and mixed cases. Mod Pathol. 2007;20:828-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Ahn H, Sim J, Kim H, Yi K, Han H, Chung Y, Rehman A, Paik SS. Lymphoepithelioma-like Carcinoma of the Renal Pelvis: A Case Report and Review of the Literature. Korean J Pathol. 2014;48:458-461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Yamada Y, Fujimura T, Yamaguchi T, Nishimatsu H, Hirano Y, Kawamura T, Teshima S, Takeuchi T, Kitamura T. Lymphoepithelioma-like carcinoma of the renal pelvis. Int J Urol. 2007;14:1093-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |