Published online May 6, 2020. doi: 10.12998/wjcc.v8.i9.1698
Peer-review started: January 26, 2020
First decision: March 15, 2020
Revised: April 9, 2020
Accepted: April 17, 2020
Article in press: April 17, 2020
Published online: May 6, 2020
Processing time: 94 Days and 20.3 Hours
Esophageal liposarcoma is a rare malignant tumor and an esophageal dedifferentiated liposarcoma (DDL) is extremely rare. There are no reports on the treatment of DDL by thoracoscopic surgery.
A 38-year-old woman presented with dysphagia and dyspnea. Imaging examination showed a large mass in the posterior mediastinum. The patient also developed respiratory failure and it was unclear whether this was caused by a mass from inside or outside the esophagus. We decided to perform thoracoscopic exploration to relieve the obstruction caused by tracheal compression. The upper segment of the esophagus was split longitudinally, and most of the mass could be removed from the esophageal lumen to the thoracic cavity. The pedicle was excised by linear cutting closers under mirrors. Little residual mass was visualized by gastroscopy. The mucous and muscular layers were closed by interrupted sutures. Pathological examination showed that the mass was a DDL. The patient did not have any dysphagia or dyspnea 2 wk postoperatively and refused any further treatment. Computed tomography and esophagoscopy did not find any recurrence at up to 20 mo postoperatively.
Thoracoscopy can be used to treat large esophageal masses.
Core tip: An esophageal dedifferentiated liposarcoma (DDL) is extremely rare. Surgery is the best choice of treatment, including aggressive open transcervical, transthoracic, and transabdominal total or subtotal esophagectomy. DDL is a low-malignancy tumor, and minimally invasive treatment can improve postoperative quality of life. There are no reports of thoracoscopic surgery for the treatment of DDL. Here, we present a case of minimally invasive treatment of a large esophageal DDL by thoracoscopy. There was no sign of recurrence and the patient achieved a high quality of life.
- Citation: Ye YW, Liao MY, Mou ZM, Shi XX, Xie YC. Thoracoscopic resection of a huge esophageal dedifferentiated liposarcoma: A case report. World J Clin Cases 2020; 8(9): 1698-1704
- URL: https://www.wjgnet.com/2307-8960/full/v8/i9/1698.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i9.1698
Esophageal liposarcoma is a rare malignant tumor, with a reported incidence of 0.1%-1.5% of all esophageal neoplasms. Most cases are well-differentiated liposarcoma[1]. Dedifferentiated liposarcoma (DDL) has a lower incidence in patients with esophageal liposarcoma. We present a patient with a large esophageal liposarcoma treated by thoracoscopic resection.
A 38-year-old woman with dysphagia for 6 mo and dyspnea for 1 wk.
The patient had no previous medical history.
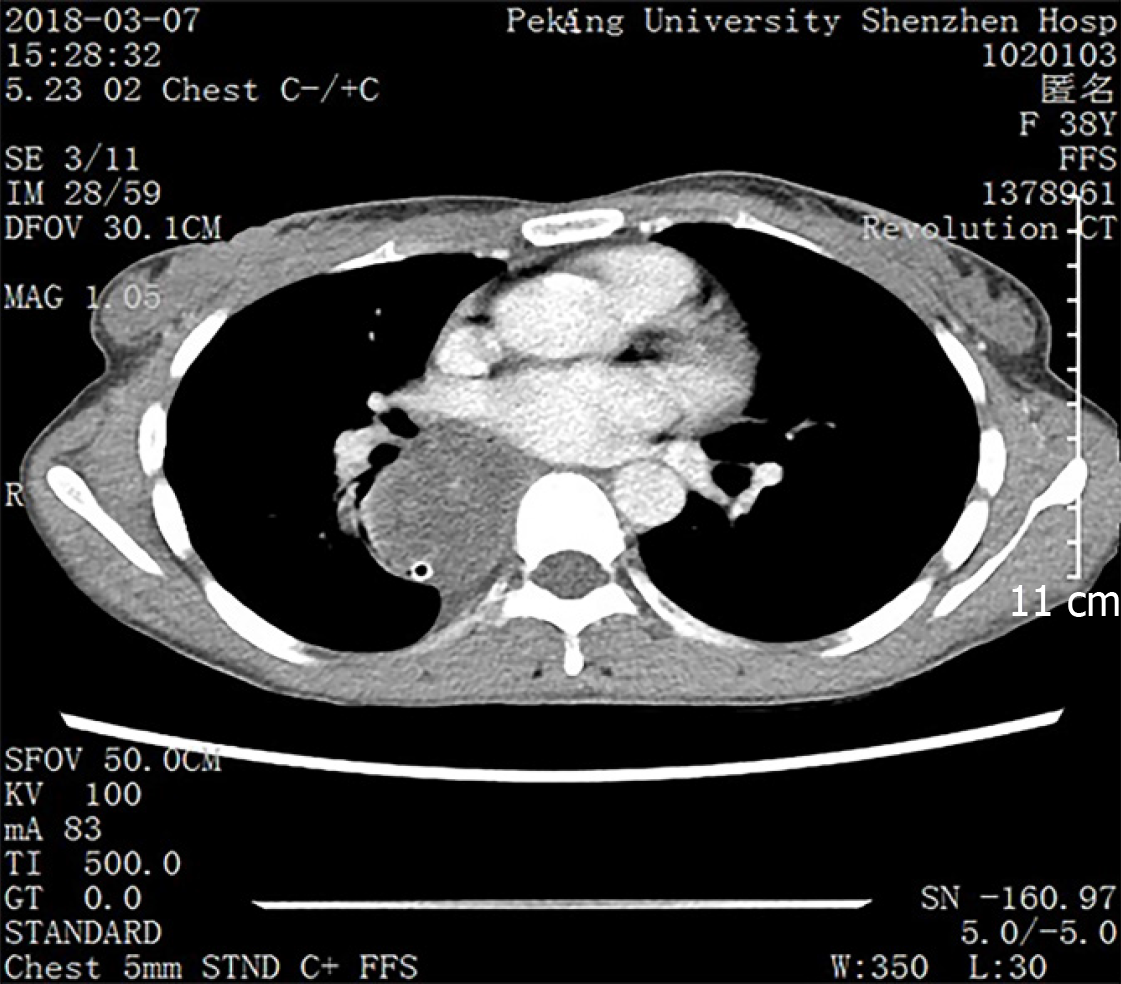
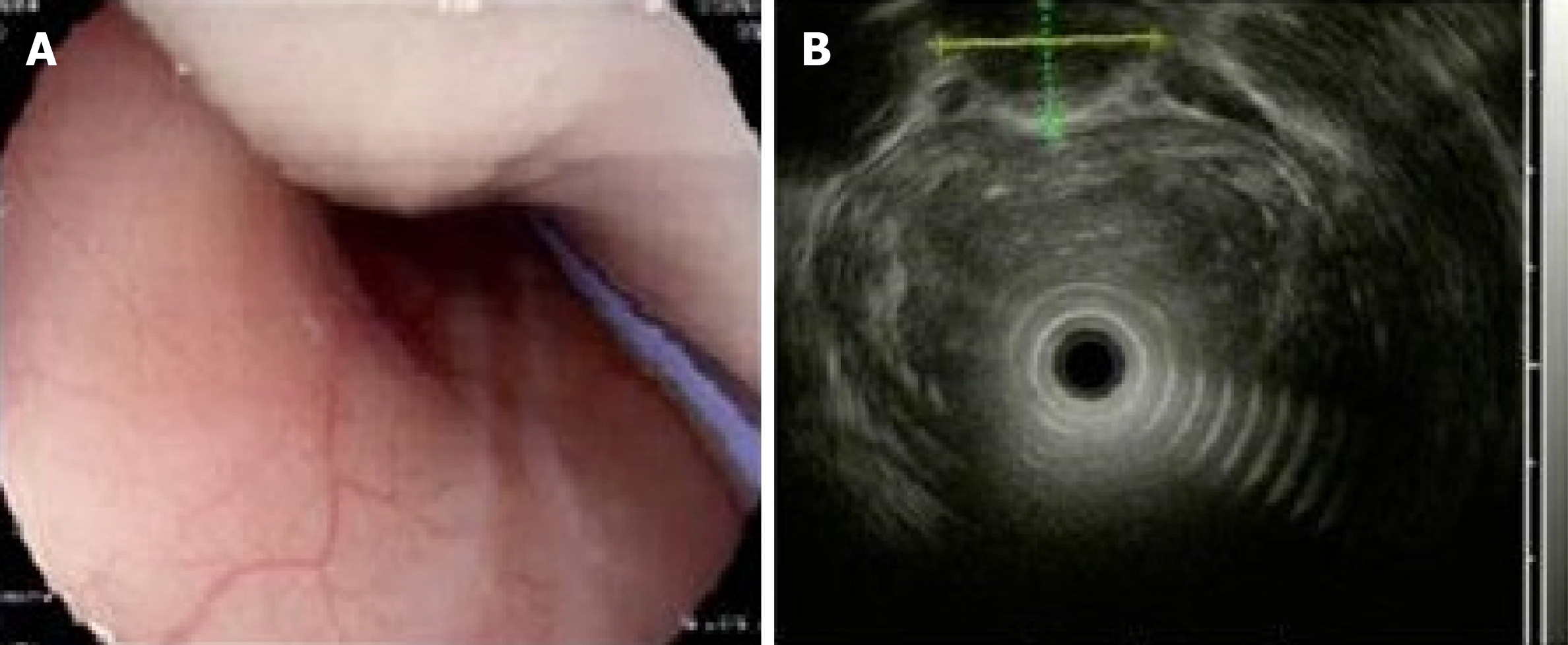
Computed tomography (CT) showed a large mass in the posterior mediastinum, which may have been caused by a large cyst or effusion inside the esophagus. The trachea and left and right main bronchi were subjected to external pressure stenosis (Figure 1). Esophagogastroscopy revealed a large mass pushing against the esophagus. Esophagogastric ultrasonography showed a homogeneous, low echogenic mass outside the esophagus, which ranged from 20 to 40 cm below the incisor, and had a cross-sectional area of 21.5 mm × 15.9 mm (Figure 2). Upper gastrointestinal angiography also showed external pressure stenosis of the esophagus (Figure 3).
The patient’s dyspnea became more serious due to the obstruction caused by tracheal compression. She developed respiratory failure and it was unclear whether this was caused by a mass inside or outside the esophagus. Exploratory thoracoscopy was performed to relieve the tracheal compression obstruction.
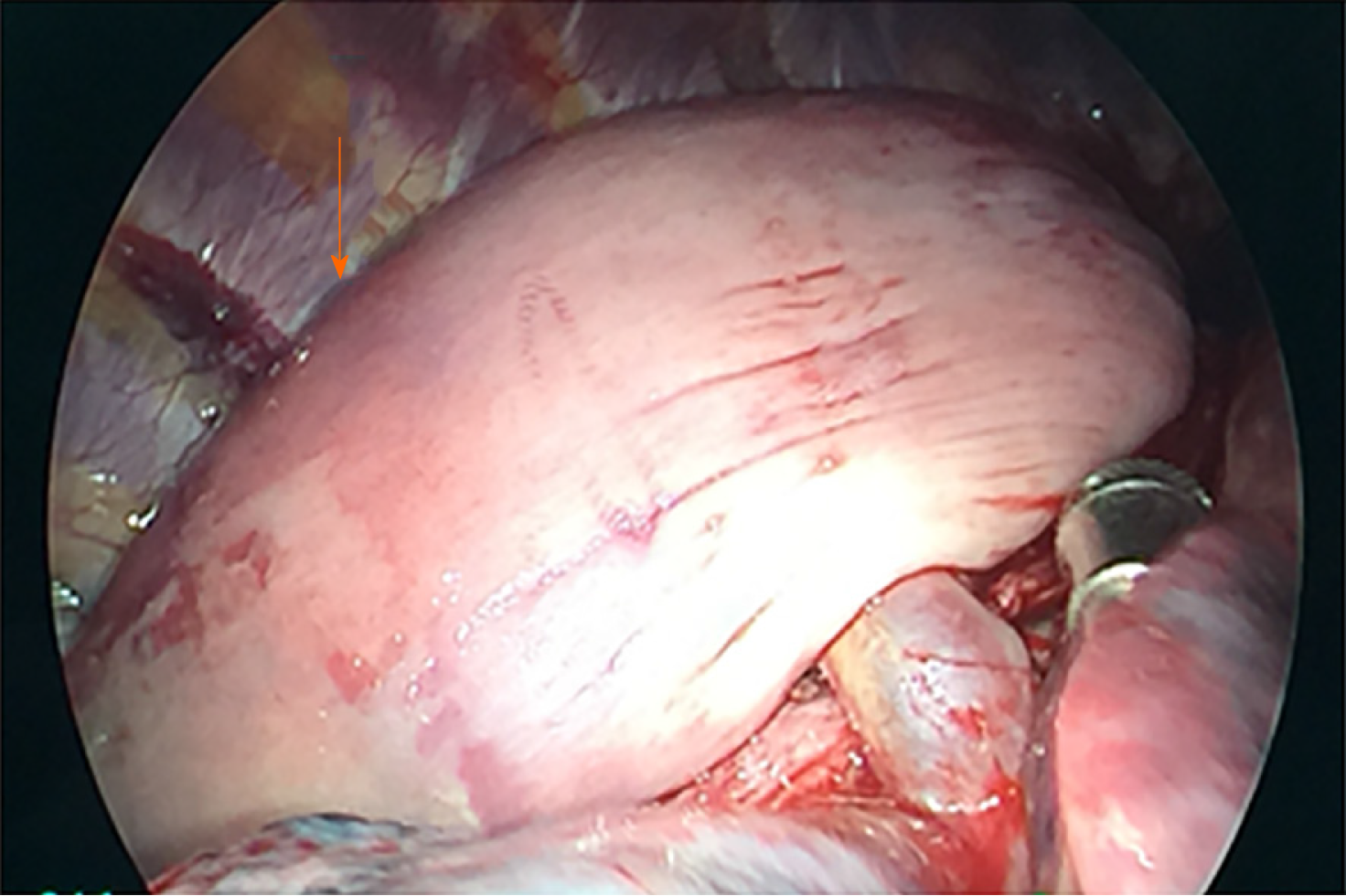
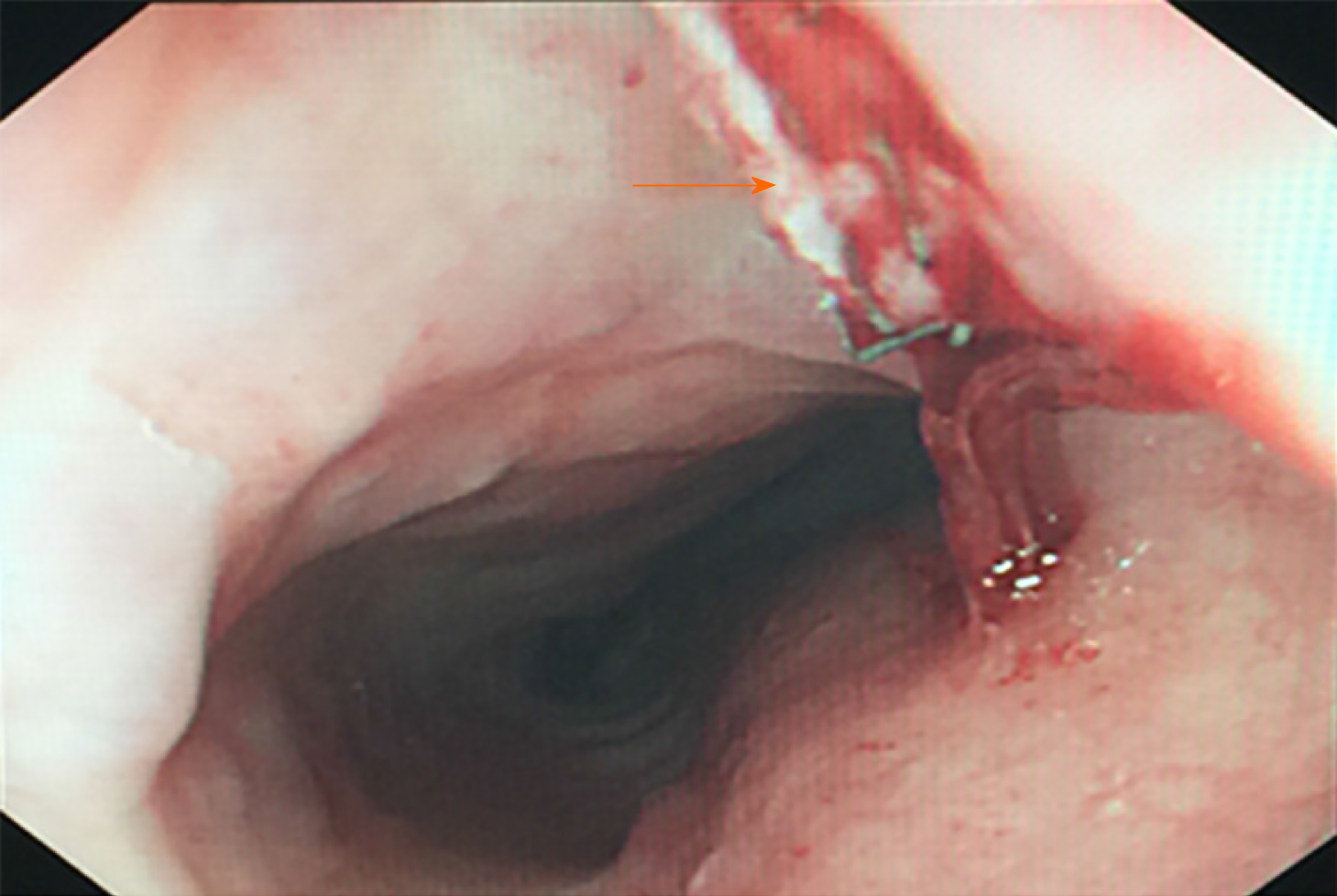
A large, smooth-surface mass occupying the posterior mediastinum was observed (Figure 4). The upper segment of the esophagus was split longitudinally, and most of the mass was extracted from the esophageal lumen to the thoracic cavity. The pedicle was excised by linear cutting closers under mirrors. Little residual mass was noted by gastroscopy (Figure 5). We considered this to be a benign tumor of the esophagus and the pedicle of the tumor was near the throat; thus, it was difficult to confirm complete resection by biopsy under endoscopy. In addition, the patient developed severe respiratory insufficiency during surgery. Due to the above reasons we were unable to confirm complete resection by biopsy pathology. The mucous and muscular layers were interruptedly sutured.
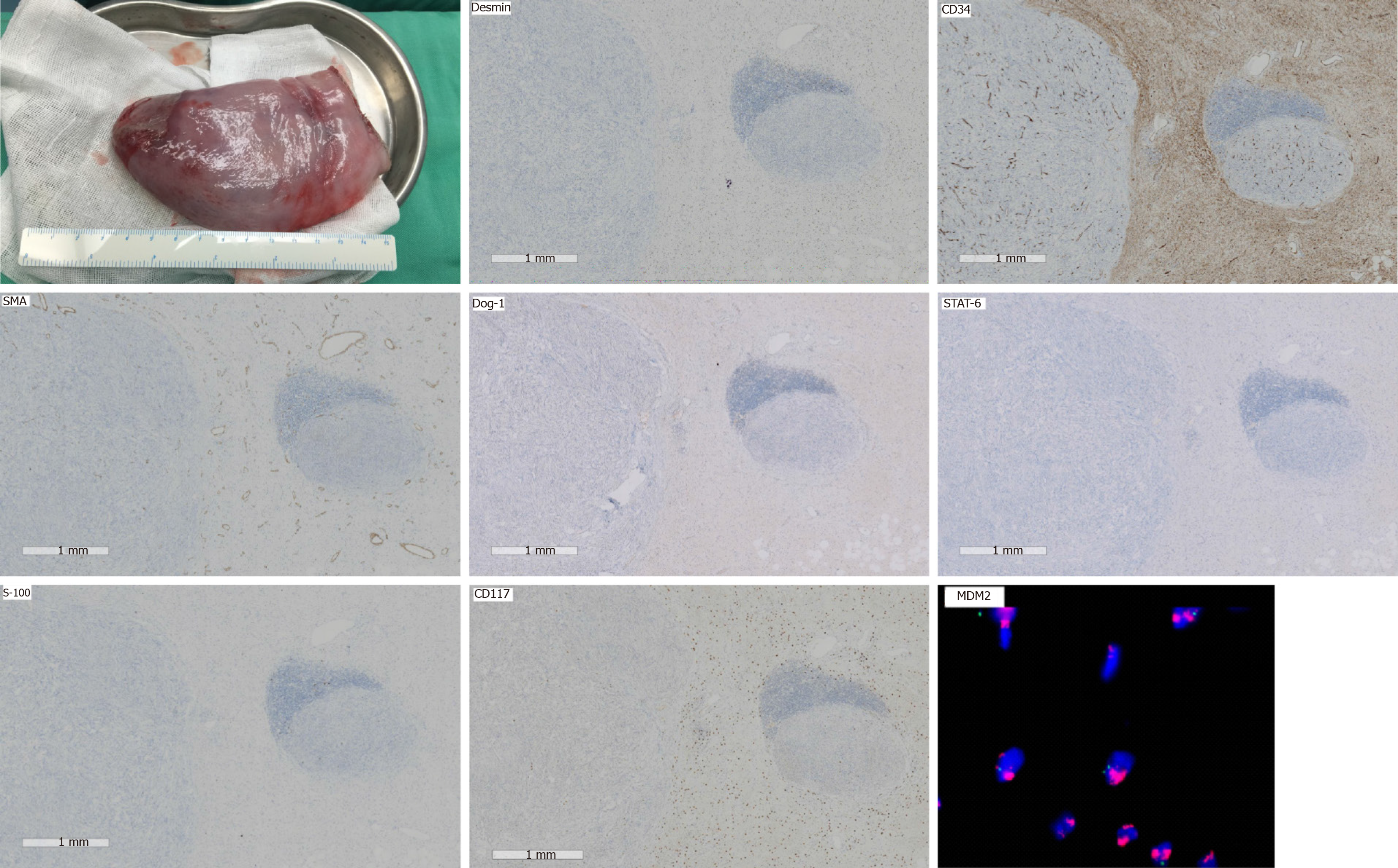
Pathological examination showed some discrete spindle cells, and a little adipose tissue (less than 5%). Immunohistochemical analysis revealed that some discrete spindle cells were positive for Desmin and CD34, and negative for S-100, SMA, DOG-1 and STAT-6. Fatty tissue was positive for S-100 protein. CD117 highlighted the intermixed mast cells and plasma cells. MDM2 gene amplification was confirmed by fluorescence in situ hybridization analysis (Figure 6).
The pathologist suspected that the mass was a DDL of the esophagus. Cleveland Medical Center Pathology Consultation considered the mass to be DDL.
We recommended that the patient undergo extended resection of the tumor pedicle with cervical incision or adjuvant treatment.
The patient did not have any dysphagia or dyspnea 2 wk postoperatively and refused any further treatment, but underwent CT and esophagoscopy every three months. The patient‘s last CT and esophagoscopy did not find any sign of recurrence at 20 mo post-operation (Figure 7).
A liposarcoma originates in the mesenchymal layer, and is one of the most common sarcomas in adults, but is rarely found in the esophagus[2]. Liposarcomas can be divided into four subtypes: Well-differentiated liposarcoma, pleomorphic liposarcoma, myxoid/round cell liposarcoma, and DDL; the latter is a rare type with a prevalence of approximately 6% of all liposarcomas[1,2,3,4]. We found only 60 reported cases of esophageal liposarcomas and just one case of esophageal DDL. Here, we present a case with minimally invasive treatment of a large esophageal DDL by thoracoscopy.
An esophageal liposarcoma grows slowly and presents with symptoms caused by compression or invasion of intrathoracic structures, most commonly dyspnea, weight loss, throat discomfort and dysphagia. Esophagoscopy reveals a submucosal lesion or extrinsic compression encompassing the esophageal lumen. CT shows a soft tissue lesion in the posterior mediastinum[1,5]. Differential diagnosis of the disease from benign esophageal tumors, such as a fibrovascular polyp, is often difficult by imaging or endoscopy[6]. We were unable to make a definitive diagnosis by frozen section analysis during the operation. In the present case, we diagnosed a large mass in the esophagus before surgery, and frozen section diagnosis was a spindle cell tumor. Esophagoscopic biopsy to distinguish liposarcoma from polyps before surgery is necessary. However, in this case we did not perform preoperative biopsy as the patient underwent emergency, life-saving surgery for obstructive respiratory dysfunction.
Surgery is the best choice of treatment for DDL[7], including aggressive open transcervical, transthoracic, and transabdominal total or subtotal esophagectomy[4,8-10].
There are four case reports of the treatment of esophageal liposarcoma with endoscopic submucosal dissection[4,7,11,12]. However, it is not possible to resect large esophageal tumors with endoscopic submucosal dissection. Other approaches have been attempted, but no thoracoscopic approaches have been reported. In the present case, our surgical approach was thoracoscopic esophagotomy and the patient did not have any postoperative discomfort.
It is not possible to give an authoritative assessment regarding the prognosis of esophageal liposarcoma after surgery as the number of cases published with long-term follow-up is insufficient for rigorous analysis. Riva et al[13] reported local recurrence in 13% of patients with esophageal liposarcoma and the average time between first treatment and recurrence was 127.67 mo[13]. Our patient is in good condition and did not have any recurrence 20 mo after surgery.
In our patient, non-curative resection of the esophageal DDL may have been performed, as we intended taking a margin biopsy by endoscopy for frozen pathology to confirm complete resection, but the tumor pedicle was near the throat, and it was difficult to confirm complete resection by biopsy under endoscopy. In addition, the patient developed severe respiratory insufficiency during surgery. Thus, we were unable to confirm complete resection by biopsy pathology during surgery.
We could not completely resect the possible residual tumor under endoscopy as the tumor pedicle was near the throat. It is unclear whether the patient should have undergone extended resection of the tumor pedicle by cervical incision as she has a high quality of life to date and we would not be able to guarantee no recurrence of the tumor even with extended resection. Therefore, we respect the choice of the patient and she is being followed up closely.
Esophageal DDL is an extremely rare tumor. We present a patient who underwent thoracoscopic resection of a large esophageal liposarcoma who had severe compressive obstructive respiratory insufficiency. Thoracoscopy can be used to treat large esophageal masses.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Fleres F, Garg PK, Wiemer EAC S-Editor: Zhang L L-Editor: Webster JR E-Editor: Xing YX
| 1. | Coindre JM, Pédeutour F, Aurias A. Well-differentiated and dedifferentiated liposarcomas. Virchows Arch. 2010;456:167-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 180] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 2. | Czekajska-Chehab E, Tomaszewska M, Drop A, Dabrowski A, Skomra D, Orłowski T, Kołodziej I, Korobowicz E. Liposarcoma of the esophagus: case report and literature review. Med Sci Monit. 2009;15:CS123-CS127. [PubMed] |
| 3. | Lokesh V, Naveen T, Pawar YS. Spindle cell sarcoma of esophagus: a rare case presentation. J Cancer Res Ther. 2010;6:100-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Takiguchi G, Nakamura T, Otowa Y, Tomono A, Kanaji S, Oshikiri T, Suzuki S, Ishida T, Kakeji Y. Successful resection of giant esophageal liposarcoma by endoscopic submucosal dissection combined with surgical retrieval: a case report and literature review. Surg Case Rep. 2016;2:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Chung JJ, Kim MJ, Kim JH, Lee JT, Yoo HS, Kim KW. Imaging findings of giant liposarcoma of the esophagus. Yonsei Med J. 2003;44:715-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | McCarthy AJ, Carroll P, Vajpeyi R, Darling G, Chetty R. Well-Differentiated Liposarcoma (Atypical Lipomatous Tumor) Presenting as an Esophageal Polyp. J Gastrointest Cancer. 2019;50:589-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Dowli A, Mattar A, Mashimo H, Huang Q, Cohen D, Fisichella PM, Lebenthal A. A pedunculated giant esophageal liposarcoma: a case report and literature review. J Gastrointest Surg. 2014;18:2208-2213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 8. | Xu S, Xu Z, Hou Y, Tan Y. Primary pedunculated giant esophageal liposarcoma: case report. Dysphagia. 2008;23:327-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Will U, Lorenz P, Urban H, Meyer F. Curative endoscopic resection of a huge pedunculated esophageal liposarcoma. Endoscopy. 2007;39 Suppl 1:E15-E16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Weaver HL, Preston SD, Wong HH, Jani P, Coonar AS. Surgical resection of a massive primary mediastinal liposarcoma with cervical extension. Ann R Coll Surg Engl. 2018;100:e22-e27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Cai MY, Xu JX, Zhou PH. Endoscopic submucosal dissection of a huge esophageal atypical lipomatous tumor (well-differentiated liposarcoma) with a 4-year recurrence-free survival. Endoscopy. 2017;49:E237-E239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Yo I, Chung JW, Jeong MH, Lee JJ, An J, Kwon KA, Rim MY, Hahm KB. Huge liposarcoma of esophagus resected by endoscopic submucosal dissection: case report with video. Clin Endosc. 2013;46:297-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Riva G, Sensini M, Corvino A, Garzaro M, Pecorari G. Liposarcoma of Hypopharynx and Esophagus: a Unique Entity? J Gastrointest Cancer. 2016;47:135-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |