Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4109
Peer-review started: May 7, 2020
First decision: June 8, 2020
Revised: June 10, 2020
Accepted: August 26, 2020
Article in press: August 26, 2020
Published online: September 26, 2020
Processing time: 137 Days and 5.6 Hours
Small bowel obstructions (SBOs) are common following a large intra-abdominal operation; however, SBOs caused by bezoars are unreported in patients following liver-kidney transplantation procedures, particularly in adults.
A 65-year-old Caucasian female presented with nausea and nonbilious emesis during her postoperative course following a simultaneous liver-kidney transplantation. She developed worsening nausea and vomiting with significant abdominal distension and obstipation. Computed tomography imaging showed a marked abnormal dilation of multiple small bowel loops with a distinct transition point that was suggestive of a small bowel obstruction. An exploratory laparotomy revealed a foreign body in the intestinal track approximately 30 cm from the ileocecal valve. The foreign body was extracted and identified as a bezoar with hair follicles and old digestive contents. Following the operation, the patient demonstrated rapid clinical improvement with resolution of nausea, emesis, and progress in bowel motility.
SBOs caused by bezoars can occur immediately following a liver-kidney transplantation and should not be discounted as a diagnosis.
Core Tip: Herein we present the management of an adult patient with a small bowel obstruction caused by a bezoar a week following a simultaneous liver-kidney transplantation. Radiographic imaging demonstrated an obstruction that required immediate surgical intervention. An exploratory laparotomy revealed a bezoar. Bezoars can occur immediately following a liver-kidney transplantation and should not be discounted as a diagnosis for a small bowel obstruction.
- Citation: Pan G, Kim RD, Campsen J, Rofaiel G. Small bowel obstruction caused by a bezoar following an adult simultaneous liver-kidney transplantation: A case report. World J Clin Cases 2020; 8(18): 4109-4113
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4109.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4109
Liver transplantation remains the standard of care for patients with end-stage liver disease (ESLD). As with all intra-abdominal procedures, there remains the risk of forming intra-abdominal adhesions in about 95% of patients[1]. Small bowel obstructions (SBOs) are a common morbidity associated with abdominal surgery[2]. Treatment modalities include both operative and nonoperative management. Conservative, nonoperative management typically consists of bowel rest, intravenous fluid rehydration, and nasogastric intubation[3]. While most SBOs resolve without surgical intervention, an estimated 24% of SBOs require emergency surgery[4]. Computed tomography (CT) scans remain a valuable tool to evaluate the etiology of the SBO as well as provide information to determine management strategies[5-7].
Bezoars are foreign bodies composed of undigested material that often persist in the gastrointestinal tract without causing obstructions[8]. In fact, bezoars are a relatively uncommon form of SBO, affecting less than 4% of all cases[9]. We are here presenting a case of a bezoar causing an acute SBO requiring operative intervention. This occurred shortly after a simultaneous liver-kidney transplant.
A 65-year-old Caucasian female developed persistent nausea and vomiting during her postoperative course approximately a week following a simultaneous liver-kidney transplantation.
Post-operative days 1 and 2 were notable for nausea and nonbilious emesis. Ondansetron was administered with gradual improvement and symptom resolution. About a week later, the patient developed worsening of nausea and vomiting with significant abdominal distension and obstipation.
The patient has a history of liver cirrhosis secondary to primary biliary cholangitis and subsequent end-stage renal disease. She also had a history of inflammatory bowel disease. She received simultaneous liver-kidney transplantation after being placed on the waiting list. Her model for end-stage liver disease score at the time of transplant was 25. The donor was a 62-year-old female who had an intraventricular hemorrhage and was declared brain dead. The liver enzymes were within normal limits, and the terminal creatinine was 0.66 mg/dL. The Kidney Donor Profile Index score was 87%.
The transplantation operation was performed using a standard Chevron incision for the liver transplant. The biliary reconstruction was performed using standard duct-to-duct anastomosis. The incision was extended in a paramedian fashion on the right side to perform the kidney transplant. The recipient’s intraoperative course related to transplantation was uncomplicated.
Laboratory examination results were within normal limits following a simultaneous liver-kidney transplantation.
Computed tomography (CT) imaging showed a marked abnormal dilation of multiple small bowel loops with a distinct transition point. This was suggestive of a small bowel obstruction (Figure 1).
Upon review of radiographic imaging, a small bowel obstruction was suspected that required immediate operative intervention.
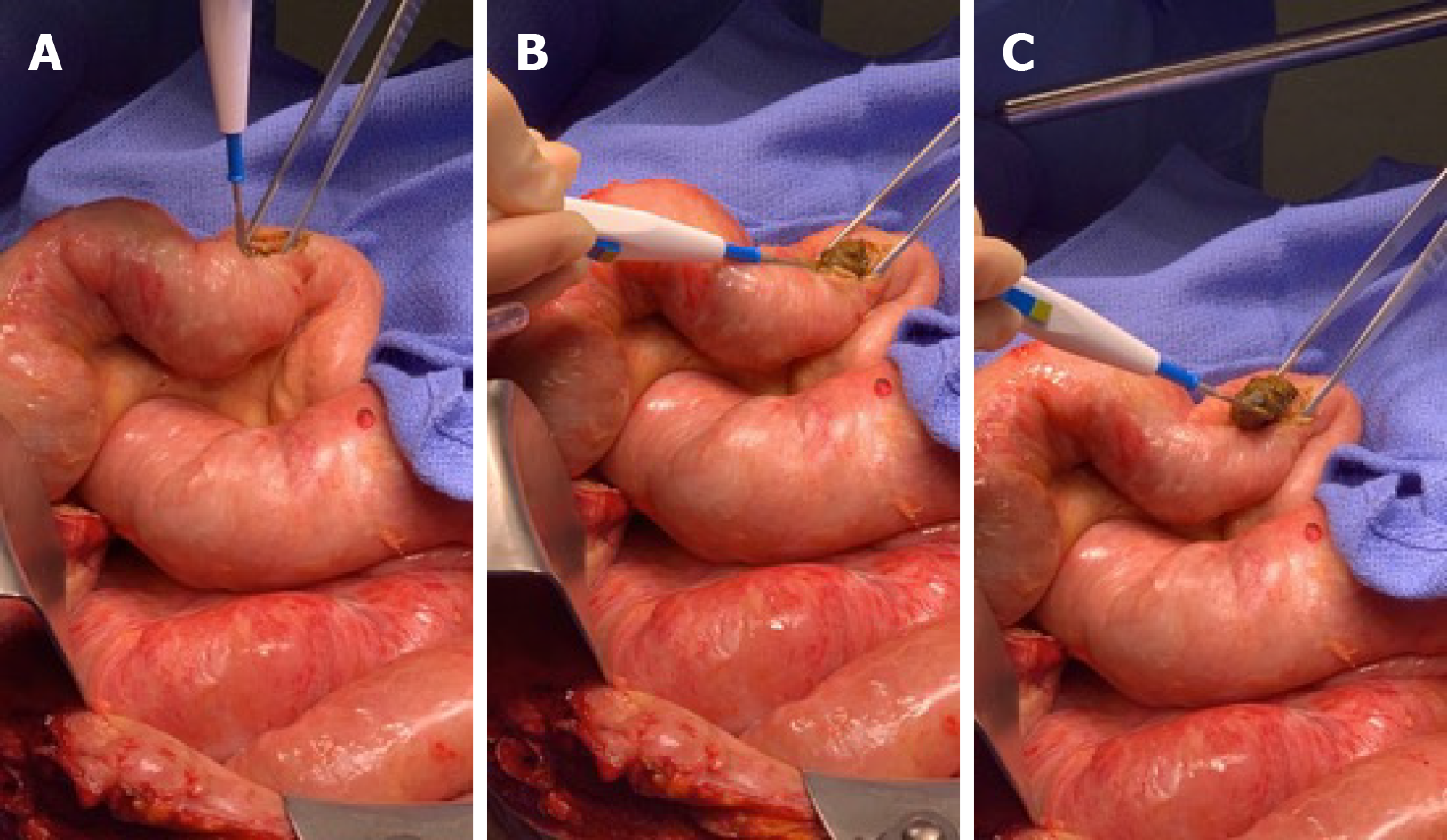
An exploratory laparotomy was performed. After examining the whole small and large intestine, a foreign body was found approximately 30 cm from the ileocecal valve. The bowel was subsequently opened, and the foreign body was identified as a bezoar with hair follicles and old digestive contents (Figure 2). The bezoar was extracted, and the bowel was closed using a side-to-side anastomosis. Pathology was notable for mild serosal reactive tissue without chronic features to suggest inflammatory bowel disease.
There were no known intraoperative complications. Following the removal of the bezoar, the patient demonstrated rapid clinical improvement with resolution of nausea, emesis, and progress in bowel motility. Patient remains asymptomatic with no evidence of bowel obstruction or food intolerance 10 mo after exploration.
Postoperative bowel obstruction is not an uncommon issue. The most common cause of bowel obstruction is adhesive disease[10]. Foreign body related obstruction is more common in pediatric populations[11]. It is however not described as a common cause in adults, especially in the immediate postoperative period[12]. In our case, the patient was practically not eating before the symptoms of bowel obstruction became apparent. She actually started having evidence of bowel function and then regressed. Workup in these scenarios should proceed following standard of care for a mechanical obstruction. CT scans are typically very sensitive in indicating the area of obstruction and suggesting a possible partial obstruction, which usually resolves spontaneously. In this case, there was clearly a complete mechanical obstruction. Adhesive disease was the presumed diagnosis, but the foreign body bezoar was the unusual incidental finding.
Bezoars are commonly separated into 4 categories based on their composition: phytobezoars (fruit or vegetable content), trichobezoars (hair), lactobezoars (milk), and pharmacobezoars (medication)[13]. Due to the narrow passage between the pylorus and small intestine, bezoars can cause an acute obstruction typically proximal to the ileocecal valve[14]. Trichobezoars are commonly described in children with the most extreme cases often attributed to Rapunzel syndrome[15]. Adult cases are uncommon and sparsely reported[16]. Gross pathological analysis of the bezoar specimen showed hair follicles present; however, a definite diagnosis of a trichobezoar was not reached.
Limited reports exist about SBOs caused by bezoars in post-transplant settings. Schwarzenberg and colleagues discuss the management gastric bezoars after pediatric liver transplantation in a case series of 3 patients[17]. Herein we present the management of an adult patient with SBO caused by a bezoar a week following a simultaneous liver-kidney transplantation.
Liver transplantation is a necessary major intra-abdominal operation for ESLD patients. Complications occur that often require surgical intervention. In a post-transplant setting, reoperation is in a hostile setting that is fraught with risks and altered anatomy. The management of an adult with an SBO caused by a bezoar post-transplant is unreported, particularly immediately following the transplantation. This case discusses a post-operative anomaly that cannot be discounted for adult transplant recipients following a large intra-abdominal operation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Akarsu M S-Editor: Gong ZM L-Editor: A P-Editor: Wu YXJ
| 1. | Menzies D, Ellis H. Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990;72:60-63. [PubMed] |
| 2. | Duron JJ, Silva NJ, du Montcel ST, Berger A, Muscari F, Hennet H, Veyrieres M, Hay JM. Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg. 2006;244:750-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 143] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 3. | Kuehn F, Weinrich M, Ehmann S, Kloker K, Pergolini I, Klar E. Defining the Need for Surgery in Small-Bowel Obstruction. J Gastrointest Surg. 2017;21:1136-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Foster NM, McGory ML, Zingmond DS, Ko CY. Small bowel obstruction: a population-based appraisal. J Am Coll Surg. 2006;203:170-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 169] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 5. | Jang TB, Schindler D, Kaji AH. Predictive value of signs and symptoms for small bowel obstruction in patients with prior surgery. Emerg Med J. 2012;29:769-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Azagury D, Liu RC, Morgan A, Spain DA. Small bowel obstruction: A practical step-by-step evidence-based approach to evaluation, decision making, and management. J Trauma Acute Care Surg. 2015;79:661-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Maung AA, Johnson DC, Piper GL, Barbosa RR, Rowell SE, Bokhari F, Collins JN, Gordon JR, Ra JH, Kerwin AJ; Eastern Association for the Surgery of Trauma. Evaluation and management of small-bowel obstruction: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S362-S369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 177] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 8. | Iwamuro M, Okada H, Matsueda K, Inaba T, Kusumoto C, Imagawa A, Yamamoto K. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc. 2015;7:336-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 214] [Cited by in RCA: 199] [Article Influence: 19.9] [Reference Citation Analysis (5)] |
| 9. | Dikicier E, Altintoprak F, Ozkan OV, Yagmurkaya O, Uzunoglu MY. Intestinal obstruction due to phytobezoars: An update. World J Clin Cases. 2015;3:721-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 10. | ten Broek RP, Issa Y, van Santbrink EJ, Bouvy ND, Kruitwagen RF, Jeekel J, Bakkum EA, Rovers MM, van Goor H. Burden of adhesions in abdominal and pelvic surgery: systematic review and met-analysis. BMJ. 2013;347:f5588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 309] [Cited by in RCA: 388] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 11. | Wright CC, Closson FT. Updates in pediatric gastrointestinal foreign bodies. Pediatr Clin North Am. 2013;60:1221-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Bower KL, Lollar DI, Williams SL, Adkins FC, Luyimbazi DT, Bower CE. Small Bowel Obstruction. Surg Clin North Am. 2018;98:945-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Khan S, Jiang K, Zhu LP, Khan IA, Ullah K, Khan S, Chen X, Wang BM. Upper Gastrointestinal Manifestation of Bezoars and the Etiological Factors: A Literature Review. Gastroenterol Res Pract. 2019;2019:5698532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Goddard SA, Lundberg PW, Jones SD. Small-Bowel Obstruction in a 45-Year-Old Woman. JAMA Surg. 2017;152:599-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Fallon SC, Slater BJ, Larimer EL, Brandt ML, Lopez ME. The surgical management of Rapunzel syndrome: a case series and literature review. J Pediatr Surg. 2013;48:830-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Kumar N, Huda F, Gupta R, Payal YS, Kumar U, Mallik D. Rapunzel syndrome in adult with mysterious presentation: a rare case report with literature review. Trop Doct. 2019;49:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Schwarzenberg SJ, Freese DK, Payne WD, Ascher NL, Sharp HL. Gastric bezoar after hepatic transplantation. J Pediatr Gastroenterol Nutr. 1989;9:119-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |