Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3553
Peer-review started: May 1, 2020
First decision: May 21, 2020
Revised: May 30, 2020
Accepted: July 17, 2020
Article in press: July 17, 2020
Published online: August 26, 2020
Processing time: 115 Days and 16.1 Hours
Reverse rotation of the midgut is a rare type of intestinal malrotation. Volvulus of the right colon or entire midgut, stenosis of the transverse colon and obstruction of the duodenojejunal junction are common complications of reverse rotation. In this study, we report the first case of intestinal obstruction associated with reverse rotation in pregnancy.
A 31-year-old woman at 36+2 wk gestation presented to the emergency department with progressive abdominal cramping, nausea and bilious vomiting. Abdominal ultrasound scanning showed dilatation of the bowel. Computed tomography scanning revealed features of reverse rotation of the midgut with intestinal volvulus. After consultation with the obstetrician, the pregnancy was terminated and exploratory abdominal surgery was performed. Intra-operatively, it was found that the mesentery of the colon and small intestine was insufficiently attached. The right colon and the small intestinal mesentery was twisted, and intestinal necrosis was observed. The duodenum and duodenojejunal junction were curved in front of the transverse colon, and the transverse colon passed through the tunnel behind the mesenteric root. Intestinal reverse rotation with volvulus was confirmed. The necrotic intestine was resected and small intestine mesenteric reconstruction was performed. The patient recovered after surgery. After leaving the hospital, the patient and her daughter remained well during an 8-month follow-up period.
We report the diagnosis, treatment and etiology of a pregnant patient with intestinal obstruction due to reverse rotation of the midgut. For similar cases, appropriate diagnosis and treatment should be carried out according to the condition of the fetus and pregnant woman.
Core tip: Reverse rotation of the midgut is the rarest type of intestinal malrotation, accounting for approximately 2%-4%. The most common feature is that the transverse colon lies behind the superior mesenteric artery and the duodenum is located in front of the superior mesenteric artery. In this study, we report the case of intestinal obstruction associated with reverse rotation of the midgut in pregnancy. Due to reverse rotation, the patient had insufficient attachment of the ascending colon and small bowel mesentery. As the uterus enlarged, the intestinal canal shifted, causing intestinal volvulus and obstruction. To our knowledge, this is the first report of a pregnant patient with reverse rotation of the midgut.
- Citation: Zhao XY, Wang X, Li CQ, Zhang Q, He AQ, Liu G. Intestinal obstruction in pregnancy with reverse rotation of the midgut: A case report. World J Clin Cases 2020; 8(16): 3553-3559
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3553.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3553
Pregnancy complicated by intestinal obstruction is very rare, with an incidence of between approximately 1/5000 and 1/66000[1]. Intestinal volvulus is responsible for 25% of acute bowel obstructions in pregnant women. More importantly, intestinal obstruction complicating pregnancy results in maternal mortality of 6% and fetal mortality of 26%[2].
Intestinal malrotation is a congenital malformation. Malrotation can be traced to a congenital anomaly of intestinal rotation in the early stages of embryonic development, with a failure of mesentery attachment to the retroperitoneal wall[3]. Most patients are diagnosed in the first year of life, it is rarely observed in adults[4,5] and is even rarer during pregnancy[6]. Reverse rotation of the midgut is a rare type of intestinal malrotation. The most common feature is that the transverse colon lies behind the superior mesenteric artery (SMA) and the duodenum is located in front of the SMA[7]. Volvulus of the right colon or entire midgut, stenosis of the transverse colon and obstruction of the duodenojejunal junction are common complications of reverse rotation.
In this report, we describe a pregnant patient with malrotation of the midgut, and describe the diagnosis, treatment and pathogenesis of this case. To our knowledge, this is the first case of malrotation of the midgut in pregnancy.
A 31-year-old woman at 36+2 wk gestation presented to the emergency department with progressive abdominal cramping, nausea and bilious vomiting.
The patient’s symptoms started the previous day. She denied fevers, diarrhea, hematochezia and melena. She was treated with intravenous fluids and antispasmodic and analgesic therapy in a local hospital. However, the patient’s symptoms did not significantly improve.
Gravidity 2, para 1-0-0-1. A history of left ovarian teratoma resection four years previously, and a new-onset right ovarian teratoma for seven mo.
Vital signs were stable. Temperature was 37.2°C, heart rate was 90 bpm, respiratory rate was 24 breaths per minute, and BP was 120/70 mmHg. Abdominal examination revealed tenderness of the bilateral abdomen and subxiphoid area, without rebound tenderness. Fundal height was consistent with gestational age.
Leukocytosis of 14.21 × 109/L, neutrophils of 90.0%, D-dimer of 6975 ng/mL, and FIB of 4.64 g/L were observed. The other laboratory examination results were unremarkable.
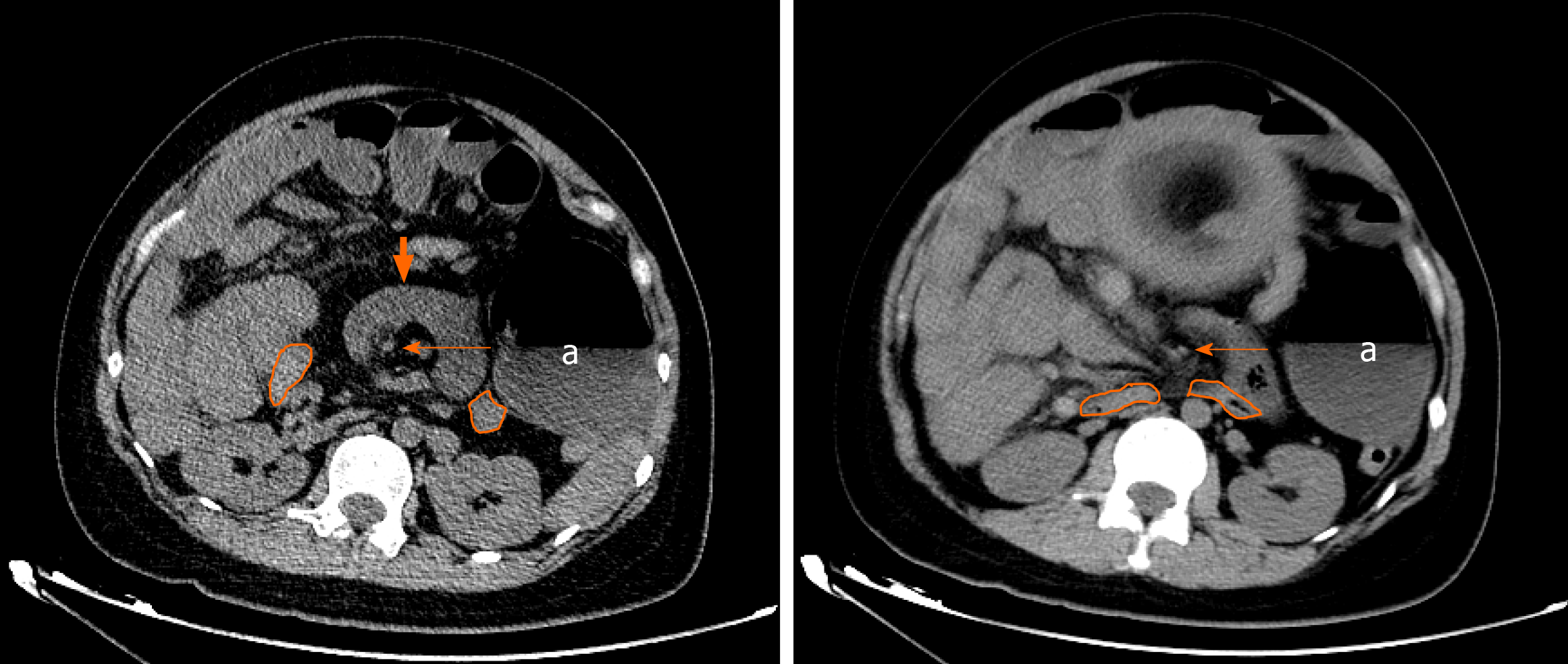
In the emergency department, abdominal ultrasound and gynecological ultrasound examination were performed. Abdominal ultrasound indicated the following: (1) Dilatation of the intestine in the abdominal cavity, with a small amount of peritoneal effusion; (2) No abnormalities were found in the gallbladder and urinary system; and (3) An enlarged appendix was not found. Gynecological ultrasound indicated the following: (1) Fetus was not deformed; and (2) Fetal heart rate was 160 bpm. According to her physical examination and ultrasound results, the patient was suspected to have intestinal obstruction. To determine the cause of intestinal obstruction, an abdominal computed tomography (CT) scan was carried out and the risks to the patient and her family were explained. The CT scan showed that the mesentery was twisted around the SMA resulting in a ‘‘whirlpool’’ sign. The dilated ascending colon had moved to the left abdomen. The transverse colon was located behind the SMA (Figure 1). The above findings suggested that the diagnosis was reverse rotation of the midgut with volvulus.
Pregnancy with volvulus and congenital reverse rotation of the midgut.
Following consultation with the obstetrician, we decided to terminate the pregnancy and perform exploratory abdominal surgery. After cesarean section, the patient gave birth to a baby girl. The baby's Apgar score was 4 at 1 min. After rescue therapy, the Apgar score rose to 9. Right ovarian teratoma exfoliation was also performed.
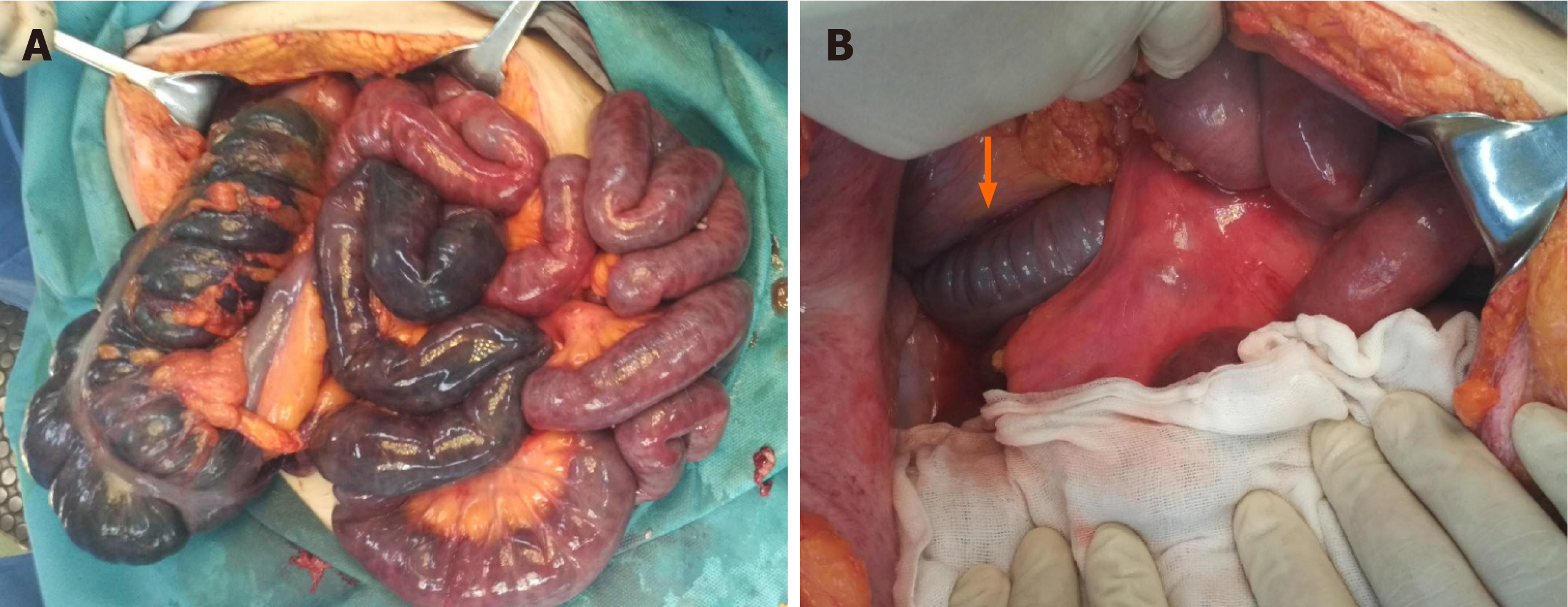
During exploratory abdominal surgery, purulent ascites was detected in abdominal cavity. The colon and small intestine mesentery was insufficiently attached. The right colon and the entire small intestinal mesentery were twisted, and the intestinal canal showed ischemic changes. The ascending colon and cecum were mobile. Although we de-rotated the mesentery and covered the ischemic intestinal tract with warm saline gauze for half an hour, the ascending colon, cecum and 78 cm of the small intestine were necrotic (Figure 2A). Further exploration of the abdominal cavity revealed that the duodenum and the duodenum jejunum were curved in front of the transverse colon, and the transverse colon passed through the tunnel behind the mesenteric root (Figure 2B). The diagnosis of reverse rotation of the midgut with volvulus was confirmed. The necrotic intestine was resected and mesenteric reconstruction was performed. The patient was transferred to the ICU where she recovered.
After leaving hospital, the mother and her daughter remained well during the 8-mo follow-up period.
Reverse rotation of the midgut is the rarest type of intestinal malrotation, accounting for about 2%-4%[8]. The incidence in females is twice than in males[9]. In normal rotation, the midgut usually rotates 90° counterclockwise and then 180° counterclockwise with the SMA as the axis. However, in reverse rotation, the midgut is rotated 90° counterclockwise and then 180° clockwise. Estrada and Gurd[7] divided reverse rotation of the midgut into two subtypes: retro-arterial type and pre-arterial type[7]. The most common is the retro-arterial type, in which the transverse colon is located behind the SMA and the duodenum is located in front of the artery, while the position of the ascending-descending colon in relation to the liver is normal. The pre-arterial type is relatively rare, that is, the relative positions of the duodenum, transverse colon and SMA are normal, but the position of the ascending-descending colon in relation to the liver is reversed (the ascending colon is left-sided and the descending colon is right-sided). Reverse rotation of the midgut often results in volvulus of the ascending colon or entire midgut due to insufficient attachment of the mesentery, which is one of the pathogenic mechanisms of intestinal obstruction caused by reverse rotation[9]. The pregnant woman in the present study, with reverse rotation of the midgut, had a retroperitoneal transverse colon and insufficient attachment of the ascending colon and small bowel mesentery. As the uterus enlarged, the intestinal canal shifted, causing intestinal volvulus and obstruction.
We performed a literature search of PubMed, based on the terms “pregnancy” and “volvulus”. The results showed that volvulus in pregnancy often occurs in the sigmoid colon, with more than 100 cases[10-12]. Volvulus in other sites of the gastrointestinal tract, such as the cecum[13-15], small intestine[16,17] and stomach[18] have also been reported. In the search results, we did not find any reported cases of volvulus in pregnancy caused by reverse rotation. Nine cases of volvulus caused by other types of intestinal malrotation were found[2,19-26]. Among them, 5 cases had extensive midgut volvulus and intestinal necrosis[19,20,23,25,26]. We performed another literature search to identify other complications caused by intestinal malrotation. The search terms used were: “Malrotation” or “nonrotation” or “reserve rotation” and “pregnancy”. In addition to the previous volvulus cases, we also retrieved one case of internal hernia[27] and one case with only symptoms of intestinal obstruction[28] (Table 1). No cases of pregnancy with reverse rotation were identified.
| Year | Author | Age (yr) | Gestational age | Imaging examination | Maternal complications | Treatment | Maternal and fetal prognosis |
| 1998 | Ventura-Braswell et al[19] | 22 | 37 WA | NA | Midgut volvulus + Intestinal necrosis | Termination of pregnancy + Surgery | Maternal recovery, Fetal survival and no malformations |
| 2010 | Gaikwad et al[20] | 27 | 33 WA | CT | Midgut volvulus + Extensive bowel necrosis | Loss of surgical opportunity | Maternal death, Fetal death |
| 2011 | Siwatch et al[21] | 23 | 20 WA | CT, Upper gastrointestinal endoscopy | Midgut volvulus | Maintained pregnancy + conservative therapy | Maternal recovery, Fetal survival and no malformations |
| 2013 | Sharma et al[2] | 28 | 9 WA | US | Transverse colon volvulus | Maintained pregnancy + surgery | Maternal recovery, Fetal survival and no malformations |
| 2013 | Kouki et al[22] | 34 | 14 WA | US, MRI | Midgut volvulus | NA | NA |
| 2014 | Hwang et al[23] | 22 | 38+2 WA | NA | Midgut volvulus + ascending colon necrosis | Termination of pregnancy + surgery | Maternal death, Fetal survival and no malformations |
| 2016 | Joyeux et al[27] | 33 | 32 WA | CT | Internal hernia | Termination of pregnancy + surgery | Maternal recovery, Fetal survival and no malformations |
| 2017 | Yin et al[28] | 23 | 9 WA-22+4 WA | MRI | Intestinal obstruction | Maintained pregnancy + conservative therapy | Maternal recovery, Fetal survival and no malformations |
| 2017 | Antunes et al[25] | 38 | 27 WA | MRI | Midgut volvulus | Maintained pregnancy + surgery | Maternal recovery, Fetal survival and no malformations |
| 2017 | Esterson et al[24] | 28 | NA | US, MRI, CT | Small bowel volvulus + superior mesenteric artery occlusion | Maintained pregnancy + surgery | Maternal recovery, Fetal survival and no malformations |
| 2020 | Chong et al[26] | 27 | 32 WA | NA | Midgut volvulus + intestinal necrosis | Termination of pregnancy + surgery | Maternal recovery, Fetal death |
Pregnancy with intestinal malrotation is relatively rare. However, once intestinal ischemia occurs, it can endanger the life of the mother and infant. Therefore, rapid diagnosis and treatment of these patients is particularly important. Some non-radiation examinations such as magnetic resonance imaging (MRI) and ultrasound are often chosen in these patients. However, the information obtained from ultrasound and MRI is often limited, and patients are often unable to cooperate with MRI due to the long time needed for this examination. CT is the best way to determine intestinal lesions, but CT is not chosen in pregnancy due to radiation exposure. Some studies have indicated that the fetal dose exceeds 100 mGy, which can significantly increase the risk of central nervous system damage, malformations and cancer[29,30]. However, the radiation dose with X-ray and CT is often less than 100 mGy[30]. Therefore, for pregnant women with suspected intestinal ischemia or perforation, low-dose CT can be performed, after excluding other factors (such as cholecystitis, appendicitis, urinary system and obstetric factors). For patients with mild symptoms, MRI or ultrasound examination can be selected. In the present case, the patient had severe abdominal colic, nausea, and vomiting. After routine antispasmodic and analgesic treatment, her symptoms were not relieved and white blood cells were elevated. These findings are highly suspicious of intestinal volvulus. When ultrasound does not detect lesions or the cause of the obstruction, CT can be performed.
Pregnant patients with intestinal malrotation usually attend the doctor due to symptoms of intestinal obstruction. Therefore, the treatment is the same as that for intestinal obstruction. For patients with mild intestinal obstruction without intestinal ischemia and sepsis, symptomatic relief and supportive treatment can be actively given, such as gastrointestinal decompression, parenteral nutrition, antispasmodic drugs, etc[21,28]. In patients who have developed serious complications, emergency surgery is required. Before 28 wk gestation, we should try to solve the obstruction while maintaining the pregnancy. After 32 wk gestation, digestive surgery must be performed after an emergency cesarean section. Between 28 and 32 wk gestation, it should be determined whether to terminate the pregnancy according to fetal development and the condition of the pregnant woman. In this case, intestinal volvulus was confirmed by CT examination, and this patient was 36 wk gestation. Following the obstetrician's evaluation, the pregnancy was terminated.
Reverse rotation of the midgut is a relatively rare congenital intestinal malrotation. We introduce the first pregnant patient with reverse rotation of the midgut, and revealed the pathogenesis of this condition. In similar cases, appropriate diagnosis and treatment is essential according to the gestational age and condition of the fetus and the condition of the pregnant woman.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Committee Member of IBD Group, Coloproctology Branch, Chinese Medical Doctor Association; Committee Member of TaTME Group, Colorectal Cancer Branch, Chinese Medical Doctor Association; Committee Member of Organ Function Protection Group, Colorectal Cancer Branch, Chinese Medical Doctor Association; Youth Committee Member of Colorectal Surgery Branch, Chinese Medical Doctor Association; Standing Committee Member of IBD Alliance, Wu Jieping Medical Foundation; Committee Member of Surgery Branch, Tianjin Medical Doctor Association; Committee Member of Colorectal Group, Surgery Branch, Tianjin Medical Association; Committee Member of IBD Expert Committee, Beijing Medical Award Foundation.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Altintoprak Fatih, Erdogan D, Viswanath YKS S-Editor: Zhang L L-Editor: Webster JR P-Editor: Xing YX
| 1. | Perdue PW, Johnson HW, Stafford PW. Intestinal obstruction complicating pregnancy. Am J Surg. 1992;164:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 134] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Sharma D, Parameshwaran R, Dani T, Shetty P. Malrotation with transverse colon volvulus in early pregnancy: a rare cause for acute intestinal obstruction. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Snyder Wh Jr, CHAFFIN L. Embryology and pathology of the intestinal tract: presentation of 40 cases of malrotation. Ann Surg. 1954;140:368-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 110] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Camera L, Calabrese M, Mainenti PP, Masone S, Vecchio WD, Persico G, Salvatore M. Volvulus of the ascending colon in a non-rotated midgut: Plain film and MDCT findings. World J Radiol. 2012;4:439-442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Sheikh F, Balarajah V, Ayantunde AA. Recurrent intestinal volvulus in midgut malrotation causing acute bowel obstruction: A case report. World J Gastrointest Surg. 2013;5:43-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Kotobi H, Tan V, Lefèvre J, Duramé F, Audry G, Parc Y. Total midgut volvulus in adults with intestinal malrotation. Report of eleven patients. J Visc Surg. 2017;154:175-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Estrada RL, Gurd FN. Surgical correction of reversed rotation of the midgut loop. Surg Gynecol Obstet. 1962;114:707-717. [PubMed] |
| 8. | Berardi RS. Anomalies of midgut rotation in the adult. Surg Gynecol Obstet. 1980;151:113-124. [PubMed] |
| 9. | Davies O, Johansen R, Goldman L. Reversed rotation of the bowel causing acute intestinal obstruction. Ann Surg. 1955;142:875-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Al Maksoud AM, Barsoum AK, Moneer MM. Sigmoid volvulus during pregnancy: A rare non-obstetric complication. Report of a case and review of the literature. Int J Surg Case Rep. 2015;17:61-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Serafeimidis C, Waqainabete I, Creaton A, Vakamacawai E, Kumar R. Sigmoid volvulus in pregnancy: case report and review of literature. Clin Case Rep. 2016;4:759-761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Tesnière M, Arnoult A, Roger N. Sigmoid Volvulus in Pregnancy. J Emerg Med. 2018;54:e129-e131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Montes H, Wolf J. Cecal volvulus in pregnancy. Am J Gastroenterol. 1999;94:2554-2556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Chase DM, Sparks DA, Dawood MY, Perry E. Cecal volvulus in a multiple-gestation pregnancy. Obstet Gynecol. 2009;114:475-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Ferris BWC, Dyke G. Caecal volvulus post-appendicectomy in pregnancy: a case report. ANZ J Surg. 2019;89:433-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Naef M, Mouton WG, Wagner HE. Small-bowel volvulus in late pregnancy due to internal hernia after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2010;20:1737-1739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Cong Q, Li X, Ye X, Sun L, Jiang W, Han Z, Lu W, Xu H. Small bowel volvulus in mid and late pregnancy: can early diagnosis be established to avoid catastrophic outcomes? Int J Clin Exp Med. 2014;7:4538-4543. [PubMed] |
| 18. | Inoue A, Mizuta H, Ito A, Tsujikawa T, Furukawa A, Murata K. Mesenteroaxial Gastric Volvulus Diagnosed with MR Imaging during the Early Stages of Pregnancy. Magn Reson Med Sci. 2019;18:243-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Ventura-Braswell AM, Satin AJ, Higby K. Delayed diagnosis of bowel infarction secondary to maternal midgut volvulus at term. Obstet Gynecol. 1998;91:808-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Gaikwad A, Ghongade D, Kittad P. Fatal midgut volvulus: a rare cause of gestational intestinal obstruction. Abdom Imaging. 2010;35:288-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Siwatch S, Noor MT, Dutta U, Kochhar R, Behera A, Singh K. Endoscopic management of a pregnant lady with duodenal obstruction due to malrotation with midgut volvulus. Trop Gastroenterol. 2011;32:339-341. [PubMed] |
| 22. | Kouki S, Fares A, Alard S. MRI whirpool sign in midgut volvulus with malrotation in pregnancy. JBR-BTR. 2013;96:360-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Hwang SM, Na YS, Cho Y, You DG, Lee JJ. Midgut volvulus as a complication of intestinal malrotation in a term pregnancy. Korean J Anesthesiol. 2014;67:S98-S99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Esterson YB, Villani R, Dela Cruz RA, Friedman B, Grimaldi GM. Small bowel volvulus in pregnancy with associated superior mesenteric artery occlusion. Clin Imaging. 2017;42:228-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Gião Antunes AS, Peixe B, Guerreiro H. Midgut Volvulus as a Complication of Intestinal Malrotation in Pregnancy. ACG Case Rep J. 2017;4:e9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Chong E, Liu DS, Rajagopal V, Strugnell N. Midgut volvulus secondary to congenital malrotation in pregnancy. BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Joyeux E, Gobenceaux AS, Hoyek T, Dellinger P, Sagot P. Intestinal malrotation complicated by an occlusive syndrome involving internal hernia in a pregnant woman. J Surg Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Yin Y, Li C, Xu C, Wu L, Deng N, Hou H, Wu B. Intestinal obstruction due to congenital malrotation complicating a multiple pregnancy: A rare case report. J Pak Med Assoc. 2017;67:308-310. [PubMed] |
| 29. | Stewart A, Kneale GW. Radiation dose effects in relation to obstetric x-rays and childhood cancers. Lancet. 1970;1:1185-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 178] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 30. | Popić Ramač J, Garaj Vrhovac V, Vidjak V, Brnić Z, Radošević Babić B. Safety of Radiographic Imaging in Pregnancy. Acta Clin Croat. 2016;55:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |