Published online Sep 6, 2020. doi: 10.12998/wjcc.v8.i17.3808
Peer-review started: May 26, 2020
First decision: July 25, 2020
Revised: August 1, 2020
Accepted: August 20, 2020
Article in press: August 20, 2020
Published online: September 6, 2020
Processing time: 100 Days and 20.5 Hours
Heterotopic gastrointestinal cysts have gastrointestinal epithelium in the cyst wall and rarely occur in the oral cavity. Most are found in the neonatal period. However, heterotopic gastrointestinal cysts that are diagnosed as a congenital tongue cyst by routine ultrasonography are extremely rare.
A 12-day-old female presented with swelling of the anterior tongue. The obstetrician had detected significant tongue swelling on fetal ultrasonography in the 35th gestational week. The female was born by cesarean delivery at gestational week 39. She soon became dyspneic, and the cyst was aspirated. After the aspiration, her breathing recovered and she started breastfeeding. The cyst was excised under general anesthesia on the 67th day. Histopathologic examination showed that that cyst wall consisted of a lining of columnar gastrointestinal-type epithelium and pseudostratified ciliated epithelium. The patient restarted breastfeeding 3 h after surgery. The postoperative course was uneventful.
Airway distress and feeding difficulty were successfully avoided by cyst aspiration, and surgical resection was performed with no perioperative complications.
Core tip: Heterotopic gastrointestinal cysts have gastrointestinal epithelium in the cyst wall and rarely occur in the oral cavity. When these cysts do occur in the oral cavity, most are found in the neonatal period. However, heterotopic gastrointestinal cysts that are diagnosed as a congenital tongue cyst by routine ultrasonography are extremely rare. In such cases, airway management immediately after delivery is particularly important, and intratracheal intubation or reduction procedures may be required. We successfully avoided airway distress and feeding difficulty by performing cyst aspiration. Cyst aspiration may improve the outcome in such rare cases.
- Citation: Lee AD, Harada K, Tanaka S, Yokota Y, Mima T, Enomoto A, Kogo M. Large lingual heterotopic gastrointestinal cyst in a newborn: A case report. World J Clin Cases 2020; 8(17): 3808-3813
- URL: https://www.wjgnet.com/2307-8960/full/v8/i17/3808.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i17.3808
Heterotopic gastrointestinal cysts have gastrointestinal epithelium in the cyst wall and rarely occur in the oral cavity[1]. When heterotopic gastrointestinal cysts do occur in the oral cavity, they frequently occur in the anterior part of the tongue and are mainly found in the neonatal period; however, some cases become asymptomatic in adulthood[2,3]. The diagnosis of a heterotopic gastrointestinal cyst as a congenital tongue cyst by routine ultrasonography is extremely rare[4-10]. Congenital tongue cysts can cause respiratory distress and require multidisciplinary treatment for airway management. Intratracheal intubation and reduction procedures may be required immediately after delivery[5-7,9]. The treatment is complete surgical resection, and there are very few cases of recurrence[2]. However, there is no consensus on the optimal timing of surgery and the effectiveness of preoperative cyst reduction procedures. Herein, we report a rare case of a congenital heterotopic gastrointestinal cyst of the tongue. Cyst aspiration successfully avoided airway distress and feeding difficulty.
A 12-day-old female was referred to our hospital for tongue swelling.
The obstetrician had detected significant swelling of the tongue on fetal ultrasonography performed in the 35th gestational week. Because of the anticipated high risk of breathing difficulty, the female was born by cesarean delivery at gestational week 39 in the presence of a pediatric surgeon.
The medical and obstetric history of the mother was unremarkable, with no family history of any congenital anomalies. The patient had no other congenital anomalies.
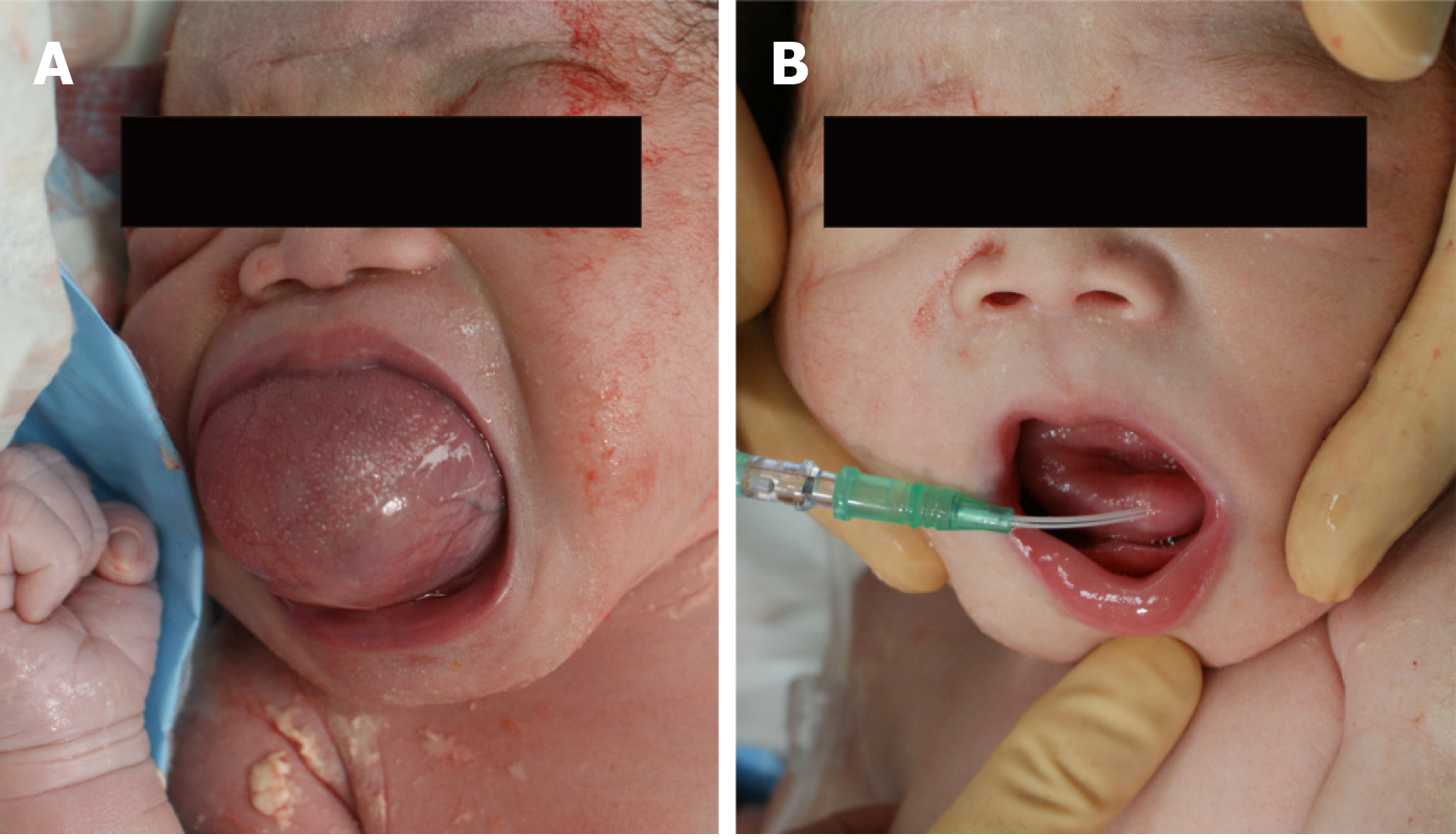
The cystic legion was located hypoglossally and measured 15 mm × 25 mm. The cyst elevated the tongue and occupied the oral cavity, preventing the mouth from closing (Figure 1A). She became dyspneic soon after delivery, and so the pediatric surgeon aspirated the cyst (Figure 1B).
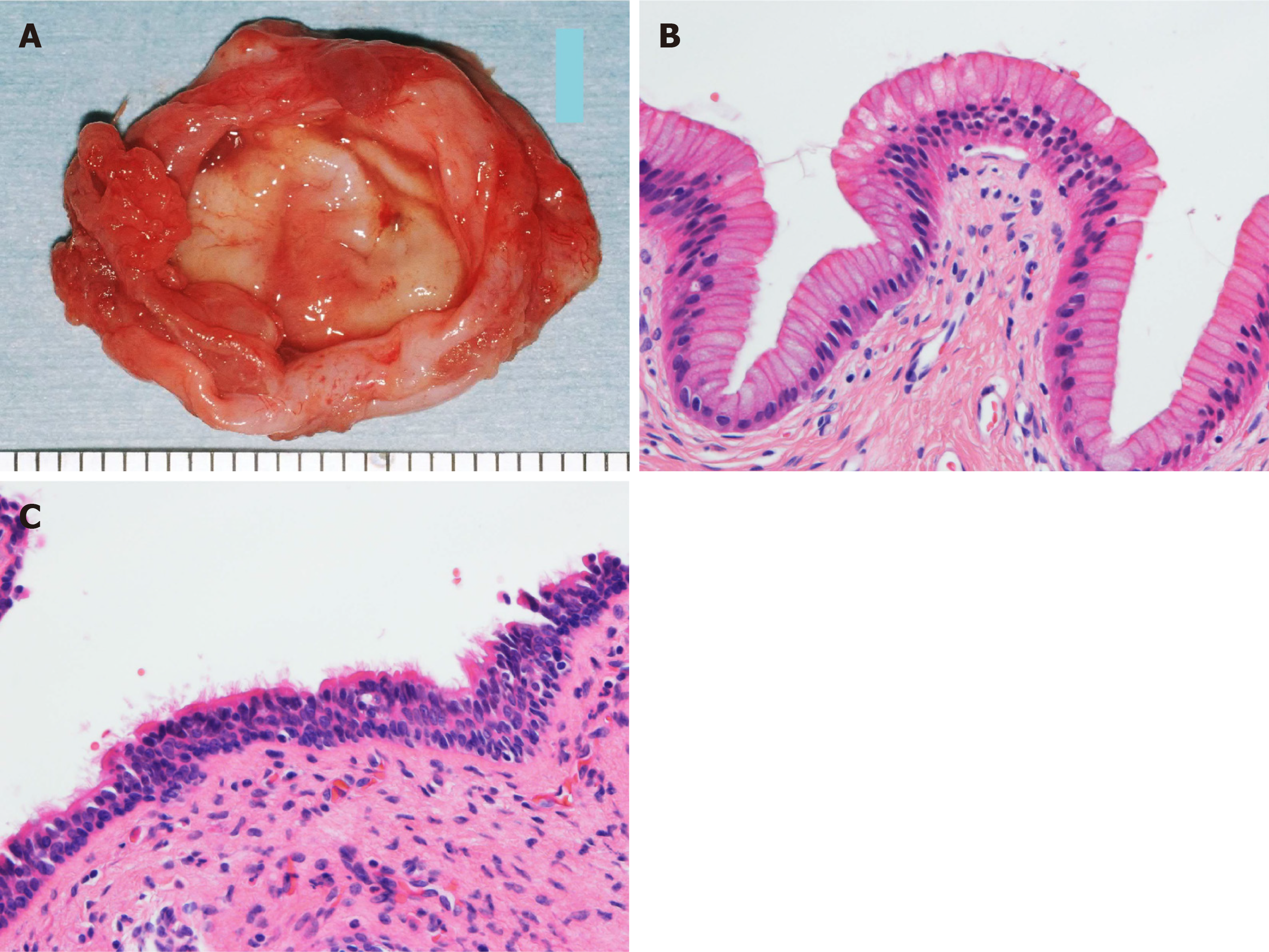
Histopathologic examination showed that the specimen was a true cyst, and that its wall consisted of a lining of columnar gastrointestinal-type epithelium and pseudostratified ciliated epithelium (Figure 2).
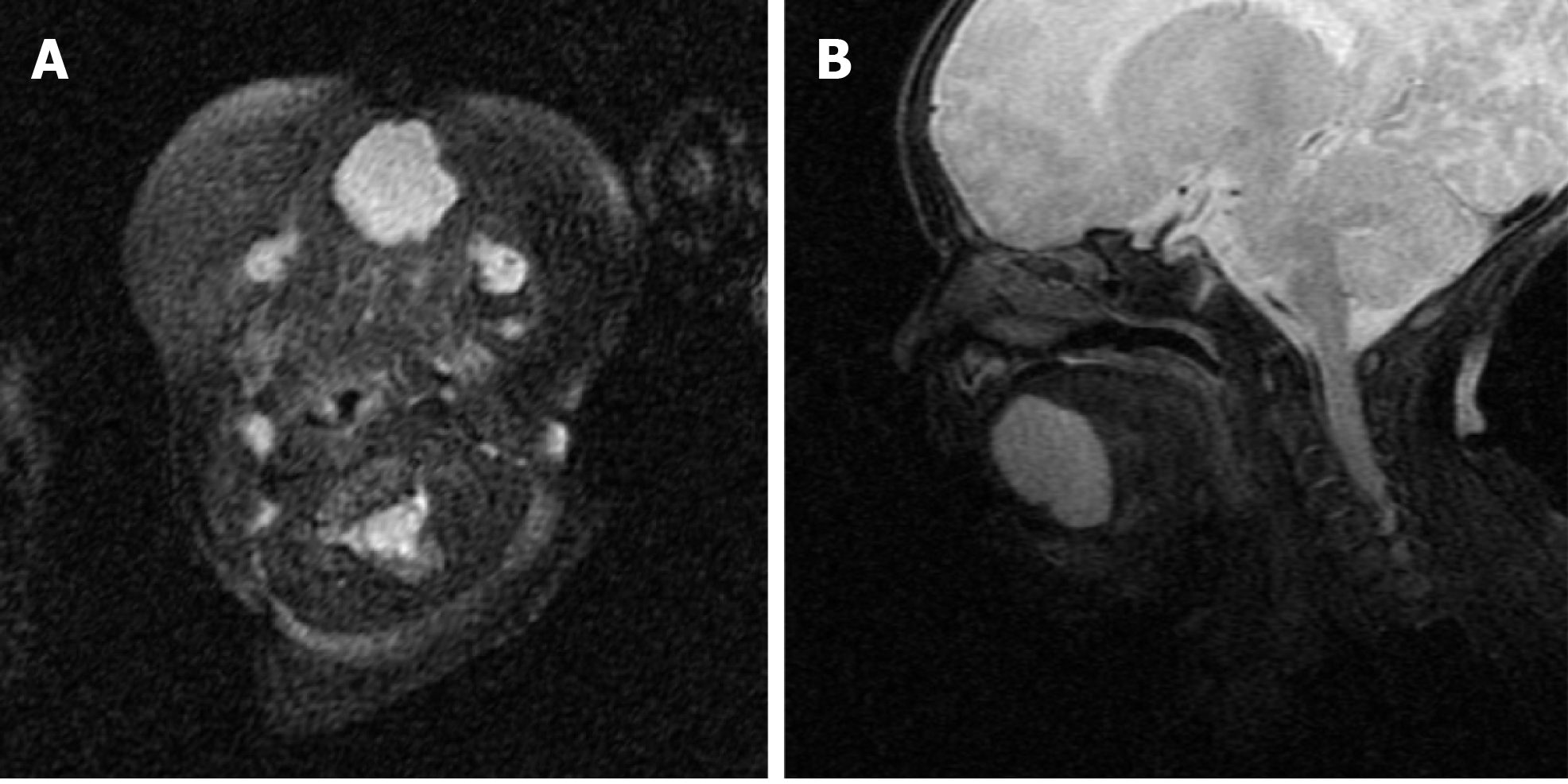
Magnetic resonance imaging (MRI) performed on the 24th day showed that the 25 mm circular-shaped cyst was located hypoglossally without expansion in the oral floor (Figure 3).
The final diagnosis was a heterotopic gastrointestinal cyst of the tongue.
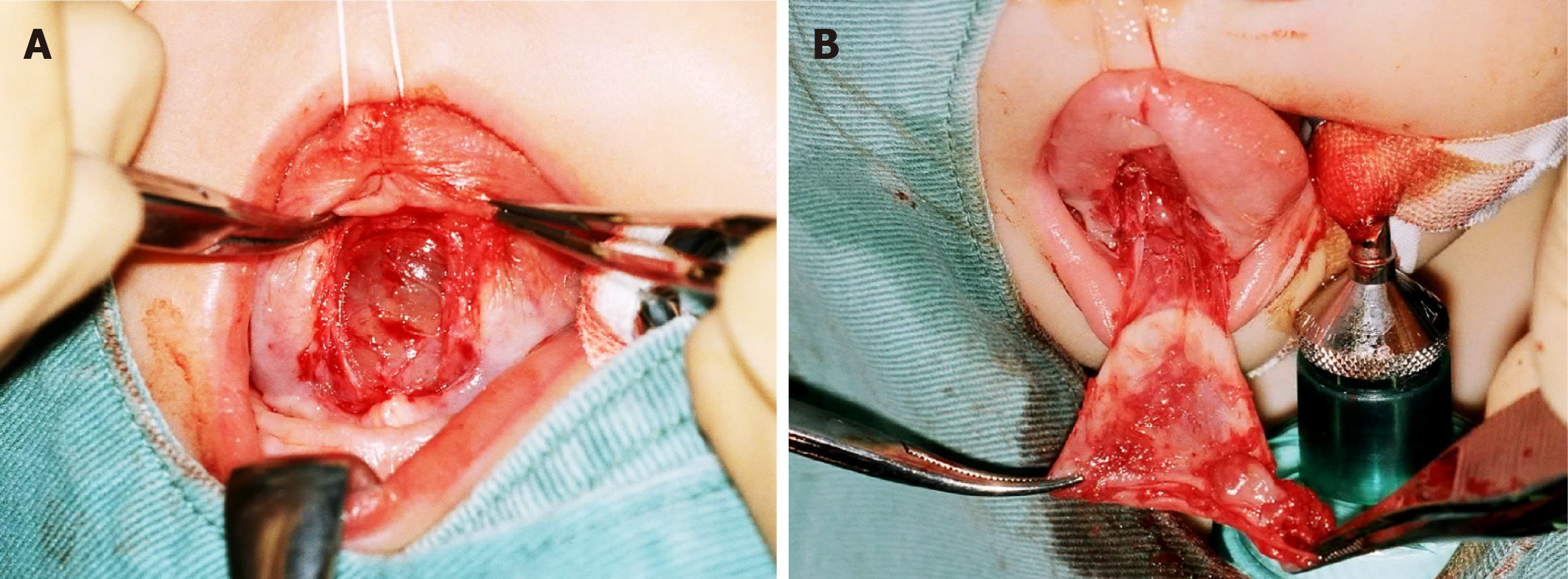
To avoid the repetition of aspiration, immediate surgical resection was recommended. However, the mother of the patient did not want her to undergo surgery in the neonatal period. Thus, a second aspiration was performed on the 7th day. However, the cyst was found to be gradually increasing in size, the excision procedure was performed with the patient under general anesthesia on the 67th day. The tongue was pulled forward and an incision was made on the anterior midline under the tongue. The submucosal tissue was bluntly dissected until the cyst wall was observed (Figure 4A). The cyst was excised by dissecting the connective tissue (Figure 4B). The cyst contained viscous dark brown fluid. The wound was sutured with absorbable thread.
The patient was able to breastfeed 3 h after surgery. The postoperative course was uneventful, and there has been no recurrence during 5 years of follow-up.
The reported congenital cystic lesions of the tongue include a ranula[11], teratoma[12], thyroglossal duct cyst[13], lymphangioma[14], and heterotopic gastrointestinal cyst. However, heterotopic gastrointestinal cyst of the tongue is rare[1]. Although this type of cyst is most commonly referred to as a heterotopic gastrointestinal cyst, it is also known by various terms such as a foregut duplication cyst, choristomatic cyst, ciliated epithelial cyst, lingual duplication cyst, cystic tumor of the tongue, unusual thyroglossal duct cyst, heterotopic large bowel cyst, enterocystoma, and alimentary tract cyst[1,3]. It is rare to see heterotopic gastrointestinal epithelium in the oral region, while it is more commonly reported in the duodenum, gallbladder, common bile duct, jejunum, Merkel diverticulum, ileum, appendix, colon, and rectum[15]. The wall of a heterotopic gastrointestinal cyst may consist of a lining of ciliated epithelium and squamous epithelium in addition to gastrointestinal epithelium[3]. The pathogenesis of a heterotopic gastrointestinal cyst is still unknown, but the cyst may arise from undifferentiated ectoderm lining of the primitive stomodeum that becomes entrapped within the oral cavity during the 4th week of fetal development[16]. Most heterotopic gastrointestinal cysts are discovered by 2 years of age[3]. The treatment is surgical resection. Possible surgical complications are Wharton's duct injury and lingual muscle injury. Preoperative MRI is helpful to show the expansion to adjacent structures and the localization of the cyst. Recurrence is rare with complete resection[1].
Cases in which a heterotopic gastrointestinal cyst is detected in the prenatal period are extremely rare. To the best of our knowledge, there are only nine cases in which a lingual heterotopic gastrointestinal cyst has been diagnosed prenatally (Table 1)[4-10]. In all of these cases, a lingual cyst was detected with ultrasonography. Large cysts on the tongue may cause airway obstruction. Therefore, prenatal ultrasonographic diagnosis is essential to predict the risk of upper airway obstruction at delivery. Multidisciplinary collaboration is also essential to formulate a careful delivery plan that ensures airway protection in the neonate[7]. Prenatal MRI is a useful way to evaluate the risk of airway obstruction[7-10]. If an airway problem is detected with echo, an ex-utero intrapartum treatment procedure may provide time to open the infant’s airway while maintaining the placental blood supply[8].
| Case | Ref. | Preoperative cyst size | Preoperative intratracheal intubation | Preoperative reduction procedure | Age at the time of surgery |
| 1 | Chen et al[6] (1997) | 50 mm × 40 mm × 30 mm | Performed | Aspiration | 0 d |
| 2 | Chen et al[6] (1997) | 25 mm × 20 mm × 15 mm | Performed | Aspiration and marsupialization | 9 mo |
| 3 | Rousseau et al[9] (2004) | 4 cm diameter | Not performed | Aspiration | 13 d |
| 4 | Hall et al[8] (2005) | 21 mm × 28 mm × 25 mm | Not performed | None | 13 d |
| 5 | Karam et al[4] (2007) | 12 mm × 16 mm | Not performed | None | 3 d |
| 6 | Hambarde et al[5] (2011) | 40 mm × 40 mm × 22 mm | Not performed | Marsupialization | 2.5 mo |
| 7 | Houshmand et al[10] (2011) | 32 mm × 26 mm × 28 mm | Not performed | None | 6 d |
| 8 | Houshmand et al[10] (2011) | 33 mm × 23 mm × 20 mm | Not performed | None | 2 mo |
| 9 | Gantwerker et al[7] (2014) | 37 mm × 23 mm × 16 mm | Performed | None | 6 d |
| 10 | Present case | 15 mm × 25 mm | Not performed | Aspiration | 67 d |
In previous reports of lingual heterotopic gastrointestinal cysts, intubation was required for airway management in three of nine cases[6,7]. The remaining seven patients were not intubated, as ultrasonographic imaging showed that there were no airway problems[4,5,8-10]. Preoperative aspiration or marsupialization was performed in four cases, while aspiration alone was performed in two cases[5,6,9]. All aspiration procedures were performed at birth. Our case was the only case in which aspiration was performed twice. The timing of cystectomy was within 2 wk in six cases[4,6-10]. Around two months in three cases (including the present case)[5,10], and at nine months in one case[6]. In all cases, there were no problems with the postoperative respiratory and nutritional statuses. Although previous reports did not describe the preoperative feeding status and intubation at the time of general anesthesia induction, the infant in our case was able to breastfeed just before the surgery, and oral intubation was easy despite the remaining swelling of the tongue.
In our case, immediate cyst aspiration was performed at birth, and the respiratory condition and feeding function were stable; therefore, surgery was postponed. There is no consensus on the optimal timing of surgical removal of congenital tongue cysts, including heterotopic gastrointestinal cysts. Kaneko et al[11] suggested that surgical resection of a congenital mucous cyst of the tongue is safely performed at 1 year of age, although the timing of surgery depends on the degree of breathing and feeding impairments, and the child’s development. However, all reported cases of prenatally diagnosed heterotopic gastrointestinal cysts, including our case, involved cyst excision within 1 year and had a good outcome[4-10]. Thus, aspiration is effective for initial airway and feeding management, but frequent aspiration should be avoided because of the risk of infection and adjacent tissue damage. If the cyst grows and repeated aspiration is difficult, it may be better to perform excision at that time.
We described the surgical treatment of a lingual heterotopic gastrointestinal cyst in a newborn. Airway distress and feeding difficulty were successfully avoided by cyst aspiration, and surgical resection was performed on the 67th day with no perioperative complications.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pota V S-Editor: Yan JP L-Editor: A P-Editor: Xing YX
| 1. | Lui B, Korman B. Congenital oral heterotopic gastrointestinal cyst: case report and review of the literature. J Otolaryngol Head Neck Surg. 2008;37:E151-E154. [PubMed] |
| 2. | Manor Y, Buchner A, Peleg M, Taicher S. Lingual cyst with respiratory epithelium: an entity of debatable histogenesis. J Oral Maxillofac Surg. 1999;57:124-7; discussion 128-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Said-Al-Naief N, Fantasia JE, Sciubba JJ, Ruggiero S, Sachs S. Heterotopic oral gastrointestinal cyst: report of 2 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:80-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Karam O, Pfister RE, Extermann P, La Scala GC. Congenital lingual cysts. J Pediatr Surg. 2007;42:E25-E27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 5. | Hambarde S, Bendre P, Taide D. Foregut duplication cyst presenting as lingual swelling: Case report and review of literature. Natl J Maxillofac Surg. 2011;2:2-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Chen MK, Gross E, Lobe TE. Perinatal management of enteric duplication cysts of the tongue. Am J Perinatol. 1997;14:161-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 7. | Gantwerker EA, Hughes AL, Silvera VM, Vargas SO, Rahbar R. Management of a large antenatally recognized foregut duplication cyst of the tongue causing respiratory distress at birth. JAMA Otolaryngol Head Neck Surg. 2014;140:1065-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Hall NJ, Ade-Ajayi N, Peebles D, Pierro A. Antenatally diagnosed duplication cyst of the tongue: modern imaging modalities assist perinatal management. Pediatr Surg Int. 2005;21:289-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Rousseau T, Couvreur S, Senet-Lacombe E, Durand C, Justrabo E, Malka G, Sagot P. Prenatal diagnosis of enteric duplication cyst of the tongue. Prenat Diagn. 2004;24:98-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Houshmand G, Hosseinzadeh K, Ozolek J. Prenatal magnetic resonance imaging (MRI) findings of a foregut duplication cyst of the tongue: value of real-time MRI evaluation of the fetal swallowing mechanism. J Ultrasound Med. 2011;30:843-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Kaneko T, Horie N, Shimoyama T. Congenital mucocele in the tongue: report of a case. J Oral Maxillofac Surg. 2012;70:2596-2599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Kulkarni K, Mane S, Rumane N, Saran S, Desai P. A rare case of giant tongue teratoma: Anesthetic management in low resource settings. Paediatr Anaesth. 2017;27:1168-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Lindstrom DR, Conley SF, Arvedson JC, Beecher RB, Carr MH. Anterior lingual thyroglossal cyst: antenatal diagnosis, management, and long-term outcome. Int J Pediatr Otorhinolaryngol. 2003;67:1031-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Paladini D, Morra T, Guida F, Lamberti A, Martinelli P. Prenatal diagnosis and perinatal management of a lingual lymphangioma. Ultrasound Obstet Gynecol. 1998;11:141-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Martone CH, Wolf SM, Wesley RK. Heterotopic gastrointestinal cyst of the oral cavity. J Oral Maxillofac Surg. 1992;50:1340-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Daley TD, Wysocki GP, Lovas GL, Smout MS. Heterotopic gastric cyst of the oral cavity. Head Neck Surg. 1984;7:168-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 1.0] [Reference Citation Analysis (0)] |