Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3567
Peer-review started: April 13, 2020
First decision: April 24, 2020
Revised: July 4, 2020
Accepted: July 23, 2020
Article in press: July 23, 2020
Published online: August 26, 2020
Processing time: 133 Days and 22.7 Hours
Cholecystectomy is a common elective procedure for cholecystic diseases, including cholecystitis and cholelithiasis. Common bile duct injury is a major complication in both open and laparoscopic cholecystectomy (LC). The number of cholecystectomies performed has increased due to popularization and application of the laparoscopic technique, which has led to an increase in the number of bile duct injuries.
A 65-year-old man presented to the General Surgery Department with a complaint of repeated right upper quadrant pain for 2 years that had worsened over the previous day. The patient had a history of gallstones and hypertension. A LC was performed; it was found that a biliary stricture of 53 h duration was caused by a ligature injury of the common bile duct during the LC. Another laparoscopic exploration was performed, and the stricture was released.
LC is a common surgical procedure, but if a complication occurs, it is important for the surgeon to consider another exploratory surgery.
Core tip: Cholecystectomy is a common elective procedure for cholecystic disease, and common bile duct injury is a major complication. We report a case of a biliary stricture caused by a ligation injury of the common bile duct during a laparoscopic cholecystectomy. The patient had a biliary ligation for 53 h with an aggravated procedure 24 d after the ligation injury. The process of patient recovery is presented, which may be helpful to other surgeons who have encountered duct injuries.
- Citation: Fan Z, Pan JY, Zhang YW. Recovery from a biliary stricture of a common bile duct ligature injury: A case report. World J Clin Cases 2020; 8(16): 3567-3572
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3567.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3567
Cholecystectomy is a common elective procedure for cholecystic disease, including cholecystitis and cholelithiasis[1]. Common bile duct injury is a major complication in both open and laparoscopic cholecystectomy (LC)[2]. With advances in laparoscopic techniques, the incidence of common bile duct injury has decreased to 0.08%–0.42%[3,4]; however, the number of cholecystectomies performed has increased due to popularization and application of the laparoscopic technique, which has led to an increase in the number of bile duct injuries[2]. The main reasons for common bile duct injuries are complete transection and incorrect ligation[5]. We report a case of a biliary stricture caused by a clamping injury of the common bile duct during a LC and the process of patient recovery, which may be helpful to other surgeons who have encountered duct injuries.
A 65-year-old man presented to the General Surgery Department of the Third People’s Hospital of Dalian with a complaint of repeated right upper quadrant pain for 2 years that had worsened over the previous day.
The patient had a history of gallstones.
The patient had a history of hypertension.
The patient had no significant personal and family history.
The physical examination was significant for pain and rebound tenderness in the right upper quadrant upon palpation.
All laboratory testing, including glutamic-pyruvic transaminase (ALT) glutamic-oxalacetic transaminase (AST), gamma-glutamyl transpeptidase (GGT), and alkaline phosphatase was normal, except that the total bilirubin (TBIL) was 28.7 μmol/L and the direct bilirubin (DBIL) was 9.1 μmol/L.
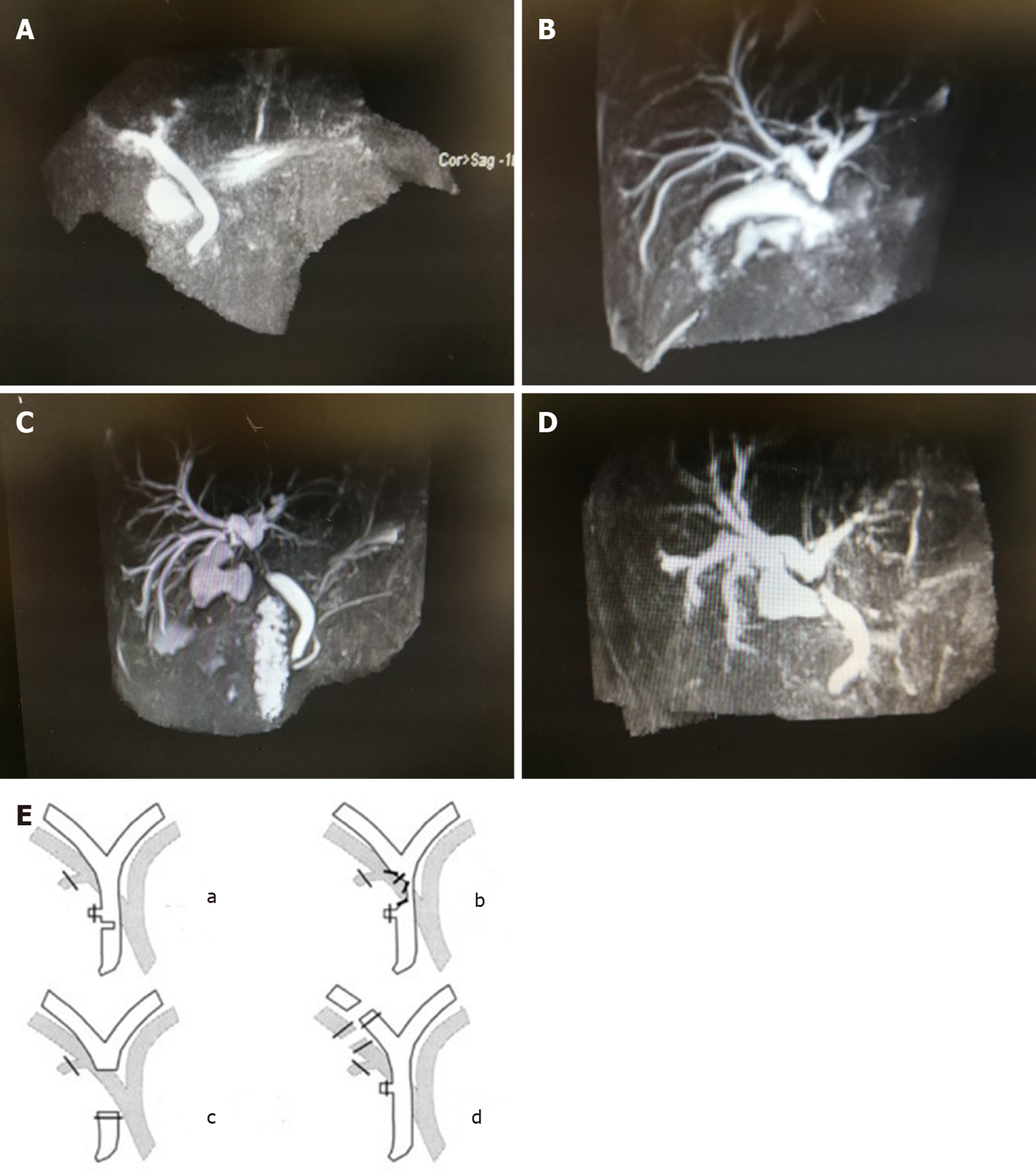
Because of the abnormal TBIL and DBIL, magnetic resonance imaging (MRI) was performed, and the MRI did not demonstrate a cholecyst and no strictures of the biliary ducts were noted (Figure 1A); ultrasonography was not performed.
A calculous cholecystitis was diagnosed.
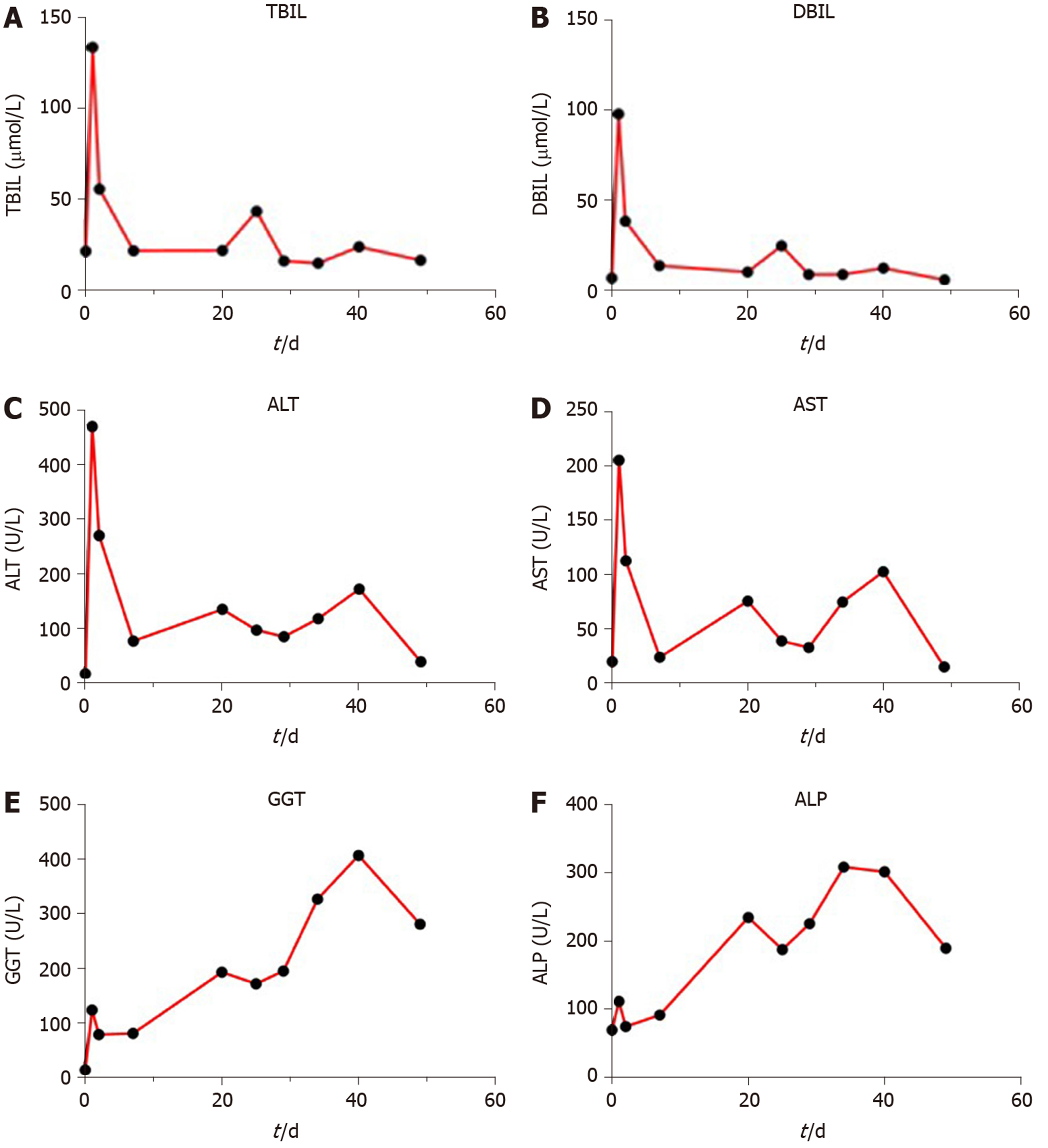
Following treatment with a cephalosporin for 6 d, the TBIL decreased to 21.7 μmol/L, and the DBIL decreased to 7.2 μmol/L. A LC was performed without apparent complication; however, inflammation around Calot's triangle was noted. The pathologic diagnosis was reported as inflammation of the gallbladder and gallstones. On post-operative day 1, the patient complained of mild pain in the right upper quadrant. The pain worsened on post-operative day 2, and the physical examination was significant for jaundice. Laboratory testing revealed the following: TBIL, 133.7 μmol/L; DBIL, 98.1 μmol/L; ALT, 470 U/L; AST, 206 U/L; GGT, 124 U/L; and alkaline phosphatase, 112 U/L. MRI showed an interruption in the mid-common bile duct (Figure 1B). Therefore, a laparoscopic exploration was performed, and the common bile duct was not filled. Intra-operative ligation of the common bile duct was demonstrated due to cholecyst duct traction, similar to a class II Stewart-Way injury (Figure 1E b). The stricture was released, and the common bile duct filled. The patient was administered anti-inflammatories and hepatoprotective therapy for 7 d. The ALT and AST levels decreased slowly, and there was rebound on post-operative day 24. Anti-inflammatories and hepatoprotective therapy were continued for another 7 d. MRI was repeated on the 26th day after releasing the ligature (Figure 1C). The ALT and AST levels had normalized by post-operative day 49. Interruption of the cholecystic bile duct was confirmed based on MRI changes (Figure 1D). The patient was asymptomatic, and the ALT and AST levels remained within the normal range on post-operative day 59.
The patient remained stable and healthy during the 10-mo follow-up evaluation.
LC became the gold standard for benign cholecystic diseases in the late 1980s, and > 750000 patients have undergone LCs in the United States[6]. However, with the large number of surgical procedures there have been a significant number of reported iatrogenic injuries. Injury of the common bile duct is a severe complication during LC, and it could lead to significant long-term morbidity, including recurrent strictures, inflammation of the biliary tract, and cirrhosis[7]. There are several causes leading to injury of the common bile duct, including anatomic variations of the extrahepatic bile ducts, inflammatory changes due to cholecystitis, intra-operative bleeding, and lack of surgical experience[2,8]. Biliary injuries that occur during LC are usually more severe than those that occur during open cholecystectomy because injuries are often near to or directly involve the second- and third-order bile ducts[8]. Based on the anatomic structure and mechanism of injury, the patient described herein had a class II Stewart-Way injury (Figure 1E)[9]. Way et al[9] reported 55 (22%) class II Stewart-Way injuries, of which 37 patients (68%) had injuries because of poor exposure. The present patient had a 2-year history of recurrent pain and inflammation around Calot's triangle. Drawing the ductus cysticus resulted in clamping the common bile duct and a stricture injury. Based on the MRI findings and elevated TBIL and DBIL levels on post-operative day 2, obstruction of the biliary tract was suspected, therefore a second laparoscopic surgery was performed to release the ligation. The time that had elapsed from ligation to release was 53 h. During the second procedure, a biliary stent was not placed, and biliary drainage was not performed. Post-operatively, the TBIL, DBIL, ALT, and AST levels slowly decreased (Figure 2A-D). On the 24th day after the second surgery, TBIL and DBIL levels increased, which suggested scarring leading to a second stricture. Thus, 7 additional days of anti-inflammatories and hepatoprotective therapy was carried out, and TBIL and DBIL levels returned to the normal range; the GGT remained elevated and decreased more slowly (Figure 2E).
We have presented a case involving a ligation injury to the common bile duct that led to a biliary stricture and provide a detailed description of the recovery process. The patient had a biliary ligation for 53 h with an aggravated procedure 24 d after the clamping injury. LC is a common surgical procedure, but if a complication occurs, it is important for the surgeon to consider another exploratory surgery.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sah DN S-Editor: Liu M L-Editor: Filipodia P-Editor: Liu JH
| 1. | Halbert C, Altieri MS, Yang J, Meng Z, Chen H, Talamini M, Pryor A, Parikh P, Telem DA. Long-term outcomes of patients with common bile duct injury following laparoscopic cholecystectomy. Surg Endosc. 2016;30:4294-4299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 2. | Zoričić I, Soldo I, Simović I, Sever M, Bakula B, Grbavac M, Marušić M, Soldo A. Common Bile Duct Stricture After Laparoscopic Cholecystectomy: Case Report. Acta Clin Croat. 2017;56:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Cai XJ, Ying HN, Yu H, Liang X, Wang YF, Jiang WB, Li JB, Ji L. Blunt Dissection: A Solution to Prevent Bile Duct Injury in Laparoscopic Cholecystectomy. Chin Med J (Engl). 2015;128:3153-3157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Halbert C, Pagkratis S, Yang J, Meng Z, Altieri MS, Parikh P, Pryor A, Talamini M, Telem DA. Beyond the learning curve: incidence of bile duct injuries following laparoscopic cholecystectomy normalize to open in the modern era. Surg Endosc. 2016;30:2239-2243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 89] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 5. | Parlak E, Odemis B, Disibeyaz S, Oztas E, Kalkan IH, Onder FO, Kucukay F, Sasmaz N, Sahin B. Cholecystectomy-related aberrant bile duct injuries and their endoscopic treatment. Surg Laparosc Endosc Percutan Tech. 2013;23:e119-e123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290:2168-2173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 316] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 7. | McMahon AJ, Fullarton G, Baxter JN, O'Dwyer PJ. Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br J Surg. 1995;82:307-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 145] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Stewart L. Iatrogenic biliary injuries: identification, classification, and management. Surg Clin North Am. 2014;94:297-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Way LW, Stewart L, Gantert W, Liu K, Lee CM, Whang K, Hunter JG. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 447] [Article Influence: 20.3] [Reference Citation Analysis (0)] |