Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4481
Peer-review started: June 1, 2020
First decision: June 19, 2020
Revised: August 7, 2020
Accepted: September 1, 2020
Article in press: September 1, 2020
Published online: October 6, 2020
Processing time: 119 Days and 0.4 Hours
A cutaneous ciliated cyst (CCC) is a rare, benign tumor in young female adults, which is usually found on the lower extremities.
We found an uncommon location of CCC in the anterolateral cervical area and reviewed the literature. A 20-year-old female complained of a well-defined, painless, palpable mass that started several years ago. The mass was tense and movable and located at the anterolateral aspect of the neck. Imaging showed a non-enhancing round mass. Surgical excision biopsy was performed, and the cystic mass was revealed to be a CCC.
The rare location of CCC can be found in anterior neck area, which should be another diagnostic option for mass on anterior neck.
Core Tip: Cutaneous ciliated cysts are benign tumor and commonly found on lower extremities of young female adults. This case shows a rare location of cutaneous ciliated cyst found on anterior neck area, which can be another diagnostic option for evaluating anterior neck mass.
- Citation: Kim YH, Lee J. Cutaneous ciliated cyst on the anterior neck in young women: A case report. World J Clin Cases 2020; 8(19): 4481-4487
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4481.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4481
Morphologic evaluation or physical examination is helpful in the differential diagnosis of benign skin lesions in the cervical region. However, if the lesion is located deep in the subcutaneous area and does not have pathognomonic findings, such as central punctum of the epidermoid cyst, the differential diagnosis can be challenging and requires further imaging modalities. Otherwise, the location of the mass can be associated with its origin. Congenital neck masses can be classified by their location. Thyroglossal duct cyst, cervical clefts, and teratomas are mostly located at the midline, and branchial cleft anomalies, lymph nodes, and thyroid lesions are mostly located in the lateral neck[1].
Cutaneous ciliated cyst (CCC) was first reported in 1978 by Farmer and Helwig. It is a rare benign tumor of Mullerian heterotopias, and it has been reported as frequent in young females after puberty[2]. The most common location is the lower extremities. There have been serial case reports that reported unusual locations of CCC, such as the back[2], abdominal wall[3], or scalp[4]. It rarely occurs in male patients, and the locations reported are in the perineum, inguinal, and shoulder areas.
To our knowledge, there are limited reports of CCC that develop in the anterolateral neck area. We report our experience and summarize previous literature.
A 20-year-old female patient visited the clinic with a palpable nodule in her right anterior neck area.
The mass was first noticed a few years previous, and she could barely remember, but it had not grown since then.
She did not have any specific medical history, including congenital anomaly. However, she had a family history of papillary thyroid cancer of her father.
The mass was located in the subcutaneous tissue of the mediolateral area of the anterior neck, close to the right head portion of the clavicle. It was movable and tense and not accompanied by pain, fever, or redness. No specific abnormality was seen on her thyroid gland and midline cervical area.
Ultrasonography showed a well-demarcated low echoic round mass, measuring 2.2 cm × 1.5 cm. The complete blood count showed that the white blood cell count was 4500/mm3, hemoglobin 13.9 g/dL, hematocrit 42.8%, and platelet count 264000 /µL. Neutrophil showed 55.82% in differential count, and lymphocyte showed 32.45%, monocyte 9.32%, eosinophil 1.70%, and basophil 0.71%. Blood chemistry results, including aspartate aminotransferase, alanine aminotransferase, total bilirubin, alkaline phosphatase, uric acid, gamma guanosine triphosphate, and lactate dehydrogenase, were within normal limits. Serum β-human chorionic gonadotropin detected to be less than 1.20 mIU/mL.
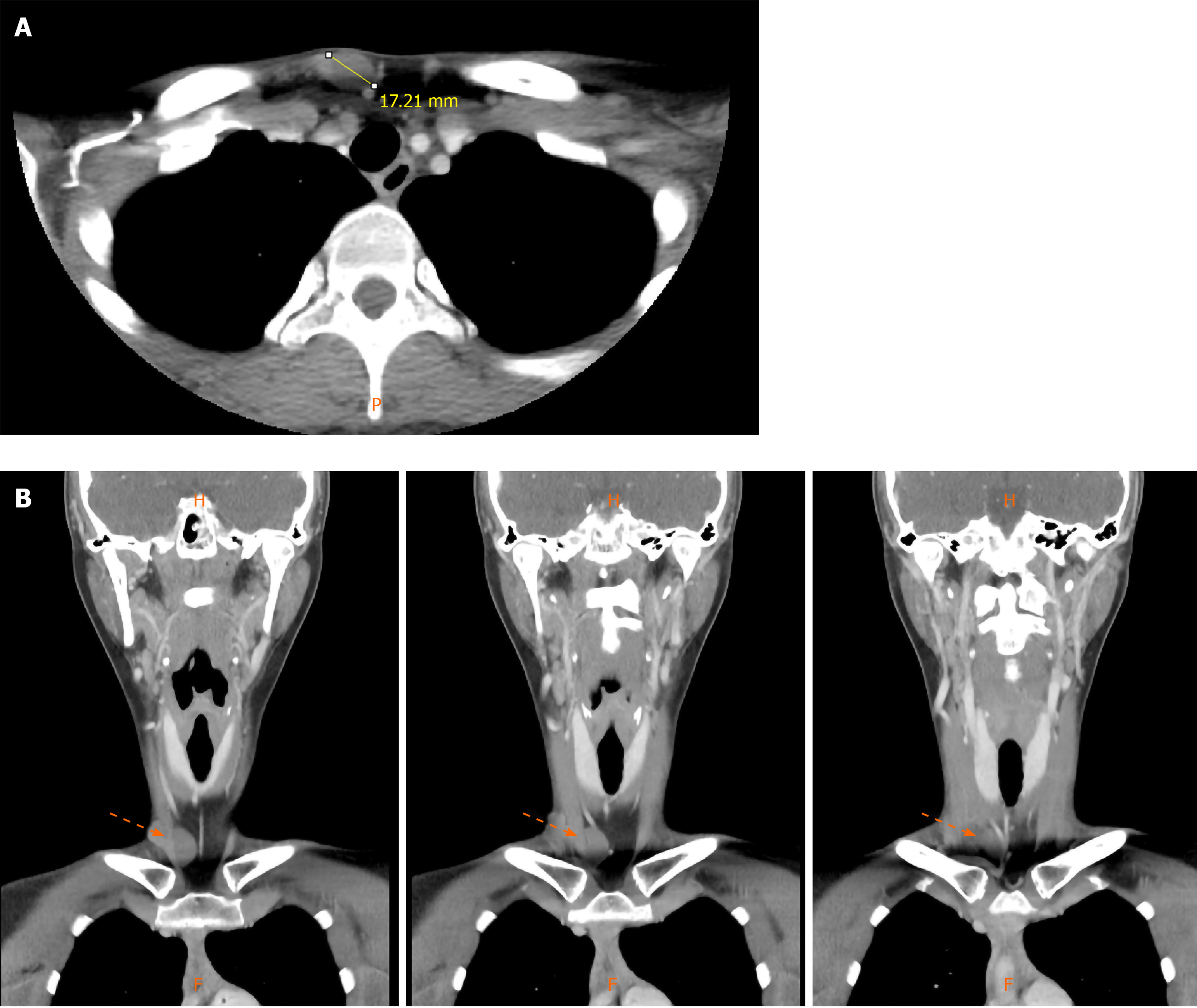
Computed tomography (CT) was performed for the differential diagnosis and spatial evaluation. Enhanced CT imaging showed a non-enhancing well-defined ovoid mass in the right paramidline supraclavicular fossa that measured 2.2 cm × 1 cm × 1.5 cm (Figure 1A and B), and the differential diagnosis from the image was dermoid or epidermoid cyst.
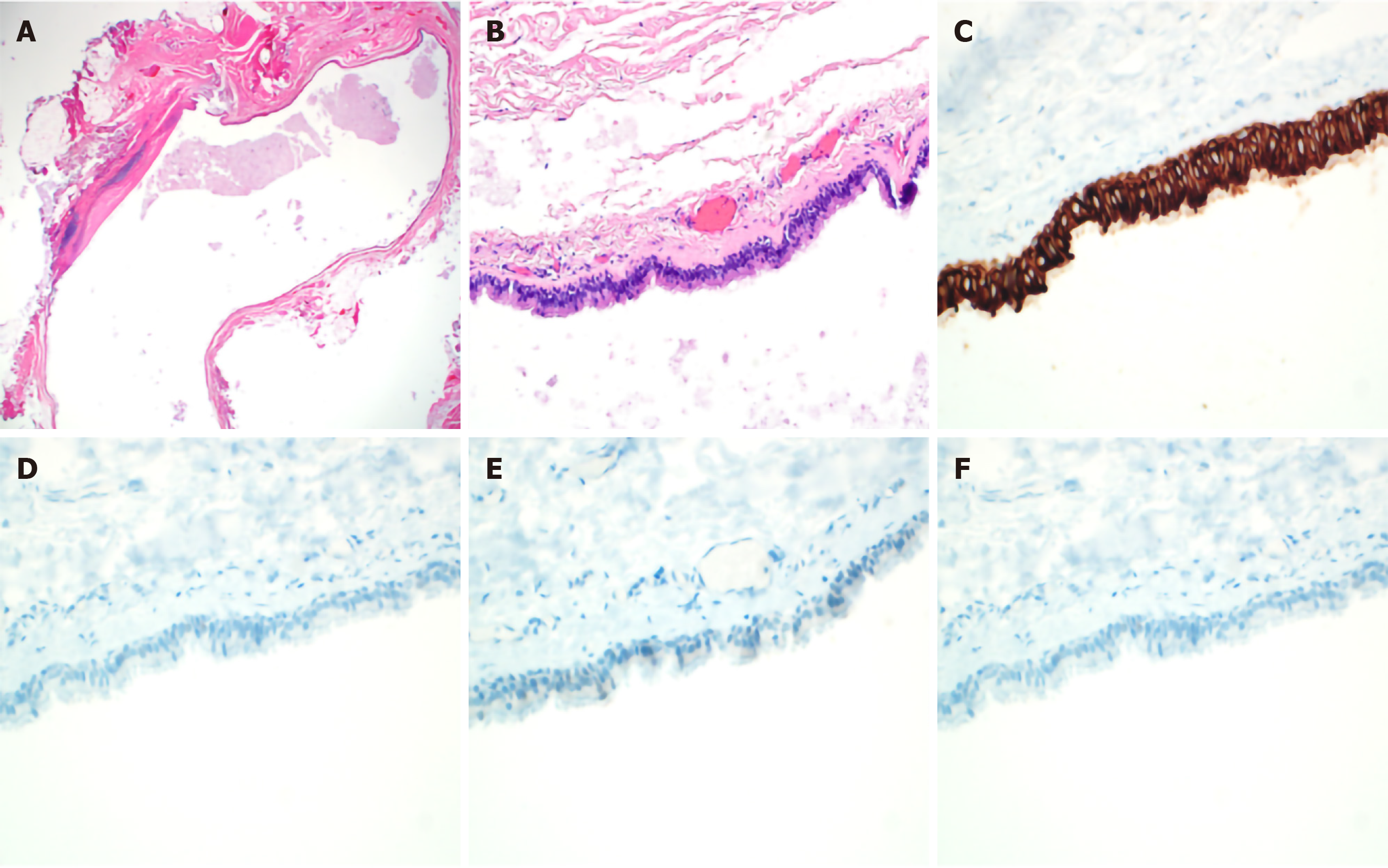
She had undergone an excisional biopsy for therapeutic and diagnostic purposes. In the gross examination, the lesion was an ovoid-shaped, solid, soft mass, and thin fibrous capsules surrounded the entire lesion. The microscopic findings revealed a well-defined and thin-walled, ovoid, unilocular cystic lesion lined by ciliated pseudostratified cuboidal to columnar epithelium showing focal intraluminal papillary projections in the subcutaneous tissue. The luminal surface of the cystic lesion was filled with amorphous proteinous materials without keratinous and solid mass-like lesion. The outer surface of the cystic lesion was completely covered with thin collagenous tissue without smooth muscle bundles. It also showed focal chronic inflammatory change with no lymphoid follicles or other components. The peritumoral subcutaneous tissue revealed no thyroid, cartilaginous, or skin appendageal tissue (Figure 2).
After complete excision of the lesion, there was no development of seroma or wound infection.
After six months of follow-up, there was no evidence of local recurrence.
The location of CCC is mostly around the perineum or lower extremities, and is also reported in the abdominal wall, back, fingertips, and scalp. We reviewed the literature available of full-text files using PubMed search between 1978 and 2019 (Table 1). Most of the clinical features were palpable cystic masses remaining indolent for months to decades, except one report of a rapid growth two months after two years from its first notice[5]. The case reports included atients of various races, including African, Caucasian, and Asian. When the mass was ruptured during operation, the cystic contents showed clear serous or yellowish fluid materials. Limited evidence of long-term follow-up was found. Ross et al[6] reported a 36-year-old female patient with CCC on the dorsal aspect of the foot, found indolent since the patient’s late teens. Santos et al[7] reported a 35-year-old male patient who had CCC in his right perineum; they reported no evidence of recurrence or malignant change during follow-up.
| Ref. | Sex (Age, yr) | Race | Clinical features of location, size and duration | Outcome |
| Park et al[17], 1982 | F (15) | NA | Upper half of right thigh, 2 cm, no increase in size over 7 mo | NA |
| Ross et al[6], 1983 | F (36) | African | Dorsal aspect of left foot, 3.5 cm, noticable at late teens | No chance since late teens |
| al-Nafussi et al[18], 1990 | F (42) | NA | A 4.5 cm painless mass with no increase in size over 2 years | NA |
| Sickel et al[19], 1994) | F (20) | African | 4 cm mass lasted over 2 years | NA |
| Trotter et al[8], 1994 | M (28) | Caucasian | dorsal aspect of left foot, 3 cm | NA |
| Ashton et al[9], 1995 | M (27) | NA | Sole of right foot 2 cm, 2 years | NA |
| Tachibana et al[5], 1995 | F (19) | Asian | Bottock, 5.5cm, 2 years | NA |
| Yokozaki et al[20], 1999 | F (23) | Asian | Right lower leg, 2.5 cm, growing during 12 months | NA |
| Dini et al[21], 2000 | F (12) | Caucacian | Sacrococcygeal area, 1.4 cm, enlarged slightly over 1 month | NA |
| Lee et al[22], 2001 | F (13) | NA | Midline coccygeal lesion, 2.5 cm | NA |
| Fontaine et al[3], 2002 | F (14) | NA | Right lower abdomen, 2 cm, 3 months, growing mass | NA |
| Ohba et al[10], 2002 | M (53) | NA | 2 cm, 2 years of history | NA |
| Vadmal et al[23], 2002 | F (18) | NA | left flank, 0.7 cm, 6-7 months duration | NA |
| Santos et al[7], 2004 | M (35) | Asian | Right perineum, 3.5 cm | No evidence of recurrence |
| Kim et al[24], 2006 | F (41) | NA | 1.5 cm, slowly growing during 3 mo | NA |
| Lee et al[11], 2006 | M (56) | NA | Right inguinal area, 1.5 cm, 3 years | NA |
| Chong et al[25], 2006 | F (16) | NA | 1 year duration of painless nodule, increasing in size | NA |
| Torisu et al[26], 2008 | F (51) | Asian | Posterior aspect of left leg, gradually increase during 2 years | NA |
| Bivin et al[2], 2010 | F (13) | African | Right leg, 2 cm, slowly growing over 2 years | NA |
| Ashturkar et al[27], 2011 | F (18) | NA | Right knee, 3 cm, gradually increasing mass during 4 years | NA |
| Gelincik et al[28], 2011 | F (25) | NA | Subcutaneous area, 2 years | NA |
| Hung et al[29], 2012 | F (16) | NA | Left thumb, 1.1 cm | NA |
| Kavishwar et al[30], 2014 | F (38) | NA | Right popliteal fossa, 3 cm | NA |
| Oh et al[31], 2014 | F (13) | Caucasian | 3 cm | NA |
| Reserva et al[4], 2014 | F (53) | African | Vertex mass, lifelong history | NA |
| Keisling et al[32], 2015 | F (14) | NA | Right lower leg, 2 cm | NA |
| Kim et al[12], 2015 | M (7) | NA | Left shoulder, 1 cm, 3 years | NA |
| Swarbrick et al[33], 2015 | M (14) | NA | Scrotal cyst | NA |
| Fabien-Dupuis et al[13], 2016 | F (16) | NA | Right thigh, 2.5 cm, 3 years | NA |
| Doğan et al[34], 2018 | F (13) | NA | Between scapula, 2 cm, few months | NA |
| Orleans et al[35], 2019 | F (37) | African | Mid back, 3.5 cm, years of history | NA |
CCC developed in male patients was found in a few reports[7-11]; the locations were the scalp, perineum, and back. There has been a debate whether it is a persistent Mullerian cyst or ciliated metaplasia in the eccrine cyst lining[12]. Because CCC has been regarded as Mullerian in origin, in addition to the morphologic evaluation under hematoxylin and eosin stain, there were reports of the use of estrogen receptor (ER), progesterone receptor, WT1, or PAX-8 immunostaining[13]. Like other studies, the results of the immunohistochemical staining for ER, S-100, and desmin in this patient were negative[9]. The choice of the diagnostic modality of a neck mass is sometimes challenging, especially if the mass is cystic nature. Cystic lesions on the lateral neck in young adult can have malignant potential, such as metastatic thyroid cancer[14,15]. Fine needle aspiration cytology (FNAC) can be useful in solid lesions or metastatic thyroid cancer, but the diagnostic yield might not be sufficient for a definite diagnosis in cystic masses. Moreover, FNAC can be performed for the diagnosis of thyroglossal duct cysts[16] or epidermal cysts. However, it might cause an infection that interferes with the subsequent surgical procedure.
The rare location of this case should be helpful to diagnostic decision of masses on the lateral neck in young female adults.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Korean Surgical Society.
Specialty type: Surgery
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Luo WR S-Editor: Wang JL L-Editor: A P-Editor: Ma YJ
| 1. | Quintanilla-Dieck L, Penn EB. Congenital Neck Masses. Clin Perinatol. 2018;45:769-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Bivin WW, Heath JE, Drachenberg CB, Strauch ED, Papadimitriou JC. Cutaneous ciliated cyst: a case report with focus on mullerian heterotopia and comparison with eccrine sweat glands. Am J Dermatopathol. 2010;32:731-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Fontaine DG, Lau H, Murray SK, Fraser RB, Wright JR. Cutaneous ciliated cyst of the abdominal wall: a case report with a review of the literature and discussion of pathogenesis. Am J Dermatopathol. 2002;24:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Reserva JL, Carrigg AB, Schnebelen AM, Hiatt KM, Cheung WL. Cutaneous ciliated cyst of the scalp: a case report of a cutaneous ciliated eccrine cyst and a brief review of the literature. Am J Dermatopathol. 2014;36:679-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Tachibana T, Sakamoto F, Ito M, Ito K, Kaneko Y, Takenouchi T. Cutaneous ciliated cyst: a case report and histochemical, immunohistochemical, and ultrastructural study. J Cutan Pathol. 1995;22:33-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Ross AJ, Schwartz RA. Ciliated cutaneous cyst of the foot. J Surg Oncol. 1983;24:90-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Santos LD, Mendelsohn G. Perineal cutaneous ciliated cyst in a male. Pathology. 2004;36:369-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Trotter SE, Rassl DM, Saad M, Sharif H, Ali M. Cutaneous ciliated cyst occurring in a male. Histopathology. 1994;25:492-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Ashton MA. Cutaneous ciliated cyst of the lower limb in a male. Histopathology. 1995;26:467-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Ohba N, Tsuruta D, Muraoka M, Haba T, Ishii M. Cutaneous ciliated cyst on the cheek in a male. Int J Dermatol. 2002;41:48-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Lee JS, Kim YC, Lee ES. Cutaneous ciliated cyst of the inguinal area in a man. J Dermatol. 2006;33:146-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Kim Y, Kim H. The Cutaneous Ciliated Cyst in Young Male: The Possibility of Ciliated Cutaneous Eccrine Cyst. Case Rep Med. 2015;2015:589831. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Fabien-Dupuis C, Cooper B, Upperman J, Zhou S, Shillingford N. Mullerian-Type Ciliated Cyst of the Thigh with PAX-8 and WT1 Positivity: A Case Report and Review of the Literature. Case Rep Med. 2016;2016:2487820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Yehuda M, Schechter ME, Abu-Ghanem N, Golan G, Horowitz G, Fliss DM, Abu-Ghanem S. The incidence of malignancy in clinically benign cystic lesions of the lateral neck: our experience and proposed diagnostic algorithm. Eur Arch Otorhinolaryngol. 2018;275:767-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Seven H, Gurkan A, Cinar U, Vural C, Turgut S. Incidence of occult thyroid carcinoma metastases in lateral cervical cysts. Am J Otolaryngol. 2004;25:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Shahin A, Burroughs FH, Kirby JP, Ali SZ. Thyroglossal duct cyst: a cytopathologic study of 26 cases. Diagn Cytopathol. 2005;33:365-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Park CH, Grisoni E, Reid JD. Cutaneous ciliated cyst case report and discussion of pathogenesis. J Pediatr Surg. 1982;17:410-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | al-Nafussi AI, Carder P. Cutaneous ciliated cyst: a case report and immunohistochemical comparison with fallopian tube. Histopathology. 1990;16:595-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Sickel JZ. Cutaneous ciliated cyst of the scalp. A case report with immunohistochemical evidence for estrogen and progesterone receptors. Am J Dermatopathol. 1994;16:76-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Yokozaki H, Yanagawa E, Harada M, Tahara E. Cutaneous ciliated cyst of the right lower leg. Pathol Int. 1999;49:354-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Dini M, Lo Russo G, Baroni G, Colafranceschi M. Cutaneous ciliated cyst: a case report with immunohistochemical evidence for dynein in ciliated cells. Am J Dermatopathol. 2000;22:519-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Lee MT, Heller DS, Lambert WC, Bethel C. Cutaneous ciliated cyst with interspersed apocrine features presenting as a pilonidal cyst in a child. Pediatr Dev Pathol. 2001;4:310-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Vadmal MS, Makarewicz K, Fontaine DG, Wright JR. Cutaneous ciliated cyst of the abdominal wall. Am J Dermatopathol. 2002;24:452-3; author reply 453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Kim DY, Park SG, Lee JH, Kim YC, Lee KH. A case of cutaneous ciliated cyst on the umbilicus mimicking omphalomesenteric duct cyst and urachal cyst. J Eur Acad Dermatol Venereol. 2006;20:1161-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Chong SJ, Kim SY, Kim HS, Kim GM, Kim SY, Jung JH. Cutaneous ciliated cyst in a 16-year-old girl. J Am Acad Dermatol. 2007;56:159-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Torisu-Itakura H, Itakura E, Horiuchi R, Matsumura M, Kiryu H, Takeshita T, Ohjimi Y, Furue M. Cutaneous ciliated cyst on the leg in a woman of menopausal age. Acta Derm Venereol. 2009;89:323-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Ashturkar AV, Pathak GS, Joshi AR. Cutaneous ciliated cyst over knee. J Cutan Aesthet Surg. 2011;4:158-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Gelincik I. Cutaneous ciliated cyst in the subcutaneous area. Indian J Pathol Microbiol. 2011;54:150-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 29. | Hung T, Yang A, Binder SW, Barnhill RL. Cutaneous ciliated cyst on the finger: a cutaneous mullerian cyst. Am J Dermatopathol. 2012;34:335-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Kavishwar VS, Waghmare RS, Puranik GV, Chadha K. Cutaneous ciliated cyst of right popliteal fossa. J Assoc Physicians India. 2014;62:85-87. [PubMed] |
| 31. | Oh JS, Bhalla VK, Needham L, Sharma S, Pipkin WL, Hatley RM, Howell CG. Müllerian-type, cutaneous ciliated cyst in the gluteal cleft mimicking a pilonidal cyst. Pediatr Surg Int. 2014;30:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 32. | Keisling M, Marinovich A, Burkey B. Photoletter to the editor: Subcutaneous ciliated Mullerian cyst. J Dermatol Case Rep. 2015;9:116-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 33. | Swarbrick N, Harvey NT, Wood BA. Cutaneous ciliated cyst of the scrotum. Pathology. 2015;47:593-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Doğan G, İpek H, Metin M, Özkayar Ö, Afşarlar ÇE. Cutaneous Ciliated Cyst in an Unusual Location: Between Two Scapulas. Case Rep Surg. 2018;2018:5961913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Orleans RA, Magro CM, Varghese GI. A subcutaneous nodule on the mid back. JAAD Case Rep. 2019;5:252-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |