Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4215
Peer-review started: April 2, 2020
First decision: April 24, 2020
Revised: April 27, 2020
Accepted: August 27, 2020
Article in press: August 27, 2020
Published online: September 26, 2020
Processing time: 172 Days and 16.8 Hours
Giant multilocular cystadenoma (GMC) of the prostate gland is a very rare benign tumor. Although the benign nature has been known, complete surgical excision is the major treatment consensus because of its high recurrence rate. We report a rare case of GMC with accompanying lower urinary tract symptoms and repeated urine retention initially thought to be symptoms of benign prostatic hyperplasia, which was treated with robot-assisted laparoscopic radical prostatectomy.
A 65-year-old man presented with a 2-year history of lower urinary tract symptoms that had deteriorated gradually within the previous six months, even though he had received treatment with a selective alpha-blocking agent. He had undergone two transurethral resections of the prostate (TURP) at a local hospital during a 4-mo interval because initial ultrasound imaging and prostatic core needle biopsy showed benign prostate hyperplasia. Upon the third recurrence, the patient underwent TURP with a green-light laser at our institution. The diagnosis was a tumor composed of variously sized dilated glandular and cystic structures lined by blended prostatic type epithelia positive for prostate-specific antigen; the final diagnosis was giant multilocular cystadenoma. Magnetic resonance imaging showed a large multilocular retrovesical mass 8.0 cm × 7.3 cm × 6.4 cm, with heterogeneous enhancement. A coexisting malignant part could not be excluded. Considering the high recurrence rate, risk of coexisting malignancy, and possible sequelae of open surgery for radical excision, the patient decided to undergo robot-assisted radical prostatectomy, with good outcomes at the 2-year follow-up.
Robot-assisted surgery for the treatment of prostate GMC provides another choice for simultaneous attention to disease-control and postoperative quality of life.
Core Tip: Giant multilocular cyst adenoma (GMC) of the prostate is a rare benign tumor without specific clinical manifestations that can easily be misdiagnosed as BPH due to obstructive urinary symptoms. We recommend individualized treatment of this rare tumor and provide our experience in the first case of prostatic GMC treated with robot-assisted radical prostatectomy that resulted in a good outcome.
- Citation: Fan LW, Chang YH, Shao IH, Wu KF, Pang ST. Robotic surgery in giant multilocular cystadenoma of the prostate: A rare case report. World J Clin Cases 2020; 8(18): 4215-4222
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4215.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4215
Giant multilocular cystadenomas (GMC) are extremely rare benign tumors that originate in the prostate, less frequently in the seminal vesicles[1] and Cowper’s glands[2]. So far, there are still no more than 30 cases reported, according to our latest review[3]. It can occur at any age; the age of patients ranges from 23[4] to 80 years[5]. The tumors are characterized as multiple loculated cysts that vary in size and morphology, usually presenting with obstructive urinary or lower intestinal tract symptoms rather than other complaints, and the prostate-specific antigen (PSA) level may or not be high. Transrectal ultrasound (TRUS) is usually performed as the initial line of investigation, which shows a huge prostate gland with heterogeneous architecture and multiple small to large cystic lesions. This condition is easily misdiagnosed initially as benign prostate hyperplasia with multiple cysts if the physician does not anticipate GMC. It is difficult to make the exact diagnosis preoperatively, and determining the therapeutic strategy is a challenge to both the radiologists and urologists alike[6]. Even if there is no invasive/infiltrating pattern in further imaging studies like computed tomography or magnetic resonance imaging, the possibility of malignancy of this huge pelvic tumor cannot be completely excluded. Currently, complete surgical excision is the consensus for treatment in most case reports.
We present a case of GMC of the prostate in a 64-year-old man who initially presented with lower urinary tract symptoms and several GMC recurrences until finally undergoing robot-assisted radical prostatectomy. To our knowledge, this case is the first reported case describing robot-assisted radical prostatectomy without lymph node dissection for recurrent GMC of the prostate.
The patient suffered from recurrent difficulty in voiding and urine retention even underwent surgical intervention for about half-a-year.
A 65-year-old Asian man presented with difficulty voiding for about 2 years that deteriorated gradually within 6 mo even if received treatment with selective alpha-blocker agent. He visited a local hospital for first aid in 2016. In addition, dry ejaculation has also disturbed for more than one year before medical intervention. The patient did not complain about any episode of hematuria, fever, or loss of weight. TRUS showed an estimated volume of 230 cm3, irregular shape with heterogeneous echotexture, and multiple cysts. A systemic core needle biopsy revealed nodular hyperplasia with inflammation and some atypical glands but no evidence of malignancy. Because of the former failed medical treatments and the recurrent weak urinary stream and urine retention, two transurethral resections of the prostate (TURP) were undertaken during a short 4-month interval (April and July 2016). Both pathology reports revealed nodular hyperplasia and chronic prostatitis with a few atypical glands weighing 5.3 g and 5.2 g, respectively. No malignancy was identified by immunohistochemistry (IHC) staining.
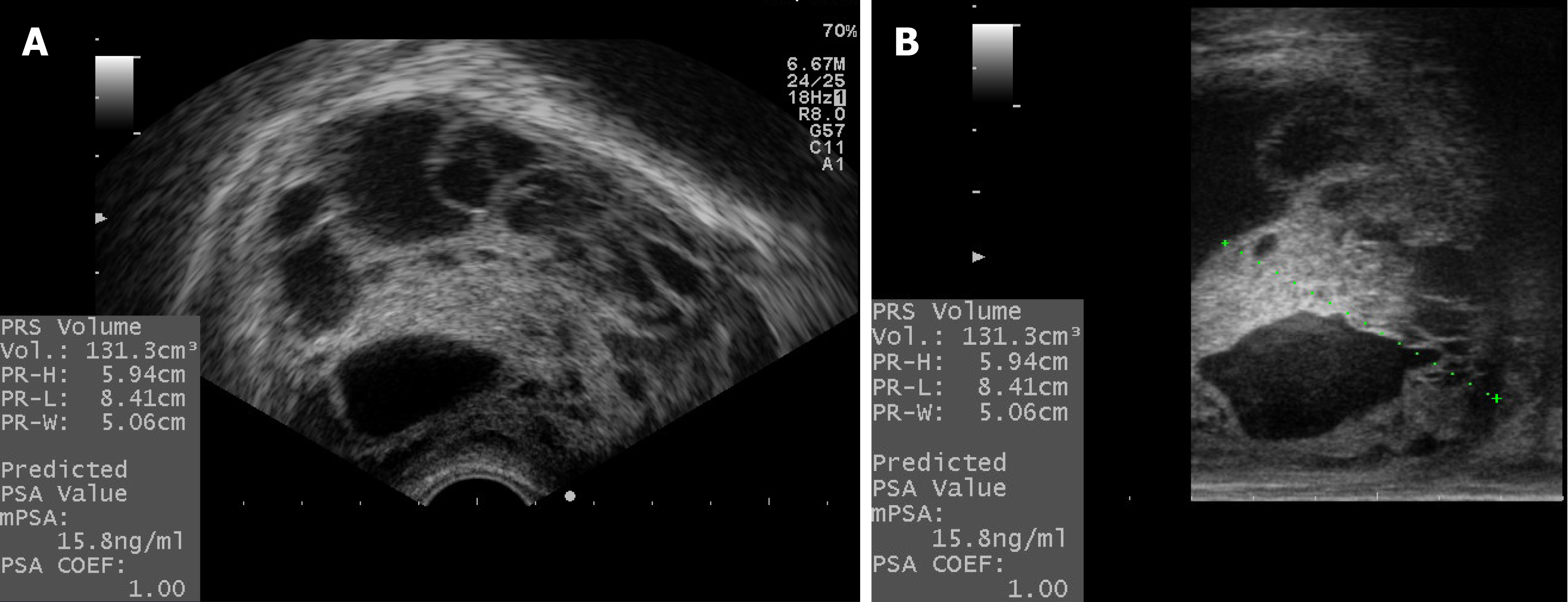
However, the patient continued to have gradually deteriorating obstructive voiding symptoms and acute urine retention for 6 months, even with 5-alpha reductase and alpha-blocker treatment. Therefore, he came to our tertiary hospital and underwent a laser prostatectomy (green-light XPS), with the consideration of TRUS still showing a huge residual prostate gland with an estimated volume of 131.3 cm3 and uroflowmetry disclosing a low peak flow and an average flow rate with a large postvoid residual urine volume. The pathology report on the resected tissues revealed multilocular cystadenoma of the prostate. Nonetheless, the patient experienced progressive difficulty in voiding 1 year after the laser prostatectomy, although the PSA levels were within the range of 4-6 ng/mL.
He had been healthy before the low urinary tract symptoms developed.
He has no habit of alcohol drinking or cigarette smoking and no specific family history.
A digital rectal examination revealed a huge elastic prostate with rectal compression, and no tender or palpable induration was noted.
A baseline biochemistry profile at presentation showed a high PSA level (13.0 ng/mL), with an otherwise normal biochemistry profile. Urinalysis was normal, with no evidence of hematuria. During the period of follow-up at our hospital from August 2016 to January 2018, the PSA levels were within the range of 4-6 ng/mL.
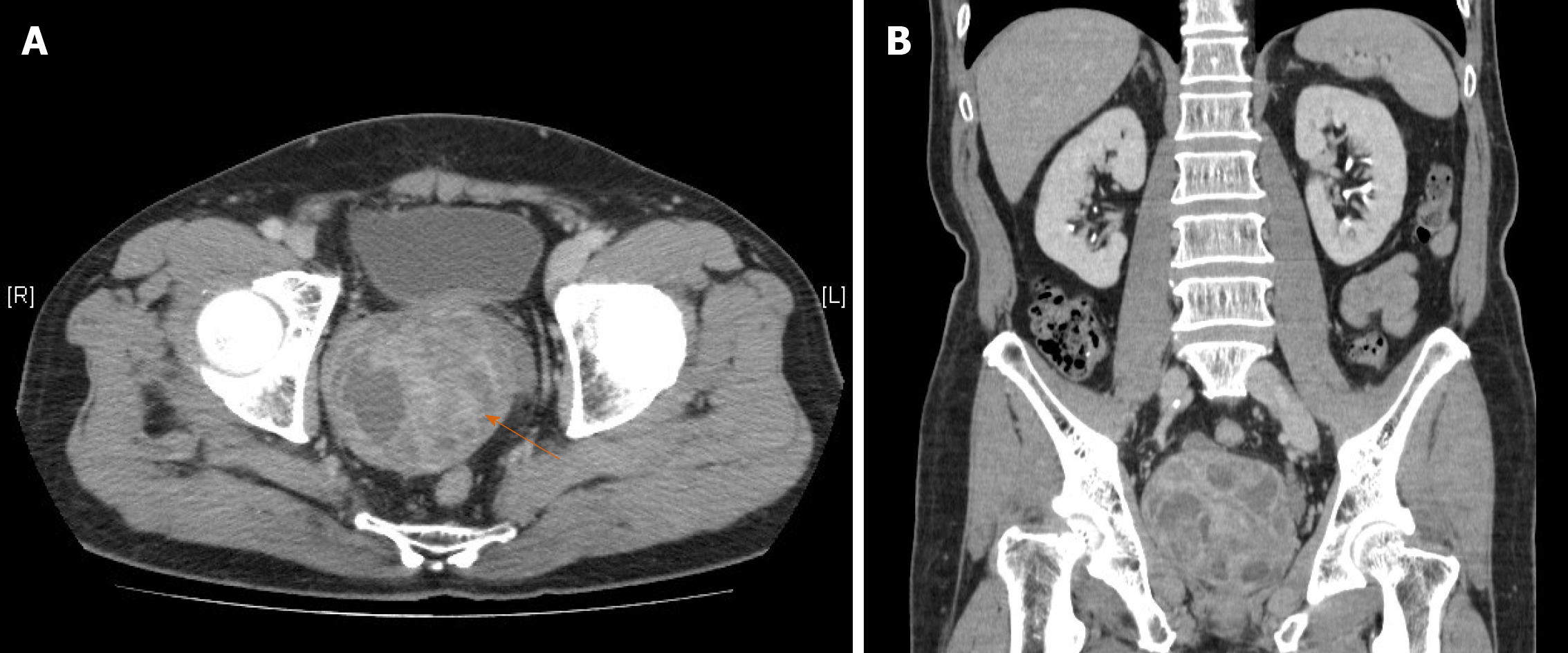
In 2016, computed tomography (CT) of the abdomen and pelvis (Figure 1) at local hospital showed an 8.2 cm × 8.1 cm × 7.8 cm multiloculated cystic prostate gland with several enhanced focal lesions. At our hospital, TRUS still showed a huge residual prostate gland with an estimated volume of 131.3 cm3 (Figure 2) even after twice TURPs at previous hospital. A subsequent magnetic resonance imaging (Figure 3) showed a large multilocular retrovesical mass, 8.0 cm × 7.3 cm × 6.4 cm, with solid parts and heterogeneous enhancement, a coexisting malignant part of the tumor, either a cystadenocarcinoma or prostate intraepithelial neoplasm should be suspected, but there were no enlarged pelvic lymph nodes.
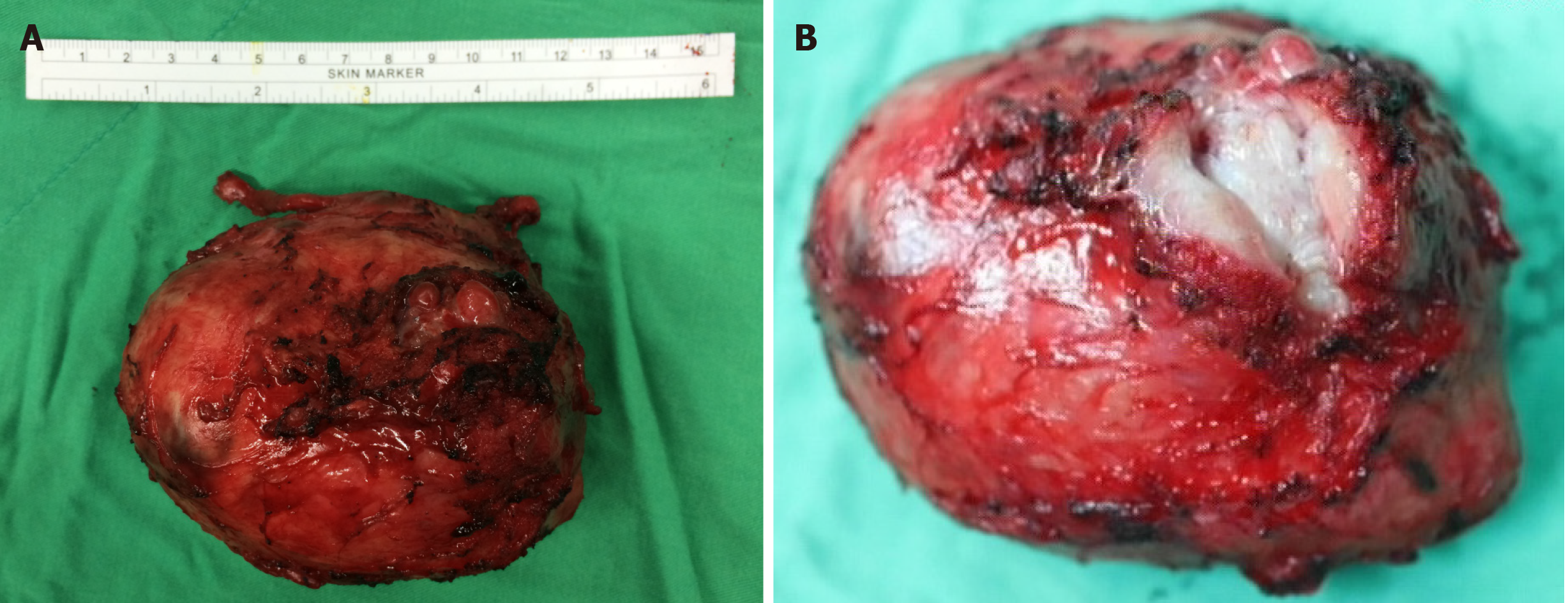
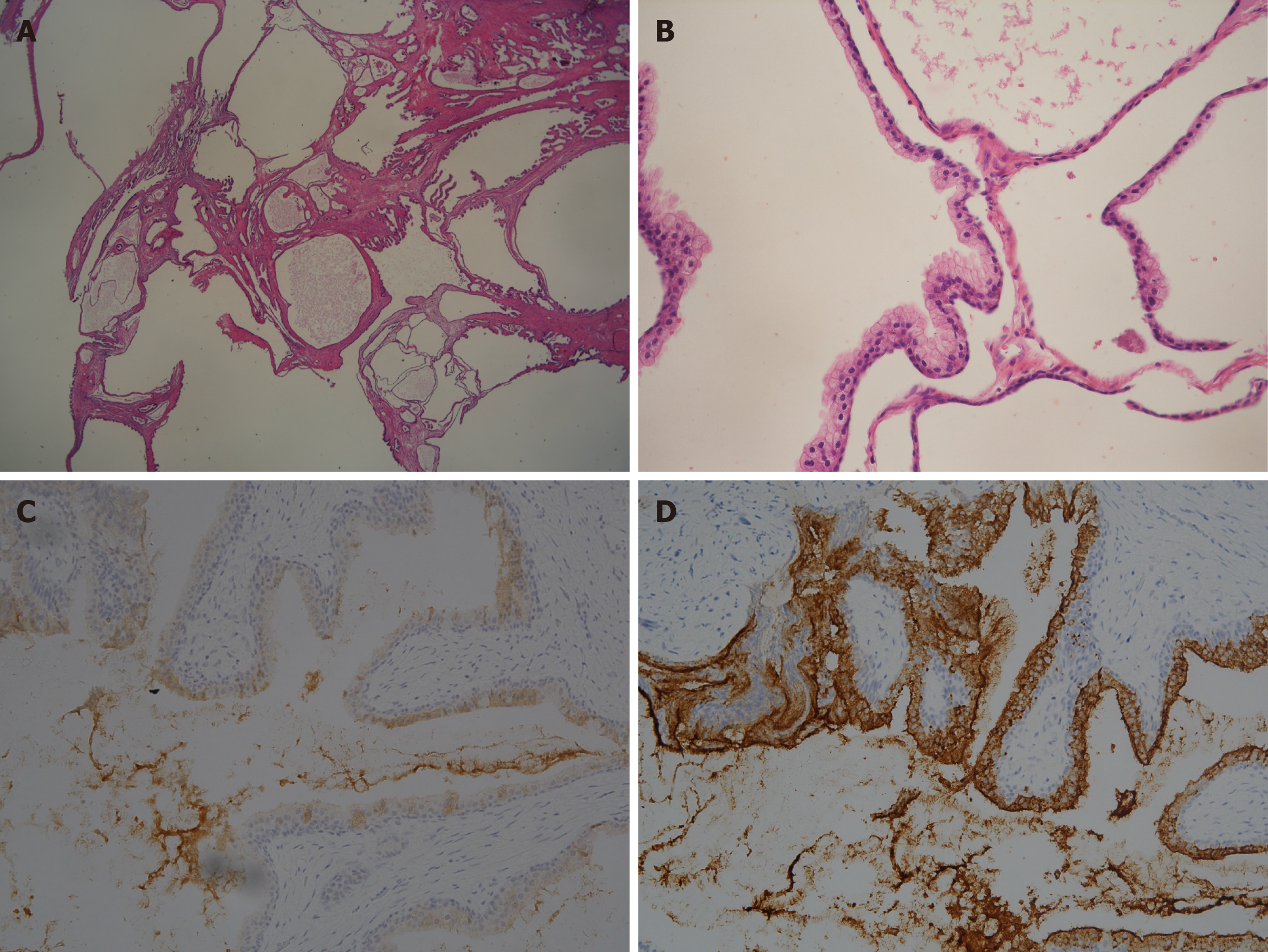
The gross prostate specimen was a solid mass 11.1 cm × 8.2 cm × 7.1 cm in size, weighing 245 g, and was almost entirely replaced by a multilocular cystic tumor (Figure 4). The tumor was nonencapsulated, with mutilocular cysts with focal hemorrhage, watery contents, and smooth cyst walls. There was no grossly invasive focus. Histologically (Figure 5), the tumor was composed of variously sized dilated glandular and cystic structures lined by blended prostatic type epithelia. Foci of florid papillary infoldings were seen in the large cysts. Focal squamous metaplasia was seen. There was fibromuscular stroma with focal adipose metaplasia. In addition, there were no atypical features or mitosis observed. The lining epithelia were positive for PSA, PSMA, CK7, and MUC2. The epithelia were negative for CDX2, CK20, MUC1, and MUC5ac on immunohistochemical staining, indicating that the tumor originated from the prostate. Final pathology indicated a giant multilocular prostatic cystadenoma.
Giant multilocular cystadenoma of prostate.
With the concerns of several recurrences, the possibility of a hidden malignancy could not be ruled out by the partially resected prostate tissue and imaging studies. Whether or not cystadenoma is a precursor of cystadenocarcinoma, we recommended radical prostatectomy after discussing these possibilities with the patient. Considering the preservation of continence and sexual function, the patient underwent transperitoneal robot-assisted radical prostatectomy without pelvic lymph node dissection. We excised the huge prostate intact, including the bilateral seminal vesicles (Figure 3), with sparing of the bilateral neurovascular bundles. Following urethrovesical anastomosis was performed with Fr. 16 silicon urethral catheter indwelled for one week.
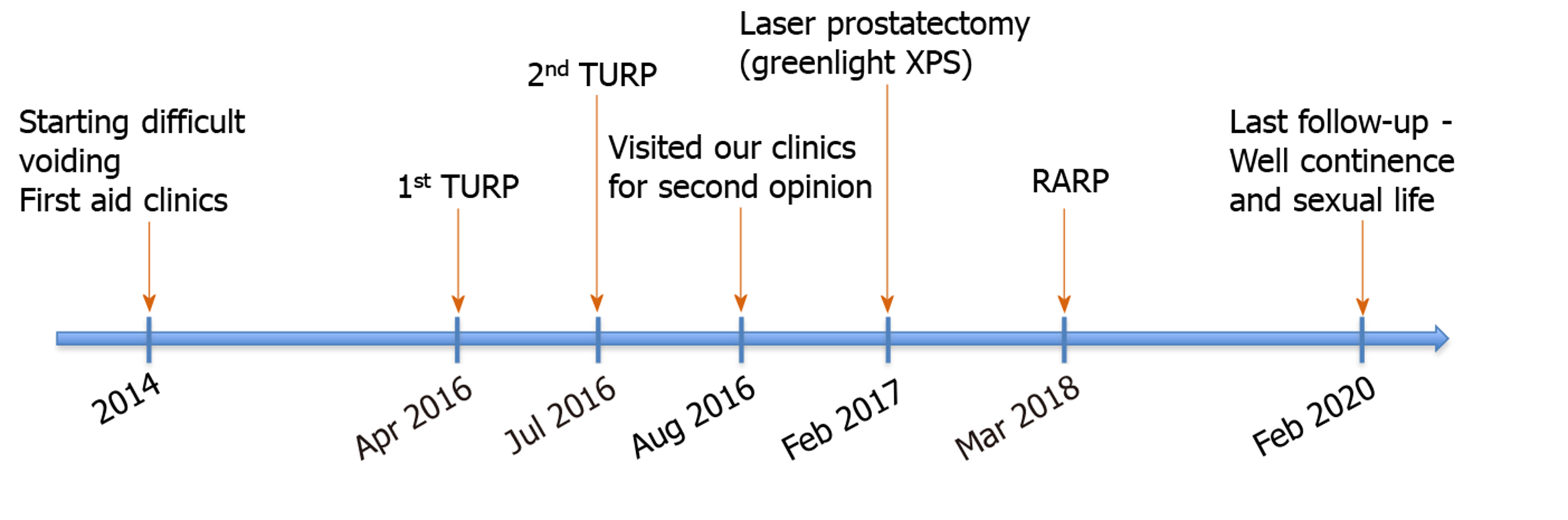
At follow-up 6 mo later, the patient remained free of lower urinary tract symptoms, except for mild stress urinary incontinence without the necessary of pad or diaper, and there were no signs of recurrence. Blood serum PSA level was lesser than 0.008 ng/mL, and uroflowmetry showed a normal urinary flow rate with minimal post-void residual urine. Although the patient complained of mild erectile dysfunction, it could improve, and he could proceed with intercourse with the help of a phosphodiesterase type 5 inhibitor (sildenafil). The patient was totally asymptomatic at the 2-year follow-up visit and made a good recovery with no complaints of any urinary disorders or sexual dysfunction. The timeline of the patient's treatment (Figure 6).
Giant multilocular prostatic cystadenoma is a rare benign neoplasm of the prostate gland with fewer than 30 reported cases since Maluf et al[7] first described it and designated it the rare entity in 1991, even including several previous reports without complete comprehension and precise descriptions of such multilocular cystic tumors of the prostate[8]. Obstructive voiding symptoms occurred in almost all reported cases. These lesions do not invade adjacent structures, and therefore, a preoperative radiologic evaluation can define the benign nature of the lesion[4].
Histologically, these lesions resemble benign prostate tissue, typically containing prostatic glands and cysts lined by benign cuboidal to columnar acinar cells with a distinct basal cell layer, lack of intracystic papillary pattern or neighboring structures infiltrating growth. PSA is positive in epithelial cells by immunohistochemical staining[9]. Interestingly, it is still unclear about the relationship between cystadenoma and cystadenocarcinoma, whether cystadenoma is a precursor of cystadenocarcinoma or not[10]. Both benign and malignant epithelial cystic tumors of the prostate may present with massive cystic pelvic tumors and cause urinary and lower intestinal tract compressive symptoms. Additionally, the PSA level was not proportionally related to the mass volume[11] or malignant risk[10], according to the past few documented cases. To date, no prior reports have confirmed a diagnosis of multilocular prostatic cystadenoma by core needle biopsy preoperatively. To distinguish between benign or malignant tumors, we can only identify a malignancy through radiographically invasive behavior or through the final pathology study of the resected specimen. Based on our experience with this patient, both imaging studies and histological reports from TURP specimens could easily lead to misdiagnosis because physicians lack experience with this rare neoplasm.
In a review of the previous literature on such cases, several treatment modalities for giant multilocular prostatic cystadenoma have been reported, including conservative treatment such as gonadotropin-releasing hormone (GnRH) antagonist[12], transurethral resection[13] or enucleation of the prostate, laparoscopic cyst resection[14], partial or complete tumor resection, even radical prostatectomy or pelvic exenteration. For now, the general consensus of management is complete surgical excision. However, looking into the different treatments in each case, a single treatment modality does not seem suitable for every case of GMC. Only one study reported that a GnRH antagonist was effective for the treatment of recurrent GMC of the prostate, and it was not feasible for that patient to undergo invasive surgery. Nonetheless, no recurrences were reported during the different follow-up periods reported in patients who underwent TURP[13] and cyst resection[14]. Furthermore, in most known situations, incomplete resection could result in recurrence despite the benign nature of the tumor. In addition, some prior patients underwent radical cystoprostatectomy, pelvic exenteration, or en bloc excision with adjacent organ sacrifice because of clinical suspicion of malignancy or severe adhesions to surrounding structures. How to achieve the balance of treatment choice and find the appropriate management for each patient is the main consideration of every clinician. We provide our recommendation based on our experience with the location and morphology of the tumor, the possibility of malignant change (elevation of PSA or highly suspicious imaging studies), and a review of the previously published literature. If there is no evidence or likelihood of malignancy and the tumor is mostly composed of multiple large cysts, simple resection or unroofing of the cysts may be considered. Similarly, if the tumor looks benign and arises from the posterior or superior side of the prostate gland and protrudes, even with an obvious stalk, complete tumor excision without prostate urethra destruction is an appropriate treatment choice. Nonetheless, if the prostate gland is almost entirely replaced by cystic tumor morphology and malignancy cannot be ruled out clinically, like in this case, radical prostatectomy is a reasonable treatment modality.
Multilocular prostatic cystadenomas are reported in men that are relatively young adults (mean age, 50 years; range, 23-80 years). Perioperative complications, postoperative pain, duration of convalescence, urinary continence, and sexual function would be important concerns in such patients. Nerve-sparing radical prostatectomy would be the better option to accomplish good disease-control with minimal recurrence, especially in cases with potential malignancy risk, as well as better functional outcomes with a lower risk of urinary incontinence or erectile dysfunction than with conventional radical prostatectomy or pelvic exenteration.
Our limited experience with treatment options in cases of such rare tumors may confine our treatment choice. Only one article has reported a minimally invasive approach with transperitoneal laparoscopic resection of cysts without complete tumor excision[14]. With the advancement of medical technology, robotic surgery has become more popular thanks to its clear three-dimensional visualization, navigation, and precise operation. We share our experience and intraoperative video of robot-assisted treatment of a huge tumor originating from the prostate gland, along with concern over a coexisting malignancy.
We performed a standard robot-assisted radical prostatectomy intraperitoneally through five trocars (12-mm supra-umbilical camera, 8-mm right medial monopolar curved scissor, 8-mm left medial Maryland bipolar forceps, 8-mm left lateral fenestrated bipolar forceps, and 12-mm right lateral assistant pole), with the patient in a steep Trendelenburg position. First, we started a posterior approach with a transverse incision made in the Denonvilliers fascia below the seminal vesicles, and blunt dissection was used to develop a plane between the posterior prostate and the rectum. Dissection of the seminal vesicles and vasa deferentia followed. Directly dissecting toward the prostatic apex was difficult because of the huge tumor mass. We then developed the space of Retzius and opened the endopelvic fascia. After ligation of deep dorsal venous complex, the bladder neck was identified and transected widely without neck preservation. The tumor was so massive that we had to first control each side prostate pedicle to preserve the neurovascular bundle (NVB). We dissected the Denonvilliers fascia caudally to create a space and identified the other side of the NVB. In turn, we developed the interfascial plane of dissection, released the NVBs in the standard fashion and preserved the cavernous nerves as carefully as possible. After completely freeing prostate en bloc, a vesicourethral anastomosis was performed, with a silicone urethral catheter placed and bladder neck reconstruction longitudinally rather than transversely. Pelvic lymph node dissection was not performed because of negative imaging findings. Some extremely large tumors are not suitable for robotic surgery.
In conclusion, GMC of the prostate is a rare benign tumor without specific clinical manifestations that can easily be misdiagnosed as BPH due to obstructive urinary symptoms. When a large multilocular cystic lesion arising between the pubis and the rectum in men with lower urinary tract symptoms, GMC should be considered in the differential diagnosis. Regardless of whether or not cystadenoma is a precursor of cystadenocarcinoma and has different tumor growth patterns in each case, we recommend individualized treatment of this rare tumor. In properly selected cases, the tumor in moderate size for fear of malignant change or potential in a relatively young male with concerns of urinary continence and sexual function, robotic assistance radical prostatectomy would be the appropriate choice of treatment. This is the first case of prostatic GMC treated with robot-assisted radical prostatectomy that resulted in a good outcome.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang XQ S-Editor: Gong ZM L-Editor: A P-Editor: Wang LL
| 1. | Lorber G, Pizov G, Gofrit ON, Pode D. Seminal vesicle cystadenoma: a rare clinical perspective. Eur Urol. 2011;60:388-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 2. | Villeda-Sandoval CI, Romero-Vélez G, Lisker-Cervantes A, Zavaleta MS, Trolle-Silva A, Oca DM, Castillejos-Molina R. Giant multicystic cystadenoma of Cowper's gland: a case report. Int Braz J Urol. 2013;39:741-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Nakamura Y, Shida D, Shibayama T, Yoshida A, Matsui Y, Shinoda Y, Iwata S, Kanemitsu Y. Giant multilocular prostatic cystadenoma. World J Surg Oncol. 2019;17:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Olgun DC, Onal B, Mihmanli I, Kantarci F, Durak H, Demir H, Cetinel B. Giant multilocular cystadenoma of the prostate: a rare cause of huge cystic pelvic mass. Korean J Urol. 2012;53:209-213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Watanabe J, Konishi T, Takeuchi H, Tomoyoshi T. [A case of giant prostatic cystadenoma]. Hinyokika Kiyo. 1990;36:1077-1079. [PubMed] |
| 6. | El-Asmar JM, Saade C, Dergham MYR, Degheili JA. Multimodality approach to imaging giant multilocular cystadenoma of the prostate: A rare entity. Radiol Case Rep. 2019;14:1117-1122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Maluf HM, King ME, DeLuca FR, Navarro J, Talerman A, Young RH. Giant multilocular prostatic cystadenoma: a distinctive lesion of the retroperitoneum in men. A report of two cases. Am J Surg Pathol. 1991;15:131-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Hauck EW, Battmann A, Schmelz HU, Diemer T, Miller J, Weidner W, Knoblauch B. Giant multilocular cystadenoma of the prostate: a rare differential diagnosis of benign prostatic hyperplasia. Urol Int. 2004;73:365-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Chowdhury MM, Abdulkarim JA. Case report. Multilocular cystadenoma of the prostate presenting as a giant pelvic mass. Br J Radiol. 2009;82:e200-e201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Paner GP, Lopez-Beltran A, So JS, Antic T, Tsuzuki T, McKenney JK. Spectrum of Cystic Epithelial Tumors of the Prostate: Most Cystadenocarcinomas Are Ductal Type With Intracystic Papillary Pattern. Am J Surg Pathol. 2016;40:886-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Park JP, Cho NH, Oh YT, Choi YD. Giant multilocular prostatic cystadenoma presenting with obstructive aspermia. Yonsei Med J. 2007;48:554-556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Datta MW, Hosenpud J, Osipov V, Young RH. Giant multilocular cystadenoma of the prostate responsive to GnRH antagonists. Urology. 2003;61:225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Loizaga A, Arceo R, Ullate V, Unda M, Flores N. [Lateral cysts of the prostate]. Actas Urol Esp. 1994;18:612-614. [PubMed] |
| 14. | Abed El Rahman D, Zago T, Verduci G, Baroni G, Berardinelli ML, Pea U, Morandi E, Castoldi M. Transperitoneal laparoscopic treatment for recurrence of a giant multilocular prostatic cystadenoma: A case report and review of the literature. Arch Ital Urol Androl. 2016;88:66-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |