Published online Sep 6, 2020. doi: 10.12998/wjcc.v8.i17.3835
Peer-review started: May 2, 2020
First decision: May 21, 2020
Revised: July 16, 2020
Accepted: July 30, 2020
Article in press: July 30, 2020
Published online: September 6, 2020
Processing time: 124 Days and 19.4 Hours
Active bleeding due to arterial injury following the acupuncture can sometimes represent a life-threatening complication. Only few reports of an actively bleeding hematoma diagnosed by contrast-enhanced ultrasound, which enables the depiction of vascular, have been reported.
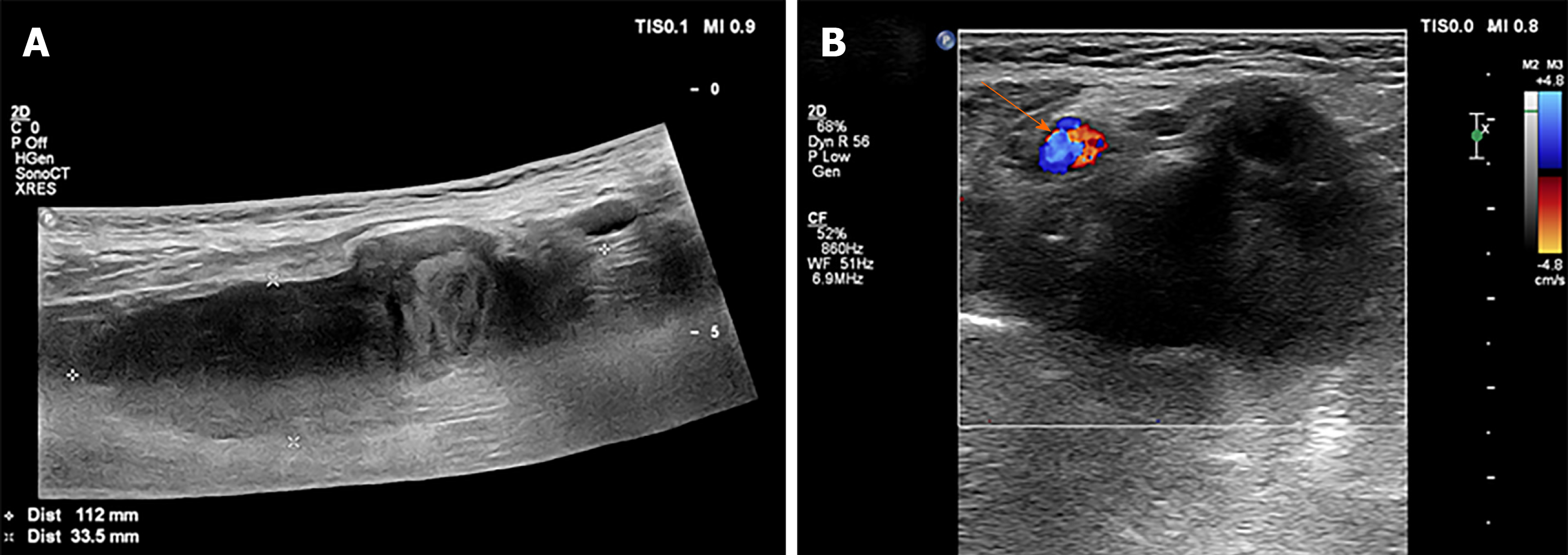
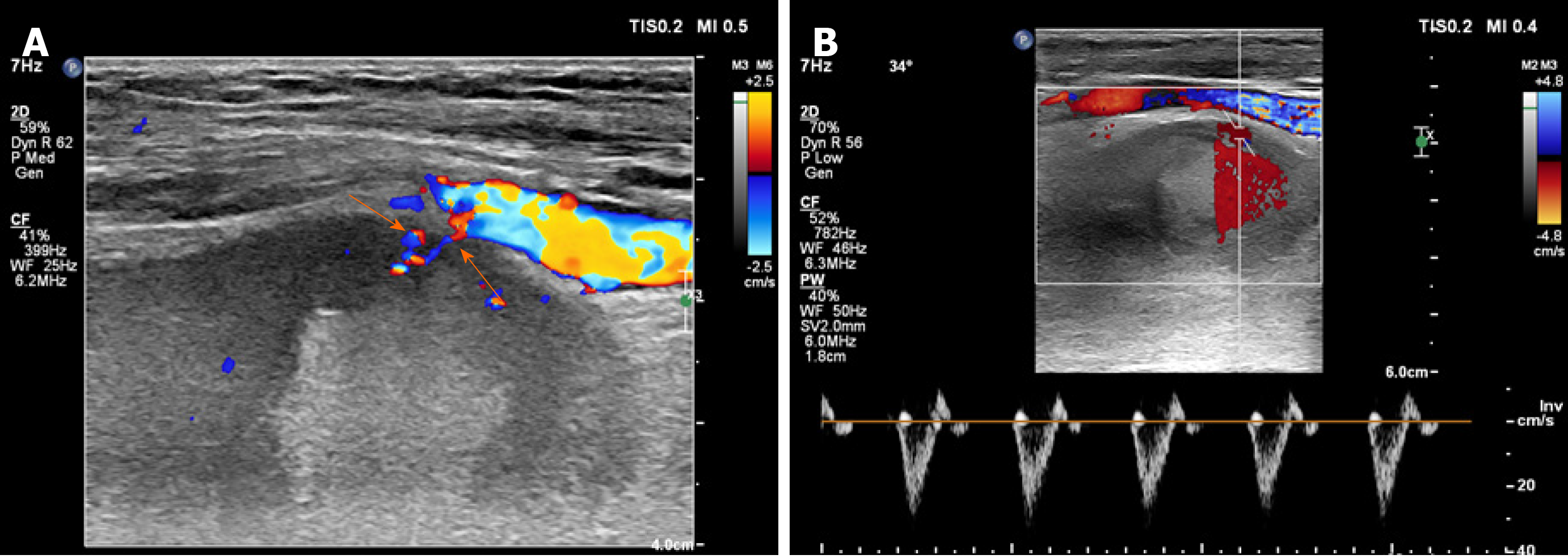
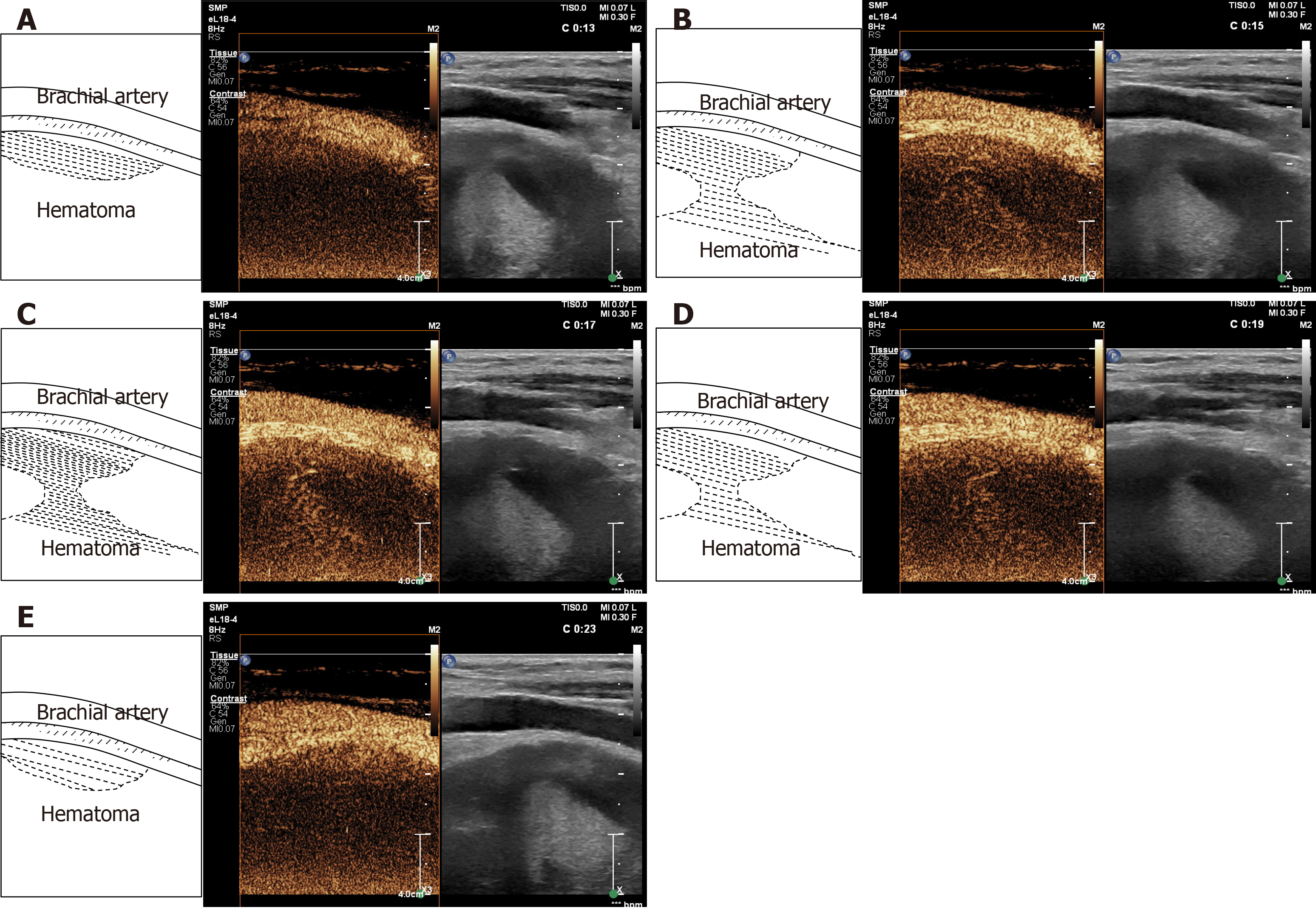
Here, we report the case of a 75-year-old woman, who presented with sudden swelling, ecchymosis, and pain in the upper left limb. She underwent an acupuncture treatment of traditional Chinese medicine followed by a deep shoulder massage 2 d before admission to hospital. A few hours after the massage, her left upper arm was red, swollen and progressively aggravated. Ultrasonography showed a large hematoma (11.2 cm × 3.5 cm × 3.4 cm) beside the left brachial artery. Color Doppler ultrasound revealed that blood flow signals of the arteries branched into the hematoma. The contrast-enhanced ultrasound showed microbubbles from the brachial artery passing into the hematoma, diffused within the hematoma with the local surge of red blood cells, and disappearing after approximately 17 s. The microbubbles were likely due to bleeding from the arteries. After pressure bandaging treatment, the hematoma became smaller (3.1 cm × 1.7 cm) and organized according to ultrasonography performed 20 d later.
This case highlights the ultimate importance of contrast-enhanced ultrasound for the diagnosis of an actively bleeding hematoma.
Core tip: Active bleeding due to arterial injury following acupuncture can sometimes represent a life-threatening complication. We present herein, a rare case of actively bleeding brachial artery hematoma diagnosed by contrast-enhanced ultrasound (CEUS). CEUS enables the depiction of microvascularization, and has the potential to replace computed tomography in assessments for active bleeding. This case highlights the ultimate importance of CEUS for the diagnosis of an actively bleeding hematoma.
- Citation: Ma JJ, Zhang B. Diagnosis of an actively bleeding brachial artery hematoma by contrast-enhanced ultrasound: A case report. World J Clin Cases 2020; 8(17): 3835-3840
- URL: https://www.wjgnet.com/2307-8960/full/v8/i17/3835.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i17.3835
Acupuncture, which involves inserting needles into different parts or points of the body, has been increasingly used as an integrative or complementary therapy for pain[1]. Complications are infrequent and usually resolve with minimal or no intervention, but major adverse events can occur[2,3]. In particular, active bleeding due to arterial injury during the vascular access can sometimes represent a life-threatening complication needing prompt surgical or endovascular embolization therapy. Imaging is necessary to confirm the diagnosis[4].
Ultrasonography is the imaging modality of choice, since it can provide detailed information about vascular anatomy without incurring the risks of invasive methods such as angiography or radiation[5]. However, it is difficult for gray-scale ultrasound to detect whether the bleeding is still ongoing. Color Doppler ultrasound can help to detect active bleeding, but may fail when the blood flow velocity is low. Contrast-enhanced ultrasound (CEUS) enables the depiction of microvascularization and has the potential to replace contrast-enhanced computed tomography (CT) in assessments for active bleeding. Moreover, it reportedly detects perfusion changes and active extravasation, and internal bleeding can be seen as a pooling of contrast medium within the hematoma. CEUS is increasingly being used when active bleeding is suspected.
We report a case in which CEUS played a key role in the rapid detection of active bleeding from the left brachial artery following acupuncture and massage.
A 75-year-old woman presented to the outpatient surgery clinic with sudden swelling, ecchymosis, and pain in the left upper limb.
She went to a small traditional Chinese medicine clinic for acupuncture treatment for shoulder discomfort 2 d previous to hospital admission. Her grandson had then given her a deep shoulder massage after the acupuncture treatment. A few hours later, the upper left arm was red and swollen, progressively aggravated.
The patient had a free medical history.
The patient’s temperature was 36.4 °C, heart rate was 85 bpm, respiratory rate was 15 breaths per minute, and blood pressure was 125/80 mmHg. The physical examination revealed swelling, ecchymosis, and pain in the left upper limb, without any other pathological signs. Our clinical consideration was first a hematoma.
The hemoglobin value was slightly decreased at 10.9 g/dL. The blood biochemistries, prothrombin, partial thromboplastin times, d-dimers, as well as urine analysis were normal.
Ultrasonography showed a large hematoma (11.2 cm × 3.5 cm × 3.4 cm) beside the brachial artery (Figure 1). The color Doppler ultrasound revealed that the blood flow signals of the arteries branched into the hematoma (Figure 2). Low mechanical index CEUS, with a bolus of 2.4 mL SonoVue, showed the accumulation of microbubbles within the hematoma, first detectable at 13 s. Microbubbles were seen emerging from the brachial artery and diffusing into the hematoma with the local surge of red blood cells, and they disappeared after approximately 23 s. The microbubbles were likely due to bleeding from the arteries (Figure 3).
The final diagnosis of the presented case is an actively bleeding brachial artery hematoma.
The patient immediately underwent pressure-bandage treatment in the clinic.
The pain was controlled after pressure-bandage treatment. After 20 d, the hematoma became smaller (3.1 cm × 1.7 cm) and organized according to ultrasonography (Figure 4).
Acupuncture is a safe and commonly applied therapy in China, but rupture of the arteries may be a complication of the technique[6]. Pseudoaneurysm is formed when there is a break in the vessel wall, so the extravasation of blood dissects the surrounding tissues, and an aneurysm sac, which retains a communication with the parent arterial lumen, is created. Then the pseudoaneurysm wall is formed by organizing hematoma and fibrous tissue. Under the influence of high arterial pressure the sac usually tends to enlarge, with a sustained risk of its rupture and hemorrhage[5]. Pressure bandaging is the main treatment for this adverse event, and deep massage should be forbidden. In this case, the hematoma might have been caused by an acupuncture needle puncturing the left brachial artery, and the intense massage aggravated the contusion of the artery.
The management of hematoma depends on the accurate diagnosis of any ongoing bleeding and identification of the type of injured vessel. Although most cases can be managed conservatively, patients with active bleeding should be monitored, and those with hemodynamic instability or ongoing blood loss might require embolization or surgical intervention[7].
CT and magnetic resonance imaging may be useful to see associated intracranial trauma, if there is a history trauma, but are not suggested for first-line imaging in sub-acute/chronic setting. The definitive diagnosis can be made with angiography, but, as this is an invasive test it is should be reserved for those to be treated directly[8]. The hematoma is easily found with gray-scale ultrasound, and its size, location, echo-structure, and relationship with the surrounding tissue can be identified[9]; most hemodynamic characteristics of tissues are better displayed by color Doppler[10,11]. However, it is often difficult to detect deep, limited location, or low-velocity blood flow because of the limitation of gray-scale and Doppler technology, thus affecting the accuracy of ultrasonic diagnosis[12]. However, CEUS can play an important role in accurately determining the bleeding activity, by showing the blood flow distribution and providing more complete information, further improving the accuracy of ultrasonic diagnosis[13,14]. A new study showed the use of a gel stand-off pad allows the detection of otherwise-missed peri- or intra-lesional flow signals on Doppler imaging, increasing the diagnostic role of this technique in differential diagnosis of superficial lesions[15]. The use of a gel stand-off pad might make less microbubbles blasting on CEUS imaging.
In this case, CEUS was used rapidly diagnose ongoing bleeding at the bedside. In addition, the time recording feature allowed the determination of an artery bleed, which correlated with the color Doppler findings. CEUS is a promising diagnostic alternative, particularly for patients for whom CT is either contraindicated or less desirable, and warrants further investigation[16,17].
Only scarce reports of an actively bleeding hematoma diagnosed by CEUS has been reported. CEUS enabled the depiction of vascular. This case highlights the ultimate importance of CEUS for the diagnosis of an actively bleeding hematoma.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Thyroid Cancer Expert Committee of Chinese Society of Clinical Oncology, Vice Chairman; Guiding Expert of Ultrasonic Medicine Committee of Beijing Women Doctors' Association, Vice Chairman; Ultrasound Group of Superficial Organs and Peripheral Blood Vessels of the Ninth Committee of Ultrasonic Medicine Branch of Beijing Medical Association of Chinese Medical Association, Member; Deputy Director of the First Thyroid Professional Committee of Beijing Anti-Cancer Association, Member; The Second Superficial Ultrasound Professional Committee of Chinese Physicians Association, Vice Chairman; The First Committee of the Medical Science Popularization Branch of the Chinese Physicians Association, the Professional Committee of Popular Science of Thyroid Diseases (Group), Member; Thyroid Professional Committee of Beijing Non-Public Medical Institutions Association, Vice Chairman; Clinical Practical Technology Branch of China Association for the Promotion of International Communication of Health Care, Member; Executive member of Ultrasonic Professional Committee of China Medical Image Quality Research Association; Standing member of the Fourth Professional Committee of Imaging Medicine of Beijing Society of Integrated traditional Chinese and Western Medicine; Professional Committee on Thyroid Diseases of China Research Hospital Association; The Standing Committee of Medical Image Quality Research Committee of China Medical Quality Management Association, Member.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A, Giorgio A, Isik A, Sartori S S-Editor: Zhang L L-Editor: Filipodia P-Editor: Xing YX
| 1. | Kelly RB, Willis J. Acupuncture for Pain. Am Fam Physician. 2019;100:89-96. |
| 2. | Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, Irnich D, Witt CM, Linde K; Acupuncture Trialists' Collaboration. Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis. J Pain. 2018;19:455-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 474] [Article Influence: 59.3] [Reference Citation Analysis (1)] |
| 3. | Zhuang Y, Xing JJ, Li J, Zeng BY, Liang FR. History of acupuncture research. Int Rev Neurobiol. 2013;111:1-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 130] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Tombesi P, Di Vece F, Ermili F, Sartori S. Active bleeding revealed by contrast-enhanced ultrasonography: beyond the abdominal cavity. J Med Ultrason (2001). 2014;41:247-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Corvino A, Catalano O, Corvino F, Sandomenico F, Setola SV, Petrillo A. Superficial temporal artery pseudoaneurysm: what is the role of ultrasound? J Ultrasound. 2016;19:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Li NC, Li MY, Chen B, Guo Y. A New Perspective of Acupuncture: The Interaction among Three Networks Leads to Neutralization. Evid Based Complement Alternat Med. 2019;2019:2326867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Salemis NS, Gourgiotis S, Karalis G. Diagnostic evaluation and management of patients with rectus sheath hematoma. A retrospective study. Int J Surg. 2010;8:290-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Walker MT, Liu BP, Salehi SA, Badve S, Batjer HH. Superficial temporal artery pseudoaneurysm: diagnosis and preoperative planning with CT angiography. AJNR Am J Neuroradiol. 2003;24:147-150. [PubMed] |
| 9. | Di Vece F, Tombesi P, Bianchi L, Bertini M, Sartori S. Contrast-enhanced ultrasonography of post-interventional hematoma: the bleeding mushroom is growing inside. J Med Ultrason (2001). 2018;45:661-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Giovagnorio F, Andreoli C, De Cicco ML. Color Doppler sonography of focal lesions of the skin and subcutaneous tissue. J Ultrasound Med. 1999;18:89-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Catalano O, Roldán FA, Varelli C, Bard R, Corvino A, Wortsman X. Skin cancer: findings and role of high-resolution ultrasound. J Ultrasound. 2019;22:423-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 12. | Isik A, Karavas E, Firat D. Spontaneous milk fistula from an axillary accessory breast. Breast J. 2019;25:154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Corvino A, Sandomenico F, Setola SV, Corvino F, Pinto F, Catalano O. Added value of contrast-enhanced ultrasound (CEUS) with Sonovue® in the diagnosis of inferior epigastric artery pseudoaneurysm: report of a case and review of literature. J Ultrasound. 2019;22:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Corvino A, Pignata S, Campanino MR, Corvino F, Giurazza F, Tafuri D, Pinto F, Catalano O. Thyroglossal duct cysts and site-specific differential diagnoses: imaging findings with emphasis on ultrasound assessment. J Ultrasound. 2020;23:139-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Corvino A, Sandomenico F, Corvino F, Campanino MR, Verde F, Giurazza F, Tafuri D, Catalano O. Utility of a gel stand-off pad in the detection of Doppler signal on focal nodular lesions of the skin. J Ultrasound. 2020;23:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 16. | Guo Q, Zhao J, Huang B, Yuan D, Yang Y, Zeng G, Xiong F, Du X. A Systematic Review of Ultrasound or Magnetic Resonance Imaging Compared With Computed Tomography for Endoleak Detection and Aneurysm Diameter Measurement After Endovascular Aneurysm Repair. J Endovasc Ther. 2016;23:936-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 17. | Tombesi P, Di Vece F, Salviato E, Galeotti R, Sartori S. Spontaneous active bleeding in thoracoacromial artery diagnoses by contrast-enhanced ultrasound - a case report. Ultraschall Med. 2012;33:E355-E356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |