Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4588
Peer-review started: April 22, 2020
First decision: August 8, 2020
Revised: August 18, 2020
Accepted: September 10, 2020
Article in press: September 10, 2020
Published online: October 6, 2020
Processing time: 158 Days and 18.6 Hours
Esophageal cancer is one of the most common causes of cancer-related death. Some patients with esophageal cancer have distant metastases at the time of diagnosis, but metastasis to the thyroid gland (MTG) and multifocal thyroid lesions alone are extremely rare.
In this case report, we present a case of a 69-year-old male with esophageal MTG. The patient visited our hospital for a routine body check-up, which revealed multifocal nodules in his thyroid lobes and enlarged cervical lymph nodes. A fine needle aspiration biopsy showed malignancies in both thyroid lesions and lymph nodes. The patient was initially diagnosed with primary bilateral thyroid cancer that spread to his lymph nodes, and a total thyroidectomy was performed. The histology showed MTG and therefore, a diagnostic work-up was implemented to determine the primary tumor. A fluorine-18-deoxyglucose positron emission tomography scan showed that the lower part of the esophagus and the lymph nodes in the neck, chest, and abdomen were involved. An esophagogastroscopy and corresponding pathology revealed distal esophageal squamous cell carcinoma. The esophageal MTG diagnosis was confirmed with pathological immunohistochemistry.
This case report highlights the difficulty in diagnosing esophageal MTG. Patients may have no malignancy history and be asymptomatic. Further diagnostic procedures are necessary after MTG is confirmed by cytology or histology, and the final diagnosis should be made according to the identification of the primary malignancy combined with pathological immunohistochemistry findings.
Core Tip: Metastasis to the thyroid gland (MTG) from esophageal cancer is rare, and only a few sporadic cases have been reported thus far. This study reports the findings of esophageal squamous cell carcinoma MTG in a 69-year-old man who presented for a routine checkup. The patient underwent bilateral thyroidectomy. The histology showed MTG. A diagnostic work-up was implemented and revealed metastasis of esophageal squamous cell carcinoma to the thyroid gland with widespread nodal involvement. He was administered four rounds of chemotherapy and is well 1 year after the diagnosis. Our findings will be of importance for diagnosing this rare condition.
- Citation: Zhang X, Gu X, Li JG, Hu XJ. Metastasis of esophageal squamous cell carcinoma to the thyroid gland with widespread nodal involvement: A case report. World J Clin Cases 2020; 8(19): 4588-4594
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4588.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4588
Esophageal cancer is the ninth most common cancer worldwide, with 572034 new cases estimated in 2018, and the sixth leading cause of cancer-related death, with 508585 cases[1]. Esophageal cancer distant metastases most commonly occur in the liver, followed by the lungs, bones, and brain[2]. Metastasis to the thyroid gland (MTG) is rare, with reported in surgical series ranging from 1.4% to 3.0%[3]. Esophageal malignancies are relatively rare sources of the thyroid metastases, compared to kidney and lung malignancies, and are only seen in 9% of patients with MTG[4]. In the clinical setting, secondary thyroid tumors only present without concurrent primary cancer symptoms or known malignancy histories in patients with MTG, and this situation can perplex physicians. We present the case of a patient with metastatic esophageal squamous cell carcinoma (ESCC) of a thyroid gland, which was initially misdiagnosed as primary thyroid cancer with cervical lymph node metastasis. After a thyroidectomy, esophageal MTG was confirmed by a fluorine-18-deoxyglucose positron emission tomography (FDG-PET-CT) combined with pathological immunohistochemistry.
An ever healthy 69-year-old Chinese male patient was hospitalized after a routine check-up that showed malignancy-suspected nodules in his bilateral thyroid lobes and enlarged cervical lymph nodes on both sides.
The patient was asymptomatic and received the treatment for the first time at our hospital.
The patient had an unremarkable past history except for diabetes and hypertension.
Physical examination revealed a 3.0 cm firm thyroid mass in the right thyroid lobe, and swollen neck lymph nodes were palpated on both sides.
The laboratory test results were normal for free triiodothyronine level (6.21 pmol/L, normal range 3.28-6.47 pmol/L), free thyroxine level (10.23 pmol/L, normal range 7.64-16.03 pmol/L), and thyroid-stimulating hormone level (1.79 mIU/L, normal range 0.51-5.91 mIU/L). The tumor markers levels were all in normal range.
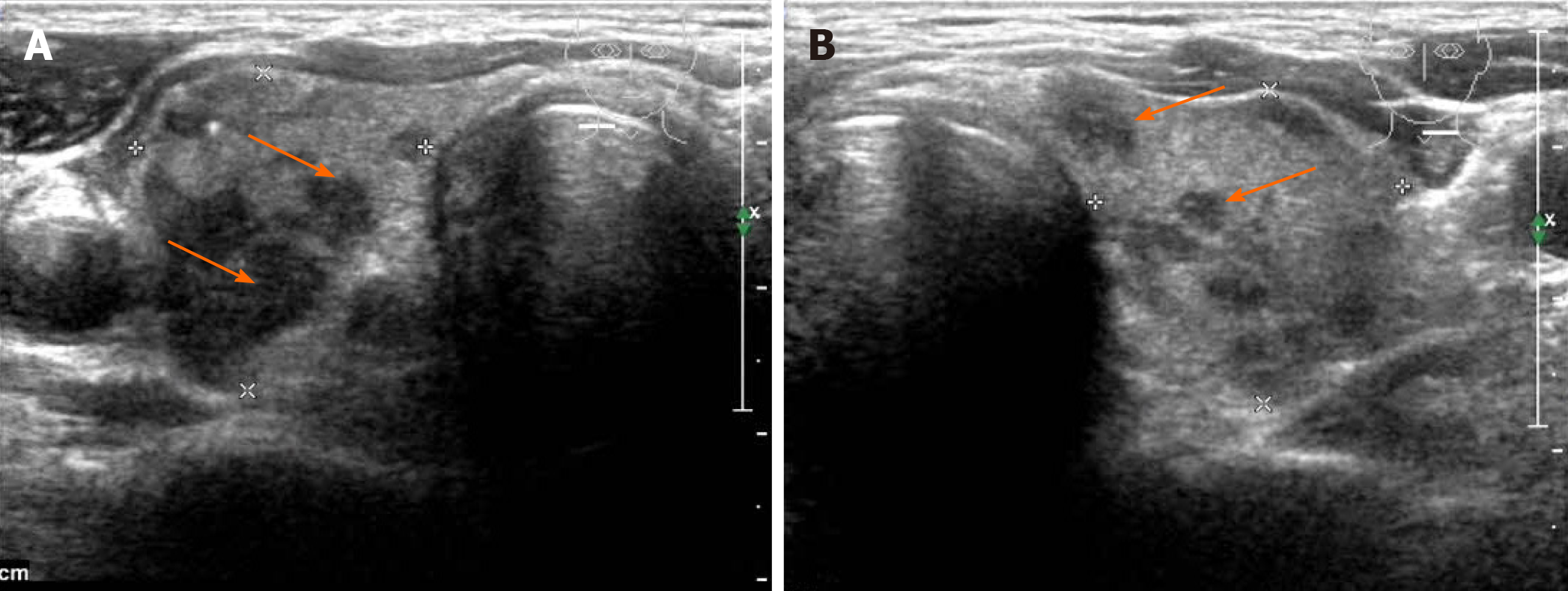
Ultrasonography revealed multiple Thyroid Imaging Reporting and Data System 4c nodules in bilateral thyroid lobes (Figure 1). Neck contrast-enhanced computed tomography (CT) scan indicated multifocal disease in the thyroid lobes and enlarged cervical lymph nodes on both sides (Figure 2).
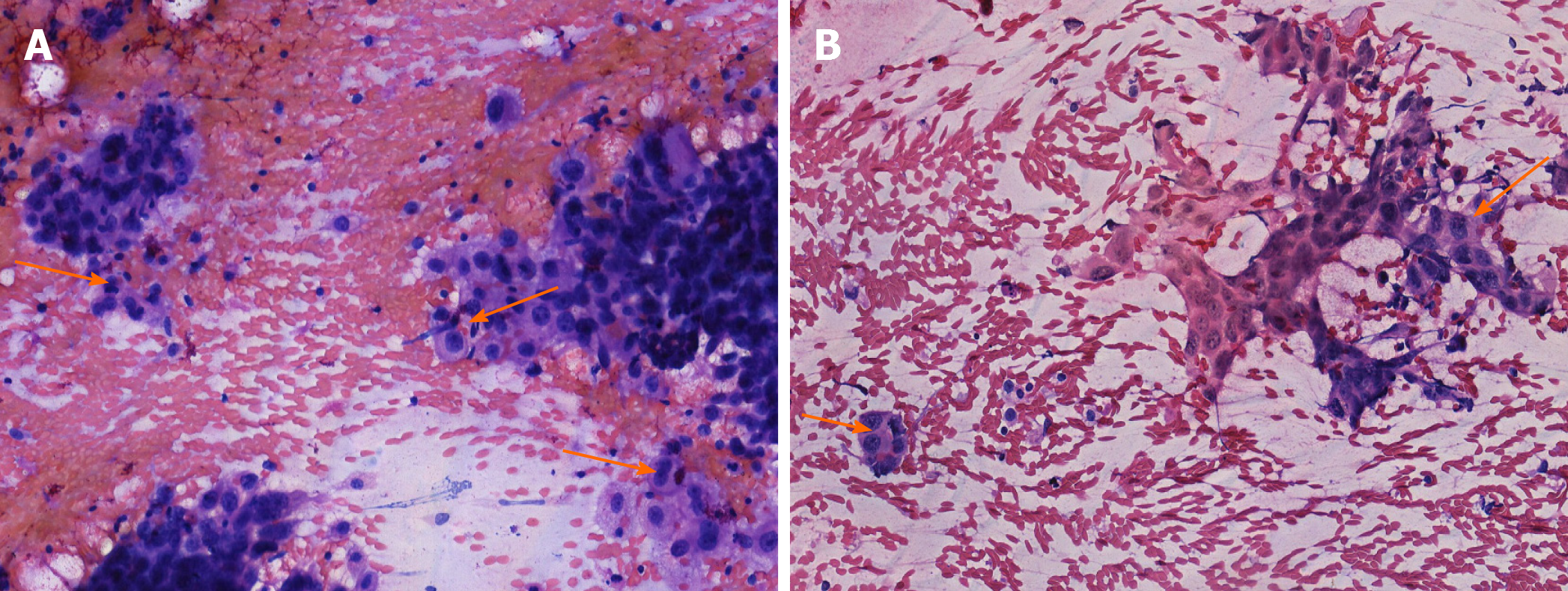
The patient underwent a fine needle aspiration (FNA) biopsy of the thyroid lesions and neck lymph nodes, which showed malignant tumor cells in both (Figure 3).
The final diagnosis of MTG from ESCC was based on the immunohistochemical panel after thyroidectomy.
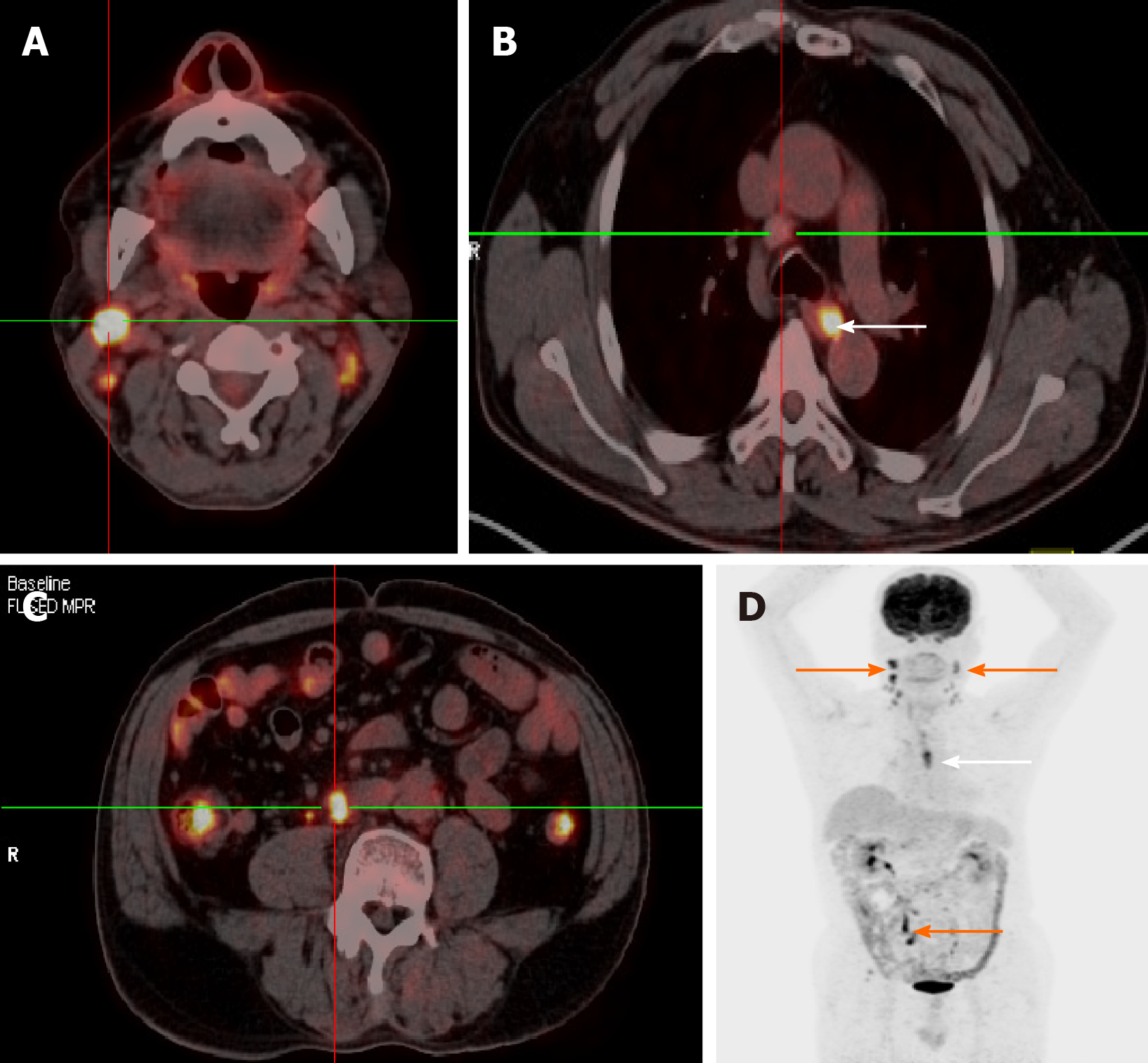
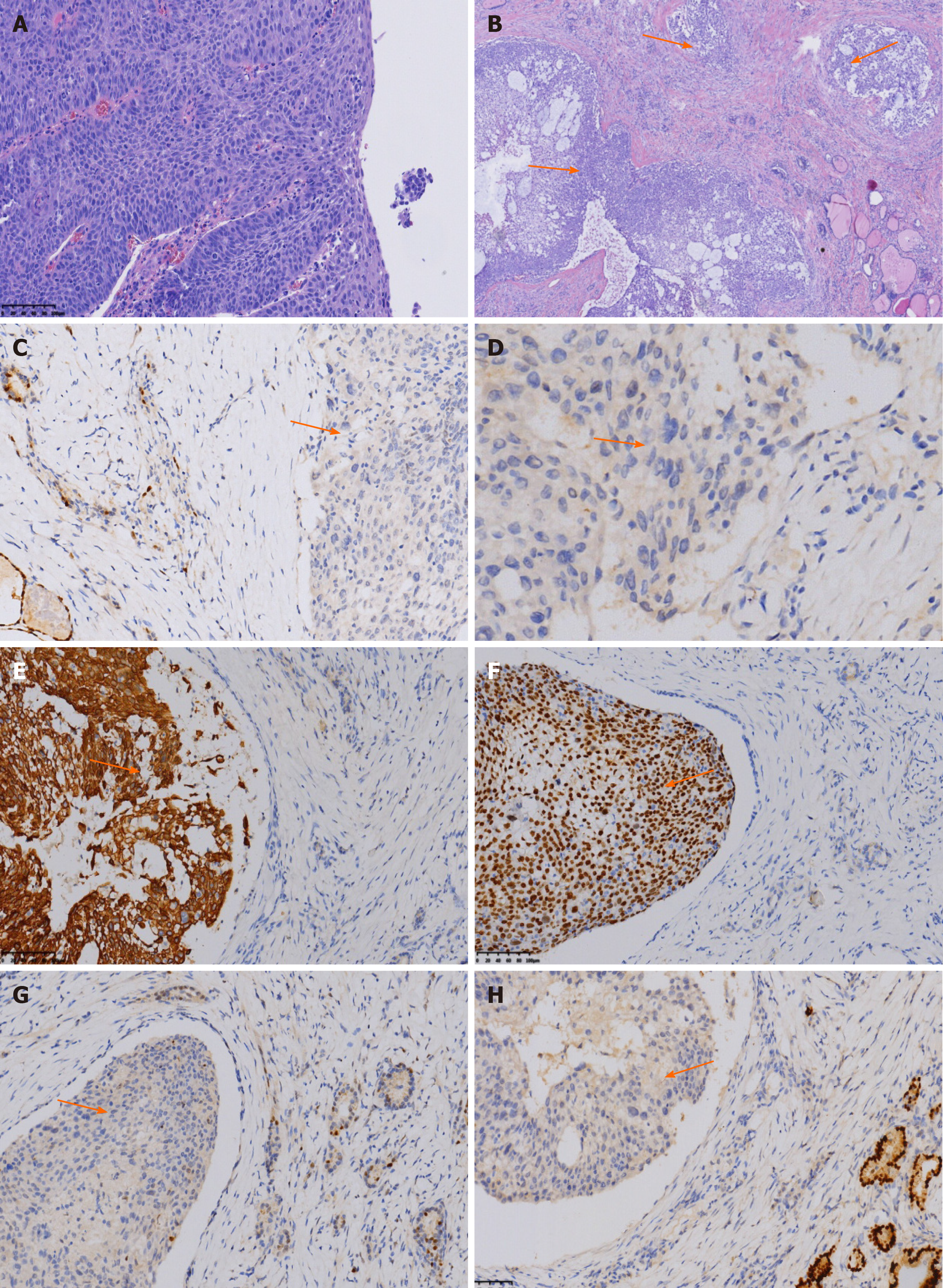
The patient received a total thyroidectomy plus bilateral level VI lymph nodes dissection. The permanent section revealed metastatic squamous cell carcinoma in the thyroid gland. Therefore, further diagnostic procedures were performed to determine the primary carcinoma. A chest CT scan revealed mediastinal nodal involvement, and an abdominal ultrasound was negative. A postoperative FDG-PET-CT was performed, which showed that the lower part of the esophagus and the lymph nodes in the neck, chest, and abdomen were all involved (Figure 4). The patient underwent an esophagogastroscopy, and a lesion was noted in the distal esophagus, in which squamous cell carcinoma was confirmed by biopsy (Figure 5A). Immuno-histochemistry of the thyroid lesions was consistent with features of metastatic ESCC (Figure 5B-H). The patient received four rounds of adjuvant chemotherapy of oxaliplatin combined with 5-fluorouracil every 3 wk and then withdrew due to the side effects.
He was followed up every 3 mo after discharge. At present, he is on traditional Chinese medicine and feels well 1 year after the diagnosis.
Although rare, esophageal MTG does occur. Physicians should keep in mind that it is necessary to perform further examinations of the cervical region when malignant, multifocal lesions in the thyroid gland are noted. MTG needs to be considered as a differential diagnosis, even in patients with no prior history of malignancy. MTG is generally regarded to result from the spread of a primary tumor by a hematogenous route. Despite its rich blood supply, the thyroid is a rare site for metastatic disease. This phenomenon is due to fast arterial flow that prevents cancer cell adhesion, and the high oxygen saturation and iodine content of the thyroid gland inhibit the growth of malignant cells[3]. The incidence of MTG is low and amounts to 2%-3% of all malignant tumors of the thyroid[5]. The most common primary malignancies that can metastasize to the thyroid gland are renal cell cancer, followed by lung cancer and breast cancer[6]. MTG from esophageal cancer is extremely rare, and only a few sporadic cases have been reported in the literature thus far[7-10]. To our knowledge, there has been no reported case of metastasis of esophageal cancer to the thyroid gland and widespread involvement of distant lymph nodes at the same time.
Metastatic disease that involves the thyroid gland may pose a diagnostic challenge. At presentation, MTG may share similarities with primary thyroid tumors, and most patients are asymptomatic[11]. MTG may be the sole presentation, without any primary tumor-related symptoms or previous malignancy history. This patient with MTG lacked symptoms of advanced-stage esophageal cancer like dysphagia, weight loss, and chest pain. The thyroid masses and neck nodal involvement were the only positive findings at the initial imaging and physical examination before the surgery. The fine needle aspiration cytology did not reveal MTG as well. Preoperative fine needle aspiration cytology is a reliable approach to establish the diagnosis. However, it has limitations with regard to distinguishing MTG from primary thyroid carcinoma. Therefore, this disease can confuse surgeons and masquerade the primary thyroid cancer metastases to cervical lymph nodes. Even after the thyroidectomy, the permanent section showed MTG. It was not an easy task to determine the primary tumor, and the work-up diagnostic procedures helped locate the primary tumor.
After all other routine examinations are negative for the primary tumor, FDG-PET-CT usually is the final resort; in some patients, the primary tumors cannot be found[4]. Although the indication of surgery for metastatic thyroid carcinomas is uncertain and does not impact overall survival, in some patients with MTG, a total thyroidectomy is warranted[12-14]. Especially for MTG multifocal disease, a total thyroidectomy should be considered and may achieve control of the central neck[6]. Furthermore, definitive histology by surgical excision may be required to confirm the diagnosis[15].
The differential diagnoses of MTG of ESCC include primary squamous cell carcinoma (PSCC) of the thyroid and mucoepidermoid thyroid carcinoma (MEC). PSCC of the thyroid resembles anaplastic thyroid carcinoma in clinical presentation. Patients with PSCC of the thyroid present with rapidly increasing neck mass invading the adjacent structures. Besides patients’ history, immunohistochemical panel is useful in diagnosing MTG. PSCC as well as squamous carcinoma component in association with other thyroid carcinomas have been shown to be positive for paired box gene 8 (PAX-8) protein[16]. Like anaplastic thyroid carcinoma, PSCC shows a high frequency of P53 overexpression[17]. In this case, PAX-8 and P53 were negative. The microscopic features of multifocal tumor nests along the vessels found in this case indicate MTG as well. The immunohistology characteristics of MEC generally demonstrate positive for thyroid transcription factor-1 (TTF1) and thyroglobulin. In this case, TTF1 and thyroglobulin were both negative. Furthermore, the immunohistochemical staining was positive for CK5/6 and P40. Combined with the results of FDG-PET-CT and esophagogastroscopy, the diagnosis of MTG from ESCC was confirmed.
It is difficult to determine the primary tumor when patients with esophageal MTG are asymptomatic and have no previous malignancies. Further diagnostic procedures are necessary after MTG is confirmed by cytology or histology, and the final diagnosis should be made according to the identification of the primary malignancy combined with pathological immunohistochemistry findings.
We acknowledge the work of the nurses and doctors of The Affiliated People’s Hospital of Ningbo University involved in the surgery and the following treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Okamoto H S-Editor: Wang DM L-Editor: Filipodia P-Editor: Wang LL
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55806] [Article Influence: 7972.3] [Reference Citation Analysis (132)] |
| 2. | Ai D, Zhu H, Ren W, Chen Y, Liu Q, Deng J, Ye J, Fan J, Zhao K. Patterns of distant organ metastases in esophageal cancer: a population-based study. J Thorac Dis. 2017;9:3023-3030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 3. | Chung AY, Tran TB, Brumund KT, Weisman RA, Bouvet M. Metastases to the thyroid: a review of the literature from the last decade. Thyroid. 2012;22:258-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 182] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 4. | Hegerova L, Griebeler ML, Reynolds JP, Henry MR, Gharib H. Metastasis to the thyroid gland: report of a large series from the Mayo Clinic. Am J Clin Oncol. 2015;38:338-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 5. | Cichoń S, Anielski R, Konturek A, Barczyński M, Cichoń W. Metastases to the thyroid gland: seventeen cases operated on in a single clinical center. Langenbecks Arch Surg. 2006;391:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 86] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Nixon IJ, Coca-Pelaz A, Kaleva AI, Triantafyllou A, Angelos P, Owen RP, Rinaldo A, Shaha AR, Silver CE, Ferlito A. Metastasis to the Thyroid Gland: A Critical Review. Ann Surg Oncol. 2017;24:1533-1539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 104] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 7. | Basu S, Nair N, Borges AM. Squamous cell carcinoma of esophagus masquerading as solitary thyroid nodule. Indian J Cancer. 2005;42:205-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Cumbo-Nacheli G, de Sanctis JT, Chung MH. Proximal esophageal adenocarcinoma presenting as a thyroid mass: case report and review of the literature. Thyroid. 2007;17:267-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Chen ED, Cheng P, Yan XQ, Ye YL, Chen CZ, Ji XH, Zhang XH. Metastasis of distal esophageal carcinoma to the thyroid with presentation simulating primary thyroid carcinoma: a case report and review of the literature. World J Surg Oncol. 2014;12:106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Kusunoki T, Murata K. A large cervical lymph node metastasis from a thoracic esophageal carcinoma considered a thyroid carcinoma at the first medical examination. Thyroid. 2005;15:1419-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Eloy JA, Mortensen M, Gupta S, Lewis MS, Brett EM, Genden EM. Metastasis of uterine leiomyosarcoma to the thyroid gland: case report and review of the literature. Thyroid. 2007;17:1295-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Chen H, Nicol TL, Udelsman R. Clinically significant, isolated metastatic disease to the thyroid gland. World J Surg. 1999;23:177-80; discussion 181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 115] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Osawa M, Takigawa N, Kiura K, Ichimura K, Matsuoka J, Hotta K, Tabata M, Tanimoto M. Isolated metastasis of lung cancer to the thyroid gland. Lung Cancer. 2007;58:156-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Papi G, Fadda G, Corsello SM, Corrado S, Rossi ED, Radighieri E, Miraglia A, Carani C, Pontecorvi A. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol (Oxf). 2007;66:565-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Nixon IJ, Whitcher M, Glick J, Palmer FL, Shaha AR, Shah JP, Patel SG, Ganly I. Surgical management of metastases to the thyroid gland. Ann Surg Oncol. 2011;18:800-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Suzuki A, Hirokawa M, Takada N, Higuchi M, Tanaka A, Hayashi T, Kuma S, Miyauchi A. Utility of monoclonal PAX8 antibody for distinguishing intrathyroid thymic carcinoma from follicular cell-derived thyroid carcinoma. Endocr J. 2018;65:1171-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Lam AK. Squamous cell carcinoma of thyroid: a unique type of cancer in World Health Organization Classification. Endocr Relat Cancer. 2020;27:R177-R192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |