Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4128
Peer-review started: April 14, 2020
First decision: July 25, 2020
Revised: August 2, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: September 26, 2020
Processing time: 160 Days and 16 Hours
The term sudden unexpected infant death (SUID) is not always properly invoked. It refers to a broad range of conditions that sometimes defy classification. There is not only a strong emotional impact on the family, but such cases are also quite complex. Underlying causes may be multiple, not always readily apparent, and have potential repercussions, especially in terms of forensics.
A 5-month-old male baby was pronounced dead following acute lung failure and cardiopulmonary arrest. The parents had immediately rushed their child to the hospital, stating the baby was found prone and not breathing. Total-body postmortem computed tomography (PMCT) was performed, revealing a hypodense material of indeterminate nature within the main airways and areas of ground-glass parenchymal change. At autopsy, the respiratory tract mucosa appeared edematous and was coated with a whitish stringy material. There was widespread airspace reduction due to parenchymal collapse. Alveolar sacs and bronchial openings contained abundant amorphous material admixed with white blood cells. Immunohistochemical studies were performed, targeting CD15, CD68, and alpha-lactalbumin. Ultimately, the focus was on alpha-lactalbumin (milk protein), which showed marked immunopositivity within alveolar spaces. Cytoplasmic staining of macrophages was also particularly prominent.
Postmortem investigations are thus essential to identify causes of death and surrounding circumstances. PMCT is a useful tool in this setting, given the frequent dearth of autopsy findings and ambiguity as to cause of death in SUID cases. These findings, later confirmed by immunohistochemical investigations, were indicative of active pneumonia due to aspirated milk. The present account illustrates the importance a broad diagnostic approach to SUID in cases of forensic concern. PMCT is a very valuable aid in cases of forensic interest, as it can provide useful information in all those situations in which the cause of death is uncertain or there are no suggestive dynamics or lesions.
Core Tip: The most frequent causes of pulmonary aspiration were caused by milk (31.8%). Predisposing factors include any condition that alters the state of consciousness or creates dysfunction of deglutition. In general, Gastric contents are related to aspiration pneumonia and present in the lungs of 30% to 40% of infants whose deaths are attributed to sudden infant death. The postmortem diagnosis of milk aspiration is a challenge for clinician and pathologist. In case of sudden unexpected infant death from milk aspiration a broad diagnostic approach is necessary for an identification of the cause of death. Postmortem computed tomography is a very valuable aid in cases of forensic interest, as it can provide useful information in all those situations in which the cause of death is uncertain or there are no suggestive dynamics or lesions.
- Citation: Maiese A, La Russa R, Arcangeli M, Volonnino G, De Matteis A, Frati P, Fineschi V. Multidisciplinary approach to suspected sudden unexpected infant death caused by milk-aspiration: A case report. World J Clin Cases 2020; 8(18): 4128-4134
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4128.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4128
Sudden unexpected infant death (SUID) by definition encompasses all categories of such events. These cases are emotionally devastating to families and often are highly complex, involving multiple and frequently elusive causes with serious repercussions, especially the forensic ramifications. Although incorrectly invoked at times, a broad spectrum of conditions that are difficult to classify qualify as SUID[1].
In guidelines published by confidential enquiry into stillbirths and deaths in infancy (CESDI)[2], the criteria for SUID are as follows: (1) Unexpected death at autopsy; (2) Death during an acute not life-threatening illness; (3) Death within 24 h after acute illness in a previously healthy infant; (4) Death from occult conditions; or (5) Death due to external factors (e.g., trauma or poisoning).
Based on the certainty of a named cause of death, SUID is categorized as I-III, where III indicates an established cause and IA denotes unexplained death, despite postmortem studies[3]. However, comprehensive postmortem investigations (i.e., death scene inspection, autopsy and pertinent biomedical diagnostics) are crucial in narrowing the field of inquiry substantially.
The scenario depicted herein illustrates how postmortem computed tomography (PMCT) and immunohistochemical (IHC) staining helped link an occurrence of SUID to aspiration pneumonia.
In particular, PMCT is a very valuable aid in cases of forensic interest, as it can provide useful information in all those situations in which the cause of death is uncertain or there are no suggestive dynamics or lesions.
A 5-month-old male baby was reportedly found prone and not breathing by the parents, who immediately rushed the child to the hospital.
On arrival, the infant was pronounced dead as a result of acute lung failure and cardiopulmonary arrest.
No previous disease to report in anamnesis.
Cardiopulmonary resuscitation had not been attempted.
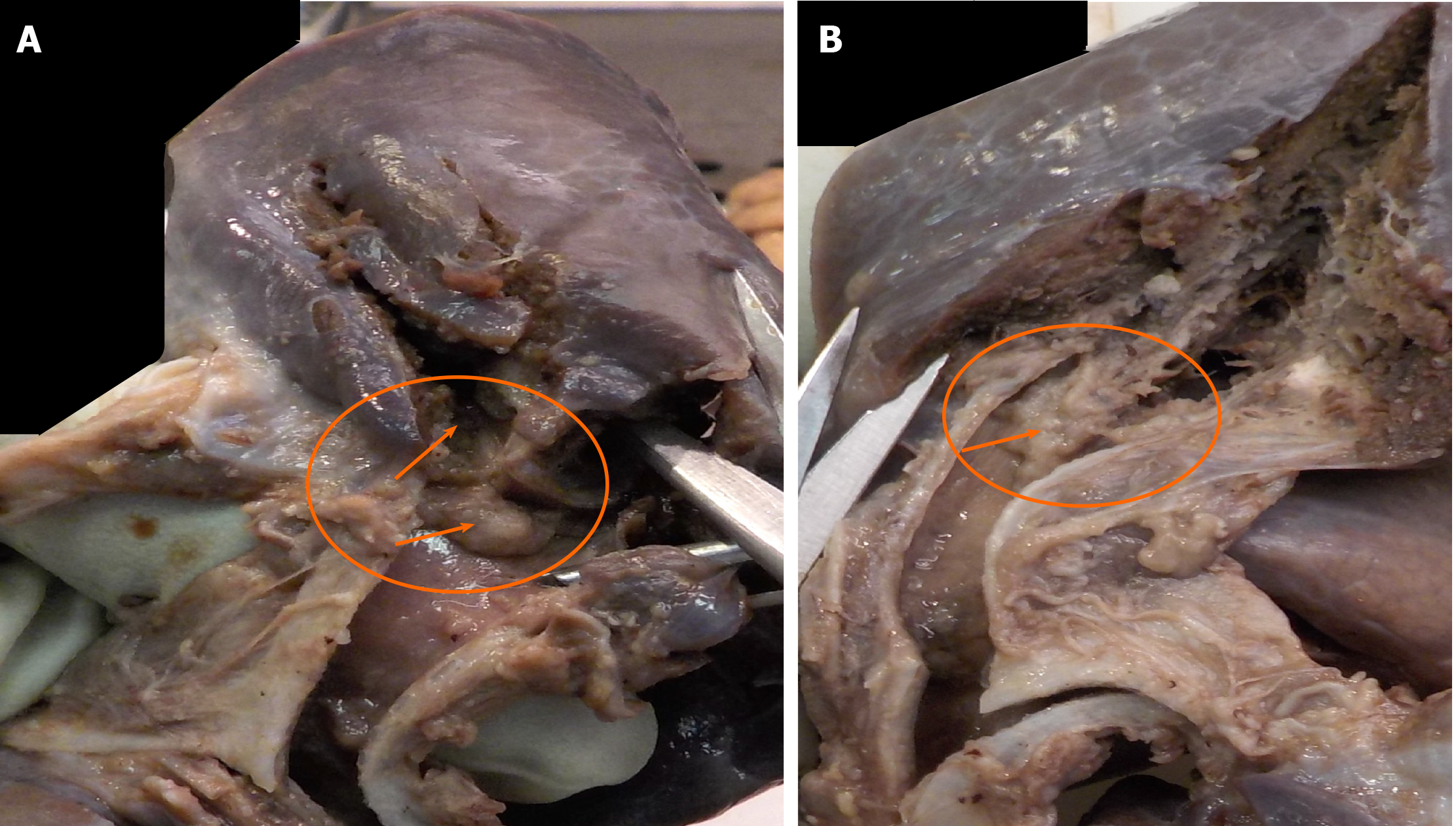
Post-mortem examination: Four days after death, the autopsy took place. The baby measured 60 cm in length and weighed 8 kg. No gross external abnormalities were detected. Internally, all major organs were normally placed and well developed. The Letulle technique was used, removing bodily contents en masse. Gross examination of the respiratory tract proceeded along posterior median axis, exposing edematous mucosal linings coated with whitish stringy material (Figure 1). The lungs were purplish in colour. After en bloc fixation, they appeared dense and congested.
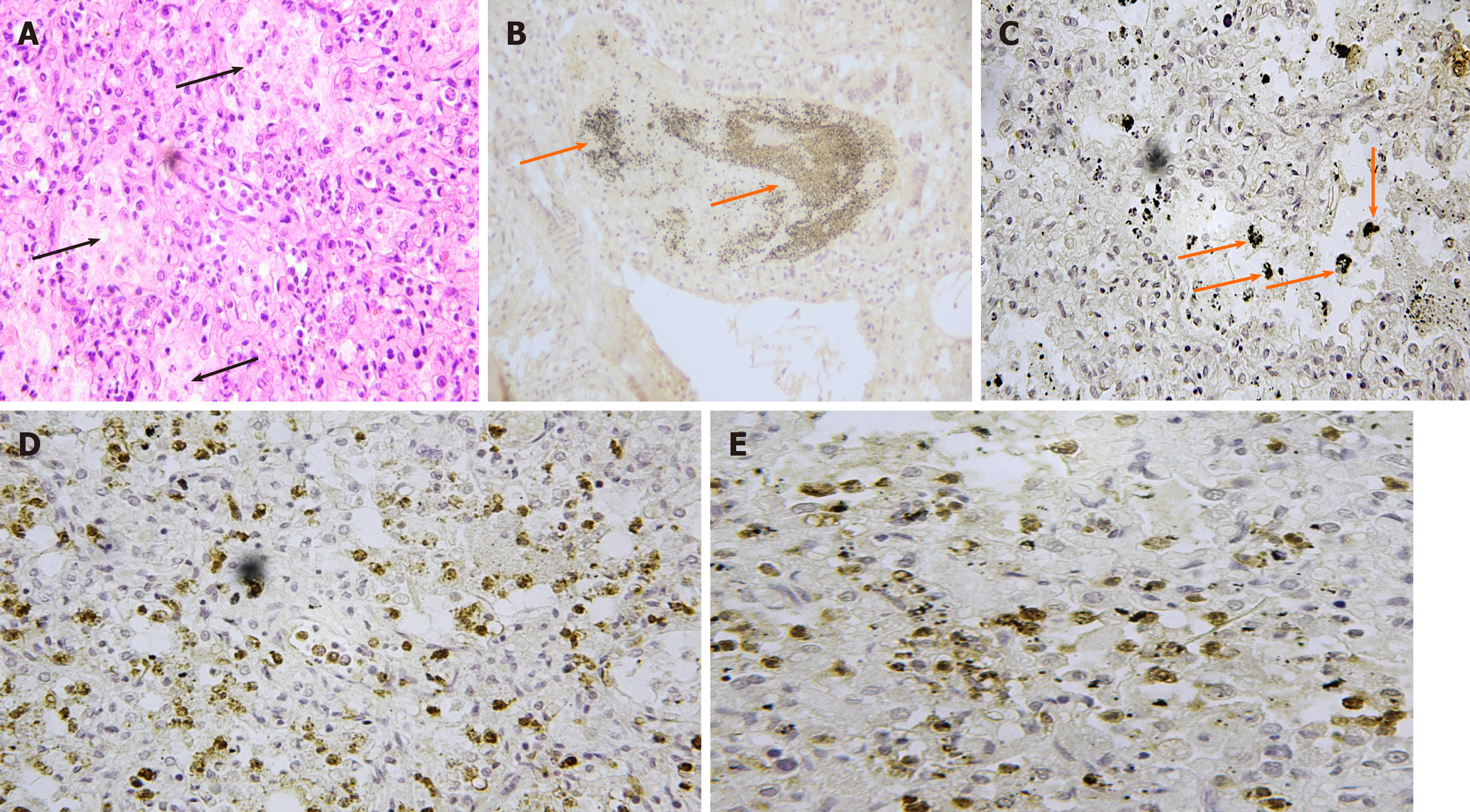
Histological examination: Thoracic and abdominal organs were sampled for routine processing and haematoxylin-eosin (HE) staining. Sections of lung tissue showed marked congestion of alveolar septal capillaries, which were also engorged with white blood cells, and widespread loss of airspace was conspicuous due to parenchymal collapse. In macrophages, there was copious cytoplasmic retention of amorphous material. The same substance, admixed with white blood cells, resided in alveolar spaces and bronchial openings. All other organs were histologically intact. Ultimately, sections of lung were subjected to IHC staining, targeting CD15, CD68, and alpha-lactalbumin. Intense CD15 positivity of alveolar content and septal capillaries was observed, whereas strong CD68 positivity was visible throughout lung parenchyma. Marked alpha-lactalbumin positivity of the intra-alveolar substance was also evident, and cytoplasmic staining of macrophages was especially prominent (Figure 2).
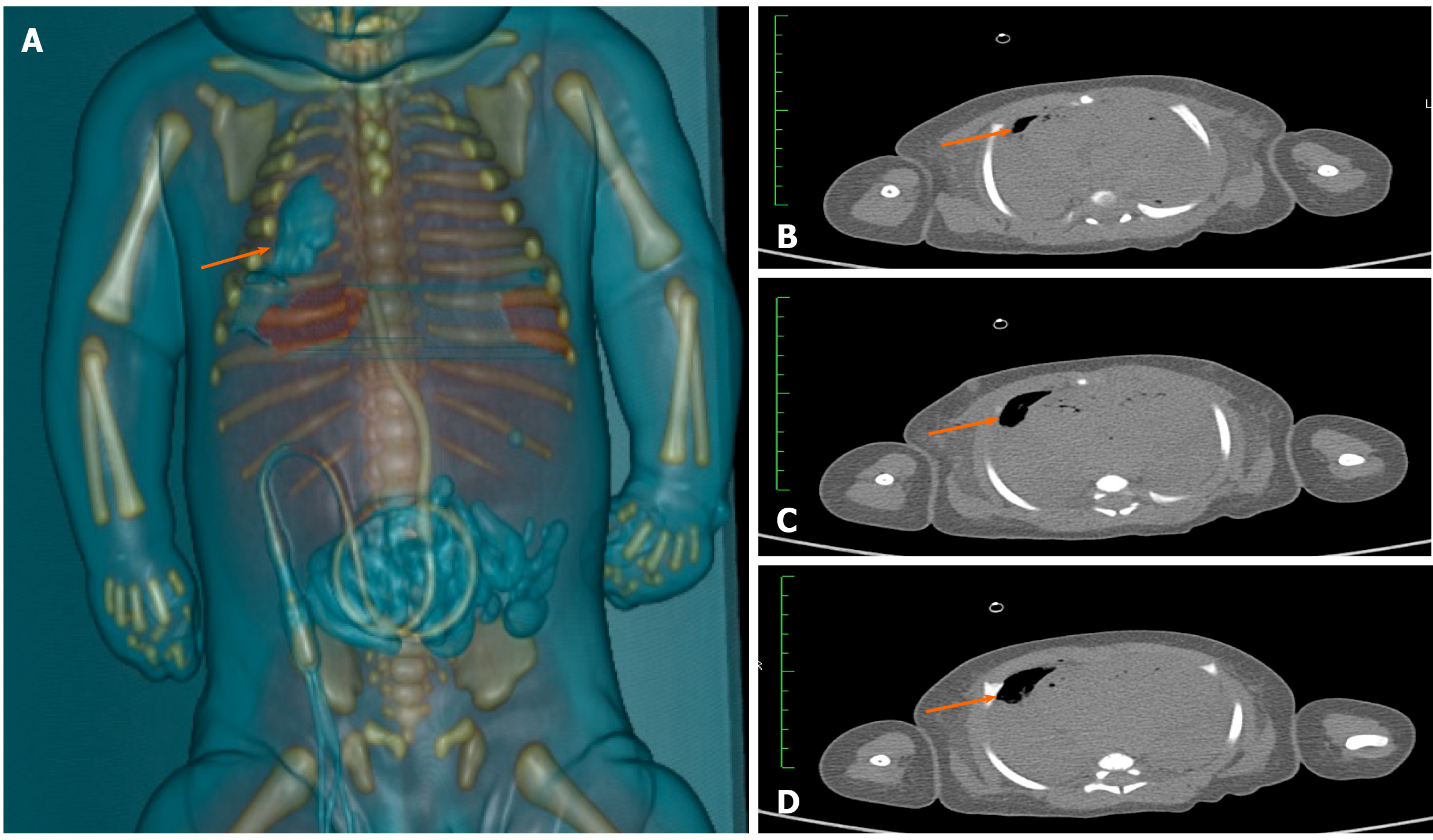
Total-body PMCT was subsequently performed. In the lungs, a hypodense material of indeterminate nature occupied the main airways bilaterally, from oropharynx to subsegmental bronchi; and ground-glass parenchymal changes were noted in areas (Figure 3).
Aspiration pneumonia due to milk aspiration.
Unfortunately, physicians were unable to intervene even with resuscitation maneuvers as the death of patient was declared at the time of hospitalization.
As previously discussed, the infant was declared dead upon admission to the hospital following a aspiration pneumonia from milk ingestion; final diagnosis was based on instrumental and immunohistochemical studies.
Aspiration pneumonia is incited by foreign materials, often of oral or gastric origin (saliva, food), that enter the bronchial tree[4]. In general, Gastric contents is related to aspiration pneumonia and present in the lungs of 30% to 40% of infants whose deaths are attributed to sudden infant death[5,6].
Predisposing factors include any condition that alters the state of consciousness or creates dysfunction of deglutition. Typically, sudden respiratory difficulties (acute dyspnea) and cough develop in conjunction with solid or liquid food intake or regurgitation of gastric contents. The severity of symptoms depends on the nature and quantity of aspirated material. In some cases, cough is accompanied by pinkish and foamy or purulent sputum production. Tachycardia, high respiratory rate, fever, fatigue, myalgia, weight loss, and general malaise, may also ensue. Other consequences are diffuse end-expiratory wheezing, cyanosis, hypoxemia, pleuritic chest pain, bronchoconstriction, and acute pulmonary edema[7,8].
In a study of Karim et al[9], on 107 children with pulmonary aspiration, the most frequent causes of pulmonary aspiration were caused by milk (31.8%) and oral secretions (19.6%). Neurological disorders were present in 29% of children, 5.6% had asphyxiation at birth and 10% were premature.
To establish the diagnosis, details of a patient’s clinical history (and risk factors) are essential and biomedical diagnostics are pivotal. Chest radiographs readily disclose parenchymal infiltrates, reflecting bodily positions at times of aspiration. In cases of suspected SUID, no distinctive histopathologic changes are encountered, only agonal phenomena, such as pulmonary edema. A comprehensive postmortem investigation is therefore mandatory, which in this instance called for assessing the death scene and its circumstances, tomographic imaging (PMCT) and IHC techniques[10,11].
Because SUID events are often unwitnessed and lack autopsy evidence to explain cause of death, PMCT studies may be immensely productive. Computed tomography is likewise considered useful in the screening of unnatural death[12,13]. Recently, the association between post-mortem magnetic resonance, post-mortem examination and related histological study of the foetus or newborn could help reduce the percentage of cases in which the cause of death remains unexplained. Lastly, it may allow a selective sampling of the organ in order to target histological investigations[14].
Milk is a common gastric component of newborns, but its triggering of aspiration pneumonia is much debated. Many authors view the presence of milk in the lungs as a postmortem artifact, secondary to cardiopulmonary resuscitation[15]. At autopsy, gastric content limited to distal lung segments (upper airways still clear) would indeed support their contention[16]. Immunohistochemistry for milk components helps to demonstrate aspirated milk in lung sections.
The postmortem diagnosis of milk aspiration is a challenge for the forensic pathologist, as Moran et al[17] outlined in 1953. To date, few post-mortem studies that evaluate the diagnostic usefulness of specific immunohistochemical assays in the diagnosis of milk aspiration as a cause of death have been published.
In 1986 Boulloche et al[18], have studied of serum IgE assay in milk aspiration and the sudden infant death syndrome. In this study only the infants with a history of milk aspiration had significantly raised global and specific IgE. Iwadate et al[19-21], in three studies they examined 105 cases of aspiration pneumonia by immunostaining with anti-human α-lactalbumin antibody; milk aspiration was detected with immunohistochemical study in 40 cases. In other case reports, the need to carry out immunohistochemical assessments in case of histological examinations show a lot of amorphous material, suspect of aspirated milk[22]. Experimental studies using a murine model have shown that the detection of aspirated milk in other organs except the lung would be clear evidence of intravital milk aspiration[23,24].
This result indicates that some degree of milk aspiration is not rare in infant death cases and the need for immunohistochemical examinations for the diagnosis of death due to milk aspiration.
In our case infant succumbed to acute pulmonary insufficiency, prompting total-body PMCT. In the lungs, the main airways contained hypodense material and ground-glass parenchymal changes were present. No alterations were identified elsewhere, implicating the lungs solely as cause of death. The autopsy itself corroborated what was detected by PMCT. Airways of the infant displayed mucosal edema and contained whitish stringy material. IHC staining of CD15, CD68, and alpha-lactalbumin in samples of lung tissue also confirmed the suspicion of aspiration pneumonia. Both CD15 (neutrophil) and CD68 (macrophage) markers were strongly positive within alveoli and throughout lung parenchyma. These features were decisive, underscoring an active inflammatory process prior to death. We also targeted alpha-lactalbumin (milk protein), which proved markedly positive within alveolar and macrophage reservoirs, linking the pneumonia to aspiration of milk. Owing to combined use of PMCT and immunohistochemistry, a cause of death was conclusively determined in this case of SUID[25].
Autopsies requested for SUID tend to be unproductive. In those cases where death can be attributable to numerous causes, PMCT may direct the clinician and the pathologist towards a specific etiology. In deaths from aspiration asphyxia, IHC staining is an essential step, helping to clarify the nature of aspirated material and confirm its presence within cellular infiltrates.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jeong KY, Pandey A S-Editor: Yan JP L-Editor: A P-Editor: Li JH
| 1. | Krous HF. Sudden unexpected death in infancy and the dilemma of defining the sudden infant death syndrome. Curr Pediatr Rev. 2010;6:5–12. [DOI] [Full Text] |
| 2. | Fleming PJ, Blair PSP, Bacon C, Berry PJ, editors. Sudden unexpected deaths in infancy. The CESDI SUDI studies 1993–1996. London: The Stationary Office; 2000. |
| 3. | Blair PS, Byard RW, Fleming PJ. Sudden unexpected death in infancy (SUDI): suggested classification and applications to facilitate research activity. Forensic Sci Med Pathol. 2012;8:312-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Byard RW, Beal SM. Gastric aspiration and sleeping position in infancy and early childhood. J Paediatr Child Health. 2000;36:403-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Thach BT. Sudden infant death syndrome: can gastroesophageal reflux cause sudden infant death? Am J Med. 2000;108 Suppl 4a:S144-S148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Lanspa MJ, Jones BE, Brown SM, Dean NC. Mortality, morbidity, and disease severity of patients with aspiration pneumonia. J Hosp Med. 2013;8:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Son YG, Shin J, Ryu HG. Pneumonitis and pneumonia after aspiration. J Dent Anesth Pain Med. 2017;17:1-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 8. | Raghavendran K, Nemzek J, Napolitano LM, Knight PR. Aspiration-induced lung injury. Crit Care Med. 2011;39:818-826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 208] [Cited by in RCA: 189] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 9. | Karim RM, Momin IA, Lalani II, Merchant SS, Sewani AA, Hassan BS, Mahmood N. Aspiration pneumonia in pediatric age group: etiology, predisposing factors and clinical outcome. J Pak Med Assoc. 1999;49:105-108. [PubMed] |
| 10. | Bartusch O, Finkl M, Jaschinski U. [Aspiration syndrome: epidemiology, pathophysiology, and therapy]. Anaesthesist. 2008;57:519-30; quiz 531-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Bennett T, Martin LJ, Heathfield LJ. A retrospective study of death scene investigation practices for sudden unexpected death of infants (SUDI) in Cape Town, South Africa. Forensic Sci Med Pathol. 2020;16:49-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Hunt CE, Darnall RA, McEntire BL, Hyma BA. Assigning cause for sudden unexpected infant death. Forensic Sci Med Pathol. 2015;11:283-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Byard RW, Duncan JR, Byard RW. The Autopsy and Pathology of Sudden Infant Death Syndrome. In: Duncan JR, Byard RW, editors. SIDS Sudden Infant and Early Childhood Death: The Past, the Present and the Future. Duncan JR, Byard RW. Adelaide (AU): University of Adelaide Press: 2018 May. Chapter 24. |
| 14. | Vullo A, Panebianco V, Cannavale G, Aromatario M, Cipolloni L, Frati P, Santurro A, Vullo F, Catalano C, Fineschi V. Post-mortem magnetic resonance foetal imaging: a study of morphological correlation with conventional autopsy and histopathological findings. Radiol Med. 2016;121:847-856 [10.1007/s11547-016-0672-z]. |
| 15. | van Rijn RR, Beek EJ, van de Putte EM, Teeuw AH, Nikkels PGJ, Duijst WLJM, Nievelstein RA; Dutch NODO Group. The value of postmortem computed tomography in paediatric natural cause of death: a Dutch observational study. Pediatr Radiol. 2017;47:1514-1522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Krous HF, Masoumi H, Haas EA, Chadwick AE, Stanley C, Thach BT. Aspiration of gastric contents in sudden infant death syndrome without cardiopulmonary resuscitation. J Pediatr. 2007;150:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | MORAN TJ. Milk-aspiration pneumonia in human and animal subjects. AMA Arch Pathol. 1953;55:286-301. [PubMed] |
| 18. | Boulloche J, Mallet E, Basuyau JP, Tayot P, Samson-Dollfus D. The value of serum IgE assay in milk aspiration and the sudden infant death syndrome. Acta Paediatr Scand. 1986;75:530-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Iwadate K, Doy M, Ito Y. Screening of milk aspiration in 105 infant death cases by immunostaining with anti-human alpha-lactalbumin antibody. Forensic Sci Int. 2001;122:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Iwadate K, Doy M, Nishimaki Y, Liang F, Takatori T, Hasekura H. Immunohistochemical examination of the lungs in infant death cases using antibodies against milk components. Forensic Sci Int. 2000;110:19-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Iwadate K, Sakamoto N, Park SH, Doy M, Iwase H, Nagao M, Takatori T. Immunohistochemical detection of human milk components aspirated in lungs of an infant. Forensic Sci Int. 1997;90:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Kibayashi K, Iwadate K, Shojo H. Milk aspiration in an infant during supine bottle feeding: a case report. Med Sci Law. 2004;44:272-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Nagai T, Aoyagi M, Ochiai E, Sakai K, Maruyama-Maebashi K, Fukui K, Iwadate K. Longitudinal evaluation of immunohistochemical findings of milk aspiration: an experimental study using a murine model. Forensic Sci Int. 2011;209:183-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Iwadate K, Aoyagi M, Sakai K, Ochiai E, Abe S, Maebashi K, Nakamura M, Fukui K. Feasibility of immunohistochemical examination of lungs to distinguish intravital milk-aspiration from postmortem “aspiration” a experimental study using a murine model. Res. Pract. Forensic Med. 2008;51:233-237. |
| 25. | Wu HH, Chen YX, Fang SY. Pleural effusion in an immunocompetent host with cryptococcal pneumonia: A case report. World J Clin Cases. 2020;8:1295-1300. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |