Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.798
Peer-review started: December 10, 2019
First decision: December 30, 2019
Revised: January 7, 2020
Accepted: January 11, 2020
Article in press: January 11, 2020
Published online: February 26, 2020
Processing time: 78 Days and 9.3 Hours
Mesenteric phlebosclerosis (MP) is a rare disease of the colon. The clinical manifestations of this disease are nonspecific and it may easily be misdiagnosed. We report a case of MP with amyloidosis in the colonic vessel walls in a patient with hypertension who had been consuming Chinese medicinal liquor for 10 years. We also review the relevant literature and summarize the characteristics of MP in patients in mainland China.
A 64-year-old man was referred to our department from his primary hospital because of abdominal pain, diarrhea, and fever for almost 10 d. Computed tomography showed colon wall thickening, with threadlike calcifications in the mesenteric vein in the transverse colon. Colonoscopy revealed purple-blue mucosa with multiple ulcers in the ascending and transverse colon. Biopsy showed thickening and calcification of the vein walls, perivascular and mucosal collagen degeneration, and amyloidosis. The patient had been consuming Chinese medicinal liquor, mainly that made from gardenia fruit, for 10 years. Based on these results, a diagnosis of MP with amyloidosis was made. After conservative treatment, the patient’s discomfort subsided and he was followed closely. The use of Chinese herbal medicine was suspected to play a role in the pathogenesis of MP.
The clinical manifestations of MP are nonspecific. Recognition of its typical imaging findings, including multiple calcifications on computed tomography and purple-blue mucosal discoloration on colonoscopy, is vital.
Core tip: Mesenteric phlebosclerosis is a rare disease of the colon, characterized by calcification of the mesenteric vein and thickening of the right hemicolon wall, with fibrosis and hyalinization. Mesenteric phlebosclerosis is difficult to diagnose because its etiology and pathophysiology are unclear, and many patients are asymptomatic or present with atypical symptoms. Herein, we report a case of mesenteric phlebosclerosis with amyloidosis in the colonic vessel walls in a 64-year-old man with hypertension who had been consuming Chinese medicinal liquor for 10 years.
- Citation: Hu YB, Hu ML, Ding J, Wang QY, Yang XY. Mesenteric phlebosclerosis with amyloidosis in association with the long-term use of medicinal liquor: A case report. World J Clin Cases 2020; 8(4): 798-805
- URL: https://www.wjgnet.com/2307-8960/full/v8/i4/798.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i4.798
Mesenteric phlebosclerosis (MP) is a rare disease of the colon, characterized by calcification of the mesenteric vein and thickening of the right hemicolon wall, with fibrosis and hyalinization[1,2]. It is considered to be a form of ischemic colitis, characterized by noninflammatory, nonthrombotic stenosis or occlusion of the mesenteric veins[3]. MP is difficult to diagnose because its etiology and pathophysiology are unclear, and many patients are asymptomatic or present with atypical symptoms. Previous studies have suggested that the disease is related to diabetes mellitus, hemodialysis, toxins, or portal hypertension, and likely associated with the use of Chinese herbal medicine[4,5]. Herein, we report a case of MP with amyloidosis in the colonic vessel walls in a 64-year-old man with hypertension who had been consuming Chinese medicinal liquor for 10 years.
In August 2016, a 64-year-old male patient presented to our department with the chief complaints of persistent, mild lower abdominal pain, diarrhea, and fever for more than 10 d.
The patient’s maximum body temperature was 39.8 °C. He was diagnosed with infective diarrhea by a local doctor and transferred to our hospital department.
The patient denied any notable medical history, except hypertension.
The patient stated that he had a history of drinking and smoking for 10 years.
At presentation, the patient’s body temperature was 37.1 °C. His heart rate was 72 beats/min. His respiratory rate was 20 breaths/min, and his blood pressure was 121/74 mmHg. His abdomen was soft and flat, with no tenderness.
Laboratory tests yielded the following results: Hemoglobin, 116 g/L; C-reactive protein, 99.3 mg/L; erythrocyte sedimentation rate, 73 mm/h; 24-h urinary protein, 0.21 g; and normal levels of blood urea nitrogen (1.98 mmol/L) and creatinine (70 µmol/L). The serum and urinary β2-microglobulin concentrations were 0.62 mg/dL and 2.31 mg/dL, respectively. The urinary kappa and lambda light chain concentrations were 10 mg/dL and 5.21 mg/dL, respectively. A fecal occult blood test was positive. All other laboratory parameters were within normal limits.
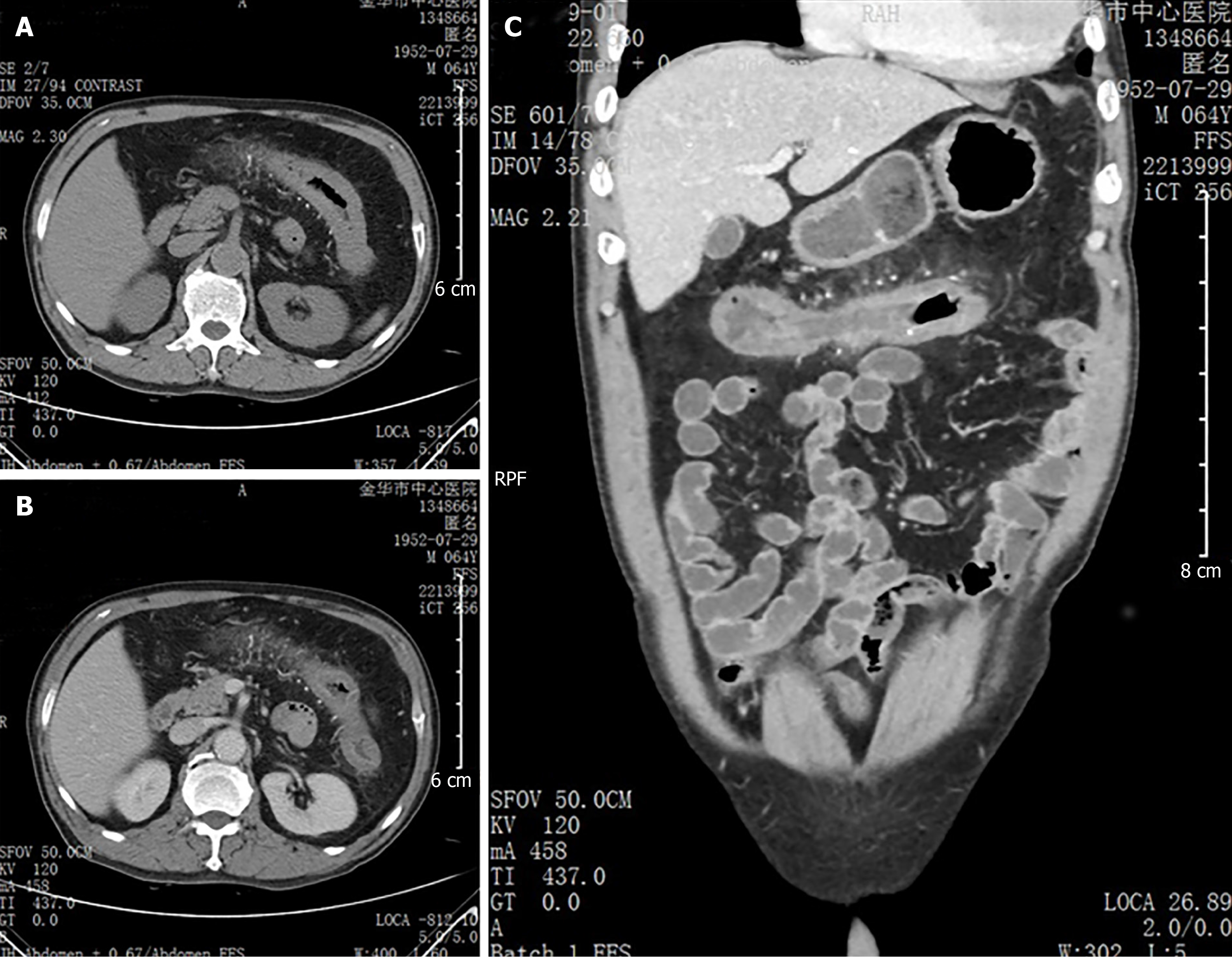
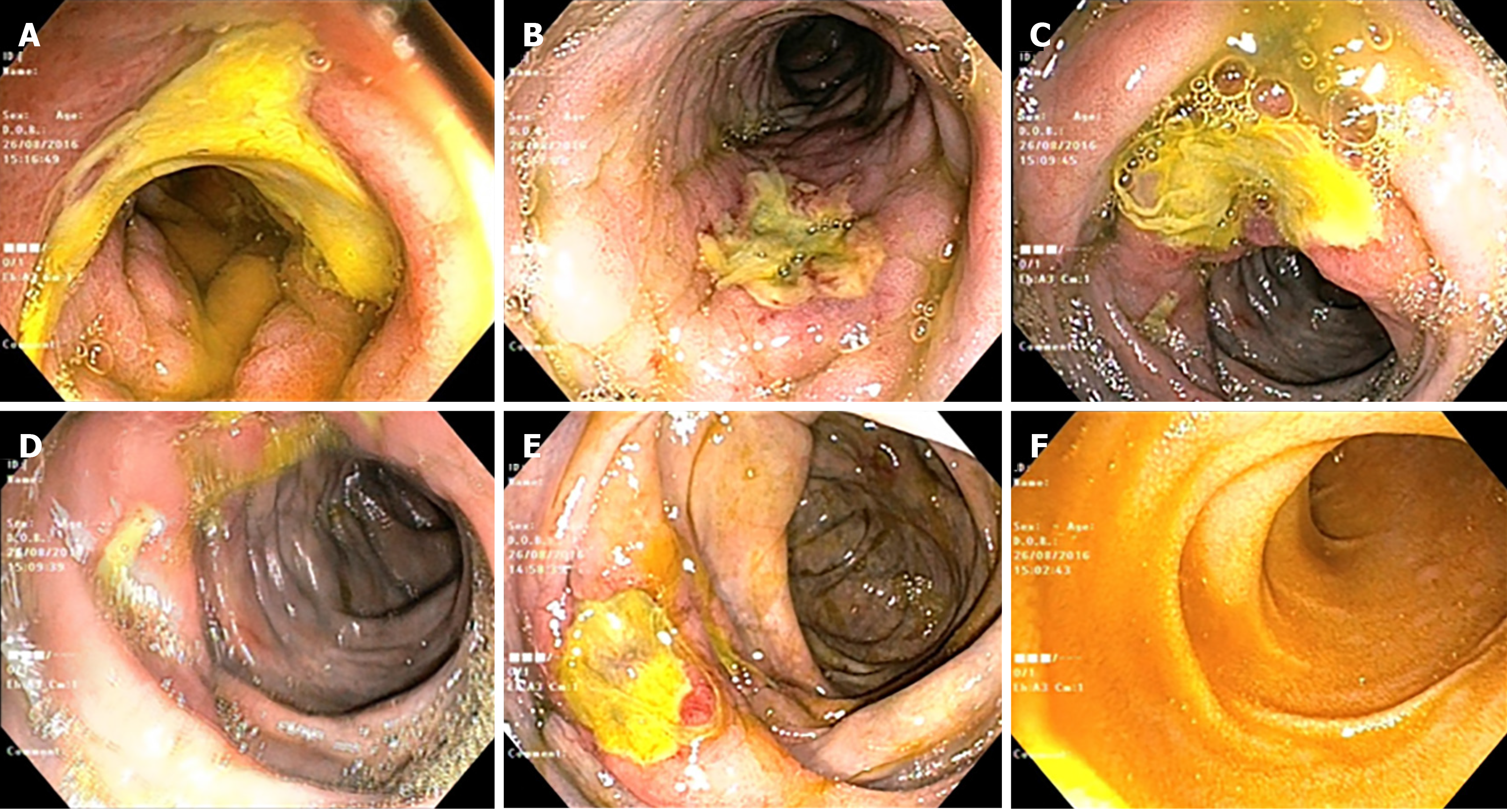
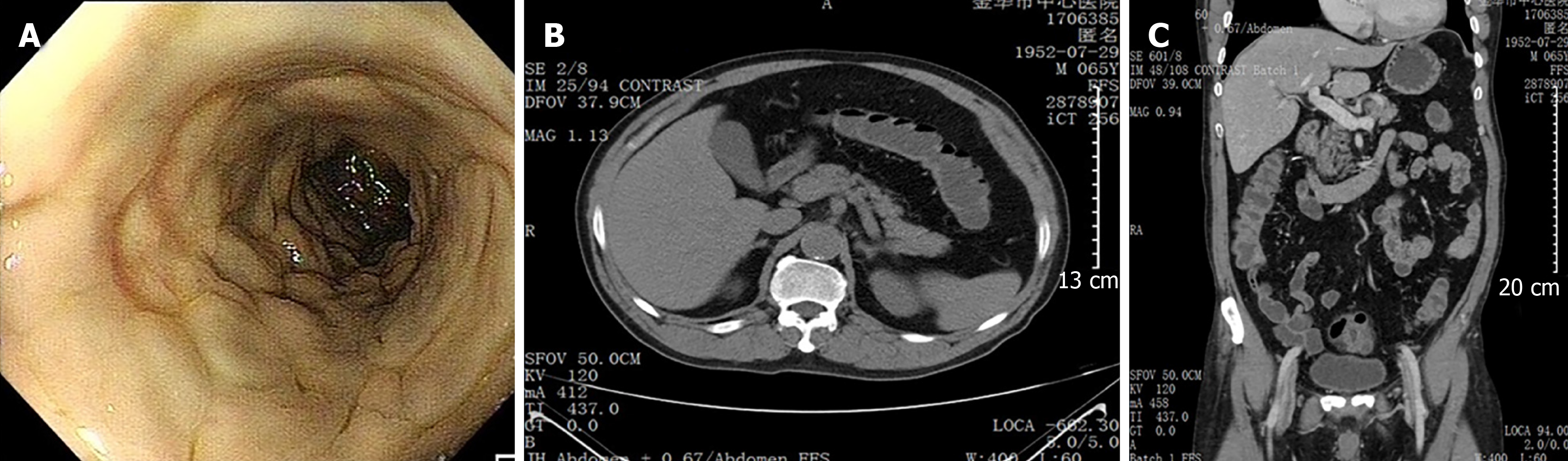
Abdominal computed tomography (CT) showed thickening of the colonic wall, with threadlike calcifications of the mesenteric vein in the transverse colon (Figure 1). No obvious obstruction point was observed. A subsequent colonoscopy revealed purple-blue mucosa extending from the ascending colon to the transverse colon. Multiple circumferential and deep ulcers were observed along the colonic wall, with sparing of the rectum (Figure 2).
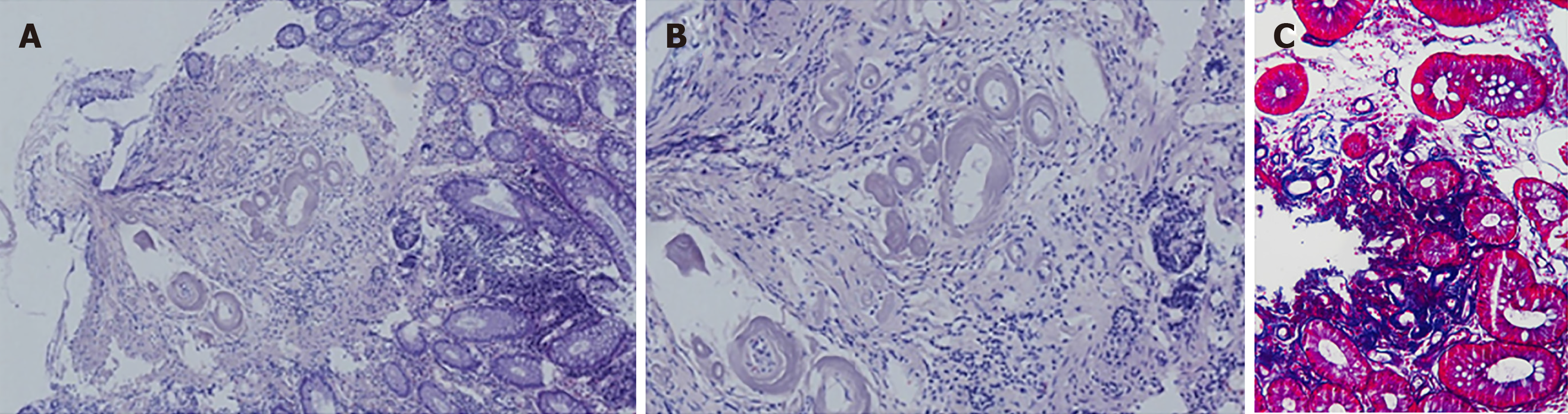
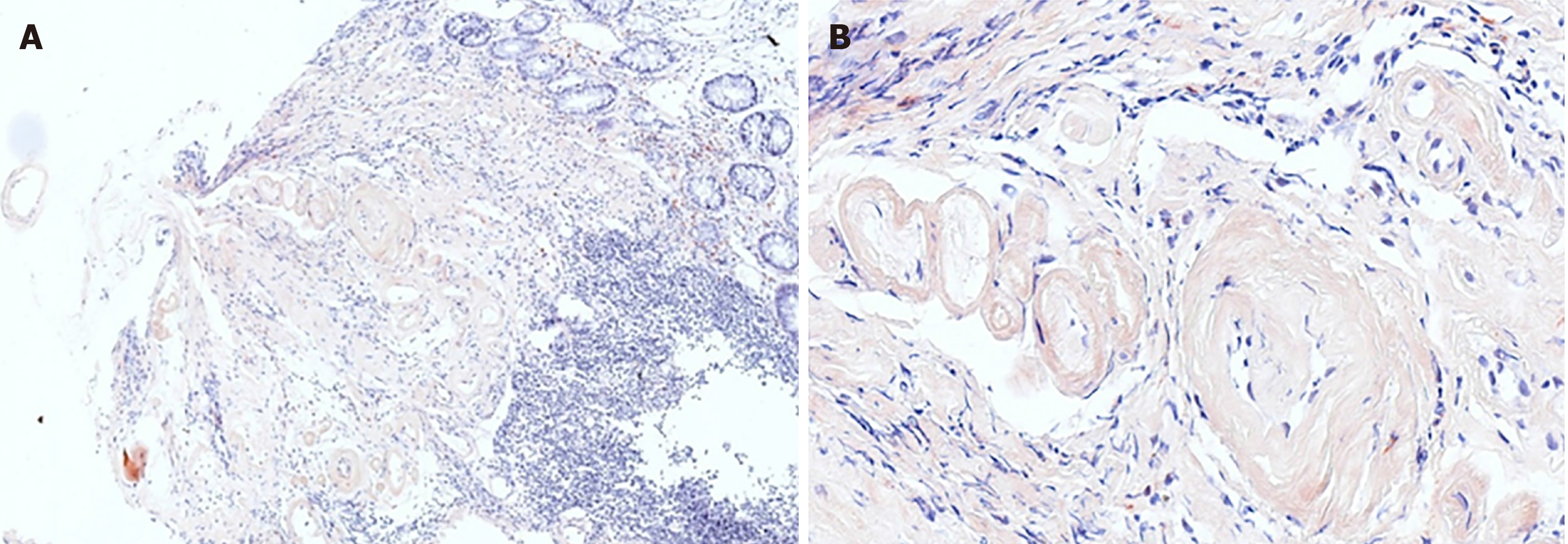
Histological examination with hematoxylin and eosin staining showed obvious thickening and calcification of the vein walls. Eosinophil infiltration of the lamina propria was also seen (Figure 3A and B). Masson trichrome staining of the biopsy material revealed dense perivascular and mucosal collagen degeneration (Figure 3C). Congo red staining highlighted amyloidosis in the venous walls (Figure 4).
Extensive anamnesis revealed that the patient had consumed Chinese medicinal liquor (nearly 100 g/d), mainly that made from gardenia fruit and containing geniposide, for 10 years. This information, combined with the clinical, radiological, endoscopic, and histological features of this case, suggested the diagnosis of MP.
We prescribed oral mesalazine (4 g/d).
The patient’s presenting symptoms were relieved 1 wk later, and he was discharged on a soft diet. He was advised to discontinue use of the Chinese medicinal liquor.
At a follow-up visit 1 mo later, routine analyses of blood parameters, liver function, renal function, and urine yielded normal findings. A follow-up colonoscopy conducted 3 mo later revealed that the ulcers had healed, but the purple-blue discoloration of the colonic mucosa persisted (Figure 5A). One year later, the colonoscopy findings remained unchanged and abdominal CT showed that the mesenteric vein calcifications had disappeared (Figure 5B and C). The patient continues to be followed in the outpatient department and has shown no symptom of recurrence to date.
Koyama et al[6] first described phlebosclerotic colitis as a form of ischemic colitis in 1991, and Iwashita et al[7] proposed it as a new disease entity in 1993. In 2000, Yao et al[8] proposed the term “phlebosclerotic colitis” to distinguish this condition from ischemic colitis caused by arterial diseases. As it is not characterized by pathological inflammation, Iwashita et al[9] proposed referring to this rare entity as idiopathic MP. Patients with MP may have no complaint, with fecal occult blood found incidentally, or they may have nonspecific signs and symptoms, such as abdominal pain, nausea, bloating, diarrhea, and obstruction[5,10]. The majority of patients are Asians, and most reported cases are from Japan[11-13]. The reported prevalence of this condition is 0.01/100000 people. The age of patients ranges from 21 to 88 years, with a male-to-female ratio of nearly 2:3[14].
To our knowledge, six cases of MP have been reported in mainland China[15-17]; the characteristics of the patients are summarized in Table 1. Two patients were female and four were male, with ages ranging from 48 to 75 years. Most of the patients reported discomfort, although their symptoms were nonspecific. Three of the six patients had histories of Chinese herbal use; data on such use were not reported for the other three patients. All cases involved the ascending and transverse colon, and the lesions progressed in the caudal direction in five cases. Calcification of the colic veins was observed in all patients. Five patients showed mucosal discoloration, primarily purple, on colonoscopy. One patient underwent surgical intervention, and three patients received conservative treatment.
| Ref. | Gender/age in yr | Chinese herbal history | Symptom (duration) | Location of lesions | Computed tomography findings | Endoscopic findings | Treatment |
| Guo et al[16] | F/62 | Yes | Abdominal pain, nausea, constipation (6 mo) | Ileocecal area, ascending colon, transverse colon | Mural thickening, calcifications of colic veins | Purple-blue mucosa | Conservative |
| Guo et al[16] | F/63 | Yes | Abdominal pain, bloating and melena diarrhea (15 mo) | Cecum to sigmoid colon | Thickened colon wall, calcifications of right, middle and left colic veins | Purple-blue mucosa, multiple ulcers | A total of colectomy with ileostomy |
| Pan et al[17] | M/48 | Yes | Stomachache, abdominal distension and constipation (mo) | Cecum to the transverse colon, sigmoid colon | Calcifications of small mesenteric veins, edematous thickening of colon wall | Dark purple edematous mucosa | NM |
| Hu et al[15] | M/57 | NM | Abdominal pain (2 wk) | Ascending, transverse, and proximaldescend-ing colon | Mural thickening, calcifications of colic wall and mesenteric vessels | Dark purple, edematous mucosa, small round ulcers | Symptomatic treatment |
| Hu et al[15] | M/56 | NM | Defecation (2 mo) | Ileocecal junction to descending colon | Calcifications of colic wall and mesenteric vein; Mural thickening | Purple mucosa, multiple ulcers | Conservative |
| Hu et al[15] | M/75 | NM | For reexamination | Ascending to descending colon | Calcifications of colic wall and mesenteric vein | Mucosal hyperemia and edema | NM |
The correct diagnosis of MP requires the observation of characteristic radiological features. Abdominal x-rays may show multiple fine, linear or threadlike calcifications, mainly in the right colon and potentially showing a gradual increase to the distal colon. CT is believed to be more valuable than plain radiography for MP screening and the follow-up of patients diagnosed with the condition[8,18]. CT is useful for the detection of colon wall thickening involving mesenteric vein calcification[15]. Many patients with multiple venous calcifications require[8,9], but such calcification may be absent in the early stage of disease[19]. Ichimata et al[20] reported two cases of early-stage MP combined with adenocarcinoma of the ascending colon. The MP was difficult to diagnose, as it was in the early stage with unclear histopathological features, and the clinicians’ attention was focused on the cancer. Hence, the authors suggested that careful observation was important for the diagnosis of early-stage MP. On colonoscopy, typical findings of MP are narrowing of the colon lumen, rigidity of the colon wall, and multiple ulcerations with purple-blue or edematous mucosa[8]. The purple-blue discoloration may be the result of chronic intestinal ischemia or the absorbance of toxins by venous return[21]. Histological features of MP include thickening and calcification of the venous walls and marked fibrous deposits in the colonic wall, without thrombus formation or hemorrhage of the mesenteric vein[18,22]. In 2019, Asayama et al[23] reported a case in which a polypoid lesion caused by MP resembled colorectal carcinoma; the diagnosis of MP should thus involve careful consideration of appearance. In the present case, CT showed threadlike calcification in the mesenteric vein and microscopic analysis revealed no thrombosis or hemorrhage.
Extensive staining analyses suggested the presence of amyloidosis of the venous walls in the present case. Amyloidosis is defined by extracellular deposition of nonbranching fibrils made up of various proteins[24]; it may be primary or secondary[25]. The former involves immunoglobulin light chains and is the more common form seen in the gastrointestinal tract[26]. The latter involves serum amyloid A protein and often affects the kidney, brain, and heart[27]. In our opinion, MP produces amyloid deposits secondarily. The role of amyloidosis in this context requires further study.
The etiology and pathogenesis of MP are not well understood. Hepatic dysfunction, diabetes, alcohol, collagen disease, and dialysis have been considered as possible causes[1,4,11]. As most cases are East Asian, a region-specific lifestyle factor may be a contributor to MP development; the use of Chinese herbal medicine was recently proposed[20,28]. The precise mechanisms underlying this association remain unclear. Hiramatsu et al[21] reported that patients with MP had histories of long-term sansis (Gardenia jasminoides) use. The main component of Gardenia jasminoides, which has been used for 3000 years, is geniposide, which may affect the colonic bacteria flora and be related to the mucosal discoloration seen in MP. Nagata et al[29] reported that patients with MP had greater intakes (total dosage > 5000 g) of gardenia fruit than did patients without MP, suggesting that the long-term intake of excessive amounts of this fruit increases the risk of MP. Hirasaki et al[30] found that the discontinuation of herbal medicines could relieve the symptoms of patients with MP. Our patient also had consumed Chinese medicinal liquor containing mainly gardenia fruit for years; he did not cease this practice but began to consume less at our recommendation.
The management of MP ranges from conservative treatment to surgery, depending on the severity of disease. Asymptomatic patients require only careful follow-up. Cases complicated by colonic obstruction, perforation, or hemorrhage may require surgical treatment. When there is no sign of bowel compromise, conservative management may be considered[7]. Several studies have indicated that the discontinuation of herbal medicines containing geniposide improves patients’ symptoms, and is associated with a relatively good prognosis[16,31]. As the patient’s condition was not severe in the present case, we provided supportive care and have followed him closely.
In conclusion, MP is a rare and potentially life-threatening disease that may easily be misdiagnosed. Because the clinical manifestations of this condition are nonspecific, the recognition of typical imaging findings, including multiple calcifications on CT and purple-blue mucosal discoloration on colonoscopy, is vital. We have presented here a case of MP with the patient’s chief complaints being fever, abdominal pain, and diarrhea. CT revealed threadlike calcifications in the mesenteric vein, and endoscopy showed multiple ulcers and purple-blue mucosa. The pathological findings indicated the presence of amyloidosis. The patient, who had a history of hypertension, had been consuming Chinese medicinal liquor for a long time. Chinese herbal medicines may be involved in the etiology of MP, so their discontinuation should be recommended to patients with the condition. More prospective studies exploring the relationship between Chinese herbal medicines and the development of MP are needed.
We are very grateful to all of the physicians, nursing staff, and other caregivers in the Gastroenterology Division at Jinhua Hospital.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A, Abenavoli L, Chiba T S-Editor: Zhang L L-Editor: Filipodia E-Editor: Ma YJ
| 1. | Kato T, Miyazaki K, Nakamura T, Tan KY, Chiba T, Konishi F. Perforated phlebosclerotic colitis--description of a case and review of this condition. Colorectal Dis. 2010;12:149-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Markos V, Kelly S, Yee WC, Davis JE, Cheifetz RE, Alsheikh A. Phlebosclerotic colitis: imaging findings of a rare entity. AJR Am J Roentgenol. 2005;184:1584-1586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Feuerstadt P, Brandt LJ. Update on Colon Ischemia: Recent Insights and Advances. Curr Gastroenterol Rep. 2015;17:45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Lee SM, Seo JW. Phlebosclerotic colitis: case report and literature review focused on the radiologic findings in relation to the intake period of toxic material. Jpn J Radiol. 2015;33:663-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Song JH, Kim JI, Jung JH, Kim JH, Lee SH, Cheung DY, Park SH, Kim JK. [A case of phlebosclerotic colitis in a hemodialysis patient]. Korean J Gastroenterol. 2012;59:40-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Koyama N, Koyama H, Hanajima T, Matsubara N, Shimada T, Fujisaki. Chromic Ischemic Colitis Causing Stenosis, Report of a case. Stomach Intestine. 1991;26:455-60. |
| 7. | Iwashita A, Takemura S, Yamada Y, Hasegawa S, Yao T, Utsunomiya T. Pathomorphologic Study on Ischemic Lesions of the Small and Large Intestine. Stomach Intestine. 1993;28:927-941. |
| 8. | Yao T, Iwashita A, Hoashi T, Matsui T, Sakurai T, Arima S, Ono H, Schlemper RJ. Phlebosclerotic colitis: value of radiography in diagnosis--report of three cases. Radiology. 2000;214:188-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 60] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Iwashita A, Yao T, Schlemper RJ, Kuwano Y, Yao T, Iida M, Matsumoto T, Kikuchi M. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003;46:209-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 10. | Oshitani N, Matsumura Y, Kono M, Tamori A, Higuchi K, Matsumoto T, Seki S, Arakawa T. Asymptomatic chronic intestinal ischemia caused by idiopathic phlebosclerosis of mesenteric vein. Dig Dis Sci. 2002;47:2711-2714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Kang HY, Noh R, Kim SM, Shin HD, Yun SY, Song IH. Phlebosclerotic colitis in a cirrhotic patient with portal hypertension: the first case in Korea. J Korean Med Sci. 2009;24:1195-1199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Tsai CC, Chou JW, Chiang IP, Lai HC, Peng CY. Mesenteric phlebosclerosis. Intern Med. 2008;47:183-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Lin PY, Chai CY, Chang CC. Recurrent abdominal pain in a 55-year-old woman. Diagnosis: Idiopathic mesenteric phlebosclerosis. Gastroenterology. 2011;141:36-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Kayano H, Nomura E, Hiraiwa S, Kuramoto T, Yatabe K, Machida T, Tajiri T, Mukai M, Makuuchi H. A Case of Idiopathic Mesenteric Phlebosclerosis with Progressive Intestinal Necrosis. Tokai J Exp Clin Med. 2016;41:70-75. [PubMed] |
| 15. | Hu P, Deng L. Phlebosclerotic colitis: three cases and literature review. Abdom Imaging. 2013;38:1220-1224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Guo F, Zhou YF, Zhang F, Yuan F, Yuan YZ, Yao WY. Idiopathic mesenteric phlebosclerosis associated with long-term use of medical liquor: two case reports and literature review. World J Gastroenterol. 2014;20:5561-5566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Pan X, Wang C. A case of phlebosclerotic colitis. Clin Res Hepatol Gastroenterol. 2015;39:651-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Chang KM. New histologic findings in idiopathic mesenteric phlebosclerosis: clues to its pathogenesis and etiology--probably ingested toxic agent-related. J Chin Med Assoc. 2007;70:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Kusanagi M, Matsui O, Kawashima H, Gabata T, Ida M, Abo H, Isse K. Phlebosclerotic colitis: imaging-pathologic correlation. AJR Am J Roentgenol. 2005;185:441-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Ichimata S, Aoyagi D, Kobayashi M, Sugihara T, Nishio A, Maruyama M, Shiozawa S. Early-stage idiopathic mesenteric phlebosclerosis incidentally combined with adenocarcinoma of the ascending colon: A report of two cases. Pathol Int. 2018;68:139-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Hiramatsu K, Sakata H, Horita Y, Orita N, Kida A, Mizukami A, Miyazawa M, Hirai S, Shimatani A, Matsuda K, Matsuda M, Ogino H, Fujinaga H, Terada I, Shimizu K, Uchiyama A, Ishizawa S, Abo H, Demachi H, Noda Y. Mesenteric phlebosclerosis associated with long-term oral intake of geniposide, an ingredient of herbal medicine. Aliment Pharmacol Ther. 2012;36:575-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Yen TS, Liu CA, Chiu NC, Chiou YY, Chou YH, Chang CY. Relationship between severity of venous calcifications and symptoms of phlebosclerotic colitis. World J Gastroenterol. 2015;21:8148-8155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Asayama N, Ogawa Y, Nagata S. Mesenteric phlebosclerosis causing a polypoid lesion mimicking colorectal carcinoma. Dig Endosc. 2019;31:211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Westermark P, Benson MD, Buxbaum JN, Cohen AS, Frangione B, Ikeda S, Masters CL, Merlini G, Saraiva MJ, Sipe JD; Nomenclature Committee of the International Society of Amyloidosis. Amyloid: toward terminology clarification. Report from the Nomenclature Committee of the International Society of Amyloidosis. Amyloid. 2005;12:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 227] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 25. | Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol. 2008;103:776-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 203] [Article Influence: 11.9] [Reference Citation Analysis (2)] |
| 26. | Yamada M, Hatakeyama S, Tsukagoshi H. Gastrointestinal amyloid deposition in AL (primary or myeloma-associated) and AA (secondary) amyloidosis: diagnostic value of gastric biopsy. Hum Pathol. 1985;16:1206-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 66] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Röcken C, Shakespeare A. Pathology, diagnosis and pathogenesis of AA amyloidosis. Virchows Arch. 2002;440:111-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 147] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 28. | Shimizu S, Kobayashi T, Tomioka H, Ohtsu K, Matsui T, Hibi T. Involvement of herbal medicine as a cause of mesenteric phlebosclerosis: results from a large-scale nationwide survey. J Gastroenterol. 2017;52:308-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Nagata Y, Watanabe T, Nagasaka K, Yamada M, Murai M, Takeuchi S, Murase M, Yazaki T, Murase T, Komatsu K, Kaizuka M, Sano M, Asano K, Ando C, Taniuchi N. Total dosage of gardenia fruit used by patients with mesenteric phlebosclerosis. BMC Complement Altern Med. 2016;16:207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Hirasaki S, Matsumura K. Development of phlebosclerotic colitis under treatment with Chinese herbal therapy. Intern Med. 2014;53:1709-1710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Ohtsu K, Matsui T, Nishimura T, Hirai F, Ikeda K, Iwashita A, Yorioka M, Hatakeyama S, Hoashi T, Koga Y, Sakurai T, Miyaoka M. [Association between mesenteric phlebosclerosis and Chinese herbal medicine intake]. Nihon Shokakibyo Gakkai Zasshi. 2014;111:61-68. [PubMed] |