Published online May 6, 2020. doi: 10.12998/wjcc.v8.i9.1721
Peer-review started: December 28, 2019
First decision: January 19, 2020
Revised: March 27, 2020
Accepted: April 17, 2020
Article in press: April 17, 2020
Published online: May 6, 2020
Processing time: 124 Days and 0.5 Hours
Ventral hernia, also known as incisional hernia, is a common complication of previous surgery. The contents of ventral hernia may include omentum, preperitoneal fat, small intestine or colon. However, ventral hernia with protrusion of more than two parenchymal organs simultaneously is extremely rare, and its repair is very complex and difficult. Surgeons should make a comprehensive assessment based on their own experience and the individual characteristics of the hernia. In addition, psychological therapy should be emphasized in the whole treatment process.
We report a rare case of asymptomatic giant ventral hernia for 15 years in a 21-year-old female. The patient underwent umbilical hernia repair at the age of 1 year. Approximately 5 years later, ventral hernia recurred and repair with Mesh was performed, but the operation failed due to postoperative infection, and a huge mass appeared in the left abdominal wall. The mass increased gradually with the development and maturity of the body. Computerized tomography scan demonstrated that the patient's total spleen, part of the pancreas and left lobe of the liver were simultaneously herniated through the abdominal incisional hernia. As the patient was unable to endure the inconvenience of life and the potential risk of spleen or liver rupture, she underwent a ventral hernia repair with Mesh at our hospital. The operation was successful and the patient had a good recovery. During a 3-mo follow-up, the patient remained asymptomatic and the appearance of the surgical incision was greatly improved.
Ventral hernia is a common complication of abdominal surgery. Ventral hernia with protrusion of more than two parenchymal organs simultaneously is extremely rare. Surgeons should pay attention to the psychological treatment while restoring the abdominal physiological function in ventral hernia patients.
Core tip: We report a rare case of giant ventral hernia simultaneously containing the spleen, a portion of the pancreas and the left hepatic lobe. Abdominal parenchymal organs such as liver, spleen and pancreas are rarely found in the ventral hernia either separately or simultaneously. Surgeons should pay attention to the psychological treatment while restoring the abdominal physiological function in ventral hernia patients.
- Citation: Luo XG, Lu C, Wang WL, Zhou F, Yu CZ. Giant ventral hernia simultaneously containing the spleen, a portion of the pancreas and the left hepatic lobe: A case report. World J Clin Cases 2020; 8(9): 1721-1728
- URL: https://www.wjgnet.com/2307-8960/full/v8/i9/1721.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i9.1721
Ventral hernia is a common complication of abdominal surgery, with an incidence ranging from 9% to 20%[1]. The risk of ventral hernia is about 10% for elective abdominal surgery, while it is significantly increased to 33% following emergency abdominal operation[2]. The contents of ventral hernia may include omentum, preperitoneal adipose tissue, small intestine or colon. Ventral hernia with protrusion of more than two parenchymal organs simultaneously is extremely rare. The development of giant ventral hernia has a negative impact on the physiology of patients, such as pain, and inability to carry out daily activities. More importantly, significantly increased negative psychological effects, such as disturbances to mood, sleep, relationships with others and pleasure of life, lead to a poor quality of life[3].
We here report a rare case of asymptomatic giant ventral hernia with the protrusion of total spleen, partial pancreas and left hepatic lobe simultaneously through abdominal incision for 15 years in a 21-year-old female. The patient underwent a ventral hernia repair with Mesh at our hospital and had a good recovery.
A 21-year-old female patient was admitted to the Department of General Surgery in the Second Affiliated Hospital of Nanjing Medical University (Nanjing, China) on July 1, 2019, with chief complaints of giant ventral hernia without any other special discomfort for 15 years.
The patient underwent umbilical hernia repair at the age of 1 year. Approximately 5 years later, ventral hernia recurred and repair with Mesh was performed, but the operation failed due to postoperative infection, and a huge mass appeared in the left abdominal wall. The mass increased gradually with the development and maturity of the body.
The patient denied fever, cough, expectoration, nausea, vomiting, defecation difficulties, melena and hematochezia. There was no other significant surgery and special medications in her past medical and family histories.
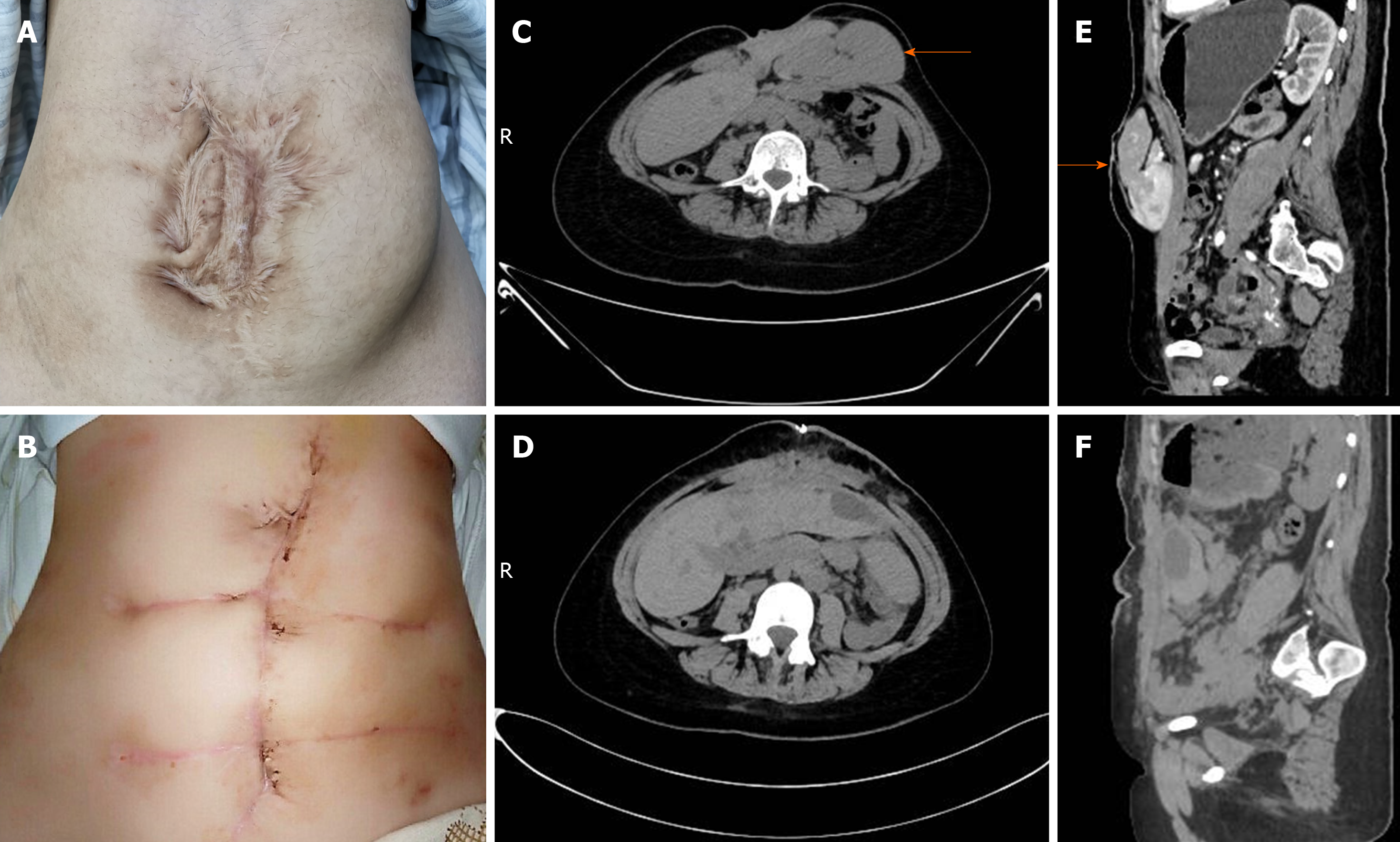
No abnormality was found in her vital signs. Physical examination showed no obvious cardiovascular or respiratory abnormalities. Her abdomen was soft and there were no obvious signs of tenderness or rebound pain. Murphy’s sign was negative. Many irregular and obsolete surgical scars could be seen on the abdominal wall. There was a giant ventral hernia about 10 cm × 10 cm with clear boundaries, tenderness and poor mobility (Figure 1A). Auscultation revealed no abnormal bowel sounds.
Electrocardiogram was unremarkable and laboratory examination results, including blood, urine, stool, liver and kidney function, and coagulation tests, were within normal ranges.
Based on the examination results, together with the patient's history and symptoms, a giant ventral hernia was diagnosed.
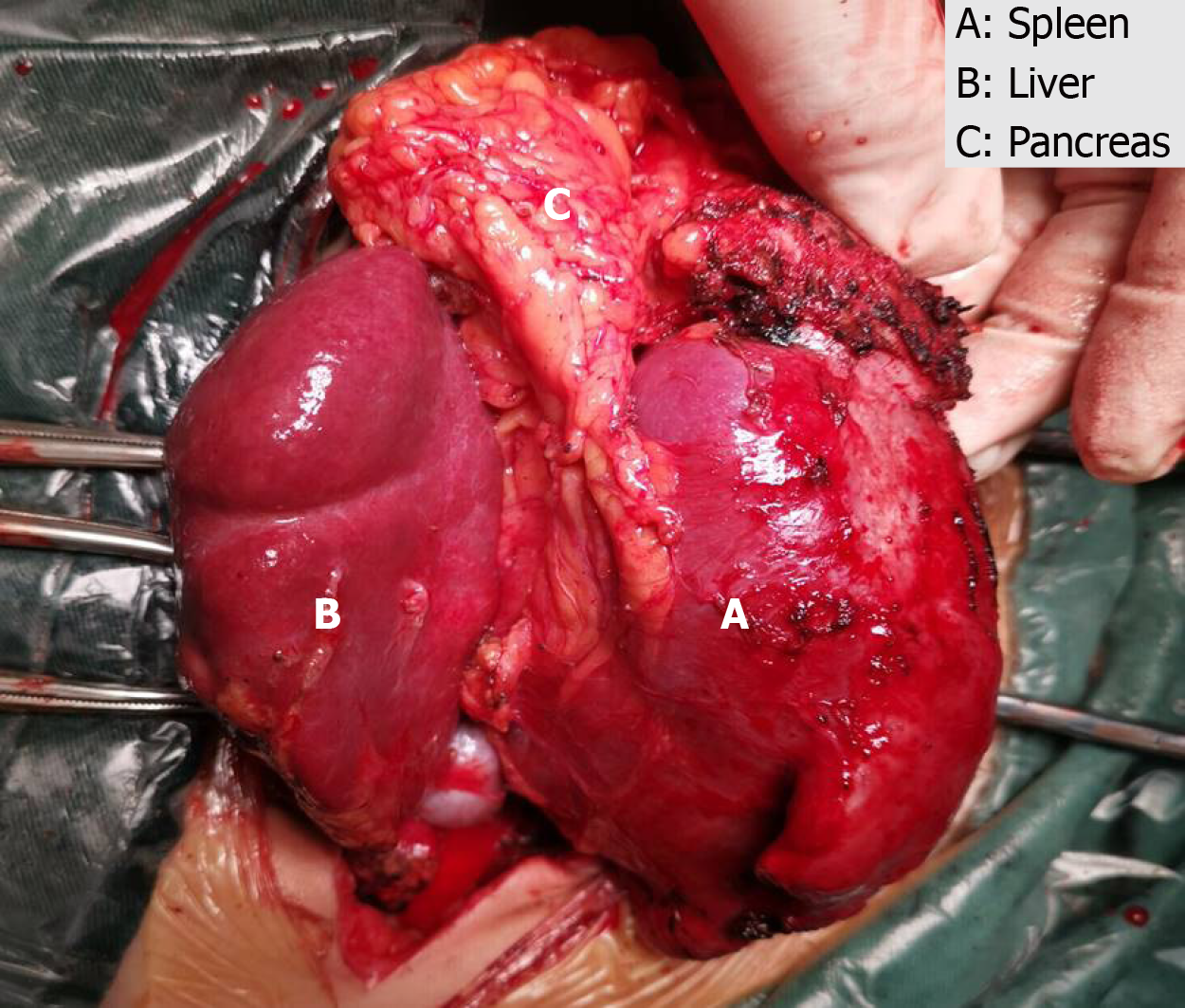
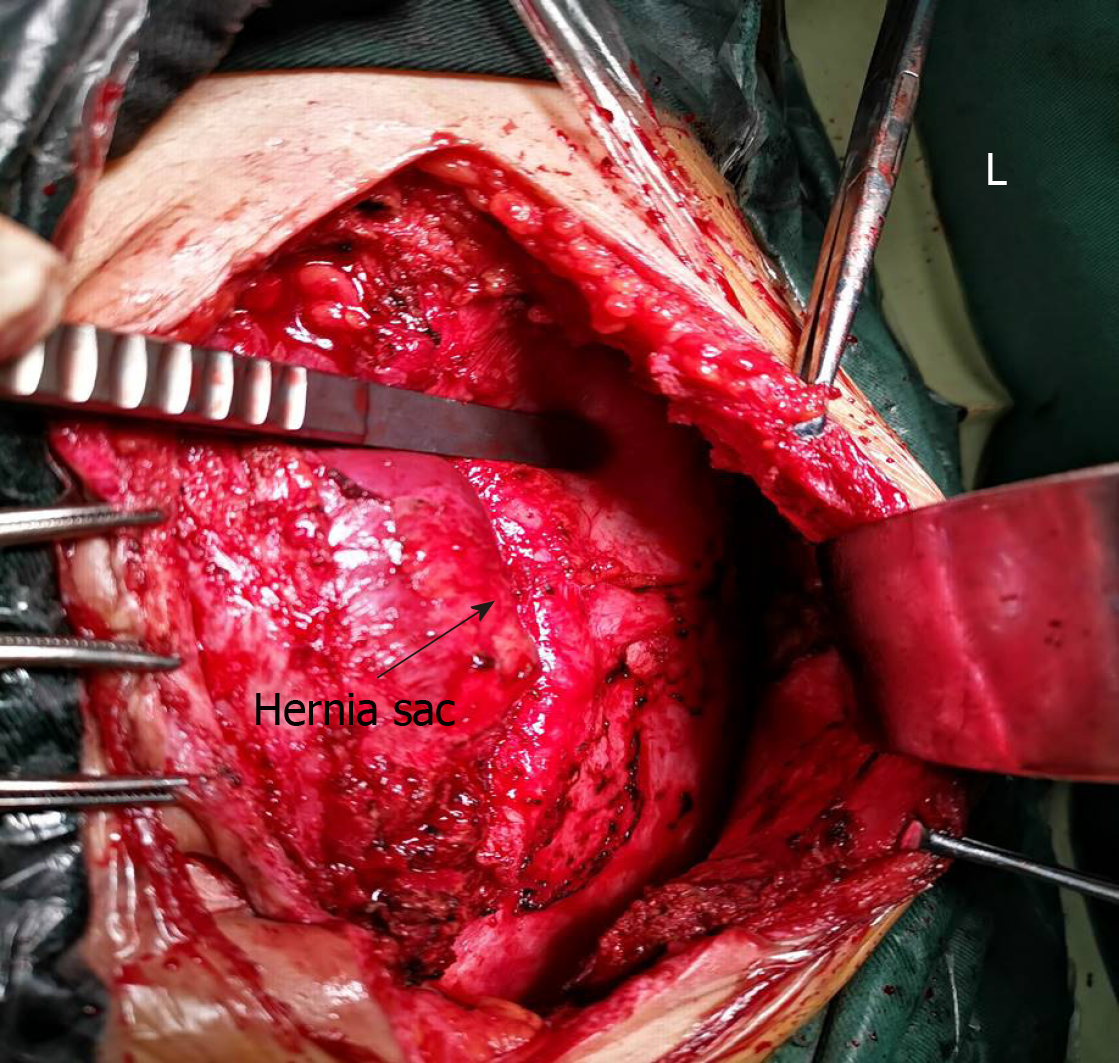
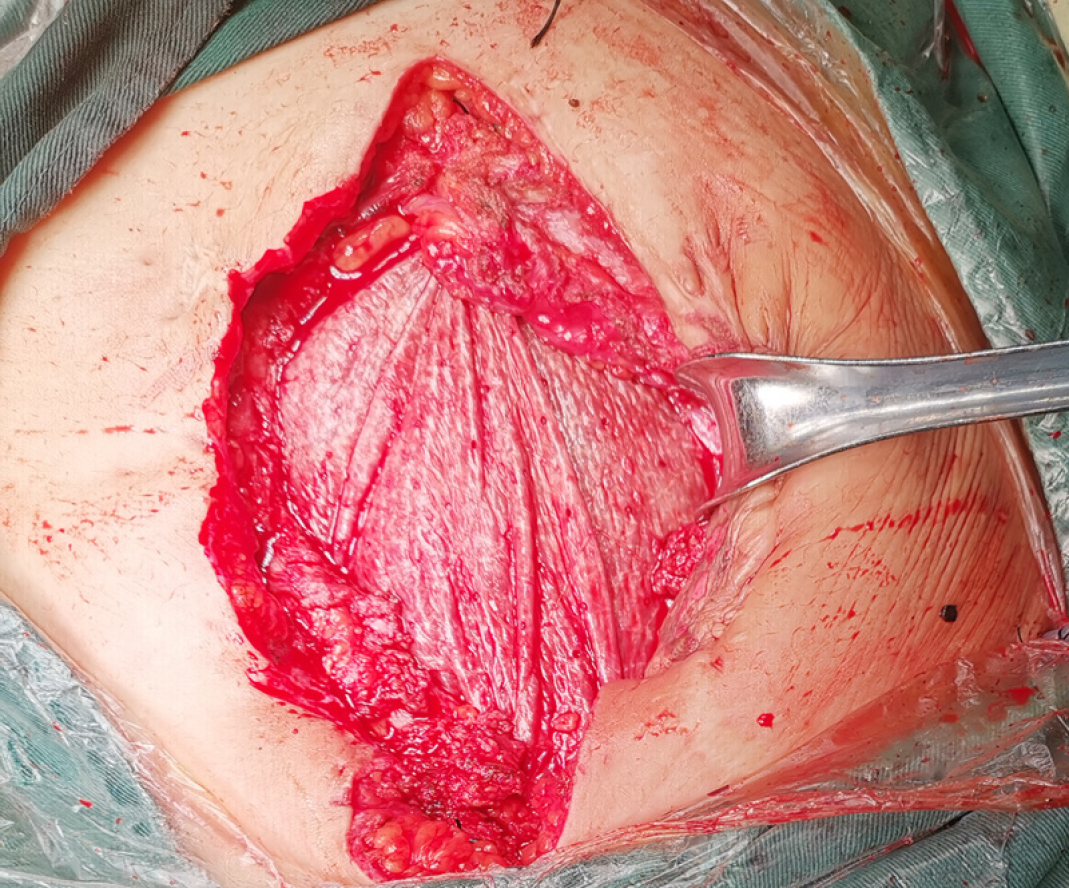
As the patient was unable to endure the inconvenience of life and the potential risk of spleen or liver rupture, she underwent a ventral hernia repair with Mesh at our hospital. Adequate pre-operative assessment and discussion were carried out due to the absence of indications for emergency surgery. During the laparotomy, between the adipose layer of the abdominal wall and the anterior sheath of the rectus abdominis, herniation of the spleen, part of the left lobe of the liver and the pancreas was observed, and the herniation was closely adhered to each other (Figure 2). The spleen, part of the left liver lobe and pancreas were safely and thoroughly separated from severe and extensive adhesions and reverted into the abdominal cavity. The hernia cystic ring was about 10 cm × 10 cm in size, and approximately 3/4 of the hernia sac was located under the left abdominal wall and 1/4 under the right abdominal wall (Figure 3). When the intra-abdominal adhesions were separated at approximately 5 cm around the defect, a COOK 15 cm × 13 cm biological Mesh was fixed to the retroperitoneum (Figure 4). Silica gel drainage tube was inserted into the left hernia sac cavity and then negative pressure ball was connected. The original skin scar was removed and tension reduction suture was made. The postoperative recovery was uneventful. Postoperative abdominal CT scan revealed that the contents of ventral hernia, including liver, pancreas, spleen and blood vessels, had returned to the abdominal cavity (Figure 1D and F).
She had a good recovery and was discharged 18 d after the operation. During the 3-mo follow-up, the patient remained asymptomatic and the appearance of the surgical incision was greatly improved (Figure 1B).
Ventral hernia is divided into congenital and acquired hernia. The latter is mainly due to previously abdominal surgery or unsuccessful hernia repair. Therefore, its repair is very complex and difficult [4]. The incidence of ventral hernia is rising rapidly due to the increase of elderly, obese and diabetic patients[5] and other factors, such as poor nutrition, surgical site infection and increased intra-abdominal pressure[6]. In the vast majority of cases, the contents of ventral hernia include small intestine, colon, fat or fibrous tissue with the most serious complication of impaired intestinal blood supply which usually leads to intestinal incarceration and necrosis[4]. Abdominal parenchymal organs such as liver, spleen and pancreas are rarely found within the ventral hernia either separately or simultaneously. The clinical cases were searched through PubMed between January 2000 and January 2019 using the following search terms, single or in combination: Hernia, liver, spleen and pancreas. Reports of hiatal hernia, diaphragmatic hernia, para-esophageal hernia, and inguinal hernia were excluded. Twenty cases were identified (Table 1). The case we present here, to our knowledge, is the first case of giant ventral hernia which simultaneously contained the spleen, a portion of the pancreas and the left hepatic lobe.
| Ref. | Age (yr) | Gender | Clinical manifestation | Imaging examination | Hernia classification | Herniated organs | Complica-tions | Treatment |
| Neelamraju et al[6], 2015 | 70 | Female | Epigastric swelling and discomfort | Abdo CT | Incisional hernia | Omentum and left hepatic lobe | None | Open incisional hernia repair |
| Sheer et al[10], 2004 | 45 | Female | Upper Abdo pain and swelling | Abdo CT | Incisional hernia | Liver | Pseudomonas sepsis; died | Conservative |
| Shanbhogue et al[17], 2009 | 48 | Female | Discomfort and swelling in the epigastrium | Abdo CT | Incisional hernia | Segment of the left hepatic lobe | None | Conservative |
| Eken et al[11], 2015 | 77 | Female | Abdo swelling, pain, nausea and vomiting | Abdo CT | Incisional hernia | Left hepatic lobe | Hepatic dysfunction | Open incisional hernia repair |
| Nuño-Guzmán et al[12], 2012 | 70 | Female | Right Abdo pain, nausea, vomiting, and jaundice | Abdo CT | Incisional hernia | Left hepatic lobe | None | Open incisional hernia repair |
| Warbrick-Smith et al[18], 2012 | 81 | Male | Right upper quadrant Abdo pain | Abdo CT | Incisional hernia | II and III segments of the liver | None | No treatment |
| Then et al[14], 2019 | 54 | Male | Increasing abdominal girth | Abdo CT | Incisional hernia | Anterior portion of the left hepatic lobe | None | Conservative |
| Saujani et al[13], 2017 | 75 | Female | Right upper quadrant Abdo tightness and band-like pain | Abdo CT | Incisional hernia | V and VI segments of the liver | Budd-Chiari syndrome | Conservative |
| Kanakaratne et al[19], 2017 | 75 | Female | Abdo pain, nausea, vomiting, constipation and dysuria | Abdo CT | Incisional hernia | Left hepatic lobe | None | Conservative |
| Fernando et al[7], 2015 | 82 | Female | Left-sided Abdo pain, fatigue, weakness | Abdo CT | Umbilical hernia | Small bowel, colon, pancreas, spleen | Splenic rupture | Splenectomy |
| Komaei et al[8], 2019 | 67 | Female | Severe epigastric pain radiating to the back, nausea, vomiting | Abdo CT | Paraumbilical hernia | Small bowel, segments of ascending, transverse and descending colon, pancreas | Acute pancreatitis and intestinal obstruction | Emergency laparotomy, multiorgan failure; died |
| Alam et al[9], 2014 | 56 | Female | Abdo pain, nausea | Abdo CT | Umbilical hernia | Small bowel, sigmoid and transverse colon, pancreas | Acute kidney injury | Emergency laparotomy, multiorgan failure; died |
Ventral herniation of spleen is extremely rare and almost all spleen-related hernias have been found to be associated with various types of diaphragmatic hernia, with only one case of congenital umbilical hernia. CT confirmed that spleen, small intestine, colon and pancreas protruded through umbilical hernia in an 82-year-old female patient who presented with left abdominal pain and weakness. Splenectomy and abdominal wall reconstruction were carried out without delay to avoid the rupture of the spleen with hemorrhage[7]. Few studies have reported that pancreas exists in umbilical or paraumbilical hernia. According to the previous literature, in 3 of the 12 patients, pancreas protruded through umbilical hernia (n = 2) and paraumbilical hernia (n = 1), rather than ventral hernia. In addition to pancreas, herniation of small intestine, colon (n = 3) and spleen (n = 1) could also be found. Although pancreatic herniation is rare, its clinical manifestations and complications are serious as the incarceration of the head of pancreas could easily lead to acute pancreatitis. The most serious clinical symptoms were found in a 67-year-old female patient who suffered from severe epigastric pain radiating to the back, nausea and vomiting caused by acute pancreatitis and intestinal obstruction. The patient died of multiple organ failure 20 d later although emergency operation was performed[8]. Another 56-year-old female patient with pancreatic herniation had a similar outcome and died of multiple organ failure 24 h after surgery[9]. The occurrence of hepatic herniation in 9 patients was all related to incisional hernia. The most frequent symptom of hepatic herniation was abdominal pain (n = 6) and swelling (n = 5). Among the 9 patients, 5 received observation and conservative treatment for the primary disease, but one of these patients died 9 d after admission due to Pseudomonas sepsis[10]. Open incisional hernia repair was performed in 2 patients[6,11] and in another case, the same surgery was performed simultaneously with the common bile duct exploration[12]. Although hepatic herniation usually protrudes through a large area of abdominal wall defect, it rarely leads to serious clinical manifestations. Hepatic encephalopathy or hepatic dysfunction occurred in a patient when the herniated left hepatic lobe was present[11]. In another patient, herniation of the right hepatic lobe might contribute to the clinical consequence of vascular compromise, which resulted in Budd-Chiari syndrome[13]. At present, there are no relevant epidemiological data due to the rarity of hepatic herniation[14].
All of the 12 cases were diagnosed by CT scan. Although it is not a routine imaging examination, CT scan is recommended for the diagnosis, especially for the content of hernia and the choice of treatment strategy[6]. Surgeons can evaluate and determine the safest and desirable Mesh placement method based on CT scan. Enhanced abdominal CT scan can assess the relationship between abdominal viscera and defects, especially in obese patients and those with a history of recurrent ventral hernia. Although enhanced abdominal CT may not be helpful in assessing whether or not there is adhesion, or the degree of adhesion, it can discover hidden signs of inflammation or infection, which helps determine what surgical approach will be adopted and whether Mesh will be used or not[15]. As such, in this case, although the patient was asymptomatic and liver function was normal, enhanced abdominal CT scan was performed to evaluate whether there was acute pancreatitis or the hepatic vein was compressed.
The type of herniated parenchymal organs is important for the choice of treatment strategy. When the spleen or pancreas protrudes through the hernia ring, patients often need to receive surgical treatment (elective or emergency operation) because of the serious complications caused by this pathological condition[8,9]. However, hepatic herniation alone rarely causes serious clinical manifestations, conservative treatment might be the first choice. Surgical treatment must be comprehensively evaluated only when conservative treatment is ineffective, and the benefits from the operation outweigh the risks[6]. In clinical practice, surgeons should make a comprehensive assessment based on their own experience and the individual characteristics of the hernia, such as the location, size and different organs of the herniation. In the present case, intraperitoneal Onlay Mesh repair of the open ventral hernia was performed using biological Mesh. Considering that the patient was a 21-year-old young woman, we chose an absorbable biological Mesh to avoid the possible pain and influence on body growth that might be caused by the non-retractable Mesh.
The development of giant ventral hernia has a negative impact on the physiology of patients, such as pain, and inability to carry out daily activities. The skin of abdominal wall in many patients with ventral hernia has not been repaired satisfactorily although the ventral hernia was successfully repaired, consequently declining the patient's sense of self-worth[16]. More importantly, significantly increased negative psychological effects, such as disturbances to the mood, sleep, relationships with others and pleasure of life, lead to a poor quality of life[3]. In our case, the young woman suffered from a giant ventral hernia for nearly 15 years. Many serpentine scars on her abdominal wall made her almost autistic. In addition, she was advised not to take exercise like other students because of the potential risk of liver and spleen rupture during school time. These unusual pressures caused the patient to be self-abased. During the treatment, multiple serpentine scars on the abdominal wall were removed simultaneously, and psychological comfort and encouragement were provided. At the time of discharge, the patient had almost got rid of the psychological shadow.
We report an extremely rare case of giant ventral hernia simultaneously containing the spleen, part of the pancreas and liver, which has been successfully treated. We highlight that surgeons should avoid abdominal hernia when performing abdominal surgery in obese, elderly and diabetic patients. In addition, we recommend that surgeons should pay more attention to the psychological treatment while restoring the abdominal physiological function in ventral hernia patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Balaban DV, Milone M S-Editor: Zhang L L-Editor: MedE-Ma JY E-Editor: Qi LL
| 1. | Diener MK, Voss S, Jensen K, Büchler MW, Seiler CM. Elective midline laparotomy closure: the INLINE systematic review and meta-analysis. Ann Surg. 2010;251:843-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 226] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 2. | Argudo N, Pereira JA, Sancho JJ, Membrilla E, Pons MJ, Grande L. Prophylactic synthetic mesh can be safely used to close emergency laparotomies, even in peritonitis. Surgery. 2014;156:1238-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Chung L, O'Dwyer PJ. Pain and its effects on physical activity and quality of life before operation in patients undergoing elective inguinal and ventral hernia repair. Am J Surg. 2014;208:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Clay L, Stark B, Gunnarsson U, Strigård K. Full-thickness skin graft vs. synthetic mesh in the repair of giant incisional hernia: a randomized controlled multicenter study. Hernia. 2018;22:325-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Halligan S, Parker SG, Plumb AA, Windsor ACJ. Imaging complex ventral hernias, their surgical repair, and their complications. Eur Radiol. 2018;28:3560-3569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Neelamraju Lakshmi H, Saini D, Om P, Bagree R. A ventral incisional hernia with herniation of the left hepatic lobe and review of the literature. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Fernando EJ, Guerron AD, Rosen MJ. A case of splenic rupture within an umbilical hernia with loss of domain. J Gastrointest Surg. 2015;19:789-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Komaei I, La Malfa G, Damiano C, Sarra F, Cassaro G, Barbera A, Bartolotta M, Currò G, Navarra G. Voluminous paraumbilical hernia containing the pancreas - An unusual cause of acute pancreatitis: A case report. Ann Med Surg (Lond). 2019;45:6-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Alam N, Zeidan S, Lamparelli M. A rare case of umbilical hernia containing the pancreas. J Surg Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Sheer TA, Runyon BA. Recurrent massive steatosis with liver herniation following transplantation. Liver Transpl. 2004;10:1324-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Eken H, Isik A, Buyukakincak S, Yilmaz I, Firat D, Cimen O. Incarceration of the hepatic lobe in incisional hernia: A case report. Ann Med Surg (Lond). 2015;4:208-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Nuño-Guzmán CM, Arróniz-Jáuregui J, Espejo I, Valle-González J, Butus H, Molina-Romo A, Orranti-Ortega RI. Left hepatic lobe herniation through an incisional anterior abdominal wall hernia and right adrenal myelolipoma: a case report and review of the literature. J Med Case Rep. 2012;6:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Saujani S, Rahman S, Fox B. Budd-Chiari syndrome due to right hepatic lobe herniation: CT image findings of two rare clinical conditions. BJR Case Rep. 2017;3:20160133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Then EO, John F, Ofosu A, Gaduputi V. Anterior Hepatic Herniation: An Unusual Presentation of Abdominal Incisional Hernia. Cureus. 2019;11:e4066. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Earle D, Roth JS, Saber A, Haggerty S, Bradley JF, Fanelli R, Price R, Richardson WS, Stefanidis D; SAGES Guidelines Committee. SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc. 2016;30:3163-3183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 16. | van Ramshorst GH, Eker HH, Hop WC, Jeekel J, Lange JF. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg. 2012;204:144-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 282] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 17. | Shanbhogue A, Fasih N. Education and imaging. Hepatobiliary and pancreatic: herniation of the liver. J Gastroenterol Hepatol. 2009;24:170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Warbrick-Smith J, Chana P, Hewes J. Herniation of the liver via an incisional abdominal wall defect. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Kanakaratne SD, Asokan G, Liyanage C. Unusual case of ventral liver herniation. ANZ J Surg. 2017;87:950-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |