Published online Sep 6, 2020. doi: 10.12998/wjcc.v8.i17.3890
Peer-review started: March 25, 2020
First decision: July 4, 2020
Revised: July 18, 2020
Accepted: July 30, 2020
Article in press: July 30, 2020
Published online: September 6, 2020
Processing time: 163 Days and 1.5 Hours
Multilevel artificial cervical disc replacement and anterior hybrid surgery have been introduced as reliable treatments for multilevel cervical degenerative disc disease. Surgical techniques are important for resolving patients’ symptoms and maintaining the normal functioning of cervical implants. However, the use of inappropriate surgical strategies could lead to complications such as implant migration and neurological deficit. In this paper, we summarize our surgical strategies used in multilevel cervical disc replacement and hybrid surgery into five major notes.
We share the key notes and our surgical procedures in the form of four typical case presentations. All patients were diagnosed with cervical degenerative disc disease with myelopathy or radiculopathy and needed multilevel cervical spine surgery. The first case demonstrated that index levels indicating the presence of highly serious spinal cord compression required a prioritized decompression. The second case demonstrated that the disc replacement should be performed before fusion in cervical hybrid surgery. The third and forth cases demonstrated that a top-down implantation sequence was needed in continuous two-level cervical disc replacement. The symptoms of all patients were significantly relieved after surgery.
We hope that our surgical strategies can help improve the performance and outcomes of multilevel cervical spine surgery.
Core tip: We share our surgical strategies and surgical procedures in treating multilevel cervical degenerative disc disease in the form of four typical case presentations. We hope that our surgical strategies can help avoid the postoperative complications and improve the performance and outcomes of multilevel cervical spine surgery.
- Citation: Wang XF, Meng Y, Liu H, Hong Y, Wang BY. Surgical strategy used in multilevel cervical disc replacement and cervical hybrid surgery: Four case reports. World J Clin Cases 2020; 8(17): 3890-3902
- URL: https://www.wjgnet.com/2307-8960/full/v8/i17/3890.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i17.3890
Multilevel cervical degenerative disc disease, a growing public health concern, is defined as two or more segments of the cervical spine that begin to degenerate, causing significant cervical disability and a loss of productivity. Anterior cervical discectomy and fusion (ACDF) is a classic treatment for multilevel cervical spondylosis, although it has some limitations involving the pseudarthrosis and degeneration of adjacent segments[1,2]. In recent decades, with the development of nonfusion surgery, the efficacy and safety of using artificial cervical disc replacement (CDR) for single-level or multilevel cervical degenerative disc diseases has been demonstrated by several prospective studies from the United States Food and Drug Administration and by some meta-analyses[3-8]. In contrast to ACDF, CDR has the advantages of preserving the segmental range of motion (ROM) at a surgical level, preventing the acceleration of degeneration in adjacent segments, and avoiding complications such as nonunion or pseudoarthrodesis[9,10]. It has been reported that for two-level cervical spondylosis, two-level CDR has the same effects as two-level ACDF for the recovery of neurological function, and it even has superior results when assessed in terms of scales such as the Neck Disability Index score[11,12]. As a relatively new type of surgery, anterior hybrid surgery (HS) incorporates CDR and fusion procedures at different levels in one stage to treat multilevel cervical degenerative disc disease, and this procedure is gaining increasing attention. This method provides the most suitable treatment according to the characteristics of the disease at each level and is aimed at preserving segmental motion, avoiding long-segment fusions, and maintaining sagittal alignment and stability[13,14].
The challenges of these surgical techniques may be one of the most important reasons to discourage surgeons from using CDR or HS in multilevel cervical degenerative disc disease. In our surgical experience, the use of an inappropriate implantation sequence may lead to the migration of a previously inserted artificial disc during continuous two-level CDR[15]. In addition, many tapping processes are needed during CDR; therefore, the use of an inappropriate implantation sequence may also lead to the aggravation of spinal cord compression or the loosening of the inserted prosthesis. To perfectly maintain the normal functioning of cervical implants and to obtain satisfactory outcomes, we need to make a detailed plan for each surgical step and to perform surgery in a rational sequence. Any small imperfection in the surgical strategies of multilevel CDR and HS can cause unnecessary complications.
In this paper, we summarize our surgical strategies used in multilevel CDR and HS into five major notes, and we share the notes and our surgical procedure in the form of four typical case presentations. We hope that our strategies can help improve the performance and outcomes for multilevel CDR and HS. We also discuss the most suitable surgical procedures for these surgeries.
We have performed more than 800 CDR and 300 HS procedures in the past 15 years (all surgeries were performed by the same senior surgeon, H.L.). This experience allowed us to generate rational implantation strategies for multilevel CDR and HS. The safety profile and clinical outcomes of multilevel cervical spine surgery have been reported by our team before[16-18].
Spinal compression is usually highly severe in patients with multilevel cervical degenerative disc disease, and many tapping processes are needed during CDR; theoretically, if we do not decompress the index levels completely, the compression can be aggravated by the tapping procedure during implantation of the artificial disc. In addition, redundant tapping processes may affect the stability of the inserted implant or prosthesis by generating vibrations. Therefore, we suggest that two general principles of the strategies are necessary: First, the aggravation of spinal cord compression should be carefully avoided during manipulations; and second, the stability of the inserted prosthesis should not be influenced. To achieve these two general principles, five notes require attention.
First, for multilevel CDR or HS, decompression of the disc spaces and preparation of the endplates of all surgical segments should be carried out before the implants are inserted. Second, an appropriately sized implant trail or a rail punch should be used to maintain the intervertebral disc height before implantation of the prosthesis. Third, index levels indicating highly serious spinal cord compression require that decompression be prioritized. Fourth, for HS, CDR should be performed before cervical fusion surgeries such as ACDF and anterior cervical corpectomy decompression and fusion (ACCF). Finally, for surgeries including continuous two-level CDR, the rasping, drilling, and cutting processes of both surgical segments should be performed before artificial disc implantation, and the implantation of an artificial disc is a priority at upper index levels.
Details of the surgical procedures are stated below in the form of four typical case presentations.
The patients in the four cases were diagnosed with cervical degenerative disc disease. Surgical treatments were necessary for all patients to relieve their symptoms.
Case 1 (index levels indicating the presence of highly serious spinal cord compression requiring that decompression be prioritized): Neck pain and numbness of both upper limbs for 8 mo.
Case 2 (performance of disc replacement before fusion surgeries in HS): Numbness in both upper limbs for 1 year.
Case 3 (following a top-down implantation sequence in continuous two-level CDR): Neck pain and weakness of the right upper limb for 6 mo.
Case 4 (migration of an already inserted artificial disc during continuous two-level CDR due to the use of an inappropriate implantation sequence): Numbness of the left upper limb for 10 mo.
Case 1: This is a 54-year-old man who presented with neck pain and numbness of both upper limbs for 8 mo. He saw a doctor for conservative treatment 6 wk ago. However, his symptoms did not relieve.
Case 2: This is a 51-year-old woman who presented with numbness in both upper limbs for 1 year. The symptoms did not relieve after 4 wk of conservative treatment outside our hospital.
Case 3: A 41-year-old woman complained of neck pain and weakness of the right upper limb for 6 mo. The symptoms did not relieve after 3 mo of conservative treatment outside our hospital.
Case 4: A 45-year-old woman complained of numbness of the left upper limb for 10 mo. The numbness progressively aggravated and she experienced weakness in the left and right upper limbs for 6 mo.
Case 1: No abnormalities.
Case 2: Upon physical examination, the muscle strength of the right upper limb was found to be decreased.
Case 3: Upon physical examination, the muscle strength of the right arm was found to be decreased.
Case 4: No abnormalities.
No abnormalities.
Case 1: Upon examination, sensation was decreased in both upper limbs, as was muscle strength.
Case 4: Upon examination, the muscle strength of both upper limbs was found to be decreased.
The preoperative laboratory examinations reveal no abnormalities.
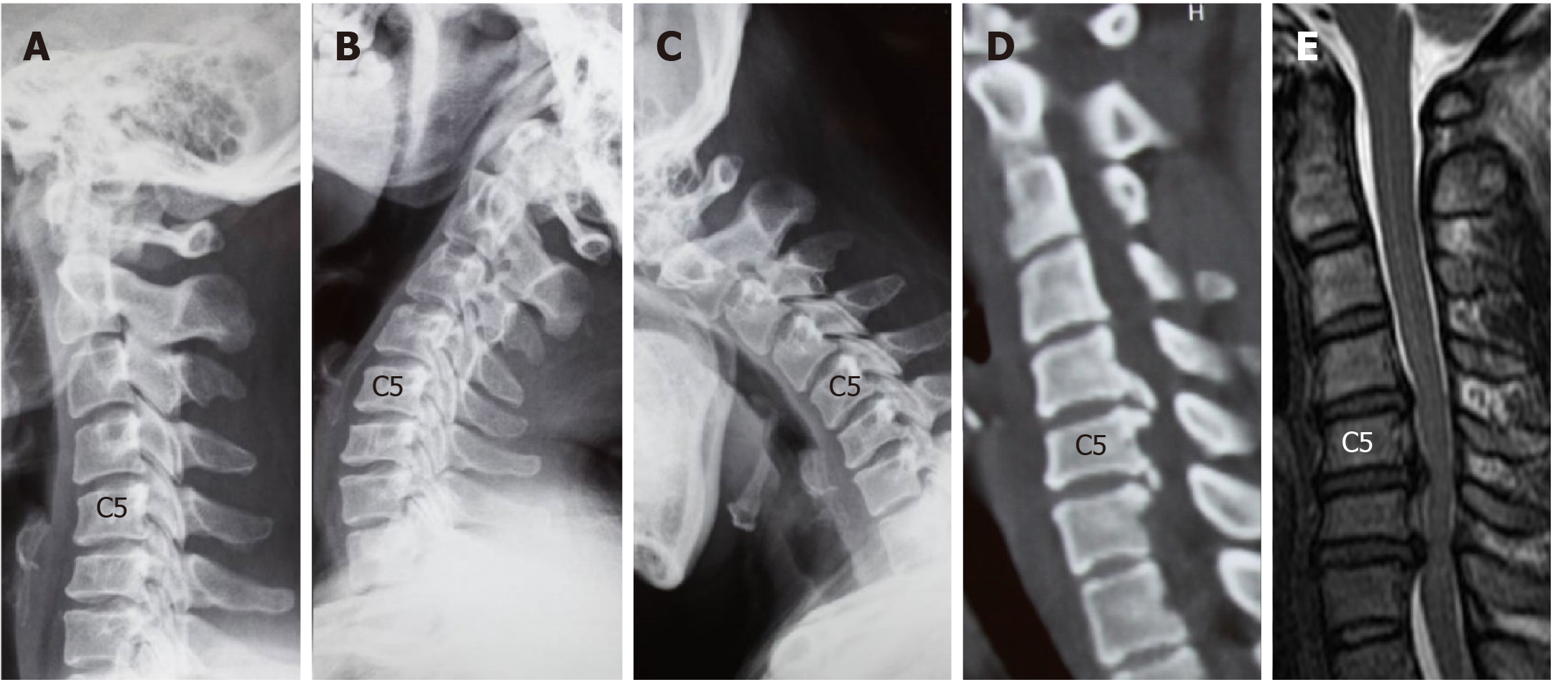
Case 1: A lateral radiograph showed a straightened cervical alignment, but this returned during flexion-extension movement. The disc height and ROM at C4/5 were reserved. A computed tomography (CT) scan showed severe osteophytes at the posterior border of C5/6 and C6/7 that needed extensive decompression. Magnetic resonance imaging (MRI) revealed cervical disc herniation at C4/5 and C6/7, and intervertebral foramen stenosis existed at C5/6 and C6/7 (Figure 1).
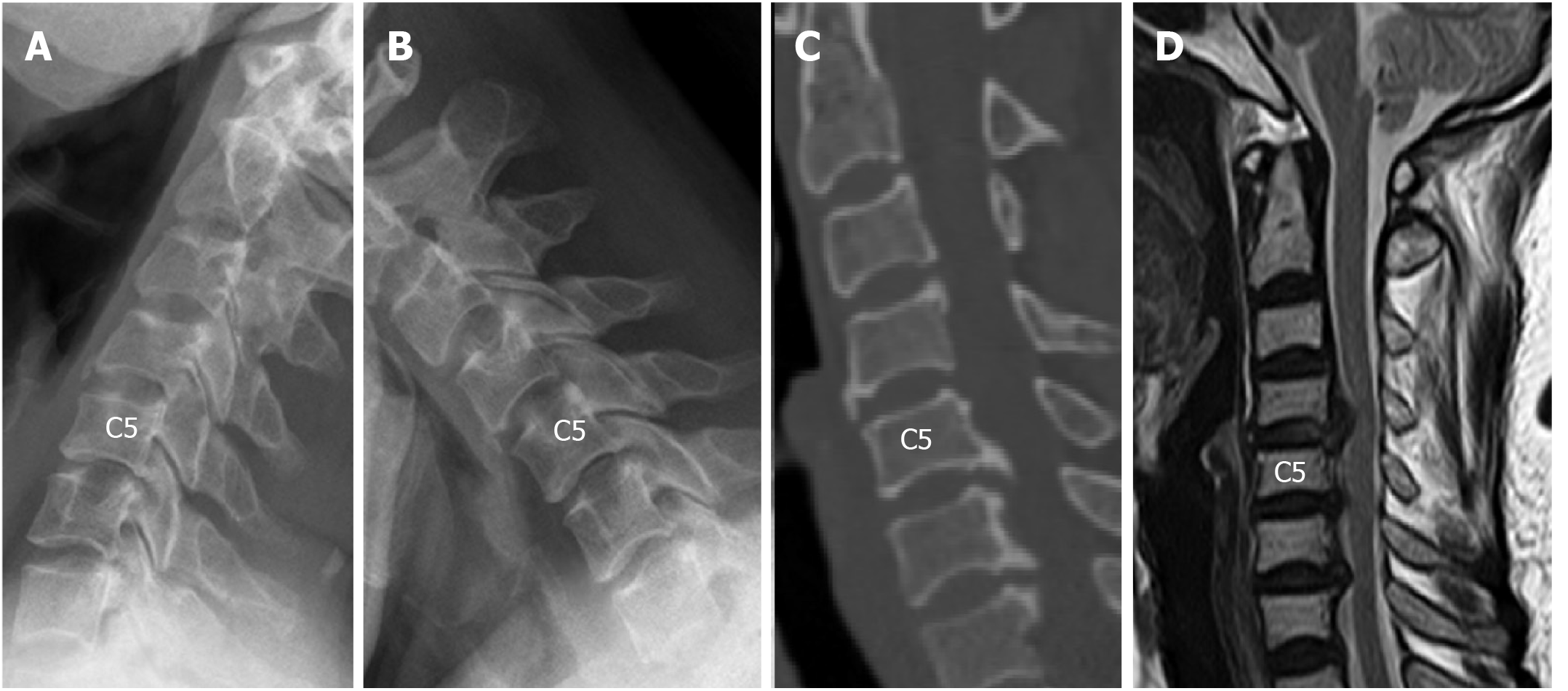
Case 2: The radiographs revealed that the intervertebral disc height was preserved at C4/5, C5/6, and C6/7, while the ROM at C5/6 was obviously decreased. A CT scan revealed large numbers of osteophytes at the posterior-inferior border of C5 and C6, which needed a wide range of removal. MRI showed multilevel spinal cord compression at C4/5, C5/6, and C6/7, and compression at C4/5 was caused by cervical disc herniation (Figure 2).
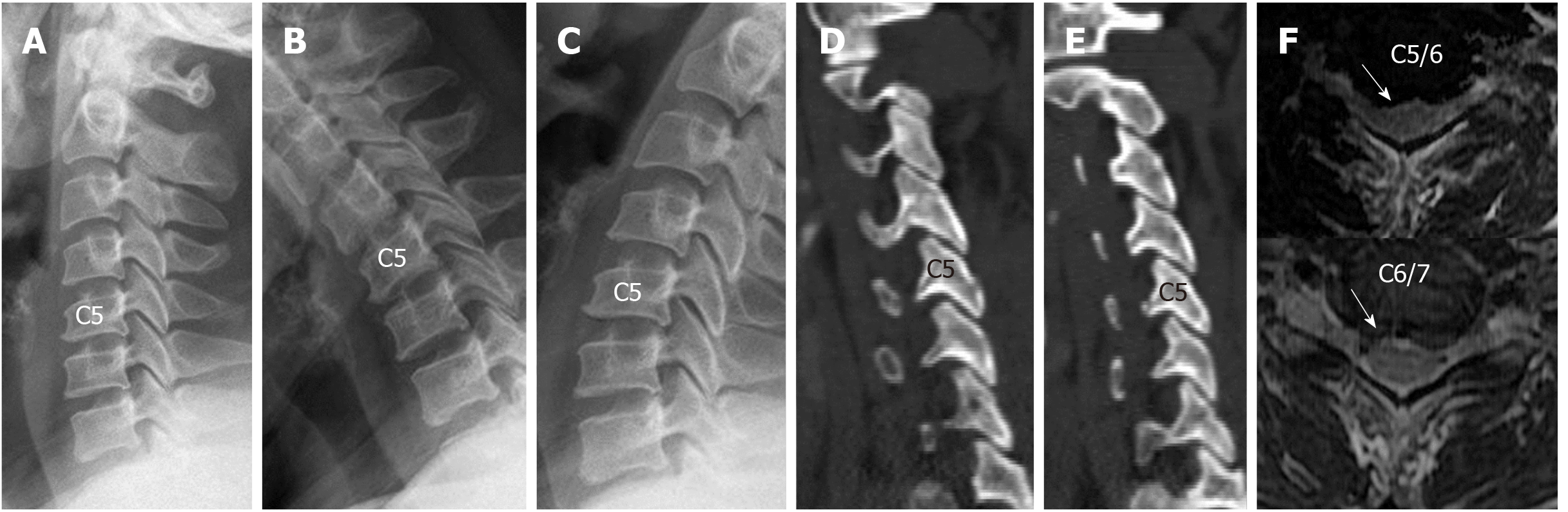
Case 3: Lateral radiographs showed that the intervertebral disc height at C5/6 and C6/7 was not obviously decreased, and the cervical alignment showed lordosis. The ROM at C5/6 and C6/7 was preserved. Spinal compression was mainly caused by disc herniation, and the facet joints were normal (Figure 3).
Case 4: Lateral radiographs showed that the ROM at C4/5 and C5/6 was preserved, and a CT scan showed that the reduction of the intervertebral disc height at both levels was < 30%. An MRI scan revealed soft disc herniation at the C4/5 and C5/6 levels (Figure 4).
C4/5 cervical disc herniation; C5/6 and C6/7 cervical spondylosis.
C4/5 cervical disc herniation; C5/6 and C6/7 cervical spondylosis.
C5/6 and C6/7 cervical disc herniation.
C4/5 and C5/6 cervical disc herniation.
We chose to perform ACCF at C6 to completely remove the osteophytes. The C4/5 segment underwent CDR to preserve ROM and avoid complications that may be caused by long segment fusion.
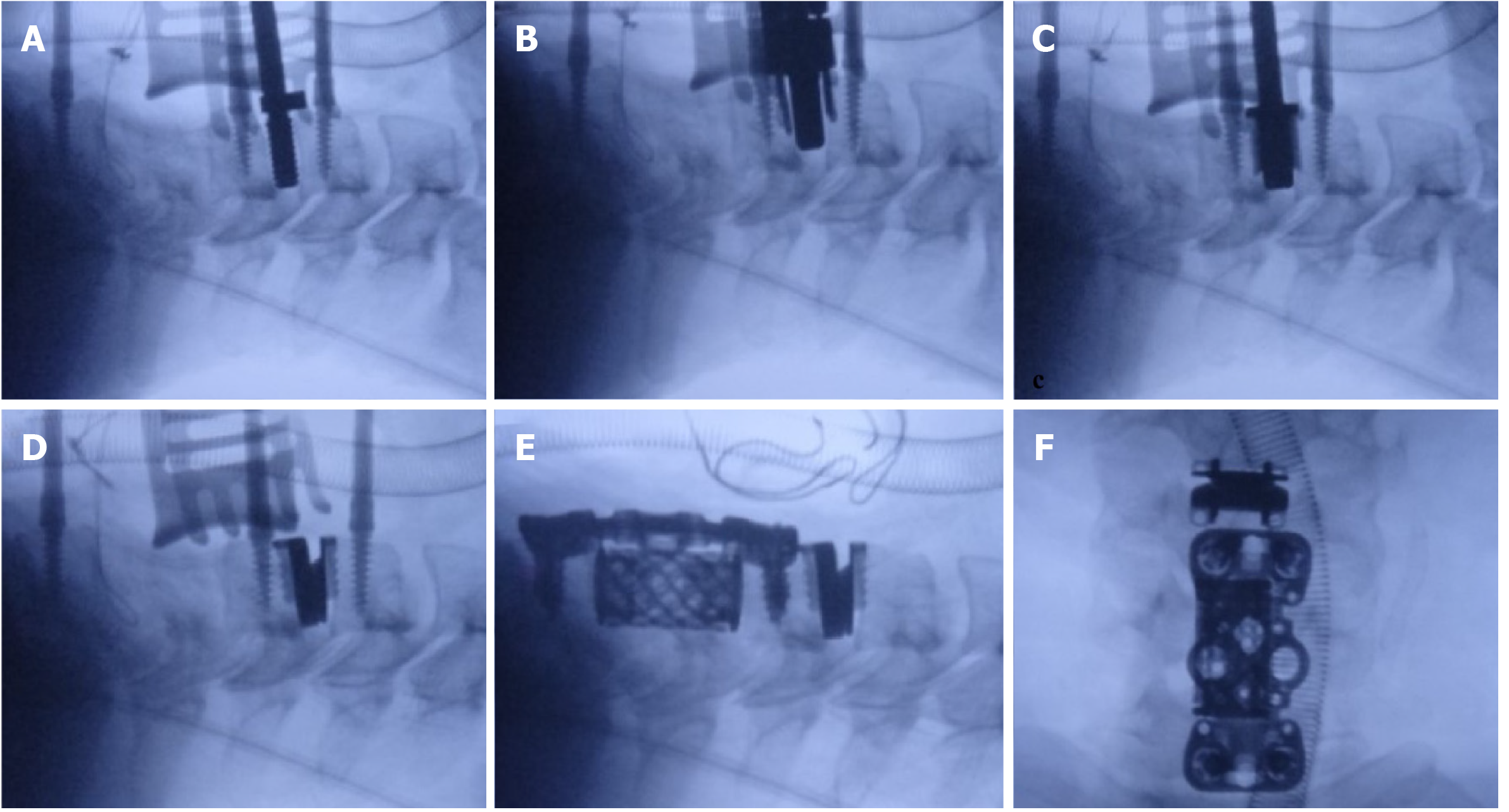
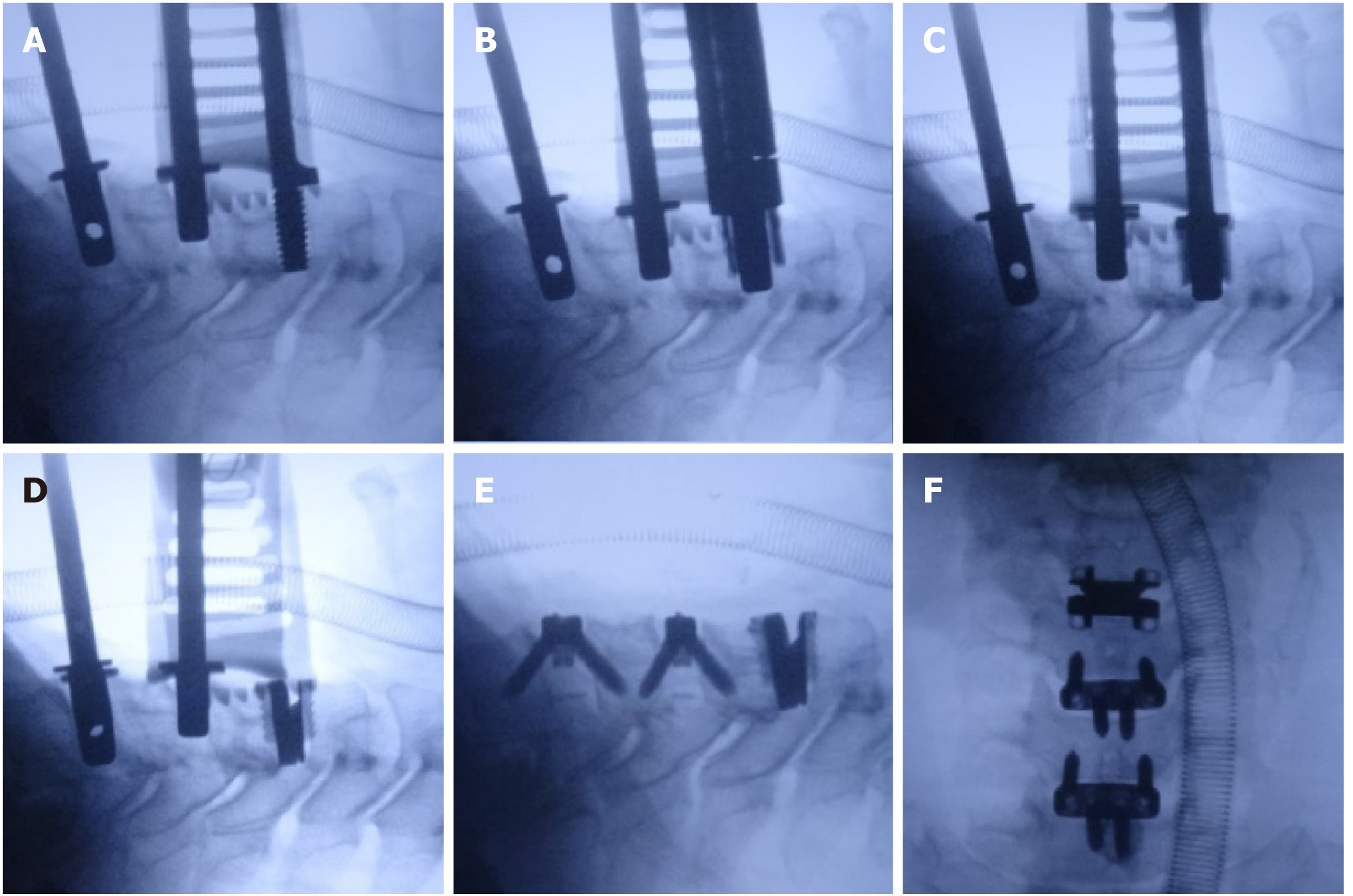
Surgical procedure (Figure 5): Because the compression at C5/6 and C6/7 was highly severe, decompression of the lower segment had to be completed first. The C6 vertebral body was cut, and the osteophytes at the posteroinferior border of C5 and at the posterosuperior border of C7 were burred away. The intervertebral foramen at C5/6 and C6/7 was decompressed. Decompression and endplate preparation were performed at C4/5. The artificial disc was implanted following a standard procedure at C4/5 (Figure 5A-D). After implanting an appropriate titanium mesh, ACCF was completed following a standard surgical process (Figure 5E and F).
We performed CDR at C4/5 using a Prestige-LP artificial disc and multilevel ACDF at C5/6 and C6/7 using the Zero-P system (Depuy Synthes Companies, United States).
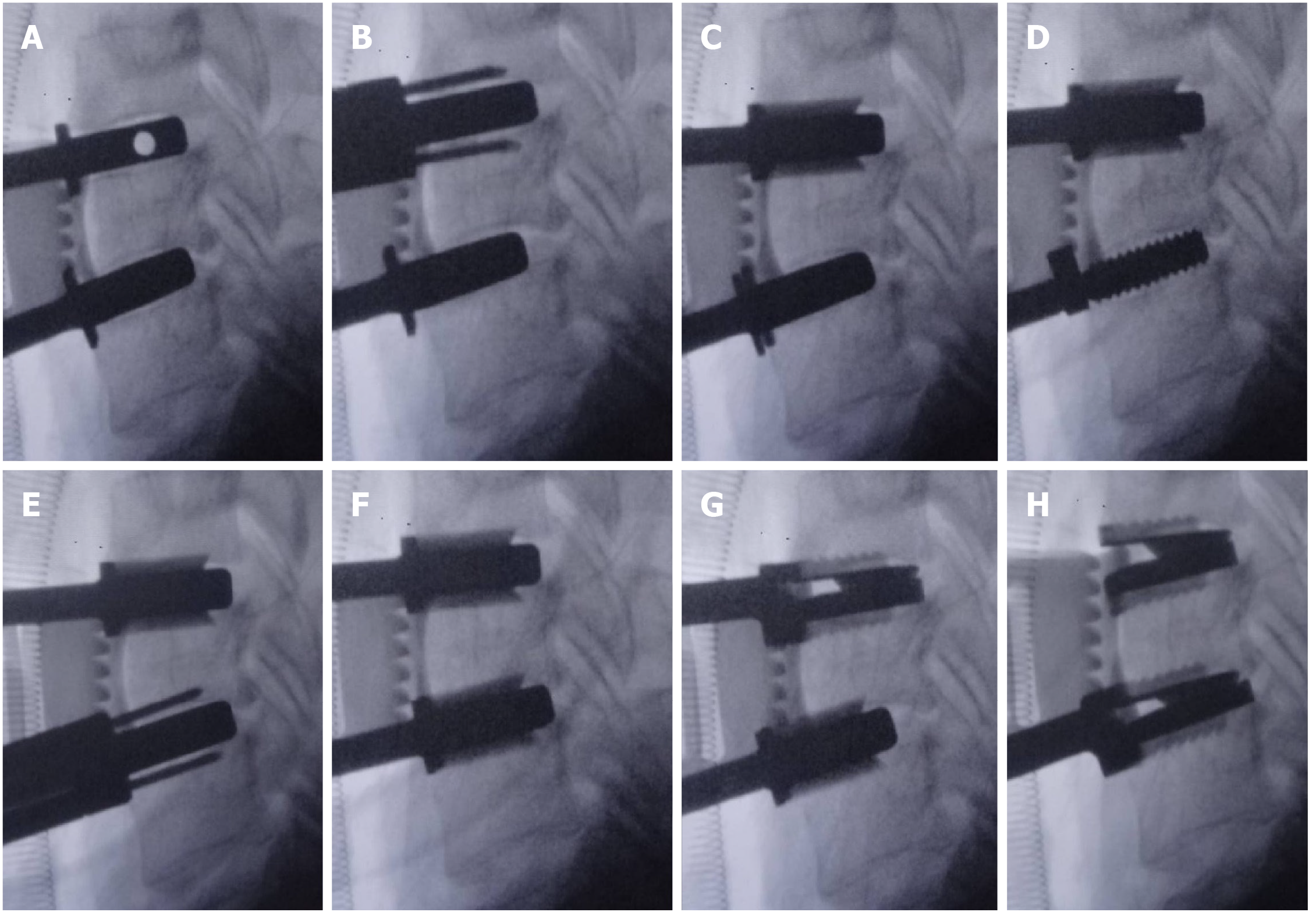
Surgical procedure (Figure 6): Decompression and endplate preparation were performed in a reasonable sequence. Index levels indicating highly serious spinal cord compression required that decompression be prioritized. An appropriately sized implant trail was used to maintain the disc space. The implant trail at C5/6 and C6/7 was reserved when preparing the disc space at C4/5 (Figure 6A and B). The implantation of an artificial disc at C4/5 was finished following a standard procedure (Figure 6C and D). Zero-P systems were implanted at C5/6 and C6/7. Lateral and anterior-posterior radiographs were recorded to verify that the prostheses were in a good position (Figure 6E and D).
The patient underwent two-level CDR at C5/6 and C6/7 using the Prestige-LP artificial disc to preserve ROM at both index levels.
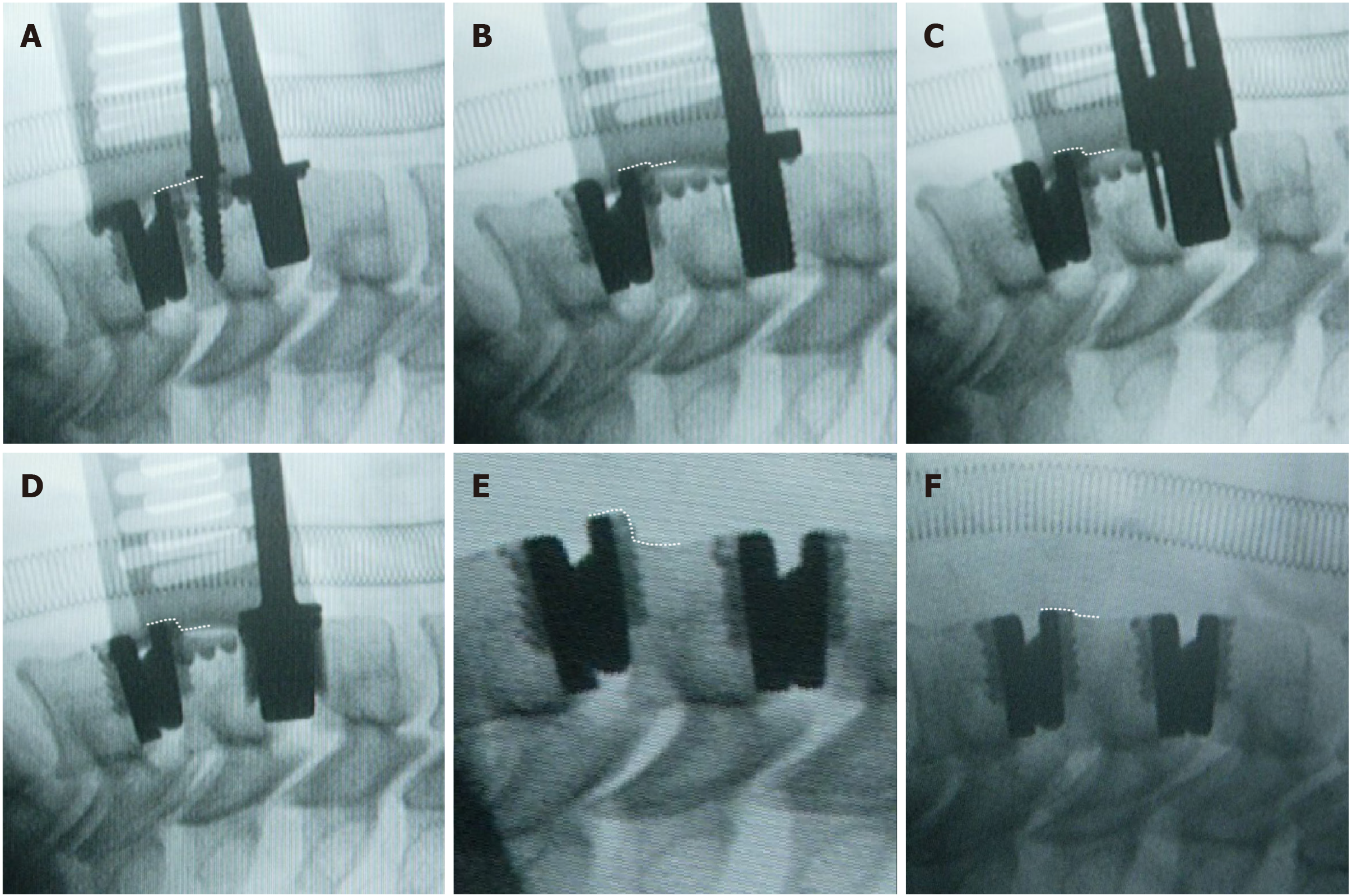
Surgical procedure (Figure 7): Decompression was performed at the C5/6 and C6/7 disc spaces. Appropriately sized implant trials were used to confirm the disc spaces (Figure 7A). Rasping, drilling, and cutting were performed at C5/6 following the standard procedures. During this process, the implant trial at C6/7 was reserved to maintain the intervertebral disc height (Figure 7B and C). Rasping, drilling, and cutting were also performed at C6/7 following the standard procedures. During this process, the rail punch at C5/6 was reserved to maintain the intervertebral disc height (Figure 7D-F). The artificial discs were implanted following a top-down sequence. First, the rail punch at C5/6 was removed, and an appropriately sized artificial disc was implanted; second, the rail punch at C6/7 was removed, and an appropriately sized artificial disc was implanted (Figure 7G and H).
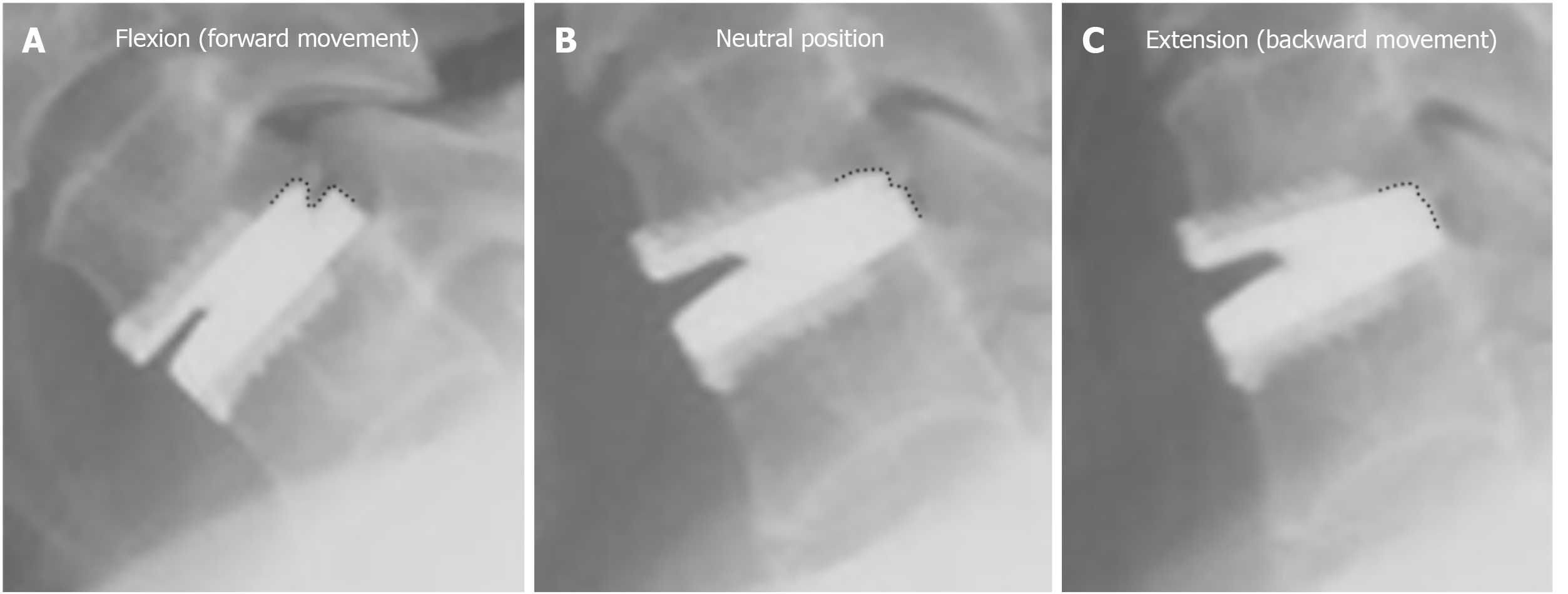
The examination findings revealed that the patient was able to undergo two-level CDR at C4/5 and C5/6 using the Prestige-LP artificial disc. During the implantation of the second artificial disc, the upper tab of the previously inserted artificial disc at C5/6 migrated forward due to the use of an inappropriate implantation sequence.
We followed a standard process to finish the decompression and the implant size selection procedure at C4/5 and C5/6, respectively. Then, we finished rasping, drilling, cutting, and disc implantation at C5/6 following a standard process (Figure 8A). A lateral radiograph revealed that the artificial disc at C5/6 was in a good position. We then started to address the C4/5-disc space. After the rasping procedure, the upper tab of the C5/6 artificial disc migrated forward (Figure 8B), and the upper tab continued to migrate during the drilling, cutting, and implantation of an artificial disc at C4/5 (Figure 8C-E). To test whether the artificial discs and index segments were unstable, we recorded flexion-extension intra-operative radiographs and found that the migration of the artificial disc at C5/6 was not aggravated during flexion and extension. For this reason, we tapped the upper tab at C5/6 back to the correct position (Figure 8F).
Complete decompression was performed in this patient; therefore, the symptoms were significantly relieved after surgery.
Complete decompression was performed in this patient; therefore, the patient obviously recovered.
After surgery, the patient’s symptoms were significantly relieved. Both prostheses were stable, and the ROMs at C5/6 and C6/7 were maintained during the long-term follow-up.
One week after surgery, we did not find migration of the artificial disc at C5/6. We tracked the patient for 8 years. Migration of the upper tab at C5/6 appeared 1 mo after surgery, but the migration did not progress over the next 8 years[15].
Compared with multilevel fusion surgeries, multilevel CDR and HS avoid limitations including the loss of ROM and the acceleration of adjacent segment degeneration. In addition, cervical HS is an individualized treatment option for multilevel cervical degenerative disc disease based on the degenerative features of each segment. While there are several technical challenges to performing multilevel CDR and HS, these approaches can be optimal options for properly indicated individuals. In this paper, we share our surgical strategies used in multilevel CDR and HS and sum up the main points as follows:
Note 1: For multilevel CDR or HS, decompression of the disc spaces and preparation of the endplates of all surgical segments should be carried out before the implants are inserted.
Note 2: An appropriately sized implant trail or a rail punch should be used to maintain the intervertebral disc height before implantation of the prosthesis.
Note 3: Index levels indicating highly serious spinal cord compression require that decompression be prioritized.
Note 4: For HS, CDR should be performed before cervical fusion surgeries such as ACDF and anterior cervical corpectomy decompression and fusion.
Note 5: For surgeries including continuous two-level CDR, the rasping, drilling, and cutting processes of both surgical segments should be performed before artificial disc implantation, and the implantation of an artificial disc is a priority at upper index levels.
By presenting four typical cases, we discuss the main processes used in different kinds of surgery in detail.
In case 1, we first decompressed the C5-7 segments, which showed more serious compression, as mentioned in note 3. Some evidence suggests that the intense manipulation involved can lead to undesirable damage to the spinal cord during surgery[19-21]. Additionally, as we described earlier, spinal cord compression is usually more serious for multilevel cervical spondylosis. These findings indicate that spine surgery requires elaborate and gentle manipulation, especially during multilevel anterior cervical surgeries. Moreover, many tapping processes are performed during CDR; therefore, in cases where spinal cord compression is aggravated and causes unwanted damage during the tapping procedure, an index level with highly serious spinal cord compression requires prioritized decompression.
This is a typical case demonstrating our implantation strategies used in multilevel cervical HS. We first performed decompression and endplate preparation for all segments before implantation, as described in note 1. This helps to avoid too much manipulation with fluoroscopy.
When we dealt with one of the surgical segments, other surgical disc spaces were maintained with an appropriately sized implant trail, as described in note 2. This could contribute to the stability of the index segments during implantation. For example, after removing the intervertebral disc at C5/6, the mainly connected part of the C5 and C6 vertebrae did not exist. Therefore, the integral cervical spine was broken into two relatively independent parts, and the ROM of the C5 vertebra relative to the C6 vertebra increased. By reserving the implant trail at the C5/6 level, the cervical spine became whole again, and the relative motion of the C5 vertebra was limited. If we had not reserved the implant trail at C5/6, the C5 vertebra would rock with the tapping processes during rasping, drilling, cutting, and implanting, and this condition does not favor the CDR procedures. Some surgeons consider the distraction of the disc to be easier if the trail is not inserted while operating the next level. However, the implantation of Prestige-LP does not require a “distraction-compression” process.
In multilevel cervical HS, we perform CDR before fusion surgeries, as described in note 4. As mentioned earlier, CDR requires many tapping processes. The vibration generated by excessive tapping processes causes the fusion cage or the screws to loosen if CDR is performed last. For this reason, a reduction in the number of tapping processes is needed to ensure the stability of the implants that have been inserted, and it is better to perform CDR before fusion surgeries.
In this case of continuous two-level CDR, we reserved an implant trail or rail punch in one of the disc spaces to maintain the intervertebral disc height when dealing with the other disc space, as described in note 2.
The principles of performing continuous two-level CDR are listed in note 5. We first finished the rasping, drilling, and cutting processes at both levels before artifact implantation. If we performed rasping, drilling, and cutting at C5/6 after the implantation of the artificial disc at C4/5, the primary stability of the inserted artificial disc might have been affected by the impact force and vibration generated by those tapping processes. In addition, we implanted the artificial disc at C4/5 (the upper segment) primarily; otherwise, if we followed a bottom-up implantation sequence, the already inserted prosthesis at C5/6 (the lower segment) would migrate when implanting the prosthesis at C4/5 (the upper segment), as that occurring in case 4.
The migration of a previously inserted artificial disc is related to the design philosophy of the Prestige-LP cervical disc. The Prestige-LP disc is designed with a ball and trough structure, with the ball on the upper tab and the trough on the lower tab. Furthermore, the ball on the upper tab is located towards the back (Figure 9). This unique structure allows the upper tab of the Prestige-LP cervical disc to move transversely relative to the lower tab, as the forward displacement is longer, and there is little backward transverse displacement (Figure 9A-C).
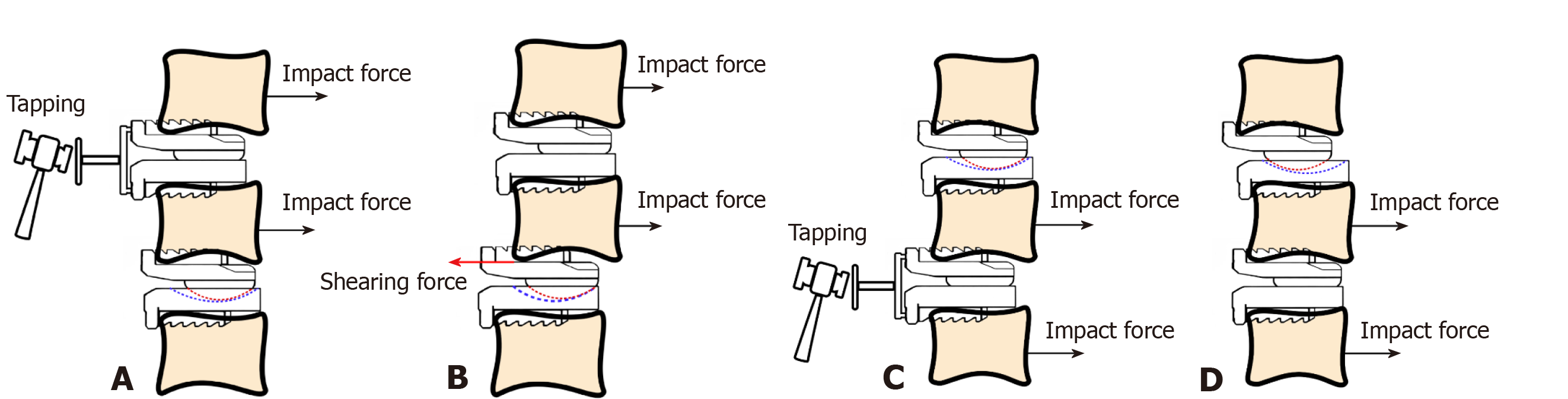
In case 4, we followed a bottom-up sequence and first inserted a prosthesis at C5/6; then, we started working with the disc space at C4/5. Therefore, the C5 vertebral body and the inserted prosthesis at C5/6 were subjected to many redundant tapping processes. Every tapping process generated an impact force that allowed the C5 vertebra as well as the upper tab of the prosthesis at C5/6 to move backward (Figure 10A and B). As described previously, the upper tab of the Prestige-LP cervical disc could barely move backward relative to the lower tab; consequently, when the C5 vertebral body continued to move backward with the impact force while the upper tab remained unmoved, a shearing force was generated between the C5 vertebral body and the upper tab of the prosthesis at C5/6 (Figure 10B). For this reason, the upper tab of the previously inserted prosthesis at C5/6 migrated forward. Conversely, if we had followed a top-down sequence and first inserted a prosthesis at C4/5 and then at C5/6, the migration of the previously inserted prosthesis at C4/5 would not have occurred (Figure 10C and D). The explanation for this is that if we subsequently insert a prosthesis at C5/6, the C5 vertebral body as well as the lower tab of the prosthesis at C4/5 will be affected by the impact of the tapping processes (Figure 10C). Considering that the upper tab was able to move forward relative to the lower tab, the lower tab at C4/5 would have moved backward together with the C5 vertebral body, which is different from the situation in case 4. The anterior border of the socket on the lower tab at C4/5 would not continue to contact the ball on the upper tab, so the transverse movement of the lower tab at C4/5 could not be blocked. Therefore, the shearing force between the C5 vertebral body and the lower tab at C4/5 would not be generated, and migration of the prosthesis would not occur (Figure 10D).
A major limitation of this study is that we did not report the cumulative incidence of the effectiveness and of the complications of these procedures. Another limitation is that we did not compare our surgical techniques with other procedures. Future study should address these issues.
The use of an inappropriate implantation sequence in multilevel cervical spine surgery may lead to complications such as the migration of a previously inserted artificial disc, the aggravation of spinal cord compression, and the loosening of implants. We verified the rationality and safety of our strategies by performing many surgeries and by carefully analyzing each case. We hope that our surgical strategies can help improve the performance and outcomes of multilevel cervical spine surgery. We believe that meticulous attention to surgical procedures can help surgeons improve the performance of multilevel cervical disc replacement and hybrid surgery.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Stavroulopoulos A S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Li JH
| 1. | van Eck CF, Regan C, Donaldson WF, Kang JD, Lee JY. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine (Phila Pa 1976). 2014;39:2143-2147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Carrier CS, Bono CM, Lebl DR. Evidence-based analysis of adjacent segment degeneration and disease after ACDF: a systematic review. Spine J. 2013;13:1370-1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, Darden B. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9:275-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 410] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 4. | Anderson PA, Nassr A, Currier BL, Sebastian AS, Arnold PM, Fehlings MG, Mroz TE, Riew KD. Evaluation of Adverse Events in Total Disc Replacement: A Meta-Analysis of FDA Summary of Safety and Effectiveness Data. Global Spine J. 2017;7:76S-83S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Janssen ME, Zigler JE, Spivak JM, Delamarter RB, Darden BV 2nd, Kopjar B. ProDisc-C Total Disc Replacement Versus Anterior Cervical Discectomy and Fusion for Single-Level Symptomatic Cervical Disc Disease: Seven-Year Follow-up of the Prospective Randomized U.S. Food and Drug Administration Investigational Device Exemption Study. J Bone Joint Surg Am. 2015;97:1738-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 6. | Lavelle WF, Riew KD, Levi AD, Florman JE. Ten-year Outcomes of Cervical Disc Replacement with the BRYAN Cervical Disc: Results From a Prospective, Randomized, Controlled Clinical Trial. Spine (Phila Pa 1976). 2019;44:601-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 96] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 7. | Gornet MF, Lanman TH, Burkus JK, Dryer RF, McConnell JR, Hodges SD, Schranck FW. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial. J Neurosurg Spine. 2019;1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | Gornet MF, Burkus JK, Shaffrey ME, Schranck FW, Copay AG. Cervical disc arthroplasty: 10-year outcomes of the Prestige LP cervical disc at a single level. J Neurosurg Spine. 2019;31:317-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 9. | Laxer EB, Brigham CD, Darden BV, Bradley Segebarth P, Alden Milam R, Rhyne AL, Odum SM, Spector LR. Adjacent segment degeneration following ProDisc-C total disc replacement (TDR) and anterior cervical discectomy and fusion (ACDF): does surgeon bias effect radiographic interpretation? Eur Spine J. 2017;26:1199-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Park DK, Lin EL, Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion: in vivo quantitative radiographic analysis. Spine (Phila Pa 1976). 2011;36:721-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Phillips FM, Lee JY, Geisler FH, Cappuccino A, Chaput CD, DeVine JG, Reah C, Gilder KM, Howell KM, McAfee PC. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. 2-year results from the US FDA IDE clinical trial. Spine (Phila Pa 1976). 2013;38:E907-E918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 162] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 12. | Gornet MF, Lanman TH, Burkus JK, Hodges SD, McConnell JR, Dryer RF, Copay AG, Nian H, Harrell FE. Cervical disc arthroplasty with the Prestige LP disc versus anterior cervical discectomy and fusion, at 2 levels: results of a prospective, multicenter randomized controlled clinical trial at 24 months. J Neurosurg Spine. 2017;26:653-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 87] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 13. | Wu TK, Wang BY, Cheng D, Rong X, Lou JG, Hong Y, Liu H. Clinical and radiographic features of hybrid surgery for the treatment of skip-level cervical degenerative disc disease: A minimum 24-month follow-up. J Clin Neurosci. 2017;40:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Wu TK, Wang BY, Deng MD, Hong Y, Rong X, Chen H, Meng Y, Liu H. A comparison of anterior cervical discectomy and fusion combined with cervical disc arthroplasty and cervical disc arthroplasty for the treatment of skip-level cervical degenerative disc disease: A retrospective study. Medicine (Baltimore). 2017;96:e8112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Meng Y, Wang X, Zhao Z, Wang B, Wu T, Liu H. Intraoperative Anterior Migration of the Prestige-LP Cervical Disc Owing to an Inappropriate Implantation Sequence During Continuous 2-Level Artificial Cervical Disc Replacement: A Case Report with 8-Year Follow-Up. World Neurosurg. 2018;116:194-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Hu L, Wu T, Liu H, Wang B, Zhang J, Meng Y, Ding C, Gao X, Hong Y. Influence of Fusion on the Behavior of Adjacent Disc Arthroplasty in Contiguous 2-Level Hybrid Surgery In Vivo. World Neurosurg. 2019;132:e929-e940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Wu TK, Meng Y, Wang BY, Hong Y, Rong X, Ding C, Chen H, Liu H. Is the behavior of disc replacement adjacent to fusion affected by the location of the fused level in hybrid surgery? Spine J. 2018;18:2171-2180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Gao X, Yang Y, Liu H, Meng Y, Zeng J, Wu T, Hong Y. A Comparison of Cervical Disc Arthroplasty and Anterior Cervical Discectomy and Fusion in Patients with Two-Level Cervical Degenerative Disc Disease: 5-Year Follow-Up Results. World Neurosurg. 2019;122:e1083-e1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Yang DL, Zhang YZ, Shen Y, Cao JM. Surgical management of cervical cord injury with ossification of the cervical posterior longitudinal ligament. Orthop Surg. 2011;3:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Mahale YJ, Silver JR, Henderson NJ. Neurological complications of the reduction of cervical spine dislocations. J Bone Joint Surg Br. 1993;75:403-409. [PubMed] |
| 21. | Daniels AH, Hart RA, Hilibrand AS, Fish DE, Wang JC, Lord EL, Buser Z, Tortolani PJ, Stroh DA, Nassr A, Currier BL, Sebastian AS, Arnold PM, Fehlings MG, Mroz TE, Riew KD. Iatrogenic Spinal Cord Injury Resulting From Cervical Spine Surgery. Global Spine J. 2017;7:84S-90S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |