Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4400
Peer-review started: May 6, 2020
First decision: May 21, 2020
Revised: June 3, 2020
Accepted: August 26, 2020
Article in press: August 26, 2020
Published online: October 6, 2020
Processing time: 144 Days and 13.4 Hours
There are many types of treatments for calcaneal fractures, including conservative treatment, conventional surgical treatment, and minimally invasive surgery. The choice of specific treatment options is still controversial. Open reduction and internal fixation are currently the most commonly used surgical procedures in the clinic. A good fracture reduction effect can be achieved by using the lateral extension incision of the calcaneus; however, many studies have reported a high incidence of postoperative incision complications. Although there are many methods for the classification of intra-articular calcaneal fractures, it is generally believed that the computed tomography (CT) classification proposed by Sanders has high application value in the selection of treatment methods and evaluation of prognosis of calcaneal fractures. However, this method has no clear guiding significance for the choice of surgical incision and surgical plan.
To explore the application and clinical efficacy of medial column classification in the treatment of intra-articular calcaneal fractures.
From July 2017 to July 2018, 91 patients, including 60 males and 31 females aged 27 to 60 years, were enrolled. All participants had closed intra-articular calcaneal fracture, and their surgical options were selected under the guidance of medial column classification. The patients’ fractures were classified according to the Sanders classification: Type II, 35 cases; Type III, 33 cases; and Type IV, 23 cases. Among them, 53 patients had medial column displacement (shortened varus) and underwent open reduction and internal fixation with L-lateral incision of the calcaneus; 38 patients had no displacement of the medial column and underwent open reduction and internal fixation with tarsal sinus incision. The calcaneus Böhler angle, Gissane angle, length, width, height, and step thickness of the articular surface were evaluated by X-ray and three-dimensional CT before and after surgery and at the last follow-up. Foot function recovery was assessed by the Maryland foot scoring criteria.
All patients were followed for 5 to 14 mo, with an average of 10.5 ± 2.9 mo. The fractures of all patients healed, and the healing time was 10 to 19 wk, with an average of 10.8 ± 1.5 wk. One patient developed wound infection 1 wk after surgery and was actively debrided and implanted with antibiotic calcium sulfate to control the infection. The patient's fracture healed 5 mo after surgery. One patient developed a sural nerve injury, and the symptoms disappeared 3 mo after surgery. The patients were assessed according to the Maryland foot scoring system: Excellent in 77 cases, good in 10, and fair in 4. The excellent and good rate was 95.6%.
Medial column classification can effectively guide the surgical selection for intra-articular fractures of the calcaneus.
Core Tip: This is a retrospective study to evaluate the application and clinical efficacy of medial column classification in the treatment of intra-articular calcaneal fractures. A total of 91 participants were selected under the guidance of medial column classification: 53 patients had medial column displacement and underwent open reduction and internal fixation with L-lateral incision of the calcaneus; 38 patients had no displacement of the medial column and underwent open reduction and internal fixation with tarsal sinus incision. According to the Maryland foot scoring system, the excellent and good rate was 95.6%. Medial column classification can effectively guide the surgical selection for intra-articular fractures of the calcaneus.
- Citation: Zheng G, Xia F, Yang S, Cui J. Application of medial column classification in treatment of intra-articular calcaneal fractures. World J Clin Cases 2020; 8(19): 4400-4409
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4400.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4400
Calcaneal fractures are the most common tarsus fractures, accounting for 2% of body fractures. Twenty-six percent of calcaneal fractures are combined with contralateral limb injuries, 10% are combined with spinal fractures, and approximately 60%-75% are intra-articular fractures[1]. At present, the lateral L incision open reduction and internal fixation technique is the most common and effective method for the treatment of displaced calcaneal fractures. However, the surgical operation causes great damage to soft tissue. Therefore, there has been much controversy about postoperative complications, such as wound infection and nonhealing[2]. With the in-depth development of minimally invasive treatment of calcaneal fractures, many doctors use the tarsal sinus approach to fix calcaneal fractures. However, this method is not effective for the reduction of the medial column, and if necessary, a medial auxiliary incision is required. At present, the choice of surgical incision is still extremely challenging and controversial, and there is currently no uniform standard for the choice of surgical approach[3]. To further improve the overall reduction effect and to explore the surgical options and individualized treatment for intra-articular calcaneal fractures, we selected 91 patients who underwent treatment from July 2017 to July 2018 at the Department of Foot and Ankle Surgery, Central Hospital Affiliated to Shenyang Medical College. According to the displacement of the patient’s medial column, they were divided into two types: Medial column displacement (shortened varus, 53 cases) and nondisplacement (38 cases). Patients with medial column displacement underwent open reduction and internal fixation with an L-lateral incision of the calcaneus; patients with medial column nondisplacement underwent open reduction and internal fixation with a tarsal sinus incision. A satisfactory effect was obtained, and the report is as follows.
The inclusion criteria were: (1) Closed fresh calcaneus fracture; and (2) Calcaneus internal fixation. The exclusion criteria were: (1) Tongue-shaped fracture; or (2) Open fracture.
In this study, 91 patients were enrolled, including 60 males and 31 females, aged 27 to 60. The patients’ fractures were classified according to the Sanders classification: 35 cases of Type II, 33 cases of Type III, and 23 cases of Type IV. After admission, the patients were treated by limb elevation to reduce swelling. Lateral and axial calcaneus X-ray examination, parallel computed tomography (CT) scan, and three-dimensional reconstruction were performed. Patients were grouped according to X-ray and CT examination results. There were 53 cases of medial column displacement (short inversion), and open reduction and internal fixation through an L-lateral incision was planned for these patients. Surgery is acceptable when the skin on the outer heel is wrinkled, and the average time is 1-2 wk after the injury. There were 38 cases of medial column nondisplacement. Open reduction and internal fixation through the tarsal sinus incision was planned, and the operation was performed 3-7 d after the injury. Cefazolin (2.0 g) was used to prevent infection 30 min before surgical anesthesia. The study was approved by the Ethics Committee of Central Hospital Affiliated to Shenyang Medical College.
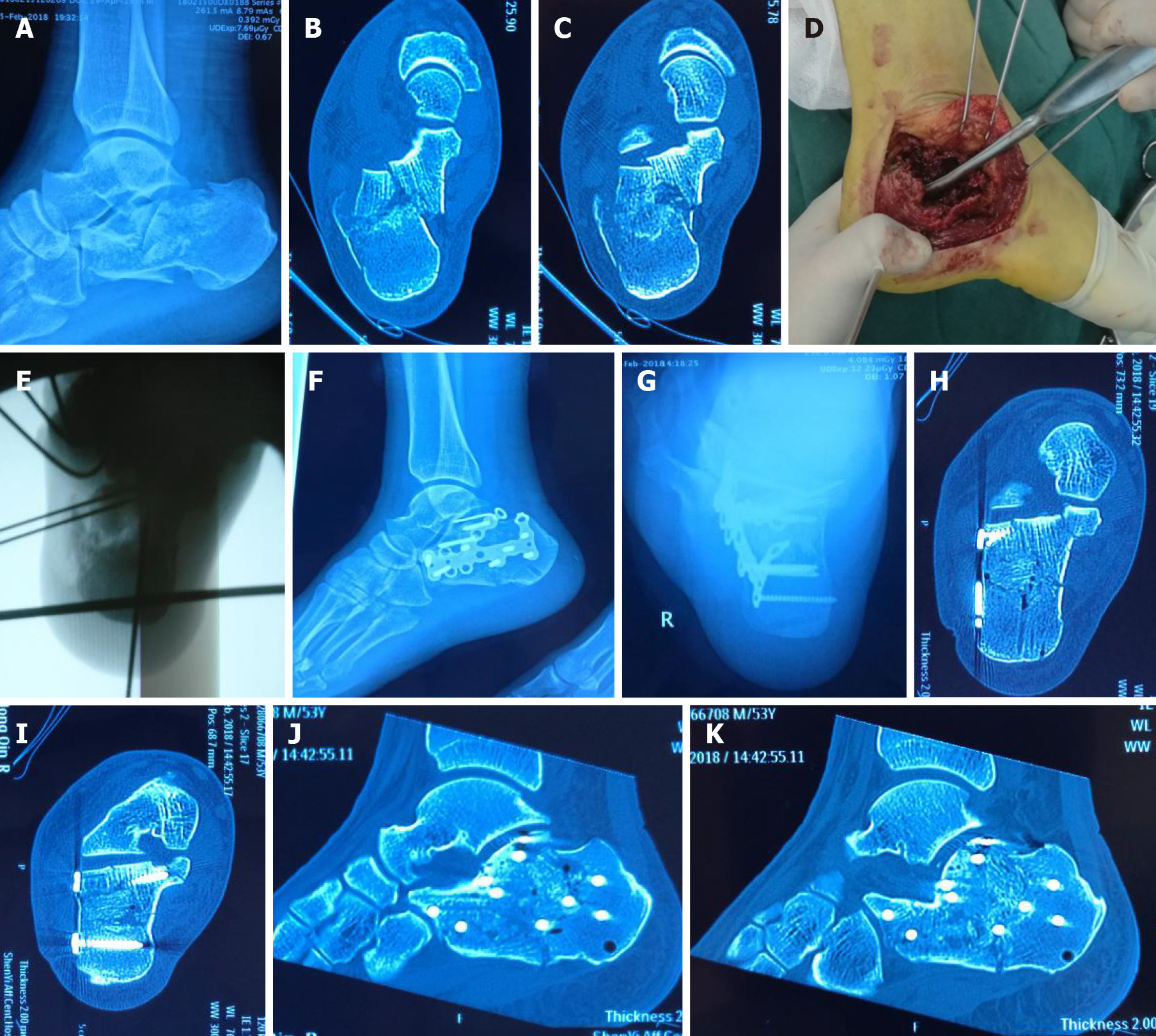
The patient was placed in the lateral position. The operation was performed with general anesthesia or subarachnoid block anesthesia. A conventional tourniquet was inflated on the thigh, and the lower limbs were sterilized and draped in a sterile manner. A traditional L-shaped incision from the lower part of the lateral malleolus was made. The incision reached the periosteum of the calcaneus. The subperiosteal soft tissue flap was separated sharply and turned up. The sural nerve was separated to protect it. The ligamenta calcaneofibulare calcaneus insertion was cut off sharply. Kirschner wires were inserted at the lateral malleolus, the lower part of the talus, and the tibia to protect the flap. The calcaneal posterior articular surface was exposed upwards, and the calcaneus protrusion and the Achilles tendon were exposed forward. The lateral or lateral posterior articular surface of the calcaneus was turned over. The posterior nodules were pulled with point-resetting forceps or a transverse Kirschner wire, and the freely collapsed posterior articular surface was removed to see the overlap and displacement of the sustentaculum tali bone block and the posterior nodule bone block and the deformation of the posterior nodule varus. Checking the stability of the sustentaculum tali bone block indicated that in some patients, the displacement of the sustentaculum tali bone block should be reset. The main fracture line was released from the external upper to the internal lower region. The posterior nodule was towed, turned over, and moved inward. Reset was performed under direct vision to restore the length, width, and force line of the calcaneus. Kirschner wires were used to fix the sustentaculum tali and posterior nodule bone blocks. After C-arm X-ray confirmation, the articular surface and the lateral wall were restored from the inside to the outside. The C-arm X-ray machine showed that the reset was satisfactory. The calcaneus plate screws were placed on the lateral wall of the calcaneus to fix it, and the sustentaculum tali screws were also implanted. During the operation, the C-arm X-ray machine showed good fracture reduction and fixation, and the position of the steel plate and the lengths of the screws were suitable. The wound was thoroughly rinsed, and bleeding was stopped; moreover, the equipment and gauze were counted. Negative pressure drainage was placed, and the subcutaneous tissue and skin were sequentially sutured. The dressing was valgus and pressure-wrapped, and the operation was completed (Figure 1).
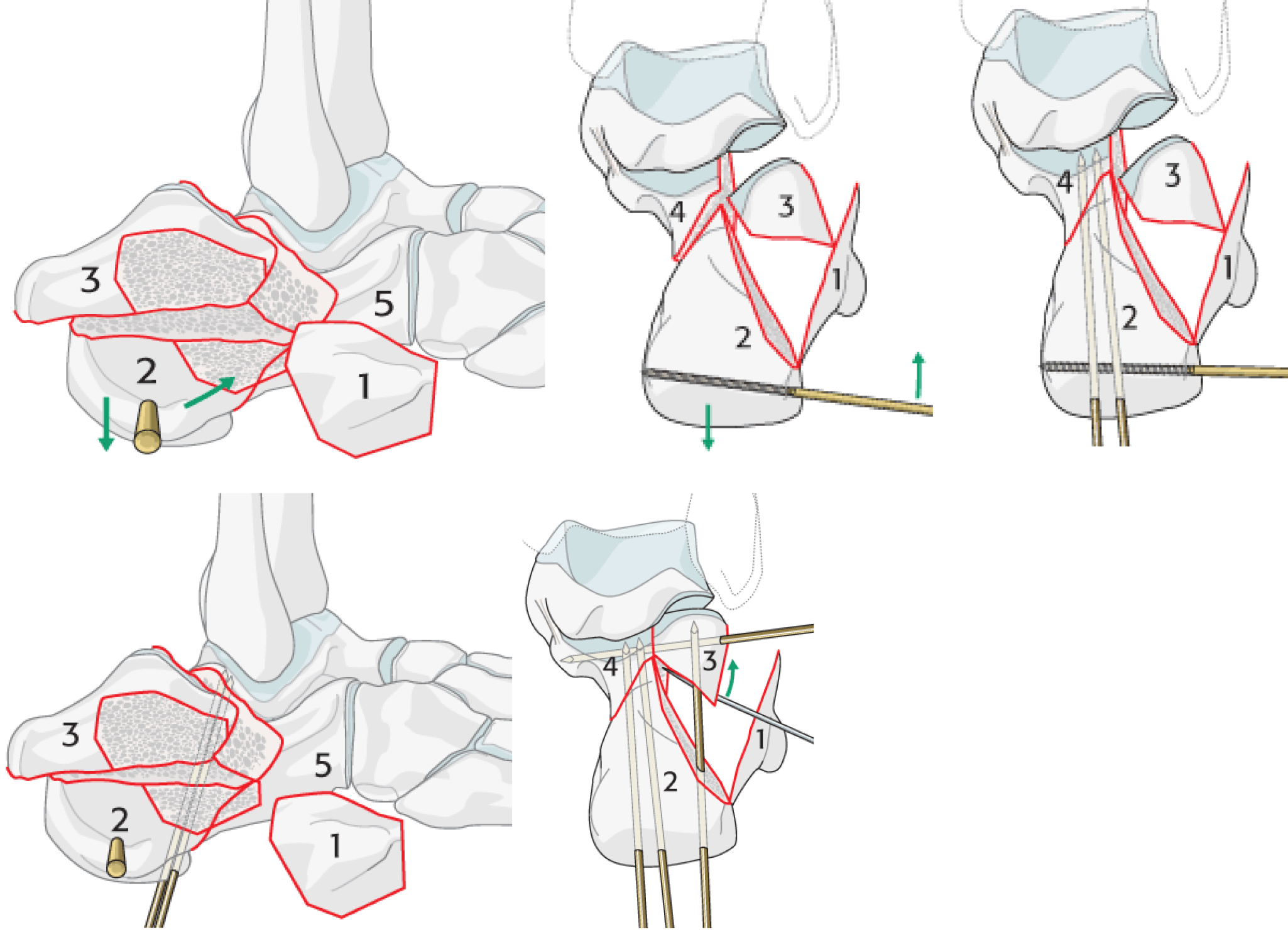
The preparation before cutting the skin was the same as described above. The external malleolus tip was placed at the base of the 4th tibia, and an incision approximately 5.0 cm long was made. The sural nerve was carefully identified and protected when cutting into the subcutaneous tissue. The peroneus longus and brevis were pulled to the metatarsal side, and the extensor muscle of the toes was partially removed and pulled to the dorsal side according to the exposure requirements. The tarsal sinus fat pad was bluntly isolated until the talus sinus was exposed. The lateral wall of the calcaneus was appropriately removed under the periosteum and opened outward. At the same time, the articular surface bone block was pulled to the outside to check whether the sustentaculum tali bone block had a displacement. If so, it was reset. The broken bone fragments in the fracture space were cleaned, and the articular surface was restored from the inside to the outside and temporarily fixed. A C-arm X-ray machine showed that the reset was satisfactory. A calcaneus plate screw was placed on the lateral wall of the calcaneus to fix it, and the screw was implanted percutaneously. The rest of the operation was the same as described above (Figure 2).
The affected foot was raised after surgery. Patients with significant pain were given analgesics. Antibiotics were routinely applied for 1 to 3 d. The incision drainage was removed 24 to 72 h after surgery. The incision was kept dry, and sutures were removed 12 to 14 d after surgery. Active toe exercise was started 24 h after surgery, and active flexion and extension exercises of the ankle joint began 1 wk later.
The calcaneus Böhler angle, Gissane angle, length, width, height, and step thickness of the articular surface were evaluated by X-ray and three-dimensional CT before and after surgery and at the last follow-up. Foot function recovery was assessed by the Maryland[4] foot scoring criteria. The score is 100 points, consisting of a 45-point pain assessment, a 40-point functional assessment, a 10-point appearance assessment, and a 5-point mobility assessment. Among them, functional assessment includes gait, walking distance, stability, support tools, limp, shoes, stairs, and ground requirements when walking.
The outcome of foot function recovery was evaluated as follows: Excellent (90 to 100 points), good (75 to 89 points), acceptable (50 to 74 points), and poor (< 50 points).
SPSS 16.0 was used to establish a database for parallel statistical analysis. The quantitative data are expressed as the mean and standard deviation. Two independent samples t-tests or t-tests (when the homogeneity of variance test was not homogeneous) were used to compare the preoperative and postoperative results. P < 0.05 was considered statistically significant, and the homogeneity test level was set at 0.1.
All patients were followed for 5 to 14 mo, with an average of 10.5 ± 2.9 mo. The fractures of all patients healed, and the healing time was 10 to 19 wk, with an average of 10.8 ± 1.5 wk. One patient developed wound infection 1 wk after surgery and was actively debrided and implanted with antibiotic calcium sulfate to control the infection. The patient’s fracture healed 5 mo after surgery. One patient developed sural nerve injury, and the symptoms disappeared 3 mo after surgery. The average Bohler angle was 13.3 ± 2.3° preoperatively and 31.5 ± 3.5° postoperatively. The average Gissane angle was 93.8 ± 3.5° preoperatively and 126.5 ± 10.3° postoperatively. The average calcaneal length was 79.5 ± 5.5 mm preoperatively and 77.8 ± 5.5 mm postoperatively; the average calcaneal width was 55.0 ± 10.0 mm preoperatively and 39.5 ± 8.8 mm postoperatively. The average calcaneal height was 32.5 ± 6.0 mm preoperatively and 45.8 ± 4.1 mm postoperatively. The average step thickness of the articular surface was 6.0 ± 3.0 mm preoperatively and 0.4 ± 0.5 mm postoperatively (Table 1). The patients were assessed according to the Maryland foot scoring system: Excellent in 77 cases, good in 10 cases, and acceptable in 4 cases. The excellent and good rate was 95.6%. The Department of Foot and Ankle Surgery, Central Hospital Affiliated with Shenyang Medical College, divides intra-articular calcaneal fractures into two types: Medial column displacement and non-displacement. In this study, there were 53 cases of medial column displacement, and the L-lateral incision of the calcaneus was used. There were 38 cases of medial column nondisplacement. The tarsal sinus incision was used to treat the articular surface and complete fixation (Figure 2). Satisfactory results were obtained. Therefore, this study confirmed that medial column classification can effectively guide the selection of surgical approaches for intra-articular calcaneal fractures, and the clinical efficacy of this classification in the treatment of intra-articular calcaneal fractures is positive.
| Timing | Böhler angle (°) | Gissane angle (°) | Calcaneal length (mm) | Calcaneal width (mm) | Calcaneal height (mm) | Step thickness of articular surface (mm) |
| Preoperative | 13.3 ± 2.3 | 93.8 ± 3.5 | 79.5 ± 5.5 | 55.0 ± 10.0 | 32.5 ± 6.0 | 6.0 ± 3.0 |
| Postoperative | 31.5 ± 3.5 | 126.5 ± 10.3 | 77.8 ± 5.5 | 39.5 ± 8.8 | 45.8 ± 4.1 | 0.4 ± 0.5 |
| Test statistics | -38.123 | -25.175 | 1.532 | 10.222 | -15.134 | 17.257 |
| P value | < 0.001 | < 0.001 | 0.095 | < 0.001 | < 0.001 | < 0.001 |
There are many types of treatments for calcaneal fractures, including conservative treatment, conventional surgical treatment, and minimally invasive surgery. The choice of specific treatment options is still controversial[5-9]. Open reduction and internal fixation are currently the most commonly used surgical procedures in the clinic. A good fracture reduction effect can be achieved by using the lateral extension incision of the calcaneus; however, many studies have reported a higher incidence of postoperative incision complications[10-14]. Some scholars[15,16] analyzed 21 studies including a total of 2046 patients with calcaneal fractures who underwent open reduction and internal fixation, and the average incidence of incision complications was 13.6%. We believe that incision complications depend on a number of factors, especially the surgeon's treatment experience[17]. The Department of Foot and Ankle Surgery, Central Hospital Affiliated to Shenyang Medical College, counted 101 patients with closed intra-articular calcaneal fractures who underwent L-incision treatment from January 2017 to July 2018. Only one case developed skin edge necrosis and was treated by flap transfer. One case developed wound infection and was actively debrided and implanted with antibiotic calcium sulfate to control the infection. The patient's fracture healed 5 mo after surgery.
In recent years, the minimally invasive concept has become a hot issue in the international surgical field. The use of the tarsal sinus incision as a surgical approach for the treatment of calcaneal fractures will become one of the popular trends[18,19].
The approach can effectively avoid damage to the related arteries and their branches[20], has less local damage to the skin, and thereby can reduce the risks of skin necrosis, wound infection, or flap pain after surgery[21] because its position is closer to the dorsum of foot, which has a richer blood supply for the soft tissues and looser surrounding skin. After the injury, it is usually not necessary to wait a long time to reduce swelling to perform surgery. Most patients can undergo surgery within 1 wk after the injury[22].
However, the focus of treatment for intra-articular calcaneal fractures is still the accurate reduction in fractures. Most scholars[23-25] believe that regardless of which treatment plan is adopted, the treatment goal needs a good recovery of the calcaneal anatomy. In most cases, poor calcaneus reduction results from poor reduction in the medial wall (column). Yao et al[26] reported that the poor reduction in the medial column after calcaneus fracture first caused unevenness of the subtalar articular surface. Whether the height of the medial column is lost or the width is not reset, the linear and positional alignment of the subtalar articular surface will be poor, and the biomechanical relationship between the talus and the calcaneus will be changed. Temporary reduction without firm fixation will result in insufficient stability of the medial column force line, often causing secondary reduction loss of the calcaneal medial column and resulting in varus deformity. The medial column is a component of the calcaneal height, width, and length, which also indirectly affects the Bohler angle and the Gissane angle of the calcaneus. Anatomic reduction and firm internal fixation of the medial column can reduce the incidence of varus deformity and facilitate the recovery of the width of the calcaneus. Compared with the height recovery of the lateral wall, the height recovery of the medial wall significantly reduces the incidence of varus deformity. Domestic scholars[27,28] used the medial auxiliary incision and distraction technique to improve the calcaneus width and further improve the postoperative outcome.
The AO Course and Mann's Surgery of the Foot and Ankle clearly indicate the order of reduction during surgical treatment of intra-articular calcaneal fractures (Figure 3): Remove or open the lateral articular surface bone block, loosen the main fracture line from the external upper to the internal lower part, pull the posterior nodule, reset and temporarily fix the posterior nodule and the sustentaculum tali bone block (accurate restoration of the medial column structure: Force line, calcaneus length, and width), and reset the articular surface (Figure 1). If the patient with a shortened medial column first undergoes articular surface reduction, the overall structural reduction is often poor, and this operation is difficult to achieve in the tarsal sinus incision. For patients with no displacement of the medial column, the articular surface can be directly restored, and the tarsal sinus incision is feasible.
Although there are many methods for the classification of intra-articular calcaneal fractures, it is generally believed that[17] the CT classification proposed by Sanders has high application value in the selection of treatment methods and prognosis of calcaneal fractures. However, this method has no clear guiding significance for the choice of surgical incision and surgical plan. At present, most scholars[14] suggest that the tarsal sinus incision can be used for Sanders Types II and III fractures. However, for Sanders Types II and III fractures with medial column shortening, the use of the tarsal sinus incision cannot effectively release the main fracture line and accurately restore the positional relationship between the sustentaculum tali bone block and the posterior nodule backbone.
In view of the above issue, the Department of Foot and Ankle Surgery, Central Hospital Affiliated with Shenyang Medical College preliminarily divided intra-articular calcaneal fractures into two types: Medial column displacement (shortened varus) and nondisplacement. In this study, there were 53 cases of medial column displacement (shortened varus), and the L-lateral incision of the calcaneus was used. First, the main fracture line was released, the posterior nodule and the sustentaculum tali bone block were reset to restore the medial wall (column), and then the articular surface was restored (Figures 1 and 3). There were 38 cases of medial column nondisplacement. The tarsal sinus incision was used to treat the articular surface and complete fixation (Figure 2), because there was no need to remove the articular surface bone block and to release the main fracture line. Satisfactory results were obtained. The patients were followed after initial use of this type of treatment. X-ray and CT examinations showed that the Böhler angle recovered to 31.5 ± 3.5°, the Gissane angle recovered to 126.5 ± 10.3°, the calcaneal length recovered to 77.8 ± 5.5 mm, the width recovered to 39.5 ± 8.8 mm, the height recovered to 45.8 ± 4.1 mm, and the step thickness of the articular surface recovered to 0.4 ± 0.5 mm. The good and excellent rate was 95.6% according to the Maryland foot scoring system. Therefore, medial column classification can effectively guide the surgical selection of intra-articular fractures of the calcaneus.
The main shortcomings of this study are that the number of cases is small and the follow-up time is short. The early efficacy is satisfactory; however, the long-term efficacy needs further follow-up. Second, the authors were good at using the tarsal sinus incision, and the Sanders Types III and IV fractures without medial column displacement were all treated with this incision. Moreover, the classification is only an initial attempt and has not been refined. We will accumulate additional cases, improve the controlled study, and continue to follow the patients to obtain relatively scientific conclusions.
The Sanders computed tomography classification of calcaneal fractures cannot guide the surgical treatment.
We tried to study a new classification to guide the surgical treatment of calcaneal fractures.
In this study, we aimed to explore the application and clinical efficacy of medial column classification in the treatment of intra-articular calcaneal fractures.
We divided intra-articular calcaneal fractures into two types: Medial column displacement (shortened varus) and nondisplacement. There were 53 cases of medial column displacement, and the L-lateral incision of the calcaneus was used. First, the main fracture line was released, the posterior nodule and the sustentaculum tali bone block were reset to restore the medial wall (column), and then the articular surface was restored.
The incidence of tarsal sinus incision failure in this type of calcaneal fracture is high. There were 38 cases of medial column nondisplacement, and the tarsal sinus incision was used. Satisfactory results were obtained.
Medial column classification can effectively guide the surgical selection of intra-articular fractures of the calcaneus.
We will accumulate additional cases, improve the controlled study, and continue to follow the patients to obtain relatively scientific conclusions.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kim ES S-Editor: Wang JL L-Editor: Wang TQ P-Editor: Wu YXJ
| 1. | Clare MP, Sanders RW. [Calcaneus fractures]. Unfallchirurg. 2011;114:869-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Spierings KE, Sanders FRK, Nosewicz TL, Schepers T. Risk factors for surgical site infections with the Sinus Tarsi Approach in displaced intra-articular calcaneal fractures; a prospective cohort study with a minimum of one year follow-up. Injury. 2020;51:1676-1680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Shi ZM, Gu WQ. Surgical management of intra-articular calcaneal fractures: our misunderstandings. Zhonghua Yixue Zazhi. 2019;99:1604-1607. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;87-95. [PubMed] |
| 5. | Giannini S, Cadossi M, Mosca M, Tedesco G, Sambri A, Terrando S, Mazzotti A. Minimally-invasive treatment of calcaneal fractures: A review of the literature and our experience. Injury. 2016;47 Suppl 4:S138-S146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Yu X, Pang QJ, Chen L, Yang CC, Chen XJ. Postoperative complications after closed calcaneus fracture treated by open reduction and internal fixation: a review. J Int Med Res. 2014;42:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Guerado E, Bertrand ML, Cano JR. Management of calcaneal fractures: what have we learnt over the years? Injury. 2012;43:1640-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Cao L, Weng W, Song S, Mao N, Li H, Cai Y, Zhou Q, Su J. Surgical treatment of calcaneal fractures of Sanders type II and III by a minimally invasive technique using a locking plate. J Foot Ankle Surg. 2015;54:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Agren PH, Wretenberg P, Sayed-Noor AS. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2013;95:1351-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 149] [Article Influence: 12.4] [Reference Citation Analysis (1)] |
| 10. | Luo X, Li Q, He S, He S. Operative Versus Nonoperative Treatment for Displaced Intra-Articular Calcaneal Fractures: A Meta-Analysis of Randomized Controlled Trials. J Foot Ankle Surg. 2016;55:821-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Benirschke SK, Kramer PA. Wound healing complications in closed and open calcaneal fractures. J Orthop Trauma. 2004;18:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 169] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 12. | Zhang G, Ding S, Ruan Z. Minimally invasive treatment of calcaneal fracture. J Int Med Res. 2019;47:3946-3954. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Haapasalo H, Laine HJ, Mäenpää H, Wretenberg P, Kannus P, Mattila VM. Epidemiology of calcaneal fractures in Finland. Foot Ankle Surg. 2017;23:321-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Sanders R, Vaupel ZM, Erdogan M, Downes K. Operative treatment of displaced intraarticular calcaneal fractures: long-term (10-20 Years) results in 108 fractures using a prognostic CT classification. J Orthop Trauma. 2014;28:551-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 124] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 15. | Rubino R, Valderrabano V, Sutter PM, Regazzoni P. Prognostic value of four classifications of calcaneal fractures. Foot Ankle Int. 2009;30:229-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Caranci F, Briganti F, La Porta M, Antinolfi G, Cesarano E, Fonio P, Brunese L, Coppolino F. Magnetic resonance imaging in brachial plexus injury. Musculoskelet Surg. 2013;97 Suppl 2:S181-S190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Cui J, Zheng G, Li X. The tarsal sinus incision reduction and percutaneous plate internal fixation for Sanders II, III calcaneal fractures. Zhongguo Linchuang Yisheng Zazhi. 2019;47:319-320. [DOI] [Full Text] |
| 18. | Di Zazzo E, Porcile C, Bartollino S, Moncharmont B. Critical Function of PRDM2 in the Neoplastic Growth of Testicular Germ Cell Tumors. Biology (Basel). 2016;5:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Yu T, Xiong Y, Kang A, Zhou H, He W, Zhu H, Yang Y. Comparison of sinus tarsi approach and extensile lateral approach for calcaneal fractures: A systematic review of overlapping meta-analyses. J Orthop Surg (Hong Kong). 2020;28:2309499020915282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Ronco V, Potenza DM, Denti F, Vullo S, Gagliano G, Tognolina M, Guerra G, Pinton P, Genazzani AA, Mapelli L, Lim D, Moccia F. A novel Ca²+-mediated cross-talk between endoplasmic reticulum and acidic organelles: implications for NAADP-dependent Ca²+ signalling. Cell Calcium. 2015;57:89-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 21. | Seat A, Seat C. Lateral Extensile Approach Versus Minimal Incision Approach for Open Reduction and Internal Fixation of Displaced Intra-articular Calcaneal Fractures: A Meta-analysis. J Foot Ankle Surg. 2020;59:356-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Lin J, Xie C, Chen K, Sun S, Zhou K, Zhou C, Shui X, Kong J. Comparison of sinus tarsi approach versus extensile lateral approach for displaced intra-articular calcaneal fractures Sanders type IV. Int Orthop. 2019;43:2141-2149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Dürr C, Apinun J, Mittlmeier T, Rammelt S. Foot Function After Surgically Treated Intraarticular Calcaneal Fractures: Correlation of Clinical and Pedobarographic Results of 65 Patients Followed for 8 Years. J Orthop Trauma. 2018;32:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Biz C, Barison E, Ruggieri P, Iacobellis C. Radiographic and functional outcomes after displaced intra-articular calcaneal fractures: a comparative cohort study among the traditional open technique (ORIF) and percutaneous surgical procedures (PS). J Orthop Surg Res. 2016;11:92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Kiewiet NJ, Sangeorzan BJ. Calcaneal Fracture Management: Extensile Lateral Approach Versus Small Incision Technique. Foot Ankle Clin. 2017;22:77-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Yao GJ, Shang J, Wang W. Effect of inadequate reduction of medial wall on the postoperative varus deformity following calcaneal fracture surgery and other influencing factors of varus deformity. Zhonghua Chuangshang Guke Zazhi. 2016;18:465-469. [DOI] [Full Text] |
| 27. | Yu T, Yang Y, Li B, Sah S, Chen K, Yu G. Importance of assistant intra-operative medial distraction technique for intraarticular calcaneus fractures. Acta Orthop Belg. 2019;85:130-136. [PubMed] |
| 28. | Chen J, Yang Z, Kong C, Wei S. Minimally invasive dual incision with mini plate internal fixation improves outcomes over 30 months in 20 patients with Sanders type III calcaneal fractures. J Orthop Surg Res. 2020;15:167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |