Published online Apr 6, 2020. doi: 10.12998/wjcc.v8.i7.1287
Peer-review started: December 20, 2019
First decision: January 7, 2020
Revised: January 13, 2020
Accepted: March 9, 2020
Article in press: March 9, 2020
Published online: April 6, 2020
Processing time: 108 Days and 5.2 Hours
Metastatic tumors of the hand are very rare. They are usually late manifestations of massive advanced malignancies. However, a small portion of acrometastases are indications of occult primary cancer. Here, we report an extremely rare case in which a scaphoid bone lesion was the initial manifestation and was found to be a metastasis from gastroesophageal junction (GEJ) cancer.
A 57-year-old male patient presented with ongoing left wrist pain and swelling after trauma. He was initially misdiagnosed with infection of the scaphoid bone and treated with antibiotics and anti-inflammatory drugs. Further radiographic investigations showed a scaphoid pathological fracture, indicating a metastatic tumor derived from the GEJ and/or right lung malignancies. Gastroscopy failed to identify the pathology of the mass at the GEJ, which grew in an exophytic pattern. A lung puncture biopsy was not performed because the patient refused the procedure. To relieve his wrist pain and obtain a definite pathology, we resected the scaphoid lesion. Based on the clinical and pathological results, the patient was finally diagnosed with multiple metastases of advanced GEJ adenocarcinoma. He underwent chemotherapy and died 6 mo after his initial presentation.
Despite the rareness of the disease, orthopedic surgeons should consider the possibility of metastasis to the bones of the hand when patients complain of persistent and progressive pain in the hand.
Core tip: Hand metastasis is very rare, especially when it is the first sign of an occult primary malignancy. Here, we report a case of a scaphoid bone lesion that had metastasized from a gastroesophageal junction adenocarcinoma; the initial manifestation was persistent wrist pain and swelling. Due to its low incidence and the lack of specific symptoms, hand bone metastasis is easily misdiagnosed, leading to delayed treatment. A review of the literature provides a systematic understanding of the epidemiology, manifestations, diagnosis, treatment, and prognosis of metastatic carcinomas of the hand. Moreover, the early detection and diagnosis of hand metastasis are needed to improve patients’ quality of life and prolong their survival.
- Citation: Zhang YJ, Wang YY, Yang Q, Li JB. Scaphoid metastasis as the first sign of occult gastroesophageal junction cancer: A case report. World J Clin Cases 2020; 8(7): 1287-1294
- URL: https://www.wjgnet.com/2307-8960/full/v8/i7/1287.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i7.1287
Metastases to the hand bones are rarely encountered in clinical practice and comprise approximately 0.1% of all osseous metastases[1]. They can be misdiagnosed as rheumatic or infectious diseases due to the lack of specific symptoms. Usually, they are late manifestations of various advanced malignancies; however, in 16% of the affected patients, they are the initial manifestation of an occult cancer[2]. Here, we report an extremely rare case of a scaphoid bone lesion that was found to be a metastasis from a gastroesophageal junction (GEJ) adenocarcinoma.
A 57-year-old male patient presented with persistent left wrist pain and swelling 2 mo after trauma.
Two months prior to this visit, the patient presented with ongoing left wrist pain and swelling after trauma. Based on an initial computed tomography (CT) scan, the patient was diagnosed with an infection of the scaphoid bone and treated with antibiotics, anti-inflammatory drugs, and rest at a local hospital. However, the pain continued to worsen, and the motion of the wrist was restricted.
The patient had undergone acupotomology therapy several months before the onset of the disease. He had a history of cerebral infarction and intestinal polyps.
The patient was a regular drinker and heavy cigarette smoker with no relevant family history.
Physical examination showed left wrist tenderness, swelling, and restriction of motion with regard to radial and ulnar deviation. The swollen area was neither warm nor erythematous.
The C-reactive protein level (49 mg/L) and the erythrocyte sedimentation rate (33 mm/h) were elevated, and the levels of tumor markers, such as carbohydrate antigen (CA)-125 (390 U/mL), carcinoembryonic antigen (CEA) (8 ng/mL), and CA211 (5.4 ng/mL), were significantly elevated.
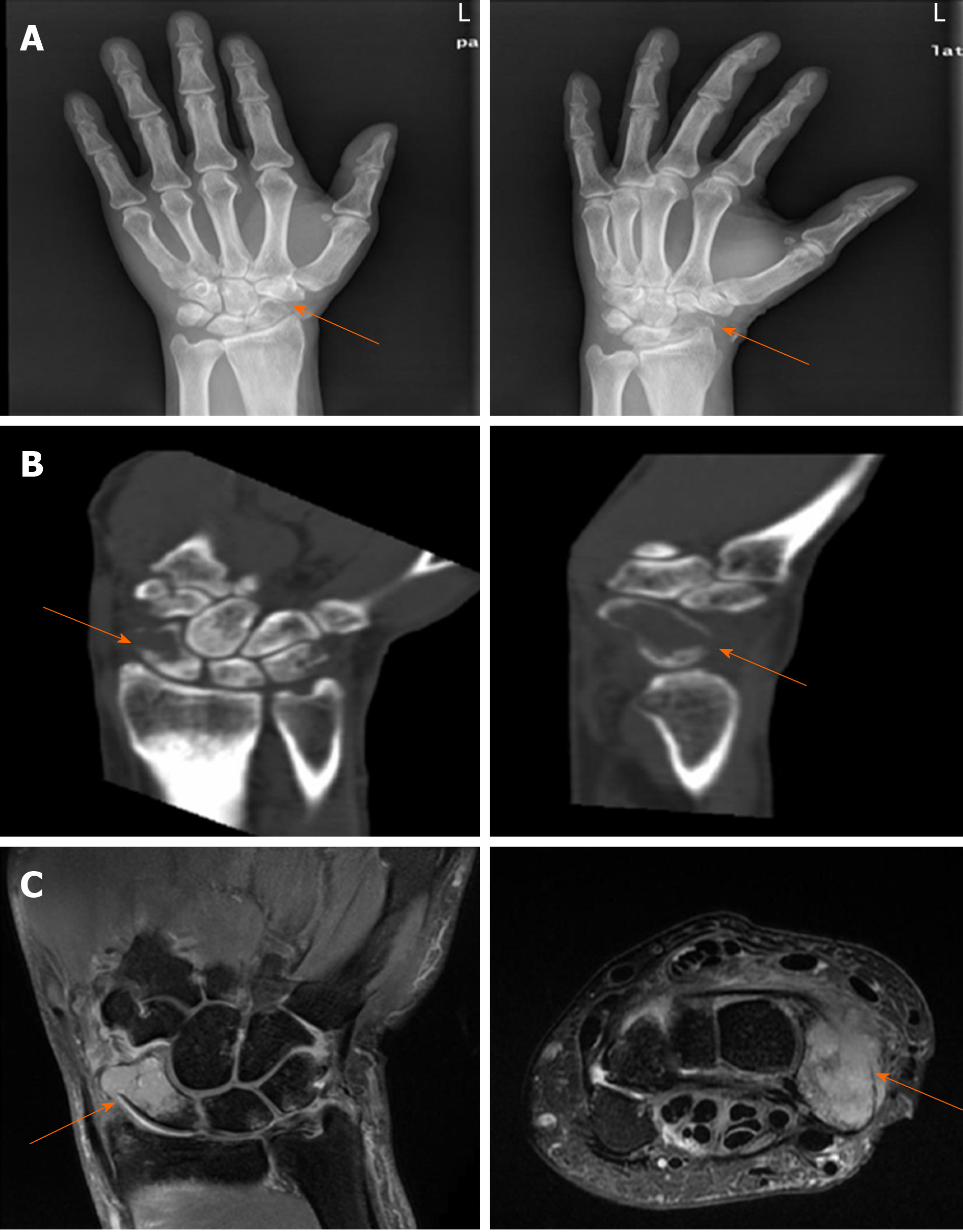
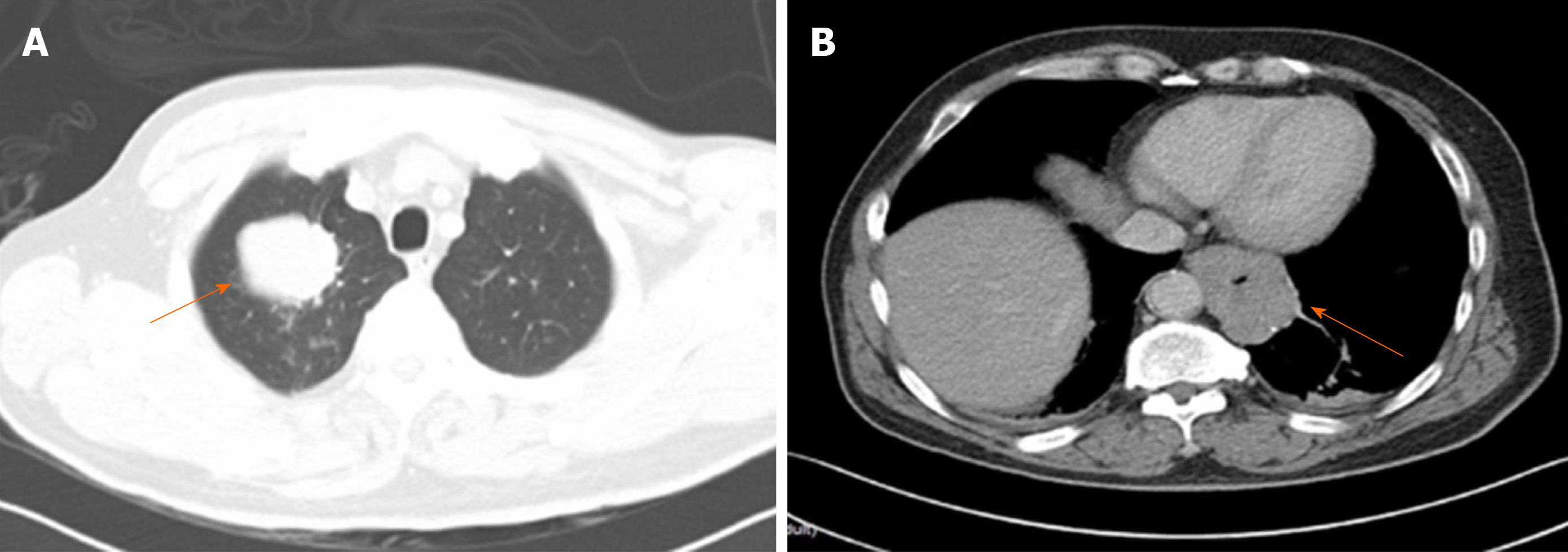
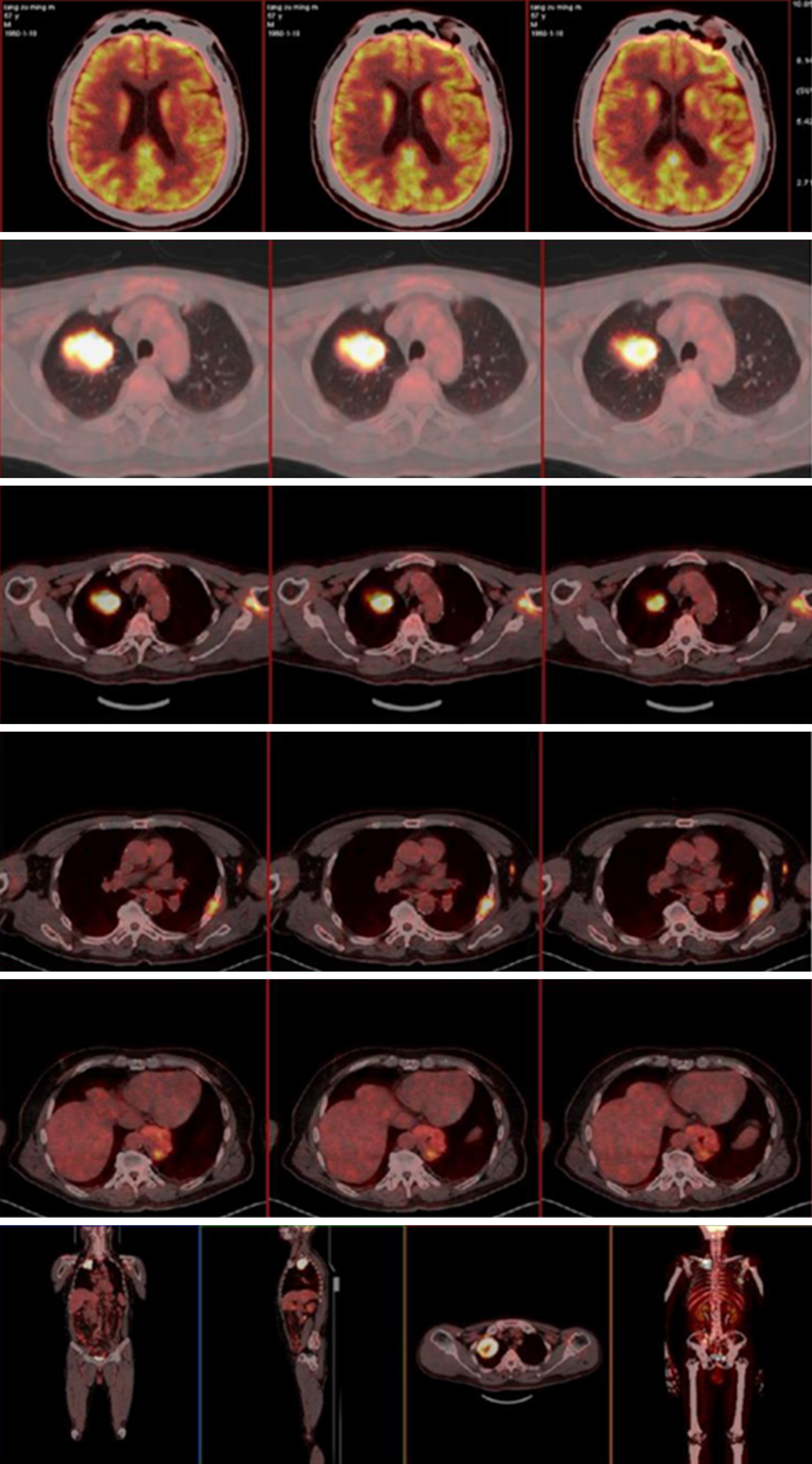
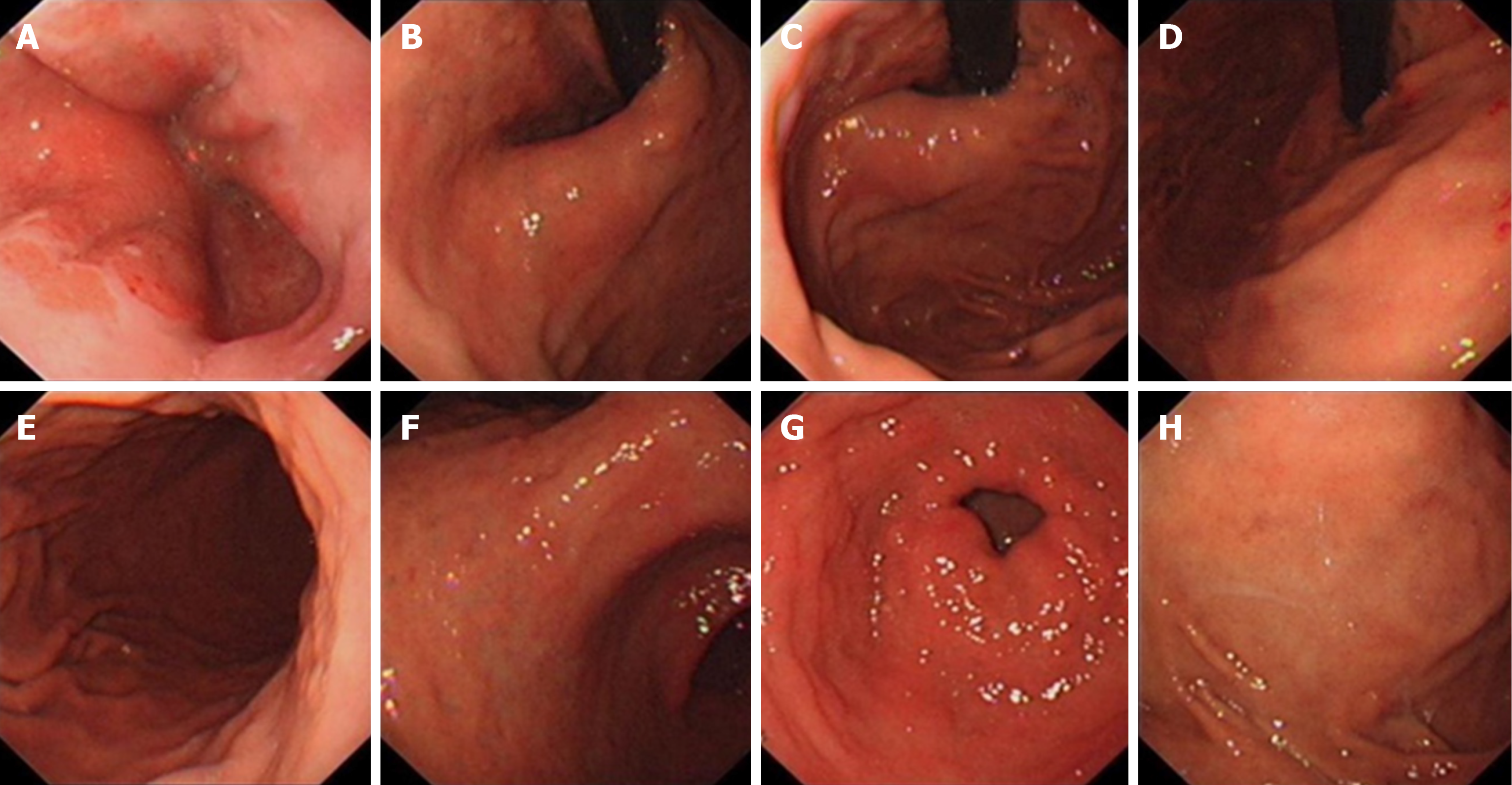
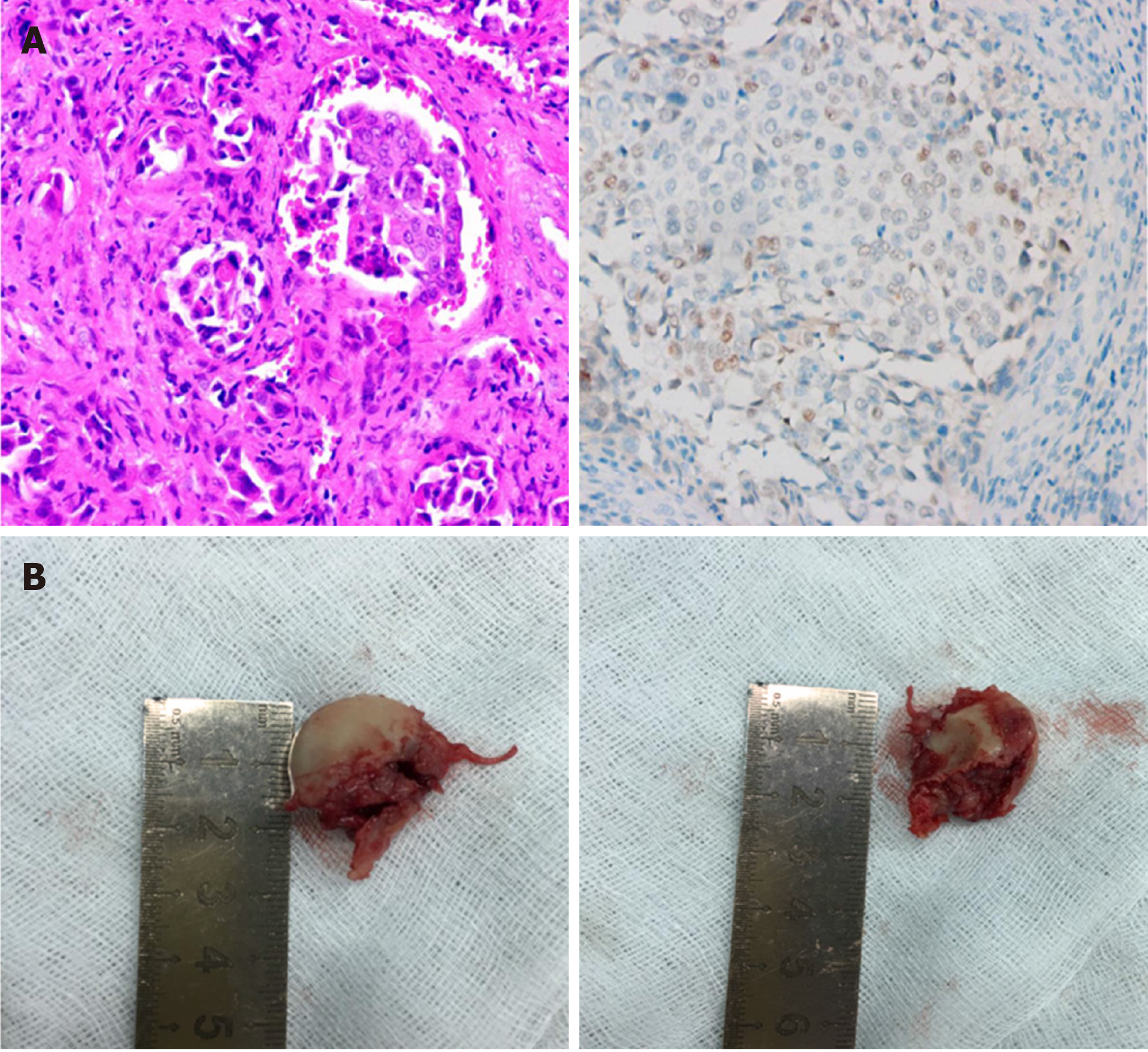
Plain radiographs showed scaphoid bone density reduction and fracture (Figure 1A). CT and magnetic resonance imaging (MRI) scans revealed scaphoid and triangular bone destruction and soft tissue swelling, indicating a pathological fracture (Figure 1B and C). A subsequent chest CT scan suggested a lower esophageal and stomachus cardiacus mass, a right lung mass, and the destruction of multiple ribs (Figure 2A and B). We then performed positron emission tomography-CT with 2-18F fluoro-2 deoxy-D-glucose that led to a strong suspicion of GEJ and/or right lung malignancies with metastases in multiple locations, including the left lung, lymph nodes, ribs, and scapula (Figure 3). A subsequent gastroscopy did not show any space-occupying lesions (Figure 4), and the biopsy showed only chronic superficial gastritis. A CT-guided percutaneous lung puncture biopsy was refused by the patient. Pathology of the left wrist showed scaphoid bone metastasis of poorly differentiated adenocarcinoma. Immunohistochemistry showed that the sample was positive for caudal type homeobox 2 (CDX2) and negative for thyroid transcription factor 1 (TTF-1) and ALK-Lung (Figure 5A).
The patient was diagnosed with GEJ cancer with multiple metastases.
To relieve wrist pain and obtain a definite pathology, the patient underwent left scaphoid lesion resection (Figure 5B). Based on the pathology results, he was treated with two courses of chemotherapy (paclitaxel and cisplatin). He subsequently discontinued chemotherapy due to intolerance.
The patient died of severe interstitial pneumonia 6 mo after his initial presentation.
Bone metastases are very common in various carcinomas and mainly occur in the axial skeleton, such as the spine, pelvis, and ribs. Metastatic involvement of the hand is extremely rare. Kerin[1] demonstrated that the incidence of hand metastasis is 0.1% among all skeletal metastases. Hematogenous spread is the most common route of tumor metastasis. The hand bones have less red bone marrow, and the remoteness of the anatomical location may account for the low incidence of this disease[3]. Trauma can contribute to acrometastasis. Repeated trauma may induce the production of chemotactic factors, such as prostaglandins, which promote cell migration and attachment. Additionally, the injury repair process creates an appropriate environment for tumor growth, invasion, and metastatic potential[4]. The incidence of hand metastasis is higher in males than in females. The lungs, gastrointestinal tract, kidneys, and breasts are the most common primary tumor sites. Within the hand, the distal phalanges are the most frequently involved bones, followed by the metacarpals, proximal phalanges, middle phalanges, and, rarely, the carpal bones[5]. To the best of our knowledge, metastasis to the carpal scaphoid bone, as was observed in our patient, has rarely been reported[6], especially as the initial symptom of a primary tumor.
The signs and symptoms of hand metastases include pain, tenderness, enlarged digits, palpable masses, ulcerations, mechanical dysfunctions, and pathological fractures, which lack specificity. Consequently, hand metastases are often misdiagnosed as osteomyelitis, soft tissue infections, gout, tenosynovitis, arthritis, or other inflammatory processes[7]. Our patient was initially misdiagnosed with a bone infection. Hence, despite its rarity, orthopedic surgeons should consider the possibility of metastases to the hand bone when patients complain of persistent and progressive pain in the hand. Radiographic investigations, such as plain radiography, CT, or MRI, play vital roles in the diagnosis of hand metastases. A positron emission tomography-CT scan can help reveal the primary tumor earlier than other techniques, as it has a sensitivity greater than 90% and a specificity of 78%[8]. The above imaging examinations can be used for auxiliary diagnosis; however, the final diagnosis should depend on pathology.
To date, there is no standard treatment for hand metastases[9,10]. Most treatments are intended to alleviate pain and protect hand function. Radiotherapy, amputation, chemotherapy, curettage, cementation, and wide excision are the most commonly used forms of treatment. Hand metastasis often reflects the widespread dissemination of the tumor, which indicates a poor prognosis. The prognosis depends on the aggressiveness of the primary tumor. The median survival is only approximately 6 mo[1,11].
In our case, we resected the lesion to relieve the patient’s discomfort and obtain pathological specimens. The pathology indicated scaphoid bone metastasis of poorly differentiated adenocarcinoma, with the characteristics of CDX2 (+), TTF-1 (-), and ALK-Lung (-). CDX2 is a pathological marker of gastrointestinal adenocarcinoma, and TTF-1 and ALK-Lung indicate lung metastatic tumors[12,13]. The exophytic growth pattern of the digestive tract tumor observed on the CT scan might explain the negative results on endoscopy and biopsy. Hence, according to the clinical and pathological findings, we concluded that the scaphoid metastasis originated from a cancer of the GEJ. The GEJ is defined as the junction between the esophagus and the stomach. In this location, esophageal squamous epithelial cells gradually transition to gastric gland cells, which can be easily damaged by gastric acid reflux and are associated with a higher risk of cancer transformation[14]. The incidence of GEJ adenocarcinoma has gradually increased over the last 20 years and is associated with obesity, smoking, and gastroesophageal reflux[15-18]. Dysphagia and retrosternal pain are often the initial manifestations. The majority of GEJ cancer patients are initially diagnosed at an advanced stage and have a poor prognosis[19]. In addition to the common sites of esophageal cancer metastases, such as the lymph nodes, lungs, liver, and bones, unexpected metastases have been increasingly reported, especially from lower esophageal cancer. The head and neck, thorax, abdominopelvic region, extremities, and multiple skin and muscle sites are the five main unexpected metastatic sites[20]. Multidisciplinary management, including surgery, chemoradio-therapy, and targeted therapy, is advised[21]. Surgery is the only curative treatment, while auxiliary perioperative chemoradiotherapy and targeted therapy can improve the survival rate[22,23]. In this case, the patient had an advanced stage of disease and was not a candidate for surgical treatment. Immunohistochemistry showed negativity for human epidermal growth factor receptor 2; hence, trastuzumab was not used.
In addition, because lung specimens were not available, it was difficult to determine whether the right lung mass was a secondary (metastasis) or primary tumor. After surgery, the patient’s quality of life was greatly improved. However, the patient survived for only 6 mo after his initial presentation, potentially due to the delayed diagnosis and the aggressiveness of the primary tumor. Therefore, early diagnosis of metastasis to the hand bone could be helpful in that it allows the initiation of an appropriate course of treatment and prolongs survival time.
Hand metastases from solid tumors are clinically rare. Usually, they are late manifestations of advanced malignancies; however, sometimes they can be the initial manifestation of an occult cancer. Because of their low incidence and nonspecific symptoms, hand metastases are often misdiagnosed. Orthopedic surgeons should not ignore the possibility of hand metastases when patients complain of persistent and progressive pain in the hand. The treatment of hand metastasis is individualized and based on the clinical symptoms and characteristics of the primary tumor. The prognosis is generally poor. It is therefore important for clinicians to detect and diagnose these cancers early.
Manuscript source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kikuchi H, Streba LAM S-Editor: Wang YQ L-Editor: Wang TQ E-Editor: Ma YJ
| 1. | Kerin R. The hand in metastatic disease. J Hand Surg Am. 1987;12:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 84] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Hayden RJ, Sullivan LG, Jebson PJ. The hand in metastatic disease and acral manifestations of paraneoplastic syndromes. Hand Clin. 2004;20:335-343, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Berrettoni BA, Carter JR. Mechanisms of cancer metastasis to bone. J Bone Joint Surg Am. 1986;68:308-312. [PubMed] |
| 4. | Lewin JS, Cleary KR, Eicher SA. An unusual metastasis to the thumb in a laryngectomized tracheoesophageal speaker. Arch Otolaryngol Head Neck Surg. 1997;123:1007-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Afshar A, Farhadnia P, Khalkhali H. Metastases to the hand and wrist: an analysis of 221 cases. J Hand Surg Am. 2014;39:923-32.e17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Naito K, Furuya H, Han C, Orita H, Sato K, Kaneko K, Obayashi O. Gastric cancer with metastases to the scaphoid: a case report. J Orthop Sci. 2015;20:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Leeson MC, Makley JT, Carter JR. Metastatic skeletal disease distal to the elbow and knee. Clin Orthop Relat Res. 1986;94-99. [PubMed] |
| 8. | Bhandari T, Brown E. Acrometastasis and the potential benefits of early positron emission tomography scanning. Ann Plast Surg. 2011;67:189-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Ghert MA, Harrelson JM, Scully SP. Solitary renal cell carcinoma metastasis to the hand: the need for wide excision or amputation. J Hand Surg Am. 2001;26:156-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Flynn CJ, Danjoux C, Wong J, Christakis M, Rubenstein J, Yee A, Yip D, Chow E. Two cases of acrometastasis to the hands and review of the literature. Curr Oncol. 2008;15:51-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | Gilardi R, Della Rosa N, Pancaldi G, Landi A. Acrometastasis showing an occult lung cancer. J Plast Surg Hand Surg. 2013;47:550-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Ma H, Yu J, Tang J. LI-cadherin and CDX2: Useful Markers in Metastatic Gastrointestinal Adenocarcinoma Cells in Serous Cavity Effusion. Appl Immunohistochem Mol Morphol. 2019;27:e75-e80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Vidarsdottir H, Tran L, Nodin B, Jirström K, Planck M, Jönsson P, Mattsson JSM, Botling J, Micke P, Brunnström H. Immunohistochemical profiles in primary lung cancers and epithelial pulmonary metastases. Hum Pathol. 2019;84:221-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Chevallay M, Bollschweiler E, Chandramohan SM, Schmidt T, Koch O, Demanzoni G, Mönig S, Allum W. Cancer of the gastroesophageal junction: a diagnosis, classification, and management review. Ann N Y Acad Sci. 2018;1434:132-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 15. | Bollschweiler E, Wolfgarten E, Gutschow C, Hölscher AH. Demographic variations in the rising incidence of esophageal adenocarcinoma in white males. Cancer. 2001;92:549-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 16. | Steffen A, Huerta JM, Weiderpass E, Bueno-de-Mesquita HB, May AM, Siersema PD, Kaaks R, Neamat-Allah J, Pala V, Panico S, Saieva C, Tumino R, Naccarati A, Dorronsoro M, Sánchez-Cantalejo E, Ardanaz E, Quirós JR, Ohlsson B, Johansson M, Wallner B, Overvad K, Halkjaer J, Tjønneland A, Fagherazzi G, Racine A, Clavel-Chapelon F, Key TJ, Khaw KT, Wareham N, Lagiou P, Bamia C, Trichopoulou A, Ferrari P, Freisling H, Lu Y, Riboli E, Cross AJ, Gonzalez CA, Boeing H. General and abdominal obesity and risk of esophageal and gastric adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2015;137:646-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Souza RF. From Reflux Esophagitis to Esophageal Adenocarcinoma. Dig Dis. 2016;34:483-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Kabat GC, Ng SK, Wynder EL. Tobacco, alcohol intake, and diet in relation to adenocarcinoma of the esophagus and gastric cardia. Cancer Causes Control. 1993;4:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 179] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Markar SR, Karthikesalingam A, Low DE. Outcomes assessment of the surgical management of esophageal cancer in younger and older patients. Ann Thorac Surg. 2012;94:1652-1658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Shaheen O, Ghibour A, Alsaid B. Esophageal Cancer Metastases to Unexpected Sites: A Systematic Review. Gastroenterol Res Pract. 2017;2017:1657310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 21. | Al-Batran SE, Homann N, Pauligk C, Illerhaus G, Martens UM, Stoehlmacher J, Schmalenberg H, Luley KB, Prasnikar N, Egger M, Probst S, Messmann H, Moehler M, Fischbach W, Hartmann JT, Mayer F, Höffkes HG, Koenigsmann M, Arnold D, Kraus TW, Grimm K, Berkhoff S, Post S, Jäger E, Bechstein W, Ronellenfitsch U, Mönig S, Hofheinz RD. Effect of Neoadjuvant Chemotherapy Followed by Surgical Resection on Survival in Patients With Limited Metastatic Gastric or Gastroesophageal Junction Cancer: The AIO-FLOT3 Trial. JAMA Oncol. 2017;3:1237-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 332] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 22. | Okereke IC. Management of Gastroesophageal Junction Tumors. Surg Clin North Am. 2017;97:265-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Klevebro F, Ekman S, Nilsson M. Current trends in multimodality treatment of esophageal and gastroesophageal junction cancer - Review article. Surg Oncol. 2017;26:290-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |