Published online Sep 6, 2020. doi: 10.12998/wjcc.v8.i17.3875
Peer-review started: May 20, 2020
First decision: June 7, 2020
Revised: June 27, 2020
Accepted: August 6, 2020
Article in press: August 6, 2020
Published online: September 6, 2020
Processing time: 106 Days and 19.2 Hours
Spontaneous rupture and hemorrhage of renal angiomyolipoma (RAML) is a life-threatening clinical emergency. When it occurs during pregnancy, it is compared to a “bomb explosion,” which makes the diagnosis and treatment more challenging. An ultrasound examination is a quick and safe examination with the benefit of no radiation exposure, which is always preferred for pregnant women. Currently, cases of spontaneous rupture and hemorrhage of RAML during pregnancy are rare, as is the diagnostic value and characteristics of ultrasound. The lack of understanding of the condition among ultrasound doctors makes it prone to misdiagnosis. In this study, we present the case of a pregnant woman who was preliminarily diagnosed with spontaneous rupture and hemorrhage of the left RAML using ultrasound and discuss the ultrasound characteristics.
A 38-year-old woman in her 19th wk of pregnancy (G2P1) was referred to our clinic for a sudden, persistent pain on the left side of the waist. She had not undergone any previous related abdominal examination. Ultrasound of the urinary system revealed a giant nonhomogenous lump in the left kidney area. The diagnosis was considered spontaneous rupture and hemorrhage of the left RAML in pregnancy via ultrasound. Her left-side waist pain continued to be intense. Subsequently, she underwent computed tomography, which led to the same diagnosis. Based on many factors, the patient underwent left nephrectomy after the induction of labor. The pathological result was the rupture and hemorrhage of a vascular leiomyoma lipoma.
Ultrasound examination plays an important role in the diagnosis of the spontaneous rupture and hemorrhage of RAML during pregnancy.
Core tip: The diagnosis and treatment of spontaneous rupture and hemorrhage of renal angiomyolipoma during pregnancy are challenging because it is a life-threatening clinical emergency. We present the case of a pregnant woman who was preliminarily diagnosed with the condition using ultrasound and discuss the ultrasound characteristics. Ultrasound is a quick and safe examination with no radiation exposure and is preferred for pregnant women. Although pathology remains the gold standard for diagnosis, ultrasound can facilitate a preliminary diagnosis, leading to differential diagnosis to reduce misdiagnosis, prompting further diagnosis and treatment. Therefore, ultrasound plays a crucial role in the diagnosis of this condition.
- Citation: Zhang T, Xue S, Wang ZM, Duan XM, Wang DX. Diagnostic value of ultrasound in the spontaneous rupture of renal angiomyolipoma during pregnancy: A case report. World J Clin Cases 2020; 8(17): 3875-3880
- URL: https://www.wjgnet.com/2307-8960/full/v8/i17/3875.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i17.3875
Renal angiomyolipoma (RAML), a common benign tumor, is composed of mature blood vessels, smooth muscle, and fatty tissue. Some scholars believe that RAML consists solely of tumors and may originate from epithelioid cells around the blood vessels[1]. Its incidence in the general population is estimated to be 0.13%, and about 80% of affected patients are women[2,3]. Spontaneous rupture and hemorrhage is a life-threatening primary complication of RAML. Pregnancy is a risk factor for increasing the size, leading to rupture of RAML. Because computed tomography (CT) exposes the patient to radiation and magnetic resonance imaging (MRI) is time-consuming, these imaging methods are not always advised for pregnant women. Ultrasound is a quick and convenient method that does not predispose the patient to radiation; therefore, it is preferred for pregnant women. However, because ultrasound doctors lack understanding of the disease, it is more prone to misdiagnosis.
A 38-year-old woman in her 19th wk of pregnancy (G2P1) was referred to our clinic for a sudden persistent pain on the left side of the waist on July 28, 2017.
The patient’s physical examination revealed tenderness over the left kidney area. Her blood pressure was 120/85 mmHg, heart rate was 86 beats/min, and body temperature was 36.8 °C. The patient had no significant medical history. She had not undergone any related abdominal examination previously.
The patient had no significant medical history. She had not undergone any related abdominal examination previously.
The patient was hospitalized and given conservative treatment, but her left-side waist pain continued to be intense. Because the size of the tumor was so large, and the fetal heart rate was unstable, the patient decided to undergo left nephrectomy after the induction of labor.
Laboratory tests indicated that the patient’s hemoglobin level was 80 g/L, and the hematocrit was 0.242 L/L. On the 2nd d, hemoglobin was 95 g/L, and the hematocrit was 0.286 L/L.
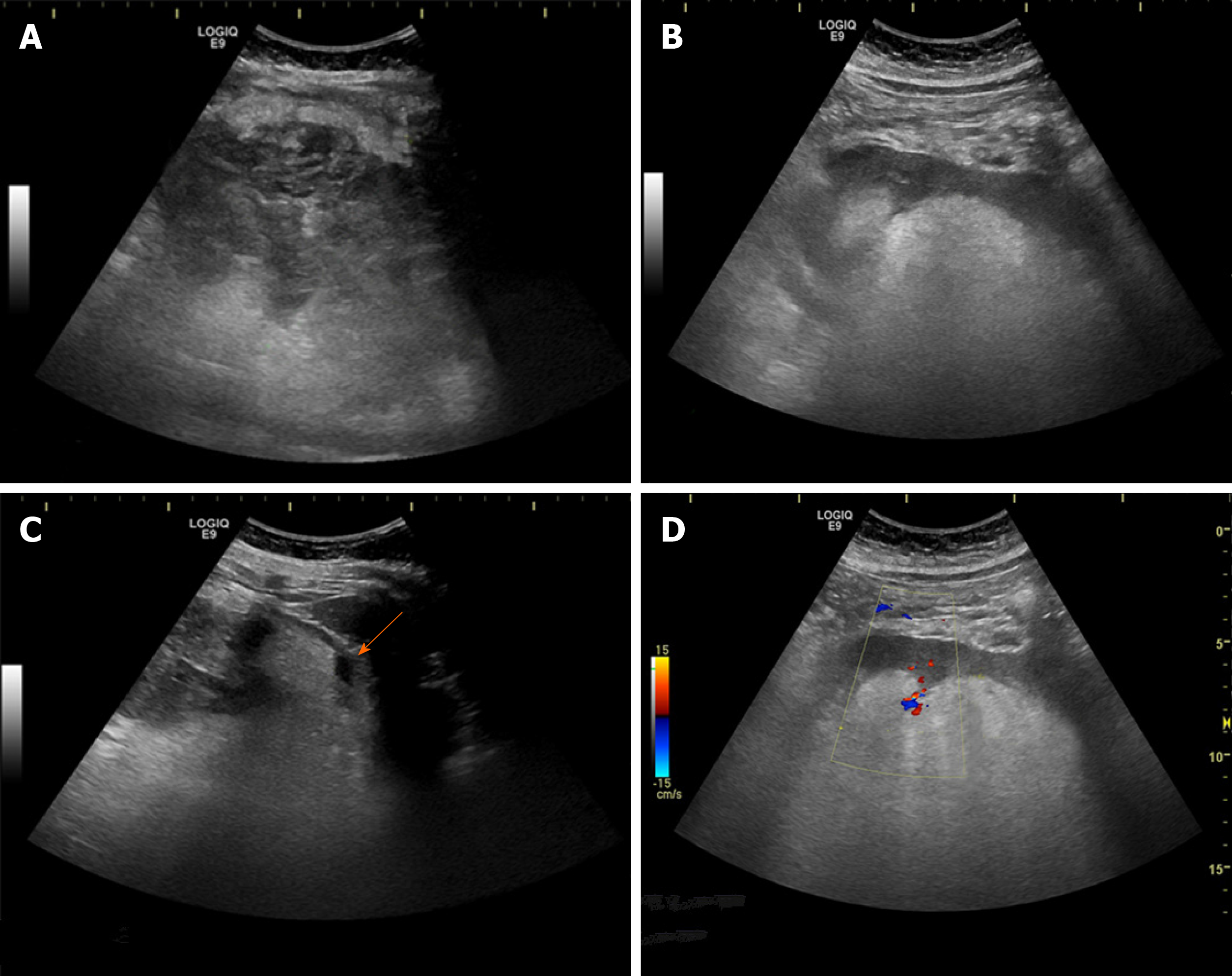
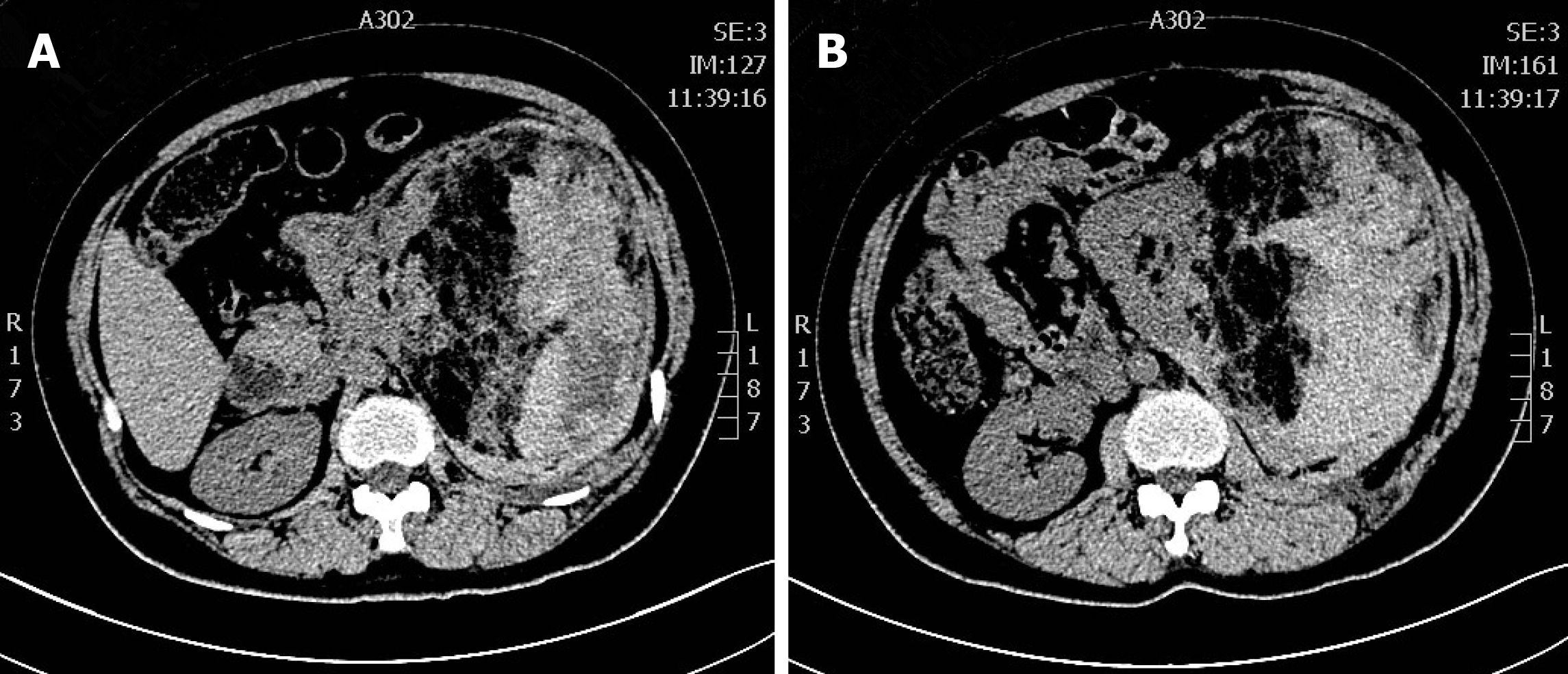
Ultrasound examination of the urinary system (LOGIQ E9, GE) revealed a giant nonhomogenous lump in the left kidney area, which had caused the left kidney to move to the midabdomen. The size of the lump was approximately 159 mm × 100 mm, and the border was faintly visible. The lump showed a “striped sign” in which the outer part was hypoechoic with a strong stripe echo (Figure 1A), and the inner part near the left kidney was hyperechoic (Figure 1B). A stripe-shaped echoless zone was seen around the lump (Figure 1C) (arrow). Color Doppler flow image showed some spot-like blood flow signals around the lump (Figure 1D). A hyperechoic nodule was seen in the right kidney with a size of 30 mm × 25 mm. There was a fetus echo in the uterus. Preoperative CT showed a large, mixed-density mass in the left kidney (Figure 2). The density of the area adjacent to the kidney was low, and the area far from the kidney showed high density.
The final diagnosis of the present case was rupture and hemorrhage of the left RAML, right kidney hamartoma, and pregnancy.
The patient underwent left nephrectomy after the induction of labor. During the operation the renal artery spurted after the left nephrectomy, the blood pressure dropped to 80/50 mmHg, and the blood loss reached 1000 mL. Four units of red blood cell suspension were transfused after emergency hemostasis, and the blood pressure rose to 100/60 mmHg. After the operation, gastrointestinal decompression and intravenous nutrition were given to the patient. The gastric tube was removed on the 2nd d after the patient exhausted. Antibiotics were continuously applied for 5 d, and the patient was discharged on the 6th d after the operation.
The pathological result was rupture and hemorrhage of the vascular leiomyoma lipoma. We instructed the patient to review regularly every 6 mo, but the patient has not reviewed in our hospital.
RAML, a common benign tumor, is composed of mature blood vessels, smooth muscle, and fatty tissue. Spontaneous rupture and hemorrhage is one of the main complications of RAML, which may be related to the lack of elastic fibers in the blood vessel wall or the sudden increase in renal intratumor and intravascular pressure. It is generally considered that tumors with a diameter of > 4 cm are more likely to rupture. However, there are tumors smaller than 4 cm that can still rupture[4]. Thus, an assessment based only on tumor size is not accurate. Aneurysm formation, tuberous sclerosis complex (TSC), pregnancy coagulopathy, trauma, and hormone levels are also closely associated with rupture[2]. About 80% of patients with TSC can develop angiomyolipoma[2], and approximately 20% of patients have TSC[5]. The TSC-related renal hamartomas tend to be multiple, large, and bilateral, and these lesions are more likely than isolated lesions to rupture[6].
Although rupture and hemorrhage of RAML during pregnancy is rare, this condition has received increasing attention because of the difficulty of diagnosis and treatment. The rupture of RAML can occur at various stages of pregnancy. One study reported that the mean gestational age of patients was 27.7 wk, and the average tumor size was 10.1 cm at the time of diagnosis[7]. Pregnancy also plays a role in the growth and rupture of RAML, but the mechanism is not clear. Studies have shown that about 25% of patients have estrogen and progesterone receptors in tumor specimens, and estrogen levels increase during pregnancy, which may accelerate tumor growth[8]. In addition, the increase in circulating blood volume during pregnancy, which causes an increase in blood pressure, coupled with the rise of intra-abdominal pressure, may contribute to the growth and rupture of RAML.
In the clinical setting, patients may present with severe pain on one side of the waist, and the huge mass may be palpated or can manifest as gross hematuria. As we all know, ultrasound is a quick and safe examination with no radiation exposure, and it is always preferred for pregnant women. Because a typical RAML is rich in fat, ultrasound examination is sensitive and can show a hyperechoic nodule. For the low-fat RAMLs, ultrasound, which shows various forms of echo mode, is not very sensitive or accurate[9]. At this time, an ultrasound must be combined with other imaging methods, such as CT and MRI.
The ultrasound findings of rupture and hemorrhage of RAML show a strong, lamellar heterogeneous echogenic mass, similar to “onion skin” in the kidney area when it occurs under the renal capsule. It should be distinguished from the nonbleeding hamartomas, which also can appear as mixed. If the tumor ruptures and bleeds out of the renal capsule, there is a stripe echoless zone around the hematoma, and the no-echo area may be more reliable for the diagnosis of the rupture. The Color Doppler flow image can measure the blood flow of the tumor and determine the presence of an aneurysm. Contrast-enhanced ultrasound can identify the presence of hematomas and the existence of active bleeding and aneurysm formation[10].
Differential diagnosis includes obstetric factors such as abruptio placentae, placenta previa, uterine rupture, and ruptured ectopic pregnancy. In addition, it also needs to be distinguished from bilateral renal cell carcinoma, perinephric abscess, and primary retroperitoneal tumor. Renal cell carcinoma has general characteristics of cancer. The patient with typical renal cell carcinoma will have intermittent, painless, gross hematuria clinically. Most of them are hypoechoic on ultrasound, and the color blood flow is mostly spherical. For the atypical cases, combining enhanced CT or MRI can improve the accuracy of diagnosis.
In summary, although the gold standard for diagnosis is pathology, ultrasound examination can facilitate a preliminary diagnosis with its characteristics. Combining clinical data (female with TSC, related medical history, multiple bilateral hyperechoic nodules, and clinically with acute low back pain) can increase the accuracy of ultrasound diagnosis.
In the ultrasound images of this case, the inside part of the mass near the left kidney was homogeneously hyperechoic, which highly suggested the diagnosis of hamartoma. The lateral part of the mass was hypoechoic with a strong stripe-like echoless area, which suggested the diagnosis of rupture and hemorrhage. In addition, the patient appeared with a sudden persistent pain on the left waist, and the ultrasound showed a right kidney hamartoma, which was more helpful for the diagnosis.
At present, no consensus has been reached on the optimal treatment for this condition. When an RAML is detected during pregnancy, the patient should be informed of the risk of rupture. If the tumor is large (i.e. > 4 cm), active surgery or arterial embolization before pregnancy is recommended. Studies have shown that renal artery embolization with less trauma has better nephron retention than surgery[11], especially for patients with TSC or bilateral multiple hamartomas[12]. For patients with ruptured hemorrhage during pregnancy, the most appropriate treatment depends on the gestational week and the condition of the pregnant woman. When RAML causes maternal hemodynamic instability, it should be managed actively with surgical treatment or arterial embolization simultaneously with antishock therapy. If the patient’s blood pressure is stable, and tumor bleeding is steady with no progression, temporary conservative treatment can be considered[13]. Alongside close clinical observation, the patient may choose natural birth or pregnancy termination before treating the lesion. After 28 wk of pregnancy, if the fetus’s lungs are mature and the mother’s condition is severe, a cesarean delivery may be required to terminate the pregnancy. There are some successful cases in the literature of conservative treatment[13-15], and there is also a case report of a patient who underwent radical nephrectomy during pregnancy while continuing the pregnancy to full term, which of course, is associated with very great challenges[16].
In addition, for the patients undergoing conservative treatment, ultrasound has an advantage of no fetal radiation damage. For the patients who cannot perform MRI in the emergency department, or who need emergency surgery in critical condition, ultrasound is an important method to make the diagnosis and differential diagnosis.
In this case, the patient’s left-side waist pain remained intense after conservative treatment. Taking into consideration the huge size of the tumor and the patient’s general condition, there was a great risk of continuing the pregnancy, and she chose to terminate the pregnancy and underwent left nephrectomy.
Rupture and hemorrhage of RAML during pregnancy is compared with a “bomb explosion,” which is life-threatening. Ultrasound has many advantages, such as rapid diagnosis and no radiation. Although ultrasound examination lacks specificity, it can lead to a preliminary disease diagnosis, facilitating a relevant differential diagnosis to reduce misdiagnosis, which can prompt further treatment. Therefore, ultrasound examination played an important role in the diagnosis of the condition during pregnancy. Depending on the patient’s condition, treatment should be individualized.
Manuscript source: Unsolicited manuscript
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aoki H S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Xing YX
| 1. | Stone CH, Lee MW, Amin MB, Yaziji H, Gown AM, Ro JY, Têtu B, Paraf F, Zarbo RJ. Renal angiomyolipoma: further immunophenotypic characterization of an expanding morphologic spectrum. Arch Pathol Lab Med. 2001;125:751-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Wang C, Li X, Peng L, Gou X, Fan J. An update on recent developments in rupture of renal angiomyolipoma. Medicine (Baltimore). 2018;97:e0497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Gimeno Argente V, Bosquet Sanz M, Bonillo García MA, Gómez Pérez L, Pontones Moreno JL, Jiménez Cruz JF. [Conservative surgery of bilateral renal angiomyolipoma during pregnancy]. Actas Urol Esp. 2006;30:633-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Prischl FC, Spöttl P. Spontaneous rupture of angiomyolipoma of the kidney. Wien Klin Wochenschr. 2017;129:217-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Bora A, Soni A, Sainani N, Patkar D. Emergency embolization of a bleeding renal angiomyolipoma using polyvinyl alcohol particles. Diagn Interv Radiol. 2007;13:213-216. [PubMed] |
| 6. | Nelson CP, Sanda MG. Contemporary diagnosis and management of renal angiomyolipoma. J Urol. 2002;168:1315-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 261] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 7. | Çetin C, Büyükkurt S, Demir C, Evrüke C. Renal angiomyolipoma during pregnancy: Case report and literature review. Turk J Obstet Gynecol. 2015;12:118-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Morales JP, Georganas M, Khan MS, Dasgupta P, Reidy JF. Embolization of a bleeding renal angiomyolipoma in pregnancy: case report and review. Cardiovasc Intervent Radiol. 2005;28:265-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Halpenny D, Snow A, McNeill G, Torreggiani WC. The radiological diagnosis and treatment of renal angiomyolipoma-current status. Clin Radiol. 2010;65:99-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 129] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 10. | Catalano O, Cusati B, Nunziata A, Siani A. Active abdominal bleeding: contrast-enhanced sonography. Abdom Imaging. 2006;31:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | dos Santos MM, Proença SM, Reis MI, Viana RM, Martins LM, Colaço JM, Nunes FM. Spontaneous rupture of renal angiomyolipoma during pregnancy. Rev Bras Ginecol Obstet. 2014;36:377-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Wright T, Sooriakumaran P. Renal angiomyolipoma presenting with massive retroperitoneal haemorrhage due to deranged clotting factors: a case report. Cases J. 2008;1:213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Storm DW, Mowad JJ. Conservative management of a bleeding renal angiomyolipoma in pregnancy. Obstet Gynecol. 2006;107:490-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Gyimadu AO, Kara O, Basaran D, Esinler I. Conservative management of a retroperitoneal hemorrhage following a ruptured renal angiomyolipoma in pregnancy. J Obstet Gynaecol Res. 2011;37:156-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Kira S, Sawada N, Miyamoto T, Mitsui T, Zakoji H, Takeda M. Hemorrhagic Renal Angiomyolipoma in Pregnancy Effectively Managed by Immediate Cesarean Section and Elective Transcatheter Arterial Embolization: A Case Report. J Endourol Case Rep. 2016;2:65-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Preece P, Mees B, Norris B, Christie M, Wagner T, Dundee P. Surgical management of haemorrhaging renal angiomyolipoma in pregnancy. Int J Surg Case Rep. 2015;7C:89-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |