Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3578
Peer-review started: March 9, 2020
First decision: June 18, 2020
Revised: June 26, 2020
Accepted: July 15, 2020
Article in press: July 15, 2020
Published online: August 26, 2020
Processing time: 169 Days and 5.4 Hours
Acute generalized exanthematous pustulosis (AGEP) is a severe cutaneous adverse reaction characterized by sterile pustules on erythematous skin associated with fever and leukocytosis. The annual incidence of AGEP is estimated to be 1-5 cases per million. Cases of AGEP with oral mucosa involvement have been reported. However, reports of AGEP involving airway mucosa are limited.
We report a 42-year-old woman with serious AGEP involving the airway mucosa. The patient initially developed fever and a small rash on her forehead and face. Over the next 2 d, she developed a diffuse, pustular rash over her trunk and legs. In addition, she complained of a cough with white foam-like sputum, chest tightness and dyspnea. Four days later, due to dyspnea, her mental status started to gradually deteriorate. She became more and more drowsy. Biopsies of the skin and airway mucosa suggested the diagnosis of AGEP. According to the European study of severe cutaneous adverse reactions group’s scoring system, the patient scored +6 indicating a probable diagnosis of AGEP. She received intravenous methylprednisolone 120 mg/12 h for 3 d, and was eventually discharged in good condition. This patient had already experienced respiratory failure and airway mucosa involvement on admission; however, the clinicians had an insufficient understanding of AGEP. Glucocorticoid was administered for more than 10 d following onset of the disease, and her overall prognosis was satisfactory.
This case represents a rare clinical feature of AGEP and an important finding for clinicians.
Core tip: Acute generalized exanthematous pustulosis (AGEP) is a rare dermatologic reaction characterized by an erythematous rash with fever, leukocytosis and pustular erosions. We report a 42-year-old Chinese woman who developed serious AGEP involving the airway mucosa. Following treatment with intravenous methylprednisolone, the patient was eventually discharged in good condition. This case represents a rare clinical feature of AGEP and an important finding for clinicians.
- Citation: Li LL, Lu YQ, Li T. Acute generalized exanthematous pustulosis with airway mucosa involvement: A case report. World J Clin Cases 2020; 8(16): 3578-3582
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3578.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3578
Acute generalized exanthematous pustulosis (AGEP) is a severe cutaneous adverse reaction characterized by sterile pustules on erythematous skin associated with fever, leukocytosis and pustular erosions. The annual incidence of AGEP is estimated to be 1-5 cases per million[1,2]. It was first reported and named by Beyrot et al[3] in 1980. We present the rare case of a 42-year-old woman who developed serious AGEP involving the airway mucosa.
Rash, fever for 8 d, and dyspnea for 12 h.
The 42-year-old Chinese woman initially presented with fever and a small rash on her forehead and face. Over the next 2 d, she developed a diffuse, pustular, itchy rash over her trunk and legs. She also complained of a cough with white foam-like sputum, and chest tightness. Four days later, due to dyspnea, her mental status started to gradually deteriorate. She required supplemental oxygen. She then became more and more drowsy. Six days later, she received endotracheal intubation and ventilator support and was admitted to the intensive care unit. She was a housewife, 1.62 m in height with a body weight of 55.4 kg.
She had a history of lumbar disc herniation. She had taken traditional Chinese medicine for back pain 1 d before the onset of fever and rash.
She had no other past medical history, and no family history of similar diseases or psoriasis.
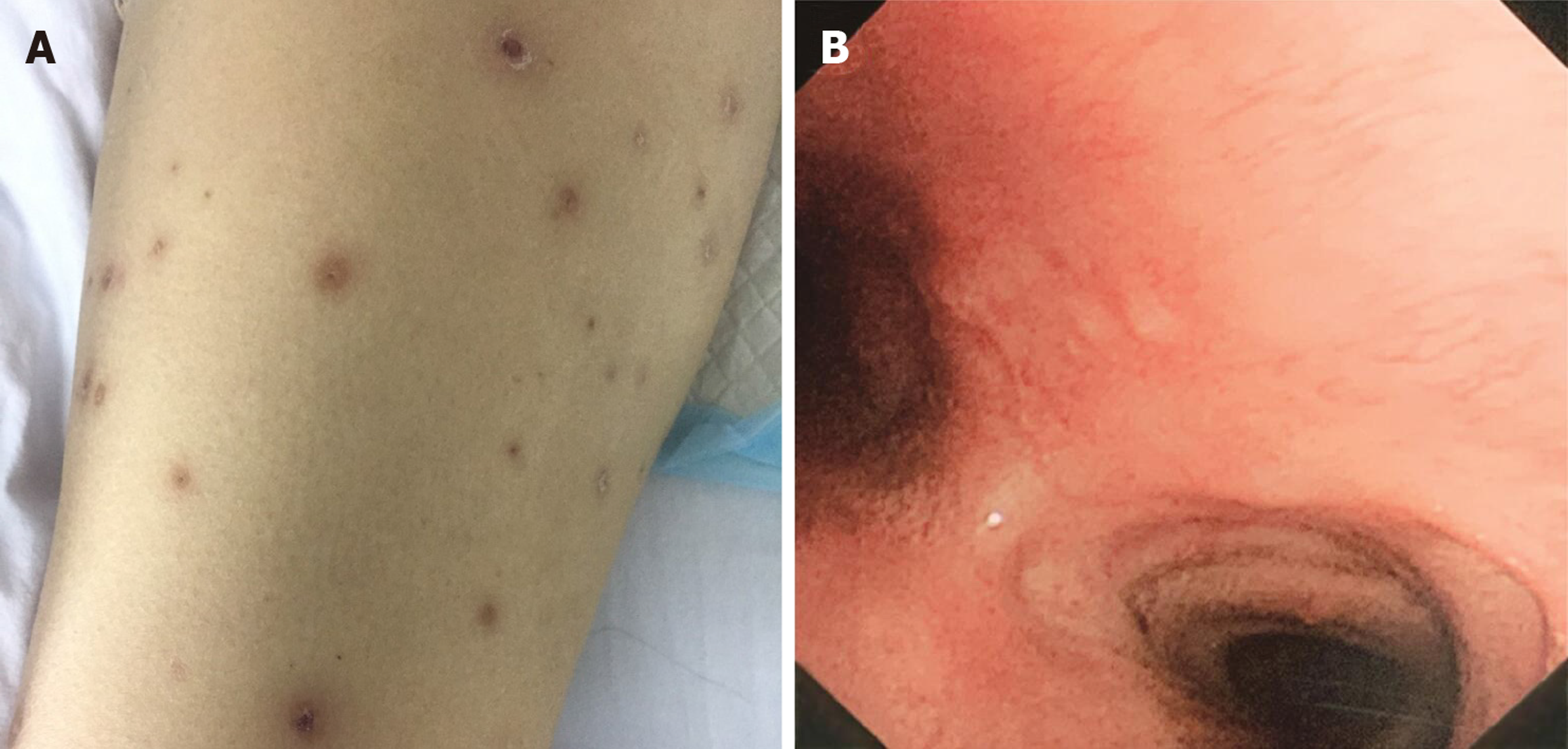
Physical examination showed diffuse, pustular rashes over her trunk and extremities (Figure 1).
Laboratory studies showed a white cell count of 15.3 × 109/L, neutrophils of 87.3%, C-reactive protein of 208.00 mg/L, and procalcitonin of 0.18 ng/mL. Blood gas analysis showed pH 7.35, PaO2 62.1 mmHg, PaCO2 58.3 mmHg, and HCO3- 31 mmol/L. A large number of white cells were seen in the pustular fluid smear. Pustular fluid culture was negative. Anti-nuclear antibody, anti-neutrophil cytoplasm antibody, anti-mitochondrial antibody, TB-GeneXpert, and T-spot were within normal limits. All blood and pustular fluid cultures were negative.
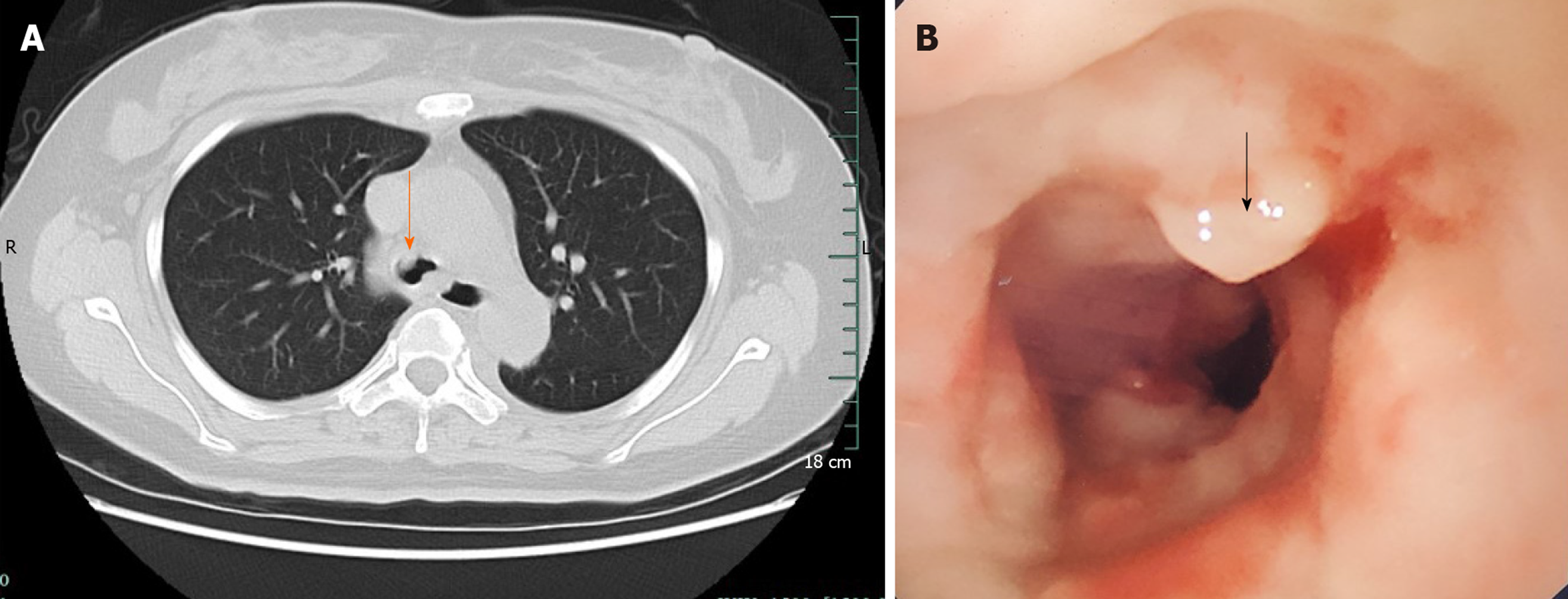
Lung computed tomography showed that the airway space was occupied and tracheoscopy was recommended. Tracheoscopy revealed an unidentified protrusion in the main bronchus (Figure 2).
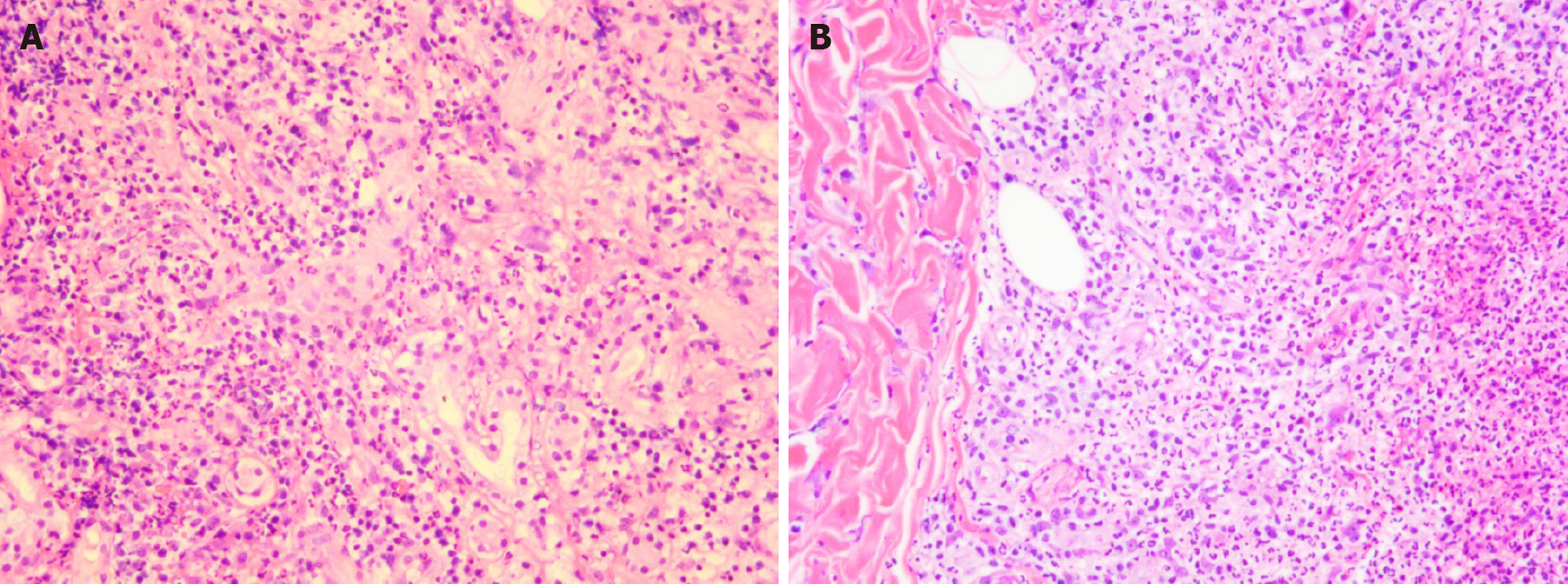
Skin and airway mucosa biopsies showed subepidermal bullous formation containing scattered neutrophils and eosinophils with occasional subcorneal neutrophilic pustules, which suggested the diagnosis of AGEP (Figure 3).
According to the European study of severe cutaneous adverse reactions group scoring system, used in the identification of AGEP, the patient scored +6, indicating a probable diagnosis of AGEP. Her final diagnosis was AGEP, acute respiratory failure (type II), and pulmonary encephalopathy.
On hospital day 5, broad spectrum antibiotics were discontinued. The patient then received intravenous methylprednisolone 120 mg/12 h on hospital day 6.
Following treatment with intravenous methylprednisolone, the patient's rash began to subside and there was desquamation of the skin after AGEP resolution (Figure 4A). The pustules gradually dried up and scabbed (Figure 4B). Post-treatment bronchoscopy showed that the airway was unobstructed (Figure 4). The patient was eventually discharged in good condition under instructions to avoid traditional Chinese medicine.
The diagnosis of AGEP includes the following: (1) Fever > 38°C; (2) Acute pustular eruption; (3) Neutrophilia; (4) Subcorneal or intra-epidermal pustules on skin biopsy; and (5) Spontaneous resolution within 15 d[1]. Our patient met all these features.
Cases of AGEP involving oral mucosa have been reported. However, cases of airway mucosa involvement are rare. The etiology of AGEP is not fully understood. More than 90% of AGEP cases are caused by drugs, such as aminopenicillins, pristinamycin, hydroxychloroquine, quinolones, sulfonamides, terbinafine, ketoconazole, diltiazem, and fluconazole[4-8]. Additional causes of AGEP, such as contact with mercury[9], have also been described. In this case, the patient took traditional Chinese medicine before the onset of the disease; thus, the possibility of AGEP caused by heavy metals in the traditional Chinese medicine or the traditional Chinese medicine itself should be considered.
AGEP is a self-limited disease with a short course and good prognosis. In severe cases, glucocorticoids should be administered. The mortality rate is less than 5%, and death is usually caused by multiple organ dysfunction and diffuse intravascular coagulation. Patients with a high risk of death are generally associated with other diseases or extensive skin lesions and mucous membrane involvement[10]. This patient had already experienced respiratory failure and airway mucosa involvement on admission; however the clinicians had an insufficient understanding of AGEP. A glucocorticoid was administered for more than 10 d after onset of the disease, and the overall prognosis was satisfactory.
AGEP is a self-limited disease with a good prognosis. This case represents a rare clinical feature of AGEP and an important finding for clinicians. Doctors should pay attention to possible AGEP, when a patient has rashes and fever.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Protopapas A S-Editor: Zhang H L-Editor: Webster JR P-Editor: Liu JH
| 1. | Roujeau JC, Bioulac-Sage P, Bourseau C, Guillaume JC, Bernard P, Lok C, Plantin P, Claudy A, Delavierre C, Vaillant L. Acute generalized exanthematous pustulosis. Analysis of 63 cases. Arch Dermatol. 1991;127:1333-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 309] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Rastogi S, Modi M, Dhawan V. Acute localized exanthematous pustulosis (ALEP) caused by Ibuprofen. A case report. Br J Oral Maxillofac Surg. 2009;47:132-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Beylot C, Bioulac P, Doutre MS. [Acute generalized exanthematic pustuloses (four cases) (author's transl)]. Ann Dermatol Venereol. 1980;107:37-48. [PubMed] |
| 4. | Sidoroff A, Dunant A, Viboud C, Halevy S, Bavinck JN, Naldi L, Mockenhaupt M, Fagot JP, Roujeau JC. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational case-control study (EuroSCAR). Br J Dermatol. 2007;157:989-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 330] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 5. | Miteva L, Kadurina M, Schwartz RA. Childhood acute generalized exanthematous pustulosis induced by oral ketoconazole. Acta Dermatovenerol Croat. 2010;18:267-270. [PubMed] |
| 6. | Vassallo C, Derlino F, Brazzelli V, D'Ospina RD, Borroni G. Acute generalized exanthematous pustulosis: report of five cases and systematic review of clinical and histopathological findings. G Ital Dermatol Venereol. 2014;149:281-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Di Lernia V, Ricci C. Fluconazole-induced acute generalized exanthematous pustulosis. Indian J Dermatol. 2015;60:212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Liccioli G, Marrani E, Giani T, Simonini G, Barni S, Mori F. The First Pediatric Case of Acute Generalized Exanthematous Pustulosis Caused by Hydroxychloroquine. Pharmacology. 2019;104:57-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Belhadjali H, Mandhouj S, Moussa A, Njim L, Amri M, Zakhama A, Zili J. Mercury-induced acute generalized exanthematous pustulosis misdiagnosed as a drug-related case. Contact Dermatitis. 2008;59:52-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Szatkowski J, Schwartz RA. Acute generalized exanthematous pustulosis (AGEP): A review and update. J Am Acad Dermatol. 2015;73:843-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 208] [Article Influence: 20.8] [Reference Citation Analysis (0)] |