Published online May 6, 2020. doi: 10.12998/wjcc.v8.i9.1666
Peer-review started: February 13, 2020
First decision: February 16, 2020
Revised: April 4, 2020
Accepted: April 21, 2020
Article in press: April 21, 2020
Published online: May 6, 2020
Processing time: 77 Days and 11.1 Hours
Granulocyte colony-stimulating factor (G-CSF) is a cytokine produced in inflammatory environments that induces differentiation and proliferation of neutrophils in bone marrow. We report a rare case of aggressive G-CSF-producing squamous cell carcinoma of the tongue exhibiting fluorine-18 deoxyglucose (FDG) accumulation in primary lesion, metastatic lymph nodes, spleen, and bone marrow on positron emission tomography–computed tomography (PET/CT).
We report a 58-year-old female with a rapid enlarged lingual mass with partial necrosis. Blood test results from the initial examination revealed a leukocyte count of 21380/µL. On PET/CT, extensive FDG accumulation was observed in the tongue and bilateral cervical lymph nodes, with elevated FDG accumulation in the spleen and bone marrow although no distant metastases were observed. We performed partial glossectomy and bilateral neck dissection. Immunohistochemical staining with G-CSF antibodies on biopsy specimen and resected samples revealed that both specimens were G-CSF positive. This is a rare case of G-CSF producing tongue carcinoma with elevated FDG accumulation in the spleen and bone marrow.
In patients with the tongue cancer and hyperleukocytosis, where FDG accumulations in the spleen and bone marrow are observed using PET/CT and when these accumulations are not caused by metastasis, G-CSF-producing tumors, with associated poor prognosis, should be considered.
Core tip: Tongue cancer is the most common cancer of the head and neck. But progress usually is not rapid. In addition, there is no accompanying hyperleukocytosis and no fluorine-18 deoxyglucose (FDG) accumulation in the spleen and bone marrow. Here we report a rare granulocyte colony-stimulating factor (G-CSF)-producing tongue carcinoma with rapid progression, with hyperleukocytosis, and FDG accumulation in the spleen and bone marrow on positron emission tomography–computed tomography. From this case, G-CSF-producing tumors should be suspected in tongue cancer when hyperleukocytosis and FDG accumulation in the spleen or bone marrow on positron emission tomography–computed tomography because G-CSF producing tumor progress rapidly and have a poor prognosis.
- Citation: Shimamoto H, Hirota Y, Kashima Y, Kinoshita N, Yokokawa M, Ikeda T, Harada H. Granulocyte colony-stimulating factor-producing squamous cell carcinoma of the tongue exhibiting characteristic fluorine-18 deoxyglucose accumulation on positron emission tomography–computed tomography: A case report. World J Clin Cases 2020; 8(9): 1666-1673
- URL: https://www.wjgnet.com/2307-8960/full/v8/i9/1666.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i9.1666
Sudden hyperleukocytosis has a range of underlying etiologies, including inflammatory diseases, acute leukemia, chronic myelocytic leukemia (CML), granulocyte colony-stimulating factor (G-CSF)-producing tumors, non-CML myeloproliferative diseases, bone marrow metastases of malignant tumors and administration of G-CSF agents. G-CSF is a cytokine produced in inflammatory environments, primarily by macrophages, fibroblasts, endothelial cells, but also to a lesser extent by other cells. In addition, it induces differentiation and proliferation of neutrophils in the bone marrow. Fluorine-18 deoxyglucose (FDG) positron emission tomography–computed tomography (PET/CT) is recognized as a useful modality for tumor imaging. FDG accumulation correlates with bone marrow and peripheral neutrophil counts. Here we report a rare case of G-CSF-producing squamous cell carcinoma of the tongue that grew rapidly and through PET/CT exhibited FDG accumulation not only in the primary lesion and metastatic lymph nodes but also in the spleen and bone marrow throughout the body.
A 58-year-old woman with an enlarged mass on the tongue was examined in our department.
The patient noticed a growth of the mass 1 mo prior to the examination.
The patient had a history of hypertension and mitral regurgitation.
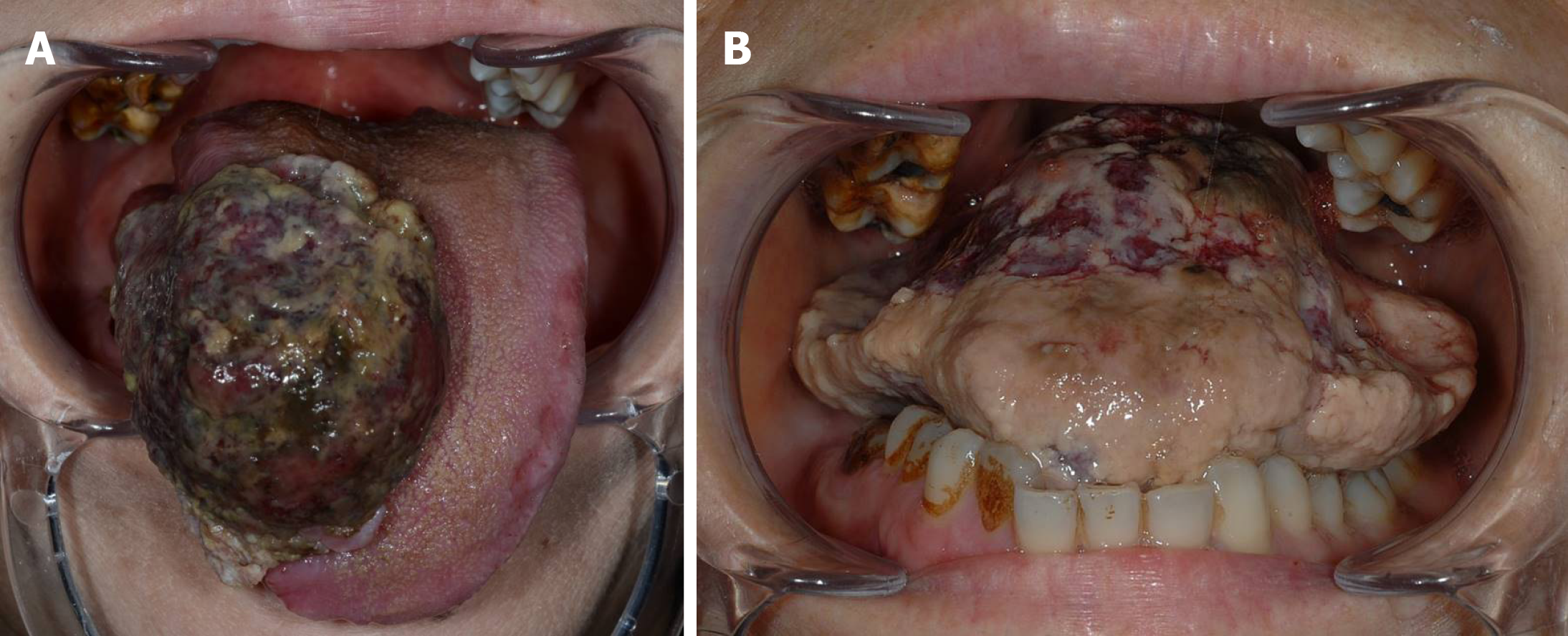
A 30 mm × 40 mm pedunculated tumor with partial necrosis was observed on the right side of the tongue (Figure 1A). The mass was growing rapidly. On admission to the hospital, the tumor continued to rapidly grow outward, filling the oral cavity to the extent that the patient was unable to close her mouth (Figure 1B).
Blood test results from the initial examination revealed a leukocyte count of 21380/µL, neutrophil of 84%, and C-reactive protein (CRP) of 0.99 mg/dL, all of which were considered high levels. Upon hospital admission, serum G-CSF level was measured at 331 pg/mL, interleukin (IL)-6 at 14.6 pg/mL and blood test revealed a leukocyte concentration of 24510/µL, neutrophils at 83%, and CRP at 0.99 mg/dL (Table 1).
| Frist visit | Administration | PO 1 d | PO 18 d | 1st ST | 2nd ST | 3rd ST | |
| Leukocytes (μL) | 21380 | 24510 | 15230 | 14250 | 77620 | 59720 | 145180 |
| Neutrophil (%) | 84 | 83 | 90 | 86 | 98 | 96 | 98 |
| CRP (mg/dL) | 0.99 | 5.10 | 9.68 | 1.14 | 5.66 | 8.70 | 13.20 |
| G-CSF (pg/mL) | 331 | 63.3 | 71.6 | 663 | 218 | 1520 | |
| IL-6 (pg/mL) | 14.6 | 63.0 | 6.30 | 10.3 | 104 |
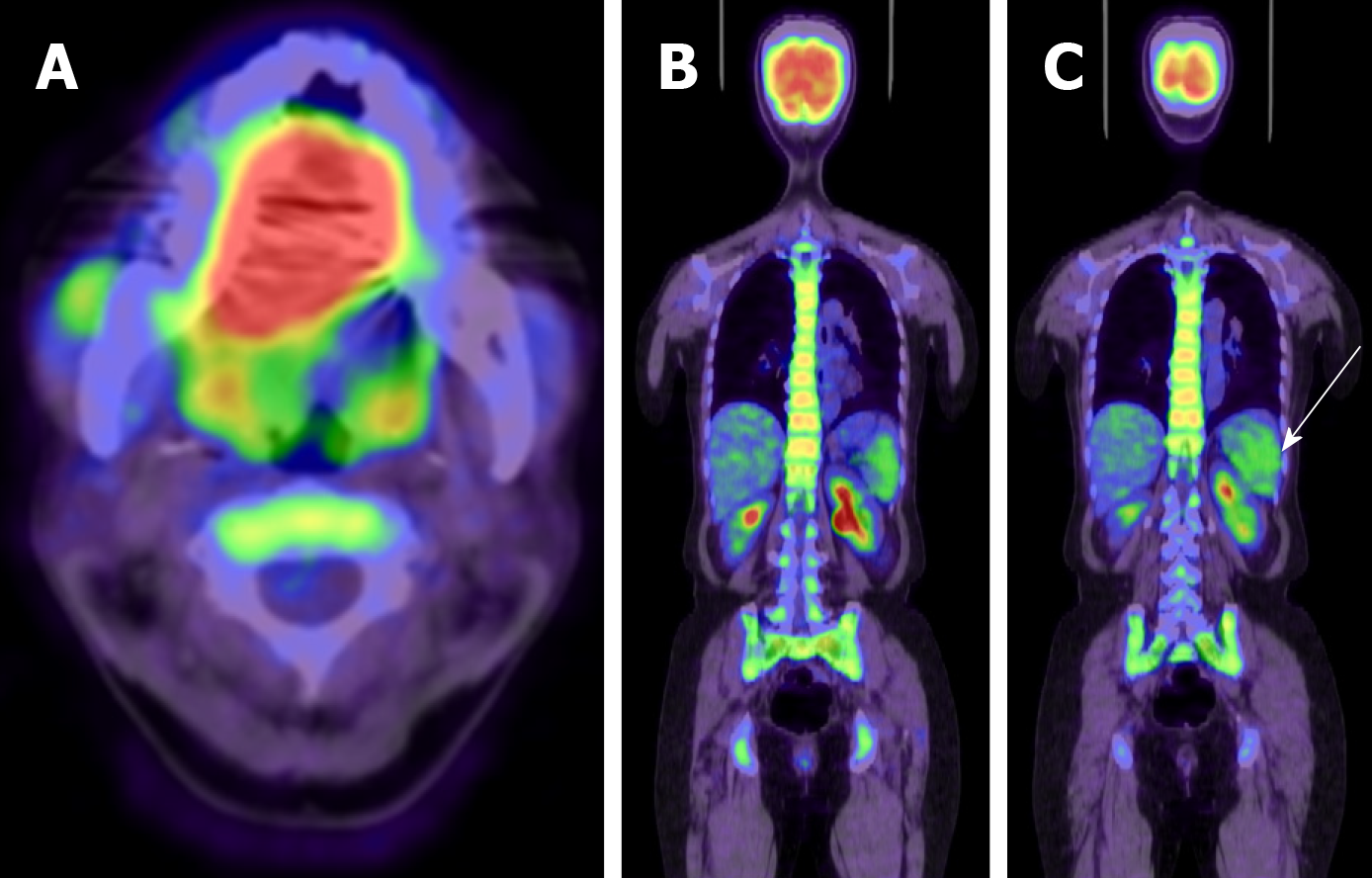
In PET/CT, extensive FDG accumulation was observed in the tongue (Figure 2A) and bilateral cervical lymph node, while elevated FDG accumulation was also observed in the spleen and bone marrow throughout the body (Figure 2B and C). No distant metastases were observed in PET/CT.
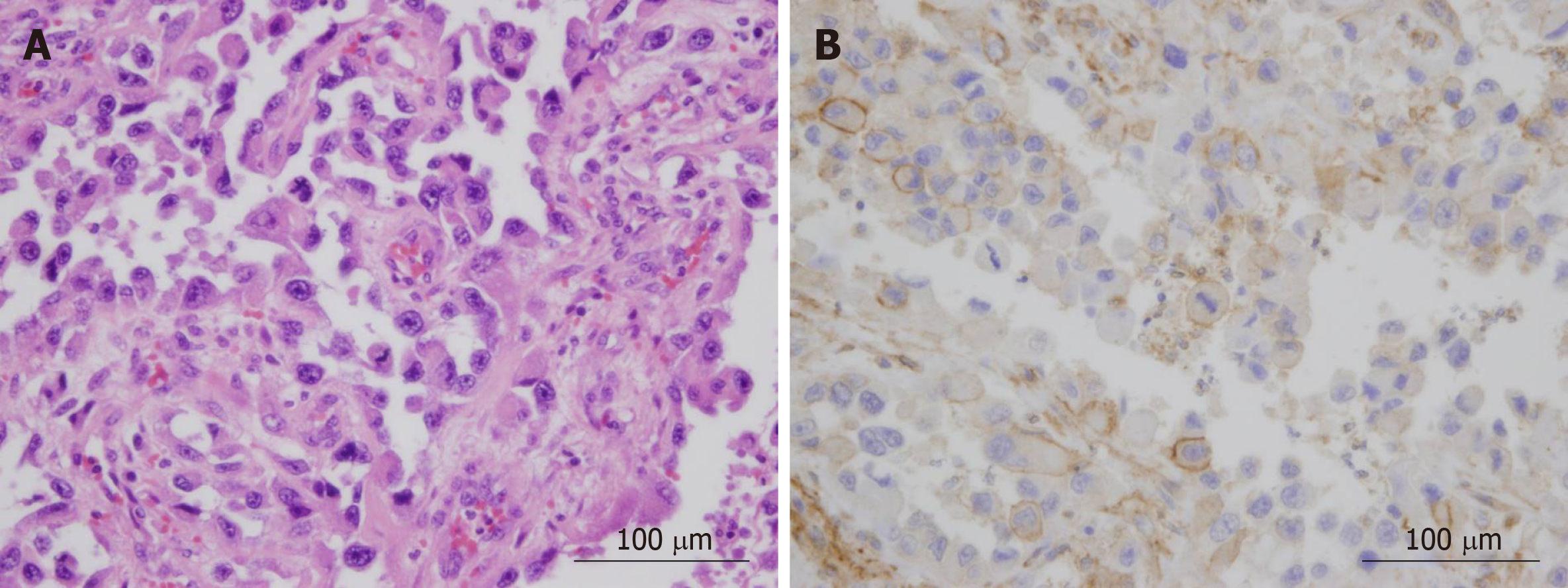
Upon histopathologic examination of tissue, large carcinoma cells with high proliferation potency were confirmed in the majority of the tumor. The majority of the tumor comprised of poorly differentiated squamous cancer cells. Immunohisto-chemical staining with G-CSF antibodies on biopsy tissue and specimens resected during surgery revealed both to be G-CSF positive (Figure 3).
G-CSF producing squamous cell carcinoma of the tongue.
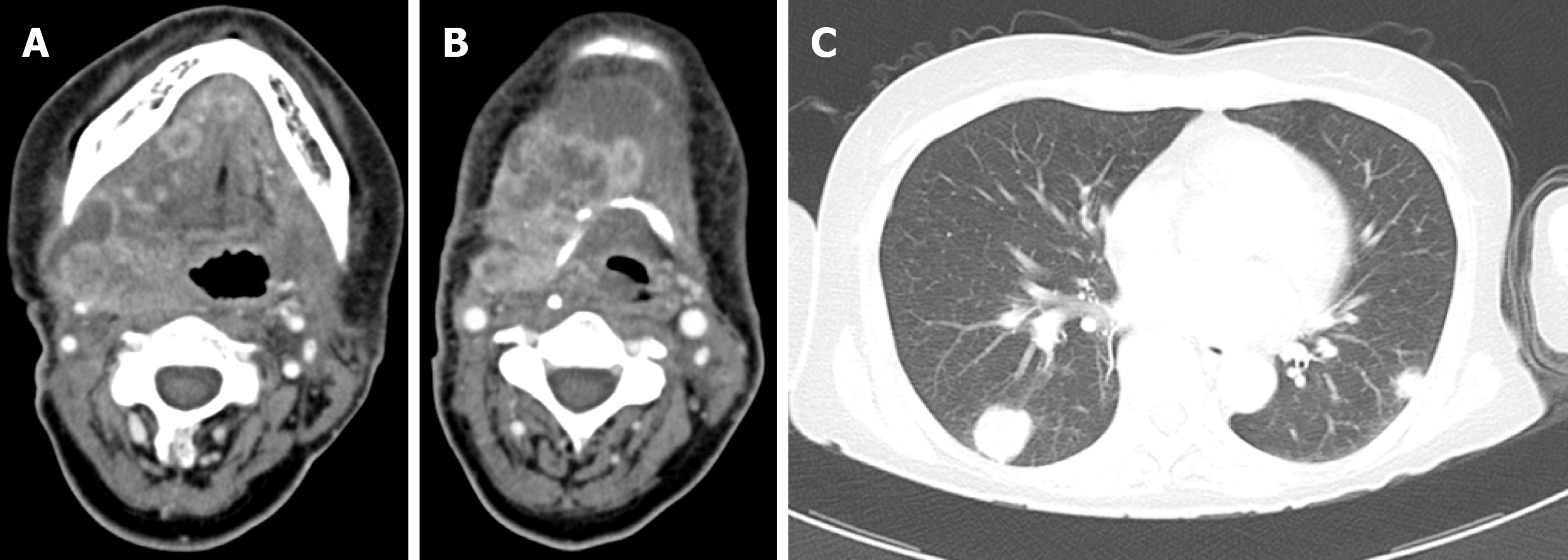
Right modified radical neck dissection type I, left supraomohyoid neck dissection, and partial glossectomy were performed. On postoperative day 1, the leukocyte count was 15230/μL, neutrophil level was 90%, CRP level was 9.68 mg/dL, and serum G-CSF level was 63.3 pg/mL, with decreases observed in leukocyte count and serum G-CSF levels compared with preoperative measurements. On postoperative day 18, CT revealed the presence of recurrence in the neck, accompanied by multiple metastases in the lungs (Figure 4). At this point, the patient exhibited leukocytes at a concentration of 77620/μL, 84% at neutrophil, CRP at 5.66 mg/dL, and serum G-CSF at 663 pg/mL. On postoperative day 23, the patient was commenced on cetuximab (first dose of 400 mg/m2 followed by 250 mg/m2) and cisplatin (80 mg/m2). Following primary systemic therapy, blood levels temporarily decreased to a leukocyte concentration of 58820/μL, CRP at 2.89 mg/dL, and serum G-CSF at 268 pg/mL. Disease progress was unable to be halted; however, blood levels eventually rose to a leukocyte concentration of 145180/μL, CRP at 13.2 mg/dL, IL-6 at 104 pg/mL, and serum G-CSF at 1520 pg/mL (Table 1).
The patient died from primary disease on postoperative day 45.
Sudden hyperleukocytosis has a range of underlying etiologies, including inflammatory diseases, acute leukemia, CML, G-CSF-producing tumors, non-CML myeloproliferative diseases, bone marrow metastases of malignant tumors and administration of G-CSF agents.
G-CSF is a cytokine that promotes the proliferation and differentiation of granulocytes, and is produced by macrophages, monocytes, and fibroblasts. Although serum G-CSF level is elevated in infectious diseases and blood diseases, malignant tumors themselves rarely produce G-CSF and are called G-CSF-producing tumor which is one of paraneoplastic syndromes that are induced by malignant tumors producing various bioactive substances[1]. Hughes et al[2] reported the presence of malignant tumor that demonstrated leukocytosis in G-CSF-producing tumor. Later, Asano et al[3] were the first to report on G-CSF-producing lung cancer.
There are four criteria for the diagnosis of G-CSF-producing tumors: Increase in leukocyte count, elevation in G-CSF levels, decrease in leukocyte count and G-CSF levels following treatment, and production of G-CSF by tumor cells[3]. This final criteria (G-CSF production by tumor cells) can be assessed by observing G-CSF staining through immunohistochemical staining[4]; however, this is said to be difficult due to weak antigenicity and significantly small amount of G-CSF protein, which is stored in cells for a short time before being released[5]. In the case presented here, G-CSF was confirmed in both the biopsy tissue and resected specimen. Furthermore, the other criteria were satisfied, based on which G-CSF-producing squamous cell carcinoma was diagnosed.
In the present case, PET/CT revealed FDG accumulation in the primary lesion metastatic lymph nodes, spleen, and bone marrow throughout the body. The relationship between G-CSF and bone marrow FDG-PET findings has previously been reported[6]. In their study, chemotherapy patients receiving G-CSF agents exhibited significantly higher standardized uptake values compared with the control group. Furthermore, another study has shown a strong correlation between FDG accumulation in the bone marrow during PET imaging and leukocyte count in the peripheral blood, particularly neutrophils[7]. The authors stated that this result reflected increased bone marrow metabolism through the stimulation of granulocytes and other substances[7].
It is thought that G-CSF increases granulocytic hematopoiesis in the bone marrow, where elevated glucose metabolism results in FDG accumulation[6]; we consider that the diffuse FDG accumulation observed in the bone marrow in the present study was due to the same mechanism G-CSF administration induces extramedullary hematopoiesis, strengthening the hematopoietic capacity of the spleen, resulting in FDG accumulation. In the present case, G-CSF produced by the tumor is considered to have accumulated in both the bone marrow and spleen. It is important therefore not to misdiagnose diffuse FDG accumulation in the spleen and bone marrow as metastatic foci.
G-CSF increases leukocyte count but does not directly cause inflammatory responses. Some tumors produce inflammatory cytokines such as IL-6, IL-1, and tumor necrosis factor-a along with G-CSF, which causes fever and an inflammatory response[8,9]. In this case, it is considered that CRP increased due to the high level of IL-6. In addition, it may cause accompanying symptoms such as hypercalcemia, but these are also considered to be related to cytokines other than G-CSF.
Interestingly, reports of G-CSF-producing tumors of the oral cavity are rare[10], with the most common location for this type of cancer being the lung[11], followed by liver[12], stomach[13], and bladder[1]. There have been only 7 cases of G-CSF-producing oral cancer, including our case[10,14-18]. Of 7 cases, 4 cases were tongue cancer and 3 cases were lower gingival cancer. Histopathologically, 6 cases were squamous cell carcinoma and 1 case was mucoepidermoid carcinoma. Despite chemotherapy, chemoradiotherapy and/or surgery was performed in each cases, all patients died of the disease within 12 mo (Table 2). G-CSF temporarily decreased after cetuximab administration, but did not stop progression of the disease in our case, although our case was the first cases administered cetuximab. Standard treatment for G-CSF-producing tumors has not been established, and it is considered to be necessary to accumulate and assess further case.
| No. | Ref. | Sex | Age | Primary site | TN classi-fication | Histological type | Deffrentia-tion | Treatment | Outcome | Survival time (mo) |
| 1 | Current research | F | 58 | Tongue | T3N2c | SCC | Poor | S+Sys. | DOD | 1.5 |
| 2 | Horii et al[14] | M | 61 | Tongue | T4N0 | SCC | Poor | S | DOD | 11 |
| 3 | Kaneko et al[15] | M | 57 | Tongue | T4aN0 | SCC | Moderate | CR+S | DOD | 9 |
| 4 | Kuroshima et al[10] | M | 78 | Tongue | T3N3 | SCC | C | DOD | 12 | |
| 5 | Ishigami et al[16] | F | 84 | Lower gingiva | T2N0 | SCC | Poor | R | DOD | 2.5 |
| 6 | Kodama et al[17] | F | 71 | Lower gingiva | T2N1 | MEC | S+CR+C | DOD | 1 | |
| 7 | Kobayashi et al[18] | F | 56 | Lower gingiva | T2N0 | SCC | Well | CR+S | DOD | 12 |
G-CSF-producing tumors progress quickly and are associated with extremely poor prognoses, as was observed in the present case. Poor prognosis is based on the fact that many G-CSF-producing tumors are undifferentiated or poorly differentiated, G-CSF increased the invasive and metastatic capacity of tumors, and G-CSF-producing tumors themselves possess an autocrine pathway, although many details remain unclear[19-21].
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hu B, Vynios D S-Editor: Ma YJ L-Editor: A E-Editor: Qi LL
| 1. | Kumar AK, Satyan MT, Holzbeierlein J, Mirza M, Van Veldhuizen P. Leukemoid reaction and autocrine growth of bladder cancer induced by paraneoplastic production of granulocyte colony-stimulating factor--a potential neoplastic marker: a case report and review of the literature. J Med Case Rep. 2014;8:147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Hughes WF, Higley CS. Marked leukocytosis resulting from carcinomatosis. Ann Intern Med. 1952;37:1085-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Asano S, Urabe A, Okabe T, Sato N, Kondo Y. Demonstration of granulopoietic factor(s) in the plasma of nude mice transplanted with a human lung cancer and in the tumor tissue. Blood. 1977;49:845-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Shimamura K, Fujimoto J, Hata J, Akatsuka A, Ueyama Y, Watanabe T, Tamaoki N. Establishment of specific monoclonal antibodies against recombinant human granulocyte colony-stimulating factor (hG-CSF) and their application for immunoperoxidase staining of paraffin-embedded sections. J Histochem Cytochem. 1990;38:283-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 37] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Akatsuka A, Shimamura K, Katoh Y, Takekoshi S, Nakamura M, Nomura H, Hasegawa M, Ueyama Y, Tamaoki N. Electron microscopic identification of the intracellular secretion pathway of human G-CSF in a human tumor cell line: a comparative study with a Chinese hamster ovary cell line (IA1-7) transfected with human G-CSF cDNA. Exp Hematol. 1991;19:768-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 6. | Sugawara Y, Fisher SJ, Zasadny KR, Kison PV, Baker LH, Wahl RL. Preclinical and clinical studies of bone marrow uptake of fluorine-1-fluorodeoxyglucose with or without granulocyte colony-stimulating factor during chemotherapy. J Clin Oncol. 1998;16:173-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 144] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Murata Y, Kubota K, Yukihiro M, Ito K, Watanabe H, Shibuya H. Correlations between 18F-FDG uptake by bone marrow and hematological parameters: measurements by PET/CT. Nucl Med Biol. 2006;33:999-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Suzuki A, Takahashi T, Okuno Y, Seko S, Fukuda Y, Nakamura K, Fukumoto M, Konaka Y, Imura H. Liver damage in patients with colony-stimulating factor-producing tumors. Am J Med. 1993;94:125-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Yoshimoto A, Kasahara K, Saito K, Fujimura M, Nakao S. Granulocyte colony-stimulating factor-producing malignant pleural mesothelioma with the expression of other cytokines. Int J Clin Oncol. 2005;10:58-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Kuroshima T, Wada M, Sato T, Takano M, Makino S. G-CSF producing oral carcinoma with diffuse uptake of FDG in the bone marrow: A case report. Oncol Lett. 2018;15:1241-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Nakamura M, Oshika Y, Abe Y, Ozeki Y, Katoh Y, Yamazaki H, Kijima H, Ueyama Y, Ogata T, Tamaoki N. Gene expression of granulocyte colony stimulating factor (G-CSF) in non-small cell lung cancer. Anticancer Res. 1997;17:573-576. [PubMed] |
| 12. | Nagata H, Komatsu S, Takaki W, Okayama T, Sawabe Y, Ishii M, Kishimoto M, Otsuji E, Konosu H. Granulocyte colony-stimulating factor-producing hepatocellular carcinoma with abrupt changes. World J Clin Oncol. 2016;7:380-386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Kawaguchi M, Asada Y, Terada T, Takehara A, Munemoto Y, Fujisawa K, Mitsui T, Iida Y, Miura S, Sudo Y. Aggressive recurrence of gastric cancer as a granulocyte-colony-stimulating factor-producing tumor. Int J Clin Oncol. 2010;15:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Horii A, Shimamura K, Honjo Y, Mitani K, Miki T, Takashima S, Yoshida J. Granulocyte colony stimulating factor-producing tongue carcinoma. Head Neck. 1997;19:351-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Kaneko N, Kawano S, Matsubara R, Goto Y, Jinno T, Maruse Y, Sakamoto T, Hashiguchi Y, Iida M, Nakamura S. Tongue squamous cell carcinoma producing both parathyroid hormone-related protein and granulocyte colony-stimulating factor: a case report and literature review. World J Surg Oncol. 2016;14:161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Ishigami T, Yoshida H, Yusa H, Yanagawa T. Gingival cancer suspected of producing granulocyte colony-stimulating factor: report of a case. J Oral Maxillofac Surg. 2001;59:804-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Kodama M, Khanal A, Habu M, Yoshioka I, Tominaga K. Granulocyte colony-stimulating factor-producing mucoepidermoid carcinoma of the mandibular gingiva. Asian J Oral Maxillofac Surg. 2009;21:54-58. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Kobayashi J, Miyazaki A, Yamamot T, Nakamori K, Suzuki R, Kaneko T, Suzuki N, Hiratsuka H. Granulocyte colony-stimulating factor-producing squamous cell carcinoma of the lower gingiva: a case report. Head Neck Oncol. 2012;4:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Berdel WE, Danhauser-Riedl S, Steinhauser G, Winton EF. Various human hematopoietic growth factors (interleukin-3, GM-CSF, G-CSF) stimulate clonal growth of nonhematopoietic tumor cells. Blood. 1989;73:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Noda I, Fujieda S, Ohtsubo T, Tsuzuki H, Tanaka N, Sunaga H, Saito H. Granulocyte-colony-stimulating factor enhances invasive potential of human head-and-neck-carcinoma cell lines. Int J Cancer. 1999;80:78-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Tachibana M, Miyakawa A, Tazaki H, Nakamura K, Kubo A, Hata J, Nishi T, Amano Y. Autocrine growth of transitional cell carcinoma of the bladder induced by granulocyte-colony stimulating factor. Cancer Res. 1995;55:3438-3443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |