Published online Apr 6, 2020. doi: 10.12998/wjcc.v8.i7.1232
Peer-review started: December 21, 2019
First decision: January 17, 2020
Revised: February 25, 2020
Accepted: March 9, 2020
Article in press: March 9, 2020
Published online: April 6, 2020
Processing time: 106 Days and 23.4 Hours
Depression is common in patients with myocardial infarction and has been independently associated with adverse outcomes. However, the association between depression and myocardial injury on cardiac magnetic resonance (CMR) in patients with ST-segment elevation myocardial infarction (STEMI) has still not been assessed.
To assess the association between depression and myocardial injury on CMR in patients with STEMI.
A total of 107 STEMI patients undergoing primary percutaneous coronary intervention (P-PCI) were analyzed in this prospectivecohort study. Each subject completed the Patient Health Questionnaire-9 (PHQ-9) to assess the presence and severity of depressive symptoms. CMR was performed at a median of 3 d after P-PCI for quantifying post-MI myocardial injury. Correlations between depression identified by the PHQ-9 and myocardial injury measured on CMR were assessed.
In this study, 19 patients (17.8%) were diagnosed with major depression identified by the PHQ-9 ≥ 10. PHQ-9 was analyzed both as a continuous variable and dichotomous variable. After multivariable adjustment, the proportion of patients with large infarction size was significantly higher in the major depression group (PHQ-9 ≥ 10) (OR: 4.840, 95%CI: 1.122–20.868, P =0.034). When the PHQ-9 was evaluated as a continuous variable, after multivariable adjustment, an increased PHQ-9 score was associated with an increased risk of large infarction size (OR: 1.226, 95%CI: 1.073–1.401, P =0.003).
In patients with STEMI undergoing PCI, depression was independently associated with a large infarction size.
Core tip: This is a prospective study with 107 ST-segment elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention(P-PCI).The association between depression and myocardial injury measured on cardiac magnetic resonance was evaluated. Depression could predict large infarction size in patients with STEMI undergoing P-PCI .
- Citation: Sun ZQ, Yu TT, Ma Y, Ma QM, Jiao YD, He DX, Jia-KeWu, Wen ZY, Wang XN, Hou Y, Sun ZJ. Depression and myocardial injury in ST-segment elevation myocardial infarction: A cardiac magnetic resonance imaging study. World J Clin Cases 2020; 8(7): 1232-1240
- URL: https://www.wjgnet.com/2307-8960/full/v8/i7/1232.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i7.1232
Patients with myocardial infarction (MI) have a high prevalence of depression[1,2]. Post-MI depression has been independently associated with higher all-cause mortality, cardiac mortality, nonfatal events and health care costs[3-11]. Altered autonomic nervous system activity[12], inflammation[13], platelet activation[14] and low brain-derived neurotrophic factor[15] may play important roles in the mechanism of depression affecting the prognosis of patients with MI. However, the detailed pathophysiological association between depression and adverse outcomes in patients with MI still needs further evaluation[16]. Cardiac magnetic resonance (CMR) is the gold standard for quantifying post-MI myocardial injury[17,18]. CMR-related variables, such as infarct size[19], microvascular obstruction (MVO)[20,21], area at risk (AAR)[22], intramyocardial hemorrhage (IMH)[23,24] and the myocardial salvage index (MSI)[25,26] are strong predictors for left ventricular remodeling and outcome in patients with MI. To date, there are no CMR data in the literature on patients with ST-segment elevation myocardial infarction (STEMI) and depression. The Patient Health Questionnaire-9 (PHQ-9) is a self-report checklist derived from the interview used in the Primary Care Evaluation of Mental Disorders[27]. The PHQ-9 assesses the presence and severity of depressive symptoms[28] and has reasonable sensitivity and specificity for patients with MI[29-33]. Other studies have also found that the PHQ-9 could identify cardiac patients at risk for adverse cardiovascular outcomes[34,35]. In this study, we aimed to assess the association between depression identified by the PHQ-9 and myocardial injury measured on CMR in patients with STEMI.
A total of 206 patients with STEMI admitted to Shengjing Hospital of China Medical University, Shenyang, China for primary percutaneous coronary intervention (P-PCI) were prospectively enrolled between November 1, 2016, and November 1, 2018. The diagnosis of STEMI should meet the following criteria to be eligible for P-PCI: (1) Chest pain present less than 12 h from onset of pain to time of catheterization; and (2) Significant ST-segment elevation (at least 0.1 mV in two or more standard leads or at least 0.2 mV in two or more contiguous precordial leads) or a new left bundle branch block. P-PCI was urgently undertaken according to the current guidelines[36,37]. Clinical data and procedural data of all cases were obtained by the investigators using electronic medical records, interventional imaging data (Picture Archiving and Communication Systems technology; Neusoft, Shenyang, China), and surgical records. The exclusion criteria were as follows: (1) No depression data (12 cases); (2) No or poor-quality CMR data (72 cases); (3) Known malignancy, severe organic failure such as end-stage liver or renal failure (4 cases); (4) Significant cognitive dysfunction, including dementia and/or stroke, or antipsychotic treatment including antidepressant drugs at the time of evaluation (2 cases); and (5) Contraindications for CMR (e.g., pacemaker or aneurysm clips) or contraindications for gadolinium-based contrast (e.g., creatinine clearance ≤ 60 mL/min/1.73m2) (7 cases). A total of 107 patients with STEMI undergoing CMR were ultimately included in this study (Figure 1). This study complied with the Declaration of Helsinki, and the Shengjing Hospital of China Medical University Research Ethics Committee approved the research protocol. Written informed consent was formally obtained from all participants.
Depressive symptoms were assessed using the PHQ-9 three days post-MI and before discharge. The PHQ-9 is a brief depression screening instrument that patients are able to complete quickly and without assistance. It includes 9 items: (1) Lack of interest; (2) Depressed mood; (3) Sleeping difficulties; (4) Tiredness; (5) Appetite problems; (6) Negative feelings about self; (7) Concentration problems; (8) Retardation; and (9) Suicidal ideation. Patients were asked to what extent the symptom was present during the last 2 wk (0 = not at all; 1 = on several days; 2 = most of the time; 3 = all of the time). A score between 0 and 27 points was obtained by the sum of the patient’s responses. A PHQ-9 score of ≥ 10 has been recommended to screen for the diagnosis of major depression[27,28].
According to the previous studies[17,18], CMR was performed at a median of 3 days (3-7 d) after P-PCI using a 3.0-T MR scanner (Philips Intera, Best, the Netherlands) with a 32-channel phased-array receiver coil. Images were ECG triggered and obtained during breath-holding at end-inspiration. Cine MR imaging was performed with a steady-state free procession cine sequence in the vertical and horizontal long-axis and short-axis of cardiac orientations. After the cine imaging, T2-weighted imaging with fat suppression was performed in the continuous short-axis orientation using a dark-blood inversion recovery fast-spin echo sequence. Late gadolinium enhancement imaging was then performed 10 min after intravenous injection of 0.2 mmol/kg gadodiamide hydrate, using an inversion-recovery technique.
Physicians who were blinded to all clinical data performed the CMR analysis using a dedicated cardiac software package. Image quality was graded on a 4-point scale: 3 = excellent, 2 = good, 1 = moderate, and 0 = unanalyzable. The structural and functional parameters of the left ventricle were analyzed from cine imagesimaging on a commercially available workstation (MASS v7.2, Medis, City, The Netherlands).
AAR was defined as hyperenhancement (myocardial edema) on T2-weighted imaging, and expressed in grams and as a percentage of the total LV mass. Areas of hypoenhancement with edema were regarded as IMH and included in the AAR. Infarct myocardium was defined as the enhanced area of myocardium on late gadolinium enhancement images. The infarct size was expressed in grams and as a percentage of the total LV mass. Areas of hypoenhancement within the infarct were regarded as MVO and included in the infarct size. The myocardial salvage index was calculated as follows: (AAR-infarct size)/AAR.
Quantitative variables with a normal distribution were represented as the mean ± SD and compared with the independent samples t-test. Quantitative variables without a normal distribution were represented as median [interquartile range, (IQR)] and compared with Mann-Whitney U-test. Categorical variables were represented as counts and proportions (%) and compared with the χ2 test. Correlations between depression identified by the PHQ-9 and myocardial injury measured on CMR were assessed using Pearson’s or Spearman’s methods. Depending on the quintile of the infarct size, a large infarct size was defined as a value in the fifth quintile (infarct size ≥ 20.94%). A binary logistic univariate regression analysis was performed to evaluate predictors of the infarct size. A binary logistic multivariate regression model was used to identify independent predictors of the infarct size. Variables with P < 0.05 in Supplementary Table 1 on univariate analysis were entered into a multivariate analysis. The results were reported as odds ratios (ORs) with associated 95%CIs. All tests were two-sided, and statistical significance was defined as P < 0.05. All statistical analyses were performed with SPSS version 19 (SPSS Inc., Chicago, Illinois, United States).
A total of 107 patients with STEMI and CMR undergoing PCI were included in this study. Among them, 19 cases (17.8%) had a PHQ-9 score of ≥ 10 and were diagnosed with major depression. As shown in Table 1, the major depression group had significantly higher heart rates on admission, higher creatinine and higher total cholesterol compared with the group of patients with a PHQ-9 score < 10. The percentage of intra-aortic balloon pump use was significantly higher in the major depression group. The major depression group also had a significant tendency towards decreasing stroke volume but increasing area at risk and infarction size (Table 2).
| Variables | Overall (n = 107) | PHQ-9 score < 10 (n = 88) | PHQ-9 score ≥ 10 (n = 19) | P value |
| Demographics | ||||
| Age, yr | 56.5 ± 10.5 | 56.2 ± 10.7 | 58.1 ± 9.8 | 0.469 |
| Male | 86 (80.4) | 71 (80.7) | 15 (78.9) | 0.863 |
| Medical history | ||||
| History of diabetes mellitus | 29 (27.1) | 23 (26.1) | 6 (31.6) | 0.628 |
| History of hypertension | 44 (41.1) | 34 (38.6) | 10 (52.6) | 0.261 |
| History of cerebrovascular disease | 12 (11.2) | 11 (12.5) | 1 (5.3) | 0.365 |
| Prior PCI | 3 (2.8) | 2 (2.3) | 1 (5.3) | 0.474 |
| Current smoking | 74 (69.2) | 61 (69.3) | 13 (68.4) | 0.939 |
| Clinical presentation | ||||
| PHQ-9 score | 4.9 ± 5.1 | 2.9 ± 2.6 | 14.3 ± 2.8 | ≤ 0.001 |
| SBP on admission, mmHg | 125.9 ± 23.8 | 125.7 ± 22.4 | 127.0 ± 30.1 | 0.823 |
| Heart rate on admission, bpm | 78.9 ± 17.2 | 77.3 ± 17.1 | 86.4 ± 16.0 | 0.037 |
| Laboratory results on admission | ||||
| Troponin-I, ng/mL | 27.0 (8.6, 58.5) | 24.7 (9.0, 56.6) | 32.8 (3.5, 80.0) | 0.504 |
| Creatinine, µmol/l | 70.2 ± 16.3 | 67.9 ± 14.8 | 80.8 ± 18.9 | 0.002 |
| Albumin, g/L | 40.5 ± 3.3 | 40.4 ± 3.2 | 40.7 ± 4.2 | 0.789 |
| Hemoglobin, g/L | 139.9 ± 22.5 | 139.6 ± 22.8 | 141.6 ± 21.5 | 0.723 |
| Fasting glucose, mmol/L | 7.38 ± 2.92 | 7.37 ± 2.96 | 7.43 ± 2.83 | 0.936 |
| BNP, ng/L | 111 (58, 239) | 107 (58, 232) | 180 (53, 473) | 0.293 |
| Total cholesterol, mmol/L | 4.83 ± 1.13 | 4.73 ± 1.14 | 5.31 ± 0.99 | 0.041 |
| Low-density lipoprotein, mmol/L | 3.07 ± 1.00 | 2.99 ± 1.00 | 3.43 ± 0.93 | 0.08 |
| High-density lipoprotein, mmol/L | 0.99 ± 0.26 | 0.97 ± 0.26 | 1.07 ± 0.27 | 0.137 |
| Triglycerides, mmol/L | 1.46 (0.99, 2.26) | 1.46 (0.99, 2.21) | 1.47 (0.60, 3.29) | 0.929 |
| Percutaneous coronary intervention details | ||||
| Door-to-balloon time, min | 80.0 (50.0, 120.0) | 81.5 (49.9, 127.8) | 67.3 (50.0, 103.0) | 0.52 |
| Culprit vessels | 0.294 | |||
| Right coronary artery | 52 (48.6) | 45 (51.1) | 7 (36.8) | |
| Left anterior descending artery | 45 (42.1) | 34 (38.6) | 11 (57.9) | |
| Left circumflex artery | 10 (9.3) | 9 (10.2) | 1 (5.3) | |
| Use of intra-aortic balloon pump | 3 (2.8) | 1 (1.1) | 2 (10.5) | 0.025 |
| Killip class I on admission | 95 (88.8) | 80 (90.9) | 15 (78.9) | 0.134 |
| TIMI flow grade 3 post-PCI | 105 (98.1) | 86 (97.7) | 19 (100) | 0.507 |
| Variable | Overall (n = 107) | PHQ-9 score < 10 (n = 88) | PHQ-9 score ≥ 10 (n = 19) | P value |
| LVEDV, mL/m2 | 132.7 ± 27.5 | 132.6 ± 23.3 | 133.4 ± 42.8 | 0.906 |
| LVESV, mL/m2 | 69.8 ± 27.1 | 67.9 ± 22.8 | 78.5 ± 41.6 | 0.123 |
| SV, mL/m2 | 62.7 ± 15.3 | 64.4 ± 14.7 | 54.9 ± 16.2 | 0.014 |
| LVEF, % | 48.5 ± 12.3 | 49.6 ± 11.5 | 43.7 ± 14.8 | 0.059 |
| AAR, % | 33.7 ± 11.7 | 32.5 ± 11.2 | 39.3 ± 12.7 | 0.023 |
| IS, % | 15.40 ± 10.12 | 13.92 ± 7.61 | 22.24 ± 16.20 | 0.001 |
| MVO | 52 (48.6) | 45 (51.1) | 7 (36.8) | 0.258 |
| IMH | 35 (32.7) | 29 (33.0) | 6 (31.6) | 0.908 |
| MSI, % | 55.8 ± 26.4 | 57.3 ± 24.8 | 49.2 ± 32.9 | 0.227 |
The univariate analysis found that multiple variables had significant effects on large infarct size: Troponin-I, high-density lipoprotein, door-to-balloon time, culprit vessels, SV, LVEF, AAR, MVO, IMH and MSI (Supplementary Table 1).
In the univariate logistic regression analysis, when PHQ-9 was evaluated as a continuous variable, an increased PHQ-9 score was significantly predictive of a large infarct size (OR: 1.191, 95%CI: 1.087–1.305, P ≤ 0.001, for per 1 unit increase) (Table 3). After adjusting for covariates, the PHQ-9 was still associated with large infarct size: The large infarct size risk increased by 22.6% per 1 increase in PHQ-9 score (OR: 1.226, 95%CI: 1.073–1.401, P = 0.003) (Table 3).
When categorized into two groups, PHQ-9 ≥ 10 (major depression) remained significantly predictive of large infarct size (Table 3). In the univariate logistic regression analysis, the major depression group had a substantially higher risk of large infarct size (OR: 4.380, 95%CI: 1.520–12.619, P = 0.006) (Table 3). In the multivariable logistic regression analysis, the major depression group still conferred a significantly higher risk of large infarct size (OR: 4.840, 95%CI: 1.122–20.868, P = 0.034) (Table 3).
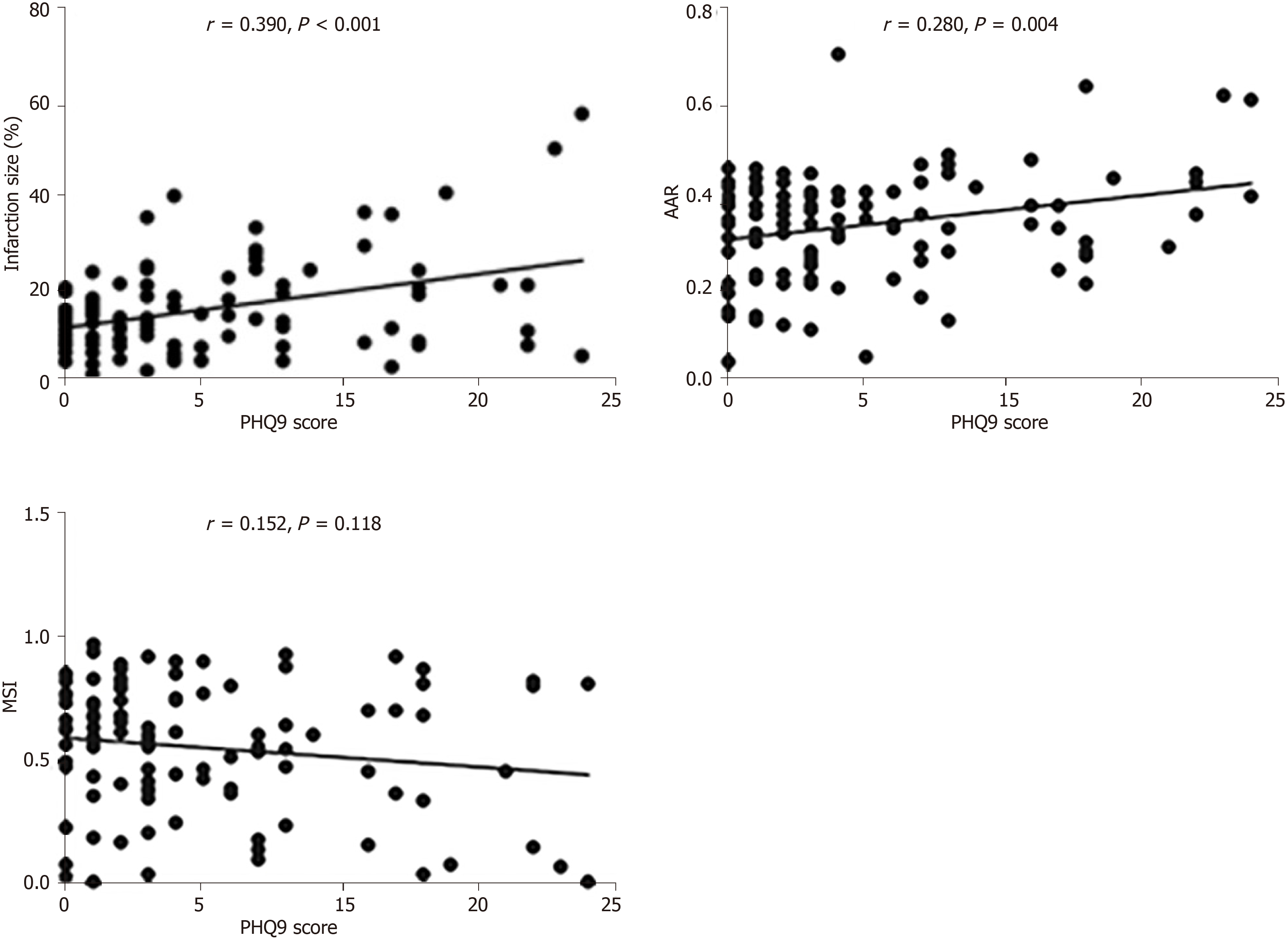
The PHQ-9 score had a significant positive correlation with IS (r = 0.390, P ≤ 0.001) and AAR (r =0.278, P = 0.004) but not with MVO, IMH and MSI (Table 4 and Figure 1).
| Correlation coefficient | P value | |
| AAR | 0.278 | 0.004 |
| IS | 0.39 | ≤ 0.001 |
| MVO | 0.038 | 0.699 |
| IMH | 0.026 | 0.793 |
| MSI | -0.152 | 0.118 |
The present study tested the association between depression identified by the PHQ-9 and myocardial injury measured on CMR in patients with STEMI undergoing PCI. The main findings were as follows: (1) PHQ-9 was an independent predictor of large infarction size; and (2) Depression could predict large infarction size in patients with STEMI undergoing PCI.
Frasure-Smith et al[3] first studied the prognostic value of depression among survivors of myocardial infarction. They found that depression was an independent risk factor for mortality at 6 months in 222 patients hospitalized following an MI, and its impact was equivalent to that of left ventricular dysfunction[3]. This observation was then verified and extended by other studies and meta-analyses, which reported that post-MI depression was independently associated with higher all-cause mortality, nonfatal events and health care costs[4-11]. In addition, other studies focused on the mechanism by which depression affects the prognosis of patients with MI[12-15]. However, the detailed pathophysiological association between depression and adverse outcomes in patients with MI still needs further evaluation[16].
CMR can accurately quantify the structural and functional parameters of left ventricular and myocardial injury post-MI[17,18]. Infarct size represents the total amount of myocardial infarction during STEMI. A previous study confirmed that infarct size, which was independent of left ventricular stunning and loading, was related to left ventricular remodeling and predicted future cardiac events[19]. AAR, which is edematous myocardium at risk of infarction but still potentially reversible, is defined as an area of hyperenhancement (myocardial edema) on T2-weighted imaging. The extent of the AAR is predictive of an increased risk of cardiovascular events in patients with AMI[22]. In this study, depression post-MI was associated with larger myocardial infarct and AAR evaluated by CMR. The results of this study provide a new pathological link to support the association of depression with adverse clinical outcomes. There is a possible explanation for this result. Acute coronary syndrome (ACS) patients with depression had higher levels of platelet micro particles and higher platelet aggregation to adenosine diphosphate and serotonin[14]. Additionally, ACS patients with depression had higher plasma concentrations of platelet factor 4 and β thromboglobulin, which are secreted from alpha granules when the platelet is activated[38]. Platelet aggregation plays a critical role in the formation of coronary thrombosis[39]. Moreover, inflammation takes part in acute thrombotic complications such as plaque rupture and plaque erosion[40]. Higher tumor necrosis factoralpha, IL-6, C-reactive protein levels and white blood cell count have been confirmed in ACS patients with depression[13,14], which indicates that depression may contribute to the maintenance of inflammatory responses. Taken together, depression may increase cardiovascular thrombosis through platelet activation and inflammation response. A greater extent of thrombus formation is related to a larger infarct size and AAR. This may provide a reasonable link between depression and adverse outcomes in patients with STEMI.
This study had several limitations. First, this study was prospective and observational, so potential confounders and selection bias could not be completely adjusted. Second, in this study, depression was assessed with a self-report questionnaire (PHQ-9) during patients’ hospitalization and not with a formal psychiatric interview. However, previous studies have confirmed that the PHQ-9 could assess the presence and severity of depressive symptoms[28], and the PHQ-9 has reasonable sensitivity and specificity in patients with MI[29-33]. Third, in this study, the time intervals between the onset of STEMI and CMR imaging were different, and the severity of myocardial injury may change over time post-MI[17,18]. This was mainly because MRI examinations are in great demand but the machines are limited in our hospital, and it was difficult to ensure the same time interval. However, there was no significant difference in the time intervals between the two groups.
In conclusion, in patients with STEMI undergoing PCI, depression was independently associated with a large infarction size. The PHQ-9 may also help us assess myocardial injury in STEMI.
Patients with myocardial infarction (MI) have a high prevalence of depression, which is related to poor prognosis. However, the detailed pathophysiology of this relationship is still unsubstantiated. Cardiac magnetic resonance (CMR) is the gold standard for quantifying post-MI myocardial injury. The Patient Health Questionnaire-9 (PHQ-9) could assess the presence and severity of depressive symptoms and has reasonable sensitivity and specificity for patients with MI. Revealing the pathological mechanisms underlying the association of depression with adverse clinical outcomes is still a main area of prognostic study of the cardiovascular field.
CMR is the gold standard for quantifying post-MI myocardial injury. Revealing the association between depression and myocardial injury measured on CMR may facilitate the detection of high-risk patients with MI and thereby improve the prognosis of patients.
This study aimed to assess the association between depression identified by the PHQ-9 and myocardial injury measured on CMR in patients with ST-segment elevation myocardial infarction (STEMI).
A total of 107 STEMI patients undergoing primary percutaneous coronary intervention (P-PCI) were analyzed in this prospective cohort study. Each subject completed a PHQ-9 to assess the presence and severity of depressive symptoms. CMR was performed at a median of 3 d after P-PCI for quantifying post-MI myocardial injury. Correlations between depression identified by PHQ-9 and myocardial injury measured on CMR were assessed.
The PHQ-9 was significantly predictive of large infarct size, and the major depression group had a substantially higher large infarct risk. The PHQ-9 score had a significant positive correlation with CMR-related variables of infarction size and area at risk.
In patients with STEMI undergoing PCI, depression was independently associated with a large infarction size. The PHQ-9 may also help us assess myocardial injury in patients with STEMI.
The results of this study provide evidence of a new pathological link to support the association of depression with adverse clinical outcomes of myocardial injury. In the future, more subjects should be incorporated to further confirm the results of this study. Mental health should be emphasized for cardiovascular disease patients. More importantly, cardiovascular physicians and psychologist should unite to fight against these diseases.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berger BM, McCarthy M S-Editor: Wang JL L-Editor: AMedE-Ma JY E-Editor: Xing YX
| 1. | Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21:30-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 566] [Cited by in RCA: 580] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 2. | Lichtman JH, Bigger JT, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lespérance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES; American Heart Association Prevention Committee of the Council on Cardiovascular Nursing; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Epidemiology and Prevention; American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research; American Psychiatric Association. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768-1775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 958] [Cited by in RCA: 951] [Article Influence: 55.9] [Reference Citation Analysis (0)] |
| 3. | Frasure-Smith N, Lespérance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1162] [Cited by in RCA: 986] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 4. | Frasure-Smith N, Lespérance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1053] [Cited by in RCA: 964] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 5. | Frasure-Smith N, Lespérance F, Juneau M, Talajic M, Bourassa MG. Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61:26-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 333] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 6. | Frasure-Smith N, Lespérance F, Gravel G, Masson A, Juneau M, Talajic M, Bourassa MG. Depression and health-care costs during the first year following myocardial infarction. J Psychosom Res. 2000;48:471-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 140] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Smolderen KG, Spertus JA, Reid KJ, Buchanan DM, Krumholz HM, Denollet J, Vaccarino V, Chan PS. The association of cognitive and somatic depressive symptoms with depression recognition and outcomes after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:328-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 170] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 8. | Shah AJ, Ghasemzadeh N, Zaragoza-Macias E, Patel R, Eapen DJ, Neeland IJ, Pimple PM, Zafari AM, Quyyumi AA, Vaccarino V. Sex and age differences in the association of depression with obstructive coronary artery disease and adverse cardiovascular events. J Am Heart Assoc. 2014;3:e000741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 9. | Smolderen KG, Buchanan DM, Gosch K, Whooley M, Chan PS, Vaccarino V, Parashar S, Shah AJ, Ho PM, Spertus JA. Depression Treatment and 1-Year Mortality After Acute Myocardial Infarction: Insights From the TRIUMPH Registry (Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients' Health Status). Circulation. 2017;135:1681-1689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 90] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 10. | de Miranda Azevedo R, Roest AM, Carney RM, Freedland KE, Lane DA, Parakh K, de Jonge P, Denollet J. Individual depressive symptoms and all-cause mortality In 6673 patients with myocardial infarction: Heterogeneity across age and sex subgroups. J Affect Disord. 2018;228:178-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, Freedland KE, Jaffe AS, Leifheit-Limson EC, Sheps DS, Vaccarino V, Wulsin L; American Heart Association Statistics Committee of the Council on Epidemiology and Prevention and the Council on Cardiovascular and Stroke Nursing. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014;129:1350-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 966] [Cited by in RCA: 825] [Article Influence: 75.0] [Reference Citation Analysis (0)] |
| 12. | de Jonge P, Mangano D, Whooley MA. Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Psychosom Med. 2007;69:735-739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 186] [Cited by in RCA: 173] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 13. | Duivis HE, Kupper N, Penninx BW, Na B, de Jonge P, Whooley MA. Depressive symptoms and white blood cell count in coronary heart disease patients: prospective findings from the Heart and Soul Study. Psychoneuroendocrinology. 2013;38:479-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Williams MS, Rogers HL, Wang NY, Ziegelstein RC. Do platelet-derived microparticles play a role in depression, inflammation, and acute coronary syndrome? Psychosomatics. 2014;55:252-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Kuhlmann SL, Tschorn M, Arolt V, Beer K, Brandt J, Grosse L, Haverkamp W, Müller-Nordhorn J, Rieckmann N, Waltenberger J, Warnke K, Hellweg R, Ströhle A. Serum brain-derived neurotrophic factor and stability of depressive symptoms in coronary heart disease patients: A prospective study. Psychoneuroendocrinology. 2017;77:196-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53:897-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 496] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 17. | Klug G, Metzler B. Assessing myocardial recovery following ST-segment elevation myocardial infarction: short- and long-term perspectives using cardiovascular magnetic resonance. Expert Rev CardiovascTher. 2013;11:203-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Ahmed N, Carrick D, Layland J, Oldroyd KG, Berry C. The role of cardiac magnetic resonance imaging (MRI) in acute myocardial infarction (AMI). Heart Lung Circ. 2013;22:243-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Wu E, Ortiz JT, Tejedor P, Lee DC, Bucciarelli-Ducci C, Kansal P, Carr JC, Holly TA, Lloyd-Jones D, Klocke FJ, Bonow RO. Infarct size by contrast enhanced cardiac magnetic resonance is a stronger predictor of outcomes than left ventricular ejection fraction or end-systolic volume index: prospective cohort study. Heart. 2008;94:730-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 330] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 20. | Wu KC, Zerhouni EA, Judd RM, Lugo-Olivieri CH, Barouch LA, Schulman SP, Blumenthal RS, Lima JA. Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation. 1998;97:765-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 985] [Cited by in RCA: 925] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 21. | de Waha S, Desch S, Eitel I, Fuernau G, Zachrau J, Leuschner A, Gutberlet M, Schuler G, Thiele H. Impact of early vs. late microvascular obstruction assessed by magnetic resonance imaging on long-term outcome after ST-elevation myocardial infarction: a comparison with traditional prognostic markers. Eur Heart J. 2010;31:2660-2668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 176] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 22. | Raman SV, Simonetti OP, Winner MW, Dickerson JA, He X, Mazzaferri EL, Ambrosio G. Cardiac magnetic resonance with edema imaging identifies myocardium at risk and predicts worse outcome in patients with non-ST-segment elevation acute coronary syndrome. J Am CollCardiol. 2010;55:2480-2488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 99] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 23. | Eitel I, Kubusch K, Strohm O, Desch S, Mikami Y, de Waha S, Gutberlet M, Schuler G, Friedrich MG, Thiele H. Prognostic value and determinants of a hypointense infarct core in T2-weighted cardiac magnetic resonance in acute reperfused ST-elevation-myocardial infarction. Circ Cardiovasc Imaging. 2011;4:354-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 163] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 24. | Mather AN, Fairbairn TA, Ball SG, Greenwood JP, Plein S. Reperfusion haemorrhage as determined by cardiovascular MRI is a predictor of adverse left ventricular remodelling and markers of late arrhythmic risk. Heart. 2011;97:453-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 123] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 25. | Eitel I, Desch S, Fuernau G, Hildebrand L, Gutberlet M, Schuler G, Thiele H. Prognostic significance and determinants of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. J Am CollCardiol. 2010;55:2470-2479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 363] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 26. | Eitel I, Desch S, de Waha S, Fuernau G, Gutberlet M, Schuler G, Thiele H. Long-term prognostic value of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. Heart. 2011;97:2038-2045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 27. | Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21545] [Cited by in RCA: 28937] [Article Influence: 1205.7] [Reference Citation Analysis (0)] |
| 28. | Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737-1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6086] [Cited by in RCA: 6847] [Article Influence: 263.3] [Reference Citation Analysis (0)] |
| 29. | Smolderen KG, Buchanan DM, Amin AA, Gosch K, Nugent K, Riggs L, Seavey G, Spertus JA. Real-world lessons from the implementation of a depression screening protocol in acute myocardial infarction patients: implications for the American Heart Association depression screening advisory. Circ Cardiovasc Qual Outcomes. 2011;4:283-292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Ren Y, Yang H, Browning C, Thomas S, Liu M. Performance of screening tools in detecting major depressive disorder among patients with coronary heart disease: a systematic review. Med SciMonit. 2015;21:646-653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Razykov I, Ziegelstein RC, Whooley MA, Thombs BD. The PHQ-9 versus the PHQ-8--is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the Heart and Soul Study. J Psychosom Res. 2012;73:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 136] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 32. | Haddad M, Walters P, Phillips R, Tsakok J, Williams P, Mann A, Tylee A. Detecting depression in patients with coronary heart disease: a diagnostic evaluation of the PHQ-9 and HADS-D in primary care, findings from the UPBEAT-UK study. PLoS One. 2013;8:e78493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 77] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 33. | DiSante JL, Bires AM, Cline TW, Waterstram-Rich K. An Analysis of the Prevalence of Depression Post-Myocardial Infarction. Crit Care Nurs Q. 2017;40:124-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Elderon L, Smolderen KG, Na B, Whooley MA. Accuracy and prognostic value of American Heart Association: recommended depression screening in patients with coronary heart disease: data from the Heart and Soul Study. Circ Cardiovasc Qual Outcomes. 2011;4:533-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 35. | Beach SR, Januzzi JL, Mastromauro CA, Healy BC, Beale EE, Celano CM, Huffman JC. Patient Health Questionnaire-9 score and adverse cardiac outcomes in patients hospitalized for acute cardiac disease. J Psychosom Res. 2013;75:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7073] [Cited by in RCA: 6652] [Article Influence: 950.3] [Reference Citation Analysis (0)] |
| 37. | O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol. 2013;61:485-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 481] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 38. | Laghrissi-Thode F, Wagner WR, Pollock BG, Johnson PC, Finkel MS. Elevated platelet factor 4 and beta-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biol Psychiatry. 1997;42:290-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 225] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 39. | Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007;357:2482-2494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1519] [Cited by in RCA: 1570] [Article Influence: 87.2] [Reference Citation Analysis (0)] |
| 40. | De Caterina R, D'Ugo E, Libby P. Inflammation and thrombosis - testing the hypothesis with anti-inflammatory drug trials. ThrombHaemost. 2016;116:1012-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |