Published online Apr 6, 2020. doi: 10.12998/wjcc.v8.i7.1223
Peer-review started: December 29, 2019
First decision: January 19, 2020
Revised: March 12, 2020
Accepted: March 19, 2020
Article in press: March 19, 2020
Published online: April 6, 2020
Processing time: 98 Days and 23.7 Hours
Paprosky type IIIB acetabular bone defects are very difficult to reconstruct. For severe defects, we developed our own cup-on-cup technique. We defined the tantalum metal (TM) revision shell with the peripheral titanium ring removed as a TM-cup augment and the cementless hemispherical acetabulum component combined with a TM-cup augment as the cup-on-cup technique.
To report the short-term results of patients with type IIIB acetabular bone defects reconstructed using the cup-on-cup technique.
We retrospectively reviewed six patients (six hips) with a mean age of 59 years who underwent acetabular reconstruction using our cup-on-cup technique between January 2015 and January 2017. All acetabular bone defects were classified as type IIIB without pelvic discontinuity using the system of Paprosky. All patients were followed both clinically and radiographically for a mean duration of 42 mo.
The mean Harris hip score improved from 32.4 pre-operatively to 80.7 at the last follow-up. The mean vertical position of the hip rotation centre changed from 60.9 mm pre-operatively to 31.7 mm post-operatively, and the mean horizontal position changed from 33.6 mm pre-operatively to 38.9 mm post-operatively. Greater trochanteric migration after extended trochanteric osteotomy occurred in one of six hips at 3 mo. There was no evidence of component migration at the last follow-up.
The short-term results suggest that our cup-on-cup technique could be considered an effective management option for Paprosky type IIIB acetabular bone defects without pelvic discontinuity.
Core tip: Paprosky type IIIB acetabular bone defects are very difficult to reconstruct. We developed our own cup-on-cup technique. We defined the tantalum metal (TM) revision shell with the peripheral titanium ring removed as a TM-cup augment and the cementless hemispherical acetabulum component combined with a TM-cup augment as the cup-on-cup technique. The short-term results suggest that our cup-on-cup technique could be considered an effective management option for Paprosky type IIIB acetabular bone defects without pelvic discontinuity.
- Citation: Du YQ, Liu YP, Sun JY, Ni M, Zhou YG. Reconstruction of Paprosky type IIIB acetabular bone defects using a cup-on-cup technique: A surgical technique and case series. World J Clin Cases 2020; 8(7): 1223-1231
- URL: https://www.wjgnet.com/2307-8960/full/v8/i7/1223.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i7.1223
Acetabular bone defects are becoming more common in revision total hip arthroplasty (THA). The reconstruction of the defects may be a surgical challenge. Several classification systems have described acetabular bone defects, but the most helpful for developing surgical strategies is the Paprosky classification[1,2]. Paprosky type IIIB defects are defined as “up and out” defects with more than 60% of the acetabular rim compromised and superomedial migration of femoral head greater than 3 cm[1].
For the reconstruction of the defects, structural allograft has been used to initially stabilise the cementless hemispherical acetabular component in the past decades[3,4]. However, due to the collapse, resorption, nonunion, loosening, and infection of the grafts, the cementless acetabular component that lacked successful biological fixation and bone graft incorporation became susceptible to loosening. The success rate of structural allografts was approximately 65% in a series of systematic reviews of the literature[3-7]. The common causes of failures were as described above[3,6,7].
To solve the above problems, “nonresorptive structural allografts”, namely, trabecular metal (Zimmer, Warsaw, IN) augments, have been widely used during the past decade[8-12]. With high frictional characteristics, low modulus of elasticity, and high volumetric porosity (70% to 80%), the acetabular component and augment posses high bone ingrowth potential and can obtain long-term biological fixation[12-14]. Therefore, multiple sizes and shapes of the acetabular augments have emerged to adapt and reconstruct various acetabular bone defects. Hemispheric acetabular components with trabecular metal augments have been reported by many authors to be associated with excellent clinical results, such as acceptable postoperative hip function, low rates of aseptic loosening and other complications during mean follow-up periods ranging from 37 to 60 mo[9-11].
Many surgeons have utilized two trabecular metal augments to reconstruct the superomedial type IIIB defects. However, the two largest trabecular metal augments cannot reconstruct the defects or restore the normal hip centre of rotation (COR) because the defects are too large. For the sake of solving the problem, we utilized a cup-on-cup technique to reconstruct the Paprosky type IIIB acetabulum bone defects and restore the normal hip COR. We defined the tantalum metal (TM) revision shell that was removed from the peripheral titanium ring as a TM-cup augment and the cementless hemispherical acetabulum component combined with a TM-cup augment as the cup-on-cup technique.
The purpose of this study was to report the short-term results of patients with type IIIB acetabulum bone defects reconstructed using our cup-on-cup technique.
We retrospectively reviewed six patients (six hips) who underwent acetabular reconstruction for Paprosky type IIIB acetabular bone defects using our cup-on-cup technique from January 2015 to January 2017 (Table 1). There were four females and two males with a mean age of 59 years (range from 29 to 73 years). The causes of revision surgery were aseptic loosening in five hips and a primary THA with severe defects because of posttraumatic acetabular comminuted fracture and infection in one hip. None of the participants had pelvic discontinuity. All patients were followed clinically and radiographically for a mean duration of 42 mo (range, 36 to 52 mo). No patients were reported as lost to either clinical or radiographic follow-up.
| Patient | Age (yr) | Gender | Height (cm) | Weight (kg) | Initial diagnosis | Prior surgeries |
| 1 | 73 | F | 157 | 53 | Femoral neck fracture, Lt. | 2014 THA |
| 2 | 57 | F | 152 | 73 | Osteonecrosis, Lt. | 2006 THA |
| 3 | 29 | M | 180 | 98 | Posttraumatic acetabular comminuted fracture, Lt. | September 21, 2012 internal fixation, September 29, 2012 debridement × 3 (September 2012; October 2012; September 2014), January 2015 debridement + antibiotic-PMMA beads |
| 4 | 60 | F | 160 | 65 | Osteonecrosis, Lt. | 2002 THA |
| 5 | 67 | M | 178 | 82 | Osteoarthritis, Rt. | 2005 THA |
| 6 | 69 | F | 157 | 69 | Osteoarthritis, Rt. | 2009 THA |
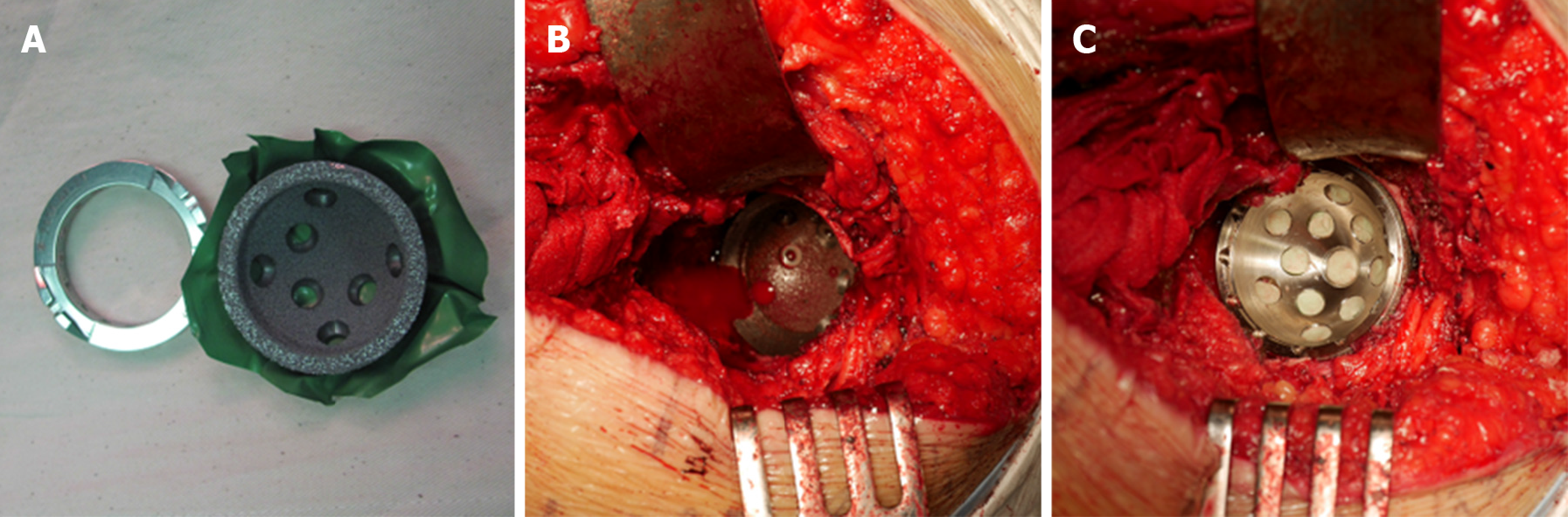
All surgeries were performed by one author (Zhou YG) at the General Hospital of the Chinese People’s Liberation Army (Beijing, China). The classification of these defects was based on pre-operative standard radiographs and computed tomography of the acetabulum and intra-operative assessment according to the Paprosky classification[1]. A standard posterior-lateral approach was used for each case. Extended trochanteric osteotomies (ETOs) were performed in two hips to remove the failed components, improve exposure, and assist in the balancing of soft tissue. Acetabular reconstruction began by removing the failed acetabular components, bone cement, and any fibre-necrotic tissue. The superomedial defects in conformity with Paprosky type IIIB were detected in six hips. Conventional hemispherical reamers of different diameters were used to detect the defects’ shape and size; the latter were constrained by the anterior and posterior acetabular walls. Then, a TM revision shell removed from the peripheral titanium ring (TM-cup augment) was inserted into the shaped defects, and the TM-cup augment with pressfit was stabilised and secured against the host bone with the screws that were placed according to the bone mass around the acetabulum. Next, hemispherical reamers of different diameters were used again to shape the acetabulum by reaming the bone at the periphery of the acetabulum and the periphery of the TM-cup augment rim. Until the size of the reamer was constrained by the acetabular walls and the augment or a stable 3-point fixation was achieved by the ischium and the augment[15], a cementless hemispherical acetabulum component (a Pinnacle or trabecular metal revision component) was inserted. The cement was only placed between the TM-cup augment and the hemispherical acetabulum component, and the rest of the surface of the cementless acetabular component was covered with the host acetabular bone (Figure 1). Additional screws were inserted into the acetabular bone through the holes in the acetabular component to enhance the initial stability. In four of the six cases, additional screws were inserted though both the acetabular component and the TM-cup augment into the ilium to further enhance fixation. To do this, we needed to create additional screw holes in the TM revision shell or the TM-cup augment with a high-speed burr.
The mean diameter of the TM-cup augment was approximately 50 mm (range from 48 to 52 mm). The Pinnacle acetabular cup was used in three hips, and the TM revision shell was used another three hips. The mean diameter of the Pinnacle acetabular cup was approximately 57 mm (range from 54 to 60 mm), and the TM revision shell was approximately 57 mm (range from 56 to 58 mm). A mean of four bone screws (range from 3 to 5) were used for each acetabular reconstruction, with a median of two screws inserted through the acetabular component (range from 1 to 3) and a median of two screws inserted through the TM-cup augment (range from 1 to 3).
Once the acetabular component and augment were secured, a liner was implanted into the acetabular component. A highly cross-linked polyethylene liner was used in five hips, and a ceramic liner was used in one hip. The femoral head size was 32 mm in one hip and 36 mm in five hips (Table 2).
| Patient | TM-Cup augment diameter (mm) | Acetabular component | Total number of screws | Liner | Femoral head diameter (mm) |
| 1 | 48 | 54 mm Pinnacle | 3 | HXLPE | 36 |
| 2 | 52 | 58 mm Pinnacle | 3 | Ceramic | 36 |
| 3 | 48 | 58 mm TM revision shell | 5 | HXLPE | 36 |
| 4 | 50 | 56 mm TM revision shell | 4 | HXLPE | 32 |
| 5 | 52 | 60 mm Pinnacle | 4 | HXLPE | 36 |
| 6 | 48 | 58 mm TM revision shell | 5 | HXLPE | 36 |
Postoperative recovery included partial weight bearing with the use of crutches for the first six weeks. Full weight bearing was allowed thereafter. The patients stayed in the hospital for a mean of 8.7 d (range from 7 to 10 d).
Clinical and radiological evaluations were performed pre-operatively; at 3 mo, 6 mo, and 1 year postoperatively; and annually thereafter. The functional results of the arthroplasty were recorded according to the Harris hip score[16]. A case was considered a clinical failure if the component was revised again or if the clinical score was worse than the pre-operative score.
Standard radiological analysis was performed on serial anteroposterior radiographs of the pelvis and lateral views of the operated hip. The vertical position of the hip COR was measured from the inter-tear drop line to the centre of the femoral head, and the horizontal position was measured between the femoral head centre and the perpendicular line from the inter-tear drop line at the tear drop[17].
The presence and evolution of radiolucent lines in the three zones of DeLee et al[18] were recorded. The component was considered unstable if a radiolucent line at least 1 mm wide crossed all three acetabular zones or if any component migration could be found. The fibrous stability of the component was characterized by a radiolucent line less than 1 mm wide that crossed two of the three zones, while the component was considered stable with the presence of bone ingrowth if the component was in close contact with the pelvic bone and no radiolucent lines were found in at least two of the three zones[19]. Radiologically, a change in the abduction angle of the acetabular component of more than 10° or a change in the vertical or horizontal position of the component > 6 mm were defined as loosening[9]. The presence of osseointegration was evaluated according to the Moore criteria[20]. Five radiographic signs were used: Absence of radiolucent lines, presence of superolateral support, medial stress-shielding, radial trabeculae, and inferomedial support. When three or more signs were present, the positive predictive value of the radiographic test was 96.9%, the sensitivity was 89.6%, and the specificity was 76.9%.
The Ethics Committee of the General Hospital of Chinese People’s Liberation Army approved the study protocol. All study participants provided written informed consent for the study.
The mean Harris hip score improved from 32.4 ± 10.1 (range from 19.8 to 50.2) pre-operatively to 80.7 ± 5.6 (range from 71.5 to 87.5) at the last follow-up. Pre-operatively, five patients had severe pain, and one had moderate pain. At the last follow-up, four patients had no pain, and two had slight pain. Pre-operatively, three patients needed a cane for long walks and three needed full-time support with crutches. At the last follow-up, all six patients could walk unaided. Pre-operatively, five patients had a severe limp, and one had a moderate limp. At the last follow-up, five patients had no limp and one had a moderate limp.
The mean vertical position of the hip COR from the inter-teardrop line changed from 60.9 ± 7.5 mm (range from 50.8 to 70.2 mm) pre-operatively to 31.7 ± 8.8 mm (range from 25.2 to 49.3 mm) postoperatively. Postoperatively, the vertical position of five patients was less than 35.0 mm and that of one was 49.3 mm. The mean horizontal position of the COR from the teardrop changed from 33.6 ± 5.0 mm (range from 28.5 to 39.5 mm) pre-operatively to 38.9 ± 5.0 mm (range from 32.7 to 47.8 mm) postoperatively.
At the last follow-up, there was no evidence of component migration compared to the initial postoperative views. A radiolucent line was noted in one of the six hips, and in this case, there was a radiolucent line smaller than 1 mm seen in zone C 3 mo after surgery. However, the radiolucent line remained stable, and no further progression was noted at the last follow-up. All the acetabular domes presented at least three or more signs of fixation, in accordance with the criteria of Moore (Figure 2).
Greater trochanteric migration after ETO occurred in one of six hips at 3 mo. The patient had a moderate limp, but she was quite satisfied with the current condition and did not expect for a surgery to fix the migrated greater trochanter.
There were no cases of deep infection, deep venous thrombosis, nerve injuries, pulmonary embolism, or death as a result of the revision procedure.
Management of Paprosky type IIIB acetabulum bone defects is a challenging and unique reconstructive procedure. Superomedial defects are very common in revision THA. To address this problem, we used our own cup-on-cup technique with a cementless hemispherical acetabulum component and a tantalum metal revision shell as a TM-cup augment. The TM-cup augment was implanted to reconstruct the superomedial defects, and then the hemispherical acetabulum component was implanted into the reconstructed acetabulum.
The TM augment was first introduced in 1997 and possesses a high coefficient of friction and porosity[14]. Moreover, TM offers good bioactive and biological bonds to host bone, and its characteristics include a high volumetric porosity, which appears optimal for bone ingrowth, and a roughened surface micro-texture that provides a scratch fit for increased initial stability upon implantation[21]. All the above properties of TM are why it is increasingly used in revision THA with severe acetabular bone defects. Recently, many short-term reports have shown encouraging results from using TM augments in type III acetabular defects (Table 3). Del Gaizo et al[10] reported that only one of 37 hips (2.7%) failed as a result of aseptic loosening during a mean follow-up period of 60 mo (range from 26 to 106 mo). Grappiolo et al[11] reviewed 55 acetabular revisions with a mean follow-up period of 53.7 mo (range from 36 to 91 mo) and reported three cases of revision for aseptic loosening (5.5%). Lingaraj et al[8] and Sporer et al[9] reported no aseptic loosening in their studies. Moreover, recurrent instability was very common in revisions[8-11].
| Ref. | Number and Paprosky type | Reconstruction technique for defects | Mean follow-up | Mean postoperative hip score | Failure resulting from aseptic loosening | Other complications requiring reoperation |
| Lingaraj et al[8] | 17 IIIA, 6 IIIB without pelvic discontinuity | 21 TM shell-augment; 1 TM shell alone; 1 acetabular component-cage | 41 mo (range, 24 to 62) | Harris hip score 75.7 (range, 53 to 100) | 0 | 2 recurrent instability, 1 early infection with irrigation and debridement |
| Sporer et al[9] | 28 IIIA | The TM shell-augment in all cases | 3.1 yr (range, 1 to 4 ) | The modified Merle d’Aubigne and postel score 10.6 | 0 | 1 recurrent instability |
| Del Gaizo et al[10] | 37 IIIA | The TM shell-augment in all cases | 60 mo (range, 26 to 106) | Harris hip score 81.5 (range, 27.0 to 99.8) | 1 (2.7%) | 5 recurrent instability, 4 infection with irrigation and debridement, 2 periprosthetic femoral fracture |
| Grappiolo et al[11] | 42 IIIA, 13 IIIB without pelvic discontinuity | The TM shell-augment in all cases | 53.7 mo (range, 36 to 91) | Harris hip score 90.5 (range, 61 to 100) | 3 (5.5%) | 1 recurrent instability |
| Current study | 6 IIIB without pelvic discontinuity | The cementless acetabulum component and TM-Cup augment in all cases | 42 mo (range, 36 to 52) | Harris hip score 80.7 (range, 71.5 to 87.5) | 0 | 1 greater trochanteric migration |
In our practice, we strived to restore the anatomical position of the hip COR to achieve effective functioning of the abductors. During the surgical procedure, in the presence of severe superior and medial migration of the hip COR, we utilized the TM-cup augment to reconstruct the superomedial defects and restored the normal position of the hip COR. The level of the hip COR was normal in five patients; we could not restore a normal hip COR in one patient due to the large superior defects. Finally, despite the large and severe size of the defects, we were able to use a medium cup size in all patients. Avoiding using jumbo-cup could also prevent impingement between the acetabular construction and soft tissue around the hip[22].
In our study, we included patients with Paprosky type IIIB acetabulum bone defects without pelvic discontinuity. During a mean follow-up period of 42 mo (range from 36 to 52 mo), none of the six hips treated using our cup-on-cup technique failed due to aseptic loosening, and only one case had greater trochanteric migration after ETO. Our cup-on-cup technique with a fluted and tapered modular stem was used in five patients, and a primary femoral prosthesis was used on one patient; none of the patients had recurrent instability.
Sheth et al[23]and Paprosky et al[1] recommended removing the peripheral titanium ring to facilitate the placement of screw holes at the periphery of a TM revision shell and gained screw access to the ischium and/or superior public ramus. We regarded the TM revision shell with a removed peripheral titanium ring as a TM-cup augment. We utilized the TM-cup augment to reconstruct the large type IIIB superomedial defects and made additional screw holes in it with a high-speed burr. Blumenfeld et al[24] described a cup-in-cup technique in which a large tantalum acetabular shell was placed onto supportive host bone in a cementless fashion and a smaller shell was cemented into the larger one, using the technique to restore offset in severe acetabular defects[24]. There was no evidence of loosening or migration during an average follow-up period of 28 mo (range from 12 to 50 mo). Based on the aforementioned report, we developed our cup-on-cup technique to reconstruct the type IIIB acetabulum bone defects. A smaller cup rode on the superomedial region of a larger one, instead of smaller cup, was implanted into the larger one (cup-in-cup technique). The larger cup was put into the true acetabular region, which make it possible that the large head was used in the revision THA.
The cup-on-cup technique achieved better clinical results in our study, but two concerns existed with this technique. One was the TM particulates that were caused by reaming the TM-cup augment rim, which may have an effect on the friction interface and may result in the increasing wear of the highly cross-linked polyethylene liner. During the surgical procedure, we used copious physiological sodium chloride solution to repeatedly wash off the particulates to minimize the damage. The other concern was the durability of the cementation between the augment and the acetabular component. We used a screw to fix the augment and acetabular component by making additional screw holes in the acetabular component or the TM-cup augment, which may prevent the failure of the cementation.
Additionally, cost may be a factor in the reconstruction of severe bone defects. The cost of the cup-on-cup technique was lower than that of using two conventional TM augments to reconstruct severe superomedial defects in China.
We acknowledge the limitations of our study. The first limitation is the retrospective design. Ideally, a randomized controlled trial should be performed comparing this type of reconstruction with other techniques, such as a structural allograft. Second, there was a very small number of patients in our study. Third, the follow-up duration was short, and further results are unknown.
In conclusion, we judge our cup-on-cup technique to be an excellent choice to reconstruct severe superomedial defects and restore the level of the normal hip center of rotation. We will continue to use the technique and follow the patients to obtain long-term clinical results.
Acetabular bone defects are becoming more common in revision total hip arthroplasty. The reconstruction of the defects may be a surgical challenge. For the reconstruction of the defects, structural allograft has been used to initially stabilise the cementless hemispherical acetabular component in the past decades. However, due to the collapse, resorption, nonunion, loosening, and infection of the grafts, the cementless acetabular component that lacked successful biological fixation and bone graft incorporation became susceptible to loosening. The success rate of structural allografts was approximately 65% in a series of systematic reviews of the literature.
Trabecular metal with high frictional characteristics, low modulus of elasticity, and high volumetric porosity (70% to 80%) has been widely used to reconstruct the defects during the past decade. Hemispheric acetabular components with trabecular metal augments have been reported by many authors to be associated with excellent clinical results. Many surgeons have utilized two trabecular metal augments to reconstruct the superomedial type IIIB defects. However, the two largest trabecular metal augments cannot reconstruct the defects or restore the normal hip centre of rotation because the defects are too large. For the sake of solving the problem, we utilized a cup-on-cup technique to reconstruct the Paprosky type IIIB acetabulum bone defects and restore the normal hip centre of rotation.
The main objective of this study was to report the short-term results of patients with Paprosky type IIIB acetabular bone defects reconstructed using the cup-on-cup technique.
Six patients (six hips) with a mean age of 59 years who underwent acetabular reconstruction using our cup-on-cup technique between January 2015 and January 2017 were retrospectively reviewed. All patients were followed both clinically and radiographically.
The mean Harris hip score improved from 32.4 pre-operatively to 80.7 at the last follow-up. Greater trochanteric migration after extended trochanteric osteotomy occurred in one of six hips at 3 mo. There was no evidence of component migration at the last follow-up.
We present the clinical and radiographical results of six patients with type IIIB acetabular bone defects. The short-term results suggest that our cup-on-cup technique could be considered an effective management option for Paprosky type IIIB acetabular bone defects without pelvic discontinuity.
Due to the retrospective nature of this study and the small sample, it is difficult to obtain reliable conclusions. However, our study provides a new surgical technique to reconstruct the Paprosky type IIIB acetabulum bone defects.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coban YK, Widmer KH S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 793] [Cited by in RCA: 770] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 2. | Sheth NP, Nelson CL, Springer BD, Fehring TK, Paprosky WG. Acetabular bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2013;21:128-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 3. | Brown NM, Morrison J, Sporer SM, Paprosky WG. The Use of Structural Distal Femoral Allograft for Acetabular Reconstruction of Paprosky Type IIIA Defects at a Mean 21 Years of Follow-Up. J Arthroplasty. 2016;31:680-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Sporer SM, O'Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction. Average ten-year follow-up. J Bone Joint Surg Am. 2005;87:760-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Gill TJ, Sledge JB, Müller ME. The management of severe acetabular bone loss using structural allograft and acetabular reinforcement devices. J Arthroplasty. 2000;15:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Garbuz D, Morsi E, Gross AE. Revision of the acetabular component of a total hip arthroplasty with a massive structural allograft. Study with a minimum five-year follow-up. J Bone Joint Surg Am. 1996;78:693-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | Piriou P, Sagnet F, Norton MR, de Loubresse CG, Judet T. Acetabular component revision with frozen massive structural pelvic allograft: average 5-year follow-up. J Arthroplasty. 2003;18:562-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Lingaraj K, Teo YH, Bergman N. The management of severe acetabular bone defects in revision hip arthroplasty using modular porous metal components. J Bone Joint Surg Br. 2009;91:1555-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Sporer SM, Paprosky WG. The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty. 2006;21:83-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 139] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 10. | Del Gaizo DJ, Kancherla V, Sporer SM, Paprosky WG. Tantalum augments for Paprosky IIIA defects remain stable at midterm followup. Clin Orthop Relat Res. 2012;470:395-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Grappiolo G, Loppini M, Longo UG, Traverso F, Mazziotta G, Denaro V. Trabecular Metal Augments for the Management of Paprosky Type III Defects Without Pelvic Discontinuity. J Arthroplasty. 2015;30:1024-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 132] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | Levine B, Della Valle CJ, Jacobs JJ. Applications of porous tantalum in total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:646-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 95] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 453] [Reference Citation Analysis (0)] |
| 15. | Gustke KA, Levering MF, Miranda MA. Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty. 2014;29:199-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Sporer SM, Paprosky WG. Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty. 2006;21:87-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 113] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 18. | DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;20-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 212] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | Moore MS, McAuley JP, Young AM, Engh CA Sr. Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res. 2006;444:176-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 165] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 21. | Long WJ, Noiseux NO, Mabry TM, Hanssen AD, Lewallen DG. Uncemented Porous Tantalum Acetabular Components: Early Follow-Up and Failures in 599 Revision Total Hip Arthroplasties. Iowa Orthop J. 2015;35:108-113. [PubMed] |
| 22. | Dora C, Houweling M, Koch P, Sierra RJ. Iliopsoas impingement after total hip replacement: the results of non-operative management, tenotomy or acetabular revision. J Bone Joint Surg Br. 2007;89:1031-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 146] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 23. | Sheth NP, Melnic CM, Paprosky WG. Acetabular distraction: an alternative for severe acetabular bone loss and chronic pelvic discontinuity. Bone Joint J. 2014;96-B:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Blumenfeld TJ, Bargar WL. Surgical technique: a cup-in-cup technique to restore offset in severe protrusio acetabular defects. Clin Orthop Relat Res. 2012;470:435-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |