Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4186
Peer-review started: April 25, 2020
First decision: May 15, 2020
Revised: May 15, 2020
Accepted: August 20, 2020
Article in press: August 20, 2020
Published online: September 26, 2020
Processing time: 148 Days and 3.4 Hours
Pleuroparenchymal fibroelastosis (PPFE) is a rare idiopathic interstitial pneumonia characterized by predominantly upper lobe involvement with pleural fibrosis and subjacent parenchymal fibrosis. Recently, there have been increasing reports of PPFE, and PPFE might coexist with other interstitial lung diseases in the lower lobe and upper lobe. However, cases of unilateral PPFE are scarce.
A 75-year-old Korean male presented to our hospital with chronic dry cough and exertional dyspnea. The patient’s symptoms started 6 mo previously and had been gradually worsening. At the time of presentation, he felt dyspnea when walking at his own pace. Radiologic findings suggested PPFE, but the lesion was localized in the upper lobe of the right lung. After multidisciplinary discussion, a transbronchial lung biopsy in the right upper lobe revealed collapsed alveoli with parenchymal fibroelastosis, and elastic van Gieson staining demonstrated septal elastosis with intra-alveolar collagenosis, which met the histopathologic criteria of definite PPFE. After multidisciplinary discussion in an experienced interstitial lung disease center, we confirmed the diagnosis of unilateral PPFE. Furthermore, we confirmed the progression of PPFE on radiologic findings during the follow-up period.
Clinicians should consider PPFE, even in cases with unilateral, predominantly upper lung involvement in interstitial lung disease patients through multidisciplinary discussion.
Core Tip: Pleuroparenchymal fibroelastosis (PPFE) has been classified among rare idiopathic interstitial pneumonia and is characterized by predominantly upper lobe involvement. However, there is increasing evidence for the coexistence of other interstitial lung diseases in the same lobe. Herein, we report a very rare case of PPFE with laterality, unilateral PPFE. The diagnosis of PPFE should be made after multidisciplinary discussion. In cases of unilateral upper lobe predominant fibrosis, physicians should consider the diagnosis of PPFE and identify the progression of PPFE after diagnosis.
- Citation: Lee JH, Jang HJ, Park JH, Kim HK, Lee S, Kim JY, Kim SH. Unilateral pleuroparenchymal fibroelastosis as a rare form of idiopathic interstitial pneumonia: A case report. World J Clin Cases 2020; 8(18): 4186-4192
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4186.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4186
Pleuroparenchymal fibroelastosis (PPFE) is a rare idiopathic interstitial pneumonia (IIP) characterized by predominantly upper lobe involvement with pleural fibrosis and subjacent parenchymal fibrosis[1]. After the first report in 2004 by Frankel et al[2], it was classified as the group of rare IIP in the international consensus classification of IIP in 2013. There was no consensus on the diagnostic criteria for PPFE, but the radiological and histopathological criteria suggested by Reddy et al[3] in 2012 has been generally accepted. Although PPFE is classified as a rare disease, recent reports increasingly reveal that PPFE may not be as rare as once thought, and various underlying conditions related with PPFE have been reported.
Cha et al[4] reported that among seven Korean patients with PPFE, three patients (42.9%) had a history of organ transplantation (two bone marrow and one liver). In our previous study, we also reported that among 26 patients with PPFE, 16 patients (61.5%) had relevant underlying conditions (eleven infection, three chemotherapy and two organ transplantation)[5]. In patients with PPFE, the coexistence of other interstitial lung diseases (ILDs) in the lower lobe has also been increasingly reported. The prevalence of coexistent ILD is relatively high (43.0%-91.7%), and among patients with ILDs, usual interstitial pneumonia was the most common radiologic and histopathologic finding[6-9]. But unilateral lung involvement in patients with PPFE is very rare; therefore, we herein report a case of unilateral PPFE.
A 75-year-old Korean man presented to our hospital with chronic dry cough and exertional dyspnea.
The patient’s symptoms started 6 mo previously and had been gradually worsening. At the time of presentation, he felt dyspnea upon walking at his own pace.
He was an ex-smoker with a 35 pack-year history. He worked for a rubber-related product manufacturer for 30 years. He was not aware of any previous respiratory disease.
During the physical examination, auscultation with a stethoscope revealed inspiratory crackles in the right upper lung field. He appeared to have a slender habitus and flattened thoracic cage. His body mass index (BMI) was 18.4 kg/m².
Laboratory findings showed that antinuclear antibody was positive (1:40, mixed and speckled pattern). Rheumatoid factor, anti-cyclic citrullinated peptide antibody and anti-neutrophil cytoplasmic antibody were unremarkable.
Pulmonary function test showed a moderate restrictive ventilatory defect and low level of diffusion capacity of carbon monoxide. Forced vital capacity and total lung capacity (TLC) were 53% and 66% of the predicted level, respectively. Defect and low level of diffusion capacity of carbon monoxide was 47% of the predicted level, and residual volume (RV) was 73% of the predicted level. RV/TLC ratio was 48%.
Bronchoalveolar lavage, performed in the right upper lobe by flexible bronchoscopy, showed few lymphocytes (9%). The other results obtained for culture were unremarkable.
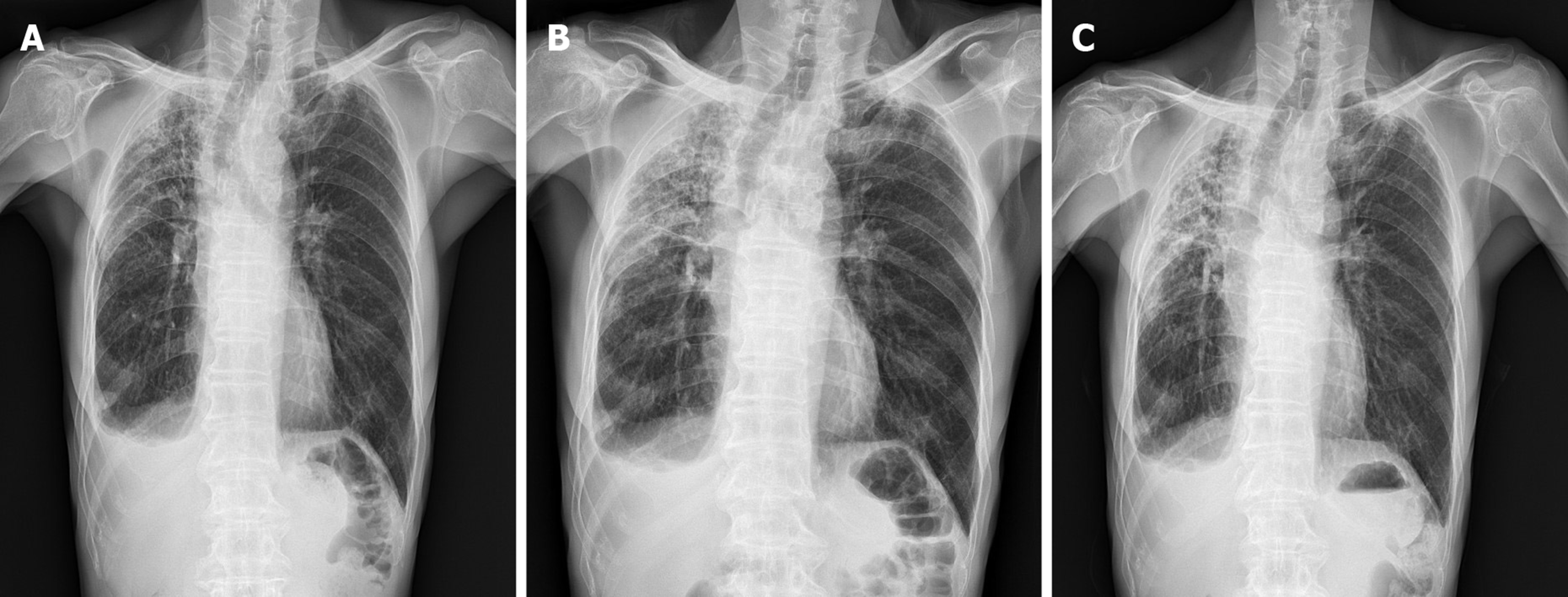
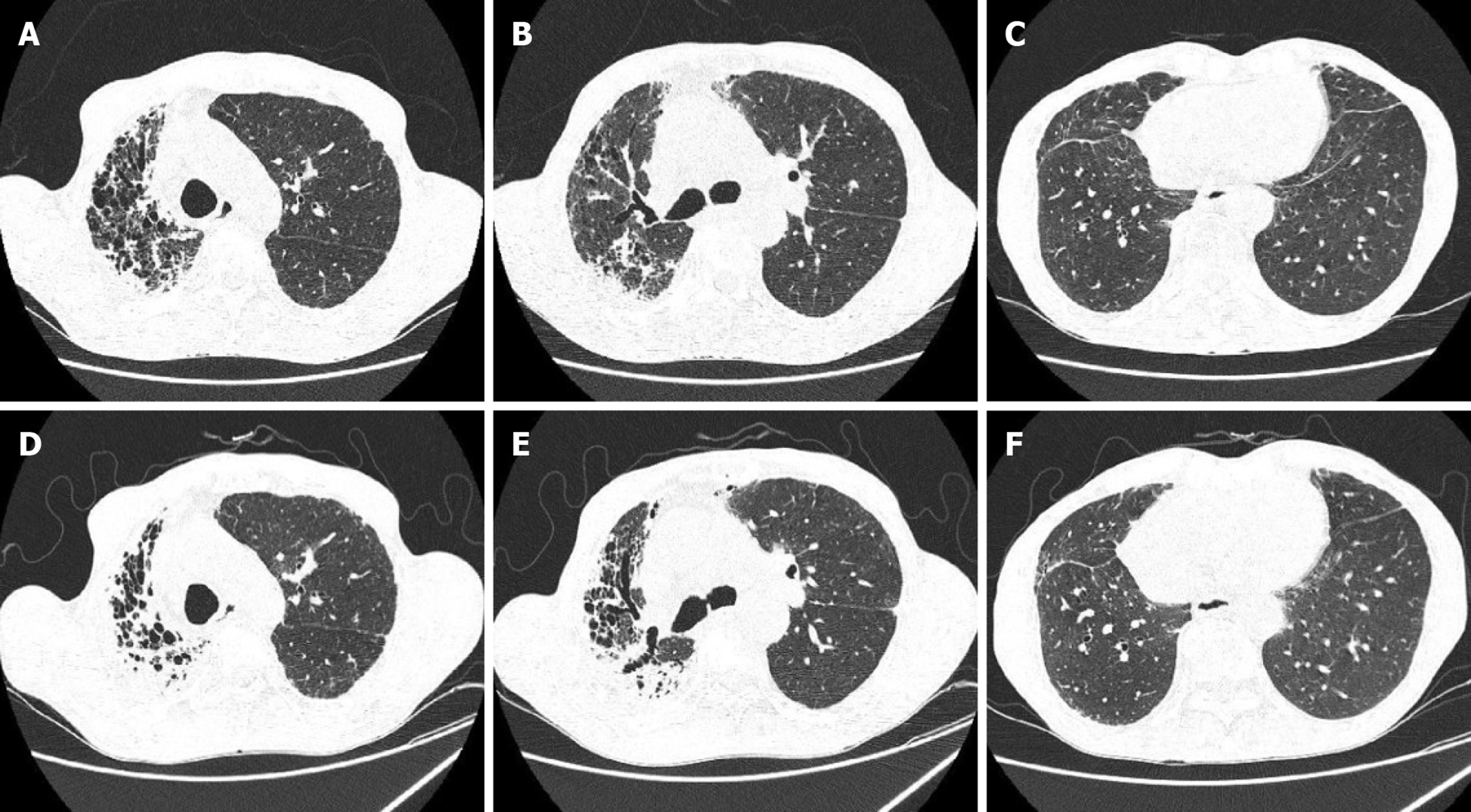
Initial chest X-ray showed a subpleural and irregularly shaped increased opacity in the right upper lung zone (Figure 1A). High-resolution computed tomography (HRCT) revealed subpleural thickening and consolidation with traction bronchiectasis in only the right upper lung field, which met the radiologic criteria of definite PPFE (Figure 2A).
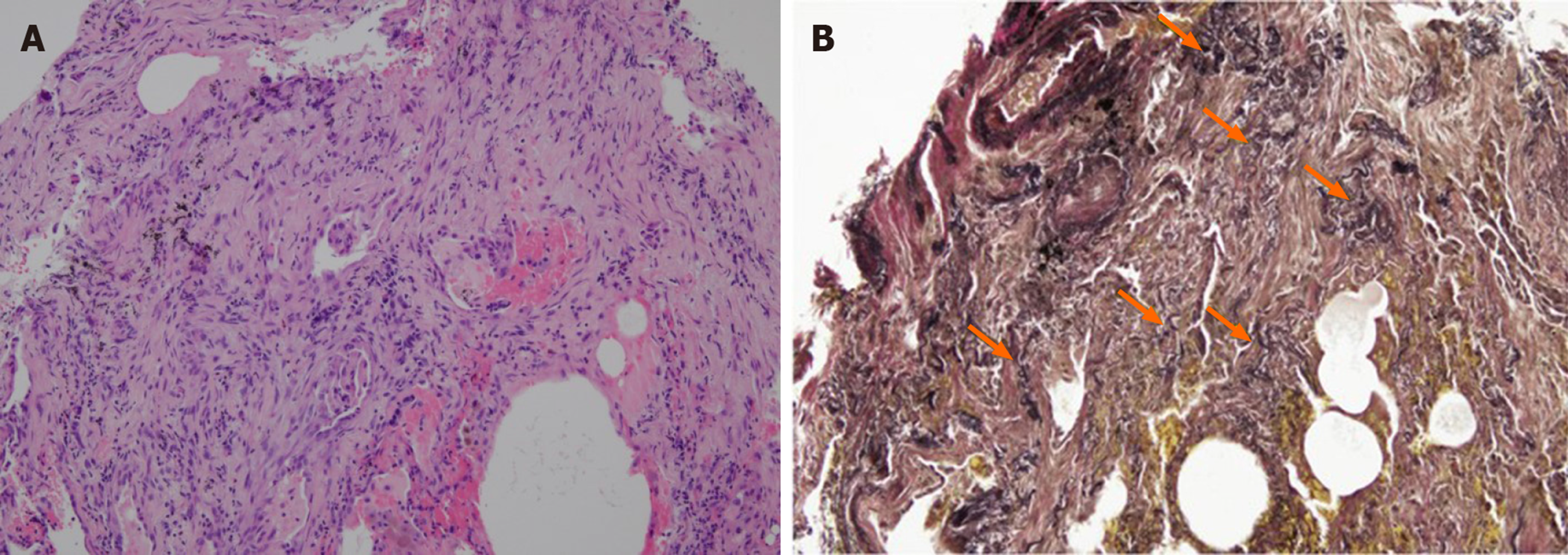
Transbronchial lung biopsy was performed in the right upper lung field to make a histopathologic diagnosis. The histopathological findings of lung tissue obtained from transbronchial lung biopsy revealed collapsed alveoli with parenchymal fibroelastosis on higher magnification view, and elastic van Gieson stain demonstrated septal elastosis with intra-alveolar collagenosis, which met the histopathologic criteria of definite PPFE (Figure 3).
The clinical information and radiologic and histopathologic data were sent to The Kanagawa Cardiovascular and Respiratory Center in Yokohama, Japan for consultation of the multidisciplinary discussion (MDD).
HRCT showed mainly ground glass opacity and fibrosis with traction bronchiectasis, suggestive of PPFE. The lesion was located in the right upper lobe only with laterality. Radiologic finding was indeterminate for usual interstitial pneumonia, suggestive PPFE.
Hematoxylin and eosin-stained images revealed dense fragmentation and dilated alveolar space surrounding alveolar with elastosis. There was no granuloma. These findings suggested PPFE with high confidence.
We diagnosed the patient with PPFE with laterality. We suggested that this abnormal presentation of PPFE may be due to occupational rubber exposure.
Through the MDDs in both our hospital and The Kanagawa Cardiovascular and Respiratory Center, the final diagnosis of the presented case was PPFE with laterality, unilateral PPFE.
Based on the diagnosis, the patient has not been treated with medications. The patient was encouraged to undergo rehabilitation with nutritional support.
After diagnosis, the patient was scheduled to attend an outpatient clinic every 3 mo to estimate his clinical symptoms and disease progression. The respiratory symptoms have not changed for 6 mo, but chest X-ray and HRCT revealed progression of the PPFE (Figures 1 and 2). On HRCT, subpleural reticulation and traction bronchiectasis with a notable volume loss in the right upper lung was significantly increased when compared to the previous exam obtained 6 mo earlier. Therefore, we identified progression of PPFE.
PPFE is a new disease entity that is classified as a rare IIP. For nearly a decade, there have been an increasing number of reports that showed the heterogeneity of PPFE, including its incidence, etiology and prognosis.
The international guideline of the American Thoracic Society/European Respiratory Society recommended MDD as the diagnostic reference standard for ILD[10]. The patient in the present case was diagnosed with unilateral PPFE after MDD involving a pulmonologist, rheumatologist, radiologist and pathologist in our hospital. However, because unilateral PPFE is so uncommon and we had never experienced it before, we also consulted with MDD in an experienced ILD center in Japan. The combination of the results from the two MDDs confirmed the diagnosis of unilateral PPFE.
In previous studies, a relatively lower BMI and a higher ratio of RV/TLC in PPFE patients compared to other IIP patients were reported as typical physiologic features of PPFE[5,6,8,11,12]. Although the reason for the lower BMI in PPFE patients is not well understood, Suzuki et al[12] suggested that the characteristics of upper lobe predominant fibrosis and a more severe restrictive ventilatory defect might exacerbate the impaired energy and protein balance, resulting in low weight and muscle wasting[12]. In terms of RV/TLC, Oda et al[7] suggested that despite upper lobe volume loss, RV/TLC was higher in PPFE patients because RV was relatively more increased than TLC owing to compensatory hyperinflation of the middle and lower lobes[7]. The patient in the present case shared similar features with the aforementioned previous studies: A lower BMI of 18.4 kg/m² and a relatively increased ratio of RV/TLC (0.48).
Having also encountered cases of upper lung field fibrosis, we included apical caps, which is defined as a wedge and triangle-shaped opacity with broad pleural contact in the apex of the lung and is a sequelae of old tuberculous infection in the differential diagnosis[13]. However, we confirmed the progression of the upper lung fibrosis over a period of 6 mo, a feature distinct from other diseases.
A number of studies report conflicting results regarding clinical outcomes in PPFE patients, and the prognosis of PPFE is not well defined. Recently, Kato et al[14] reported that among 36 patients who were clinically diagnosed with PPFE by HRCT, one-third died within 12 mo, and the median survival was 24 mo. Another previous study reported that PPFE patients had a poorer prognosis in the advanced stage than idiopathic pulmonary fibrosis patients[15]. However, in cases of rapid progression of PPFE, no treatment has been shown to be effective. Only a few case reports suggested that pirfenidone reduced the decline in lung function[16].
PPFE might be a heterogeneous disease entity. PPFE might be related to relevant underlying conditions and coexist with other ILDs with lower lung involvement. As in the present case, PPFE can exist unilaterally[17]. In the near future, PPFE must be investigated further, and clinicians need more information, including the pathogenesis, etiology, prognosis and in particular an effective treatment for PPFE.
PPFE is a rare IIP that is characterized by predominantly upper lobe involvement. However, coexistent interstitial involvement of the lower lobes has been described with increasing frequency in the literature. Herein, we reported a very rare case of unilateral PPFE. The diagnosis was confirmed by multidisciplinary discussion. In addition to fulfilling the diagnostic criteria, the patient also demonstrated the clinical features of PPFE. Physicians should consider PPFE in cases of unilateral upper lung predominant interstitial lung diseases.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Yamane M S-Editor: Zhang L L-Editor: Filipodia E-Editor: Liu JH
| 1. | Travis WD, Costabel U, Hansell DM, King TE, Lynch DA, Nicholson AG, Ryerson CJ, Ryu JH, Selman M, Wells AU, Behr J, Bouros D, Brown KK, Colby TV, Collard HR, Cordeiro CR, Cottin V, Crestani B, Drent M, Dudden RF, Egan J, Flaherty K, Hogaboam C, Inoue Y, Johkoh T, Kim DS, Kitaichi M, Loyd J, Martinez FJ, Myers J, Protzko S, Raghu G, Richeldi L, Sverzellati N, Swigris J, Valeyre D; ATS/ERS Committee on Idiopathic Interstitial Pneumonias. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2232] [Cited by in RCA: 2897] [Article Influence: 241.4] [Reference Citation Analysis (0)] |
| 2. | Frankel SK, Cool CD, Lynch DA, Brown KK. Idiopathic pleuroparenchymal fibroelastosis: description of a novel clinicopathologic entity. Chest. 2004;126:2007-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 219] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 3. | Reddy TL, Tominaga M, Hansell DM, von der Thusen J, Rassl D, Parfrey H, Guy S, Twentyman O, Rice A, Maher TM, Renzoni EA, Wells AU, Nicholson AG. Pleuroparenchymal fibroelastosis: a spectrum of histopathological and imaging phenotypes. Eur Respir J. 2012;40:377-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 262] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 4. | Cha YJ, Han J, Chung MP, Kim TJ, Shin S. Pleuroparenchymal fibroelastosis in heterogeneous clinical conditions: Clinicopathologic analysis of 7 cases. Clin Respir J. 2018;12:1495-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Lee JH, Chae EJ, Song JS, Kim M, Song JW. Pleuroparenchymal fibroelastosis in Korean patients: clinico-radiologic-pathologic features and 2-year follow-up. Korean J Intern Med. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Enomoto Y, Nakamura Y, Satake Y, Sumikawa H, Johkoh T, Colby TV, Yasui H, Hozumi H, Karayama M, Suzuki Y, Furuhashi K, Fujisawa T, Enomoto N, Inui N, Iwashita T, Kuroishi S, Yokomura K, Koshimizu N, Toyoshima M, Imokawa S, Yamada T, Shirai T, Hayakawa H, Suda T. Clinical diagnosis of idiopathic pleuroparenchymal fibroelastosis: A retrospective multicenter study. Respir Med. 2017;133:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 89] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 7. | Oda T, Ogura T, Kitamura H, Hagiwara E, Baba T, Enomoto Y, Iwasawa T, Okudela K, Takemura T, Sakai F, Hasegawa Y. Distinct characteristics of pleuroparenchymal fibroelastosis with usual interstitial pneumonia compared with idiopathic pulmonary fibrosis. Chest. 2014;146:1248-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 8. | Ishii H, Watanabe K, Kushima H, Baba T, Watanabe S, Yamada Y, Arai T, Tsushima K, Kondoh Y, Nakamura Y, Terasaki Y, Hebisawa A, Johkoh T, Sakai F, Takemura T, Kawabata Y, Ogura T; Tokyo Diffuse Lung Disease Study Group. Pleuroparenchymal fibroelastosis diagnosed by multidisciplinary discussions in Japan. Respir Med. 2018;141:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 9. | Lee SI, Chae EJ, Song JS, Lee JH, Song JW. Pleuroparenchymal fibroelastosis in patients with idiopathic pulmonary fibrosis. Respirology. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | American Thoracic Society. European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002;165:277-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2672] [Cited by in RCA: 2663] [Article Influence: 115.8] [Reference Citation Analysis (0)] |
| 11. | Kusagaya H, Nakamura Y, Kono M, Kaida Y, Kuroishi S, Enomoto N, Fujisawa T, Koshimizu N, Yokomura K, Inui N, Suda T, Colby TV, Chida K. Idiopathic pleuroparenchymal fibroelastosis: consideration of a clinicopathological entity in a series of Japanese patients. BMC Pulm Med. 2012;12:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Suzuki Y, Yoshimura K, Enomoto Y, Yasui H, Hozumi H, Karayama M, Furuhashi K, Enomoto N, Fujisawa T, Nakamura Y, Inui N, Suda T. Distinct profile and prognostic impact of body composition changes in idiopathic pulmonary fibrosis and idiopathic pleuroparenchymal fibroelastosis. Sci Rep. 2018;8:14074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 13. | Lagstein A. Pulmonary Apical Cap-What's Old Is New Again. Arch Pathol Lab Med. 2015;139:1258-1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Kinoshita Y, Watanabe K, Ishii H, Kushima H, Hamasaki M, Fujita M, Nabeshima K. Pleuroparenchymal fibroelastosis as a histological background of autoimmune diseases. Virchows Arch. 2019;474:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Shioya M, Otsuka M, Yamada G, Umeda Y, Ikeda K, Nishikiori H, Kuronuma K, Chiba H, Takahashi H. Poorer Prognosis of Idiopathic Pleuroparenchymal Fibroelastosis Compared with Idiopathic Pulmonary Fibrosis in Advanced Stage. Can Respir J. 2018;2018:6043053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Sato S, Hanibuchi M, Takahashi M, Fukuda Y, Morizumi S, Toyoda Y, Goto H, Nishioka Y. A Patient with Idiopathic Pleuroparenchymal Fibroelastosis Showing a Sustained Pulmonary Function due to Treatment with Pirfenidone. Intern Med. 2016;55:497-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Sekine A, Satoh H, Iwasawa T, Matsui K, Ikeya E, Ikeda S, Yamakawa H, Okuda R, Kitamura H, Shinohara T, Baba T, Komatsu S, Kato T, Hagiwara E, Ogura T. Unilateral Upper Lung Field Pulmonary Fibrosis Radiologically Consistent with Pleuroparenchymal Fibroelastosis after Thoracotomy: A New Disease Entity Related to Thoracotomy. Respiration. 2017;94:431-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |