Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3515
Peer-review started: January 11, 2020
First decision: April 24, 2020
Revised: May 18, 2020
Accepted: July 14, 2020
Article in press: July 14, 2020
Published online: August 26, 2020
Processing time: 227 Days and 4.6 Hours
Body parts such as the face and hands are highly exposed during daily life and burns may accumulate in these areas. In addition, residual wounds, scar hyperplasia and contracture often exist in the late stage of a deep burn in these areas, which may affect patients’ appearance, movements, and mental health. However, inadequate attention has been paid to this issue which can result in problems, such as difficulty in healing, possibility of carcinoma, chronic pain and a heavy mental burden.
To investigate the long-term medical treatment of patients with severe burns at exposed sites following a mass burn casualty event.
A retrospective analysis of 13 patients with severe burns at exposed sites was performed to determine their respective long-term medical treatment. A combined wound dressing scheme consisting of traditional Chinese and Western medicine was introduced to repair residual wounds. Active and passive functional exercises with massage, Chinese herbal baths and compression fixation were proposed to ameliorate the condition of the hands. A combination of physical, chemical and photoelectrical measures was adopted for anti-scar treatment. A psychological intervention and recovery guide was provided which corresponded to the patients’ psychological status.
Compared to patients who did not simultaneously receive the same treatment, patients who underwent systematic treatment recovered with a lower wound infection rate (P < 0.05), a shorter healing time (13.6 ± 3.2 d) compared with (19.1 ± 3.5 d) and more bearable pain during wound dressing at three days, one week and two weeks after a Chinese herbal bath (P < 0.05). Satisfactory results were achieved with regard to restored function of patients’ joints and blood supply to nerve endings, closure of the eyelids and the size of mouth opening tended to be normal, and only 7.1% of patients were diagnosed with severe scar hyperplasia and contracture deformity compared with 30.7% in the control group. In addition, the color, thickness, vascular distribution and softness score of the scars improved (P < 0.01), and the effects of the psychological intervention was remarkable as shown by the Self-Rating Anxiety Scale and Self-Rating Depression Scale.
A better prognosis can be achieved in patients in the late stage of a burn with active residual wound repair, limb functional exercise, anti-scar and psychological rehabilitation.
Core tip: Burns on the face and hands substantially affect patients’ daily life. A combination of Chinese and Western medicine was adopted to repair residual wounds. Patients were provided with individualized anti-scar and functional exercise schemes. Early psychological disorder screening and intervention were conducted. The long-term treatment of burn patients should include a combination of therapies.
- Citation: Du Y, Lv GZ, Yu S, Wang D, Tan Q. Long-term medical treatment of patients with severe burns at exposed sites. World J Clin Cases 2020; 8(16): 3515-3526
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3515.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3515
Massive burns often occur in emergencies or accidents[1], the face and hands are the areas where burns are prone to accumulate due to their exposure in daily life. In addition, the late stage of a deep burn is always accompanied by residual wounds where the colonization of drug-resistant bacteria can be detected[2], also scar hyperplasia and contracture, may result in an unpleasant appearance and physical limitations. Moreover, long-term hospitalization may isolate patients from society and their family, which adds to the high possibility of disability as well as suffering during treatment and can aggravate patients’ mental illness[3,4].
However, numerous patients, family members or even doctors have not taken these factors into account, which can result in problems, such as wound infection, difficulty in healing, excessive growth of scar tissue with contraction and deformity, etc. We adopt non-invasive anti-scar treatment which includes physical massage and hormone injection to prevent or mitigate scar formation, improve overall scar appearance, joint function and quality of life. The effect of single anti-scar treatment is often limited[5,6], some patients may be diagnosed with anxiety, dread or even post-traumatic stress disorder (PTSD), resulting in a severe decline in patient quality of life[7]. Patients are less likely to continue treatment and may lose faith in living due to long-term agony.
This study focuses on combining traditional Chinese and Western medicine to cleanse wounds and accelerate the healing process; skin grafting is conducted at the early stage of treatment along with instructions on functional exercise and rehabilitation to prevent scar hyperplasia and boost the recovery of hand function. During the treatment process, a psychological intervention was carried out to reduce the incidence of psychological problems.
The present study included 13 patients with severe burns at exposed sites in a mass burn casualty event, 3 males and 10 females with an age range of 21-25 years, and a mean age of 22.3 years. The total body surface area (TBSA) affected ranged from 18% to 36%; each patient was found to have 3-7 residual wounds, and the diameter of these wounds ranged from 0.5 cm to 7 cm. Two patients had facial wounds, 11 patients had hand wounds, and 6 patients had wounds at donor sites. Of these patients, 12 suffered severe facial burns, which were confirmed as second- and third-degree burns with 0.5%-3% TBSA; 13 patients suffered severe hand burns, which were diagnosed as second- and third-degree burns with 1%-2% TBSA; one patient also had epilepsy.
Group A were college student patients, and we randomly selected 13 patients who did not receive systematic treatment as Group B. The patients in Group B were similar to those in Group A except that they did not undergo the same treatment.
Treatment of residual wounds: There were 13 patients with different degrees of residual wounds, and the wounds of 3 patients were found to have adhesions of yellowish-brown necrotic tissue, in which Staphylcoccus aureus, Acinetobacter baumannii, and other bacteria were detected following bacterial wound culture, these patients underwent a traditional Chinese medicine bath[8]. First, the patients underwent Chinese herbal bath therapy for 10-15 min, and dirty and necrotic tissues were removed along with the secretions from wounds; next, the facial wounds were cleaned, and patients were instructed to lie flat and cover the face with gauze dipped in herbal lotion for several min, the secretions were removed using the gauze, which dislodged scabs and pustules; after that, the wounds were slowly dried with sterile gauze, followed by iodophor disinfection, the aged granulation tissue was removed according to the patients’ tolerance, and the wounds were rinsed with normal saline. Recombinant human epidermal growth factor gel (20 g, Pavay Gene Pharmaceutical Co., Ltd., Guilin, China) was applied to accelerate healing, using a sterile wound dressing. The Chinese herbal bath therapy lasted 20-30 min each time, 2-3 times/wk, and the wounds generally healed within 1-3 wk.
The Chinese herbal lotion in the Chinese herbal bath therapy was composed of the following ingredients: Shensanqi 6 g, Chuanqiong 12 g, Chiscou 20 g, Wine Angelica 20 g, Sanguisorba 20 g, Frankincense 18 g, Stir-fried Myrrh 18 g, Fresh Peel 20 g, and Skullcap 10 g. The herb particles were placed in warm water (20-30°C) and stirred, in order to ensure that the wounds were fully immersed in the lotion.
The outcome measures and evaluation criteria: (1) The distribution of bacteria around the wounds: A sample of the secretion from the wounds before and one week after Chinese herbal bath therapy was obtained, in which each sample consisted of a secretion taken from three different wounds. The samples were taken from the same sites with the same area by a surface sampling method, we collected 78 samples in total, and the final strain type in each sample depended on the majority of strains detected; (2) Duration of healing and relapse; and (3) The pain during wound dressing: Before and one week after the Chinese herbal bath therapy, a visual analog score was used to evaluate the pain with 10 grades, and the highest score represented the highest severity of pain.
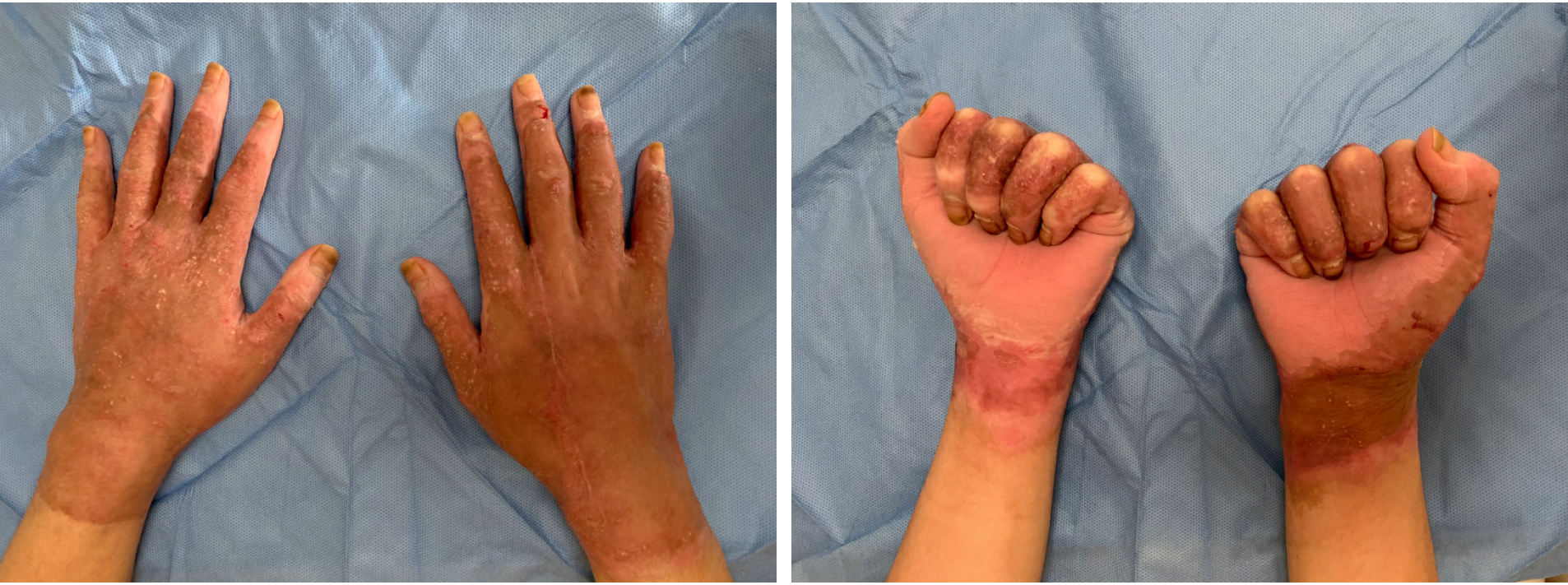
Functional exercises for hands: Patients started rehabilitative functional exercises of the hands 2 wk after skin grafting. Comprehensive rehabilitation plans were made according to the severity of hand injury: (1) Active and passive finger movements: Patients performed active and passive movements along the moving direction of joints, and the rehabilitation exercises were in the opposite direction against the flexion and stretch of the joints, e.g., scars on the flexion side, and the exercises stretched the joints. The majority of patients performed these functional exercises which were aimed at the metacarpophalangeal joints and interphalangeal joints. It was essential to assist patients to carry out the movements in the opposition direction, close the fingers together and clench their fists, as these exercises can help them regain normal hand function. Apart from the active and passive movements mentioned above, a spinning exercise around the joint axis was also essential. It was recommended that the patients exercise for 20-30 min each time several times per day, strictly follow the principle of gradual improvement, and increase the intensity and range of movement to the maximum limits of the joints. The patients were made aware that over-training can cause injuries to joint ligaments and surrounding soft tissues; however, it was essential to motivate patients to exercise regularly at any time and any place; (2) Massage: Silicone gel to soften scars and urea cream to moisturize the skin were applied, and pressure was applied to the skin surface when patients had undergone operations on the thumb pulp or thenar. The scars were gently rubbed in a circular motion with moderate force and a slow and uniform speed. The massage should last for 15 min, 3 times per day, and can accelerate the absorption of medicine, prevent scar hyperplasia, and prevent the skin around the scar from drying; (3) Chinese herbal bath therapy: The patient’s hands were immersed in herbal lotion for 5 min at 38°C, the fingers were separated and a fist was made under water to boost circulation, accelerate medicine absorption, and exercise the joints; and (4) Compressive fixation: Fixation or anti-retraction bandaging was adopted during night sleep, the scar was pressed with an elastic bandage, and fixed with a plastic brace to maintain the hands in a functional position (Figure 1). To prevent joint contracture, the bandaging was readjusted according to how the hands recovered.
The curative effect was divided into four grades based on the condition of patients’ joints and self-care ability. Treatment standards: (1) Cured: The movement of the joints fully recovered, enabling patients to take care of themselves and continue working; (2) Treatment markedly effective: The majority of joint functions were regained, the eyelids could close, the size of mouth opening was normal, hands could be clenched or half clenched, patients could basically take care of themselves, and were capable of a number of light physical labors; (3) Effective: The joint functions were partly regained, the scope of activity was expanded, hands could partly finish the movements, and patients needed assistance in daily life, and were not able to attend their workplace; and (4) Ineffective: No changes were observed before and after treatment.
Regular anti-scar therapy: At the early stage of treatment, silicone gel (Kelo-cote, IJSA Advanced Bio-Technologies Inc.) was purchased for external application. Before applying, the scar was rinsed with warm water and dried, then, an appropriate amount of gel was gently rubbed around the scar. The correct amount of gel per square centimeter was approximately equal to the size of a rice grain. The silicone gel was applied three times per day, and was rubbed for 15 min until it had naturally dried in. After that, urea cream was applied to moisturize the skin. When the skin around the scar was stable, we recommended the use of silicone gel sheets accompanied by an elastic garment to add pressure to the flat area. The specific steps are as follows: The surface was cleaned with warm water, the silicone gel sheets were placed for 4 h initially and gradually increased with intervals of 2 h each day, and extra pressure was provide with the designed elastic garment. The pressure was maintained around 20-40 mmHg (1 mmHg = 0.133 kPa) for 24 h. It was advantageous to select the maximum pressure under the precondition that it had limited effects on peripheral circulation with no obvious discomfort, and the pressure could be adjusted at any time to make the skin around the scars turn white. The time reserved for cleaning was no longer than 30 min. This routine was continued for 3-6 mo, and the elastic garment was regularly cleaned and replaced to maintain appropriate elasticity.
Anti-scar treatment for particular organs of the body: Massage therapy was conducted at the beginning of eyelid scar hyperplasia, the finger pulp was used to massage outwards along the eyelid margin, and it was essential to perform the massage therapy slowly and carefully in order to protect the skin from being damaged or infected; massage was carried out 60 times in different directions each time, and this procedure was repeated several times per day; preventive anti-scar treatment for the mouth was conducted as early as possible, hence, it was highly essential to use a mouth-gag or bottle plug to enlarge the mouth to reduce contracture. For facial treatment, a well-fitted plastic silicone gel film was used to add the precise amount of pressure to the skin.
When the grafted skin was stable, patients could have their hands wrapped in elastic gloves. To add pressure to the skin, the pressure was properly maintained and adjusted based on the patients’ reactions. Simultaneously, anti-scar treatment was conducted with silicone gel ointment and silicone gel sheets (Figure 1). It was essential to observe the spots where scar hyperplasia was obvious during compression treatment, e.g., metacarpophalangeal joints and finger webs. Thus, it was essential to stuff gauze in the respective parts to enlarge the volume for higher pressure when putting on elastic gloves.
Laser therapy: In the present research, plasma red blood dispelling therapy was performed at the early stage of scar hyperplasia with a wavelength of 500-600 nm. During laser therapy, the energy density was 7-8 J/cm2 based on patients’ tolerance, the pulse width was 15 s, with cooling of 50%, the skin was then iced for at least 30 min after therapy, and a second therapy was arranged for the next month.
Two months after wound healing, scar hyperplasia was obvious in some wounds. Patients were instructed to undergo micro-plasma laser therapy. Patients also underwent a light board skin test to confirm the appropriate range of parameters. It was favorable to have a moderate uniform reticular white scab on the skin after the test. The anesthetic paste on the surface was removed, and the scar was cleaned with clear water after alcohol disinfection. According to the shape and severity of the scars, we attempted to choose an in-motion sliding mode or stationary targeted mode or the combination of both for the treatment. The efficacy of treatment, exposure time, and treatment times were evaluated based on the expected effects and skin lesion response rate. The ranges of the parameters were as follows: The power set for in-motion sliding mode was 80-100 W, running for 2-4 times; and the direction of the roller was adjusted according to the shape of the scars. The power required for the stationary mode was set to 50-70 W, and the duration of exposure was 0.2-0.6 s. Mild or moderate erythema emerged on the normal skin around the surgical area, and the scarred skin was slightly yellowish with a small amount of oozing. Next, the treatment parameters were adjusted according to the skin endpoint reaction, the interval between treatments was 6-8 wk, and the exact number of repeated treatments depended on how well the skin recovered.
Vancouver scar scale: On the first, third, and sixth month after treatment, the Vancouver scar scale (VSS) was used to evaluate the color, thickness, blood vessel distribution, and softness of the scar.
The self-rating anxiety scale (SAS) and self-rating depression scale (SDS) were applied to evaluate the patients’ mental status, and conduct the corresponding psychological intervention in patients with negative psychology, and reevaluation was undertaken to assess the efficacy of the intervention.
The psychological intervention methods were as follows: (1) Improve the living environment, allocate wards to patients with the same disorders; (2) Humanistic care. Communicate with patients frequently and address their condition in a relaxed manner, and encourage patients to actively cooperate with treatment; (3) Support from family and society. Suggest that patients’ family members and friends should attend and assist physicians to conduct further treatment; and (4) Establish a communication-based platform. Create an on-line communication-based platform for patients to exchange experiences and boost their confidence.
In this study, SPSS 22.0 software (IBM, Armonk, NY, United States) was used to process the data. Measured data are presented as the mean ± SD. The paired t-test was used to compare the results in the same group before and after treatment. One-way analysis of variance (ANOVA) was used to indicate whether there were any statistically significant differences between the means of two or more independent (unrelated) groups. P < 0.05 was considered statistically significant.
After Chinese herbal bath therapy, the rate of bacterial detection was lower than before, and there was a change in the type of bacteria (Table 1).
| Group | Time | Staphylococcus aureus | Acinetobacter baumannii | Escherichia coli | Others | Detection rate |
| A | Before Chinese herbal bath | 15 (38.4) | 12 (30.8) | 6 (15.4) | 6 (315.4) | 100 |
| One week after the Chinese herbal bath | 3 (7.7) | 1 (2.6) | 0 (0) | 0 (0) | 10.26a | |
| B | Before Chinese herbal bath | 19 (48.7) | 10 (25.6) | 6 (15.4) | 4 (10.3) | 100.0 |
| One week after the Chinese herbal bath | 13 (33.3) | 6 (15.4) | 4 (10.3) | 3 (7.7) | 66.67c |
The duration of healing in Group A was 13.6 ± 3.2 d, which was significantly shorter than that in Group B at 19.1 ± 3.5 d (t = 5.999, P = 0.000). When the wounds had healed, two patients were found to have bubbles and bursts on their new growing skin, and the wounds healed quickly after wound dressing.
The severity of pain during wound dressing before and one week after Chinese herbal bath therapy is shown in Table 2.
| Group | Number of cases | Before treatment (scores) | 3 d after treatment (scores) | One week after treatment (scores) | On day 14 of treatment (point) |
| A | 13 | 7.3 ± 1.4 | 5.2 ± 1.5 | 3.8 ± 0.9 | 1.8 ± 0.7 |
| B | 13 | 7.0 ± 1.2 | 6.4 ± 1.0 | 5.2 ± 1.2 | 4.5 ± 1.3 |
| t value | - | 2.624 | 3.075 | 6.269 | |
| t‘ value | 1.075 | - | - | - | |
| P value | 0.3033 | 0.0222 | 0.0096 | < 0.0001 |
During 6 mo of follow-up, the blood supply in the grafted skin on both hands was satisfactory, and there was a mild color difference between the grafted skin and the surrounding skin. In addition, 78.6% of patients’ joints in the hands functioned well, they could easily grab and separate their fingers, the blood supply was satisfactory, eyelids could close smoothly, and the size of opening mouth was normal. Moreover, 14.3% of patients had scars on their fingers, and it is likely that they had ulcers on the joints after hand exercises, which may lead to slight difficulty in grasping. Closure of the eyelids and the size of mouth opening were normal and scar hyperplasia on the hands was noted in 7.1% of patients. As a result, the abduction of the thumb was reduced, the flexion of the remaining four fingers was restricted, and the patients had difficulty grasping. In addition, the size of mouth opening was reduced, and the conjunctiva was exposed when the eyes were closed.
The result of the VSS showed that there was a notable difference in the scores assigned to the color, thickness, vascular distribution and softness of the scars between the two groups (P < 0.01). In contrast to Group B, patients in Group A underwent anti-scar treatment (Table 3).
| Scale score | ||||||||
| Parameters | Group A | Group B | ||||||
| 1 wk | 1 mo | 3 mo | 6 mo | 1 wk | 1 mo | 3 mo | 6 mo | |
| Color | 1.3 ± 0.5 | 2.2 ± 0.6 | 2.0 ± 0.7 | 0.8 ± 0.6 | 1.4 ± 0.5 | 2.5 ± 0.5 | 3.0 ± 0.3 | 2.4 ± 0.7 |
| Thickness | 0.8 ± 0.4 | 2.2 ± 0.7 | 2.6 ± 1.0 | 1.0 ± 0.6 | 0.9 ± 0.6 | 2.6 ± 0.7 | 3.2 ± 0.6 | 2.7 ± 0.9 |
| Vascular distribution | 1.5 ± 0.5 | 2.5 ± 0.5 | 2.2 ± 0.8 | 0.8 ± 0.6 | 1.4 ± 0.7 | 2.4 ± 0.7 | 2.8 ± 0.4 | 2.1 ± 0.8 |
| Softness | 0.8 ± 0.6 | 2.7 ± 0.8 | 2.8 ± 0.7 | 1.2 ± 0.7 | 0.7 ± 0.6 | 3.1 ± 0.6 | 3.9 ± 1.0 | 3.8 ± 1.1 |
As shown in Table 4, on the basis of the analysis of changes in SAS and SDS scores, 8 (58.1%) patients expressed that they had little knowledge of their injury condition, 5 (38.5%) patients were skeptical about the medical treatment, and 7 (53.9%) patients were confused about their future life.
A typical case: A 22-year-old male was admitted 5 h after injury and was diagnosed as follows: (1) Second- and third-degree burns with 28% TBSA; (2) Burn shock; and (3) Severe inhalation injury. Anti-shock and organ protection treatments were immediately given to the patient. Additionally, “skin grafting and escharectomy operation” was arranged for the patient under general anesthesia three days after the injury, when the patient’s condition was stable, he was moved to a general ward. Physical examination revealed that vital signs were stable. The cicatrix, which caused the patient to feel uneasy and itchy, was red and protruded on the surface of the skin, and the blood supply in the grafted skin was acceptable with no obvious ulceration. Furthermore, multiple scabs were observed on the skin surface with skin tags, and the skin-offering wounds were healed on the left thigh. In addition, crimson scar hyperplasia was found and was associated with a certain degree of itch, the scar protruded on the skin by approximately 0.3 cm, and two residual wounds were found on the right thigh, which were 3 cm × 8 cm and 5 cm × 11 cm in size. Additionally, yellowish-brown necrotic tissues were adhered to the wounds with marked oozing. No obvious redness or swelling was observed in the surrounding skin. The patient underwent Chinese herbal bath therapy to wash the necrotic tissue on the hands. After disinfection of the wounds, recombinant human epidermal growth factor was used to accelerate healing every two days, and the wounds healed within 10 d. Then, dye pulsed light (DPL) laser therapy was conducted on the patient’s face and left thigh once a month to reduce blood vessels, three times in total, and the power density of laser therapy was 7 J/cm2, pulse width was 15 s, and cooling was 50%; when the treatment was undertaken, the skin was iced for at least 30 min until the redness of the scar started to fade gradually. When the scar was stable, the patient underwent micro-plasma treatment, the power of the in-motion sliding mode was set to 90 W, and the rolling direction of the roller was adjusted according to the shape of the scars. For local spot-like scars, the power set for stationary mode was 50-70 W, exposure time was 0.4 s, with one-time running. The endpoint reaction was defined as the observation of mild to moderate red spots on the surrounding skin, and the scarred skin was slightly brown with a little oozing. The treatment interval was 6-8 wk, and during the interval period, the treatment was complemented with silicone gel, an elastic garment, and a three-dimensional (3D) mask to prevent scars, and hand exercises were performed 2 times per day for 30 min each time. After these functional exercises, and anti-scar therapy for four months, the patient was discharged from hospital, and follow-up was arranged each mo. As shown in Figures 2 and 3, no obvious scar hyperplasia was found on the patient’s face and lower limbs, the eyes closed properly, the size of mouth opening was normal, hand function was restored, and the patient was able to live a normal life and study.
Massive burns often occur in emergencies or accidents, which may cause permanent disability. At the beginning of treatment, the focus is on saving lives; however, we found that treatment of facial and joint wounds may lead to different degrees of scar hyperplasia, contracture or even deformity, which can not only influence the function and appearance of the body, but also result in a heavy burden on patients mentally physically and financially. To our knowledge, there are four major points in the rehabilitation procedure: The first point is to repair residual wounds and close the wounds as quickly as possible; The second is functional exercises of joints, enabling patients to take care of themselves; The third point is anti-scar treatment, aimed at improving the appearance; and The fourth point is psychotherapy, which may help patients restore their confidence and return to society.
The majority of residual wounds are granulation wounds, and a number of these wounds have a small amount of adhered necrotic tissue. In the present study, we combined Chinese and Western therapeutic approaches, and the patients were initially asked to undergo Chinese herbal bath therapy, and then, recombinant human epidermal growth factor was applied. This was found to be helpful for removing secretions and necrotic tissue, improving the effect of bacterial-cleaning, reducing the absorption of toxins, and preventing infection. In addition, it can provide effective components to accelerate healing and epithelization of the wounds, reduce scar hyperplasia, and alleviate pain, and has significant diagnostic value and is consistent with the conclusions reported by Lv et al[8] and Akita et al[9].
Only a limited number of physicians have treated patients’ hands which have been severely burned. Although the wounds would heal through dressing and decrustation of the wounds, the treatment of patients’ hands tends to be limited, and may cause difficulties in the flexion of joints. Additionally, this negative impact may result in contracture of fingers, severe adduction of the thumb, stenosis of the transverse palmar arch, joint dislocation or rigidity, highly influencing the function and appearance of the hands, and causing endless suffering in patients, which can affect their personal life and mental health. Thus, we advocate that surgical techniques should be performed immediately in patients with severe burns of the hands, instructions on functional exercises and rehabilitation should be given after surgery to alleviate pain and to achieve better healing effects in a short period of time[10].
The healed wounds are often fragile and more likely to break or blister; therefore, the doctor’s manipulation must be gentle and slow, which should be carried out gradually by pressing, lifting, and pushing, in order to ensure that the range of motion is expanded step-by-step to prevent severe pain or injuries in tissues around joints. It is highly recommended to adopt functional fixation or anti-contracture fixation over joints during resting time, the longer the healing time, severe contractures may appear on muscles and ligaments around joints. Therefore, it is vital to start training with basic activities of daily living and gradually move on to light manual labor in order to restore joint function[11].
Scars are the result of skin over healing and hyperplasia after dermal injury, they affect the appearance and movement of limbs, and have a high incidence[12]. Spronk et al[13] found that scar hyperplasia was very obvious in severely burned patients, and anti-scar treatment was particularly essential in female patients. The majority of patients were young female college students with severe burns in exposed sites, involving the face, neck and hands; therefore, anti-scar treatment was essential.
At present, compression treatment is the first choice for treating hypertrophic scars after burns. The mechanism of preventing hyperplasia using elastic garments is that continuous pressure may reduce the blood and oxygen supply around scars; thus, a series of pathophysiological changes may occur in vivo, fibroblast proliferation may be inhibited and cause dysfunction of extracellular matrices (e.g., collagen), thereby activating collagenase, as well as accelerating decomposition of collagen. A scar plaster is a thin and transparent silicone gel film, and it generates oxygen tension and pressure over the skin, which can soften the scars and decrease pigmentation. To date, the application of a 3D scanning transparent silicone pressure mould has attracted significant attention, especially for scars on the face, neck, and chest, and the silicone-containing drugs are effective for treating scars. In the present study, 13 patients in the anti-scar treatment group were all instructed to wear a scar plaster, elastic garment, and a 3D facial pressure mask on their limbs and faces, and satisfactory results were achieved in 95.24% (12/13) of patients compared with those who did not undergo anti-scar treatment [11.11% (3/16)] (χ2 = 28.95, P < 0.05), which proved the effectiveness of this anti-scar treatment. The clinical condition of only one patient was not optimistic as he did not follow the instructions strictly recommended.
Recently, laser treatment has attracted considerable attention, although it is effective in treating scars, skin pigmentation, high cost, and a variety of operations remain a big challenge[14,15].
In the early stage of scar hyperplasia, plentiful blood capillaries, abundant nutrients and oxygen all accelerate the procedure; therefore, we conducted DPL treatment once per wk to close the blood vessels, and the color of the scar faded after 2-3 treatments. Following microdissection and collagen remodeling during micro-plasma treatment, the scar becomes flat and skin pigmentation improves. The side effects of this treatment were minor, which is consistent with the findings of Kono et al[16].
Treatment of scars with one therapeutic method is often not very effective, and integrating multiple methods is performed worldwide[17]. Silicone-containing drugs, scar plaster, 3D scanning silicone transparent pressure moulds, massage, and elastic garments are the most popular methods[18]. It is reasonable to individually prepare treatment plans according to different organs of the body, different physical conditions, and different types of scars. With the assistance of a professional rehabilitation therapist, anti-scar treatment and functional exercises can be further specified. By conducting an integrated, systematic, and continuous anti-scar treatment, satisfactory results can be achieved[19].
With the development of treatment methods for burns, a number of researchers have attempted to concentrate on psychotherapy as a high priority. Psychological problems mainly occur in burn patients throughout the entire treatment course[3]. Studies have revealed that numerous burn patients have mental disorders within one year after the accident. The impact of PTSD in burn patients is high with morbidity of 15%-45%, the majority of patients were female, and PTSD was often associated with depression and anxiety[20]. Pallua et al[21] studied burn patients for 5 years, and found that patients with large burn areas were more likely to have psychological problems, especially those patients with burns in exposed sites.
Holt et al[22] found that the severity of psychological problems may not only be positively correlated with the severity of injury among burn patients, but may also be associated with pain, burn sites, and age. Due to the anxiety caused by unbearable pain, patients may be at high risk of chronic PTSD, demonstrating the necessity to alleviate patients’ pain during clinical treatment[22].
After an accident, patients and their families need time to adapt to the situation. Patients’ families normally have to work while taking care of the patient, leading to increased mental pressure in patients[23].
Barnett et al[24] established a platform for burn survivors and their families to communicate together about daily care, functional exercises, and mental health, which was helpful in dealing with mental problems after an accident. The mental health of patients’ families is also of great importance, and a number of these patients are children, thus, their rehabilitation may be affected by their parents’ psychological status. Hence, during an investigation of burn patients’ mental health, it is advised to focus on patients’ emotional and anxiety changes and their family, and identify those cases who may require professional assistance and provide them with extra guidance on psychology and behavior, thereby promoting the recovery of children’s mental health indirectly[25].
Additionally, mental disorders are common in burn patients, and may last for a long time. In the present study, according to the patients in Group A, we noted that the recovery of mental health should be carried out in relation to two aspects. The first aspect is to enhance communication and guidance between physicians and patients, certain symptoms such as pain, PTSD, depression, and anxiety may last for a long time, and require early screening and intervention. A mental health test must be provided for patients with these problems as early as possible. Patients may become anxious due to fear of wound dressing; thus, it is essential to be aware of patients’ mental status and communicate with them. Understanding what is going on in their minds may be helpful for effective treatment, and both step-by-step treatment and exercise are advantageous. The second aspect is that numerous studies have been conducted related to the recovery of patients’ mental health, providing family support and social adaptive training.
In conclusion, for patients who were severely burned at exposed sites in a mass burn casualty event, we attempted to repair residual wounds, which included functional joint exercises, anti-scar treatment, and psychotherapy, which could be helpful for late-term burns; however, these four components were not separate but integrated. In the present study, we carried out systematic treatment of 13 patients in Group A, which proved to be more effective compared with patients who did not simultaneously undergo the same treatment. Satisfactory feedback was received from patients and their families, which might assist burn patients to safely return to society.
Face and hands are sites of high exposure in daily life, where burns can accumulate during a mass burn casualty event. In the late-stage of treatment, unhealed residual wounds, unpleasant appearance caused by scar hyperplasia and contracture, limited movements and heavy mental burden commonly exist in patients; however, numerous patients, their families and even surgeons have not paid enough attention to these factors.
In order to improve the clinical effect in burn patients, we summarize the experience of late treatment of severe burns in exposed sites in order to draw the attention of patients, their families and doctors.
To improve the effect of treatment in the late stage of severe burns at exposed sites and to improve patients’ quality of life to achieve an early return to society.
Patients were bathed in Chinese medicine lotion for 20 to 30 min each time, 2 to 3 times a week. The wound was covered with recombinant human epidermal growth factor after each bath; wound secretions were sampled before and one week after bathing to document the healing time and the frequency and duration of relapses, and the VAS was adopted to evaluate pain during wound dressing. Patients started rehabilitative functional exercises of the hands two weeks after skin grafting. Comprehensive rehabilitation plans were made according to the injury severity of patients’ hands: (1) Active and passive finger movements; (2) Scar massage; (3) Chinese herbal bath therapy; and (4) Anti-contracture fixation during motionless periods. Silicone gel ointment, cicatricial paste and elastic clothing were used for long-term anti-cicatricial treatment. Finger massage and mouth opening expansion were used for special areas such as the eyelids and perioral area to combat cicatricial contracture, while DPL and micro-plasma treatment were used for accurate cicatricial therapy to reduce cicatricial formation. A psychological intervention was conducted in patients by improving the living environment, providing humanistic care, enhancing family and social support and establishing a communication-based platform.
We attempted to repair residual wounds using functional joint exercises, anti-scar treatment, and psychotherapy, which could be helpful for late-term burns. In the present study, we performed systematic treatment in 13 patients, we received satisfactory feedback from patients and their family, which might assist burn patients to safely return to society.
We regard residual wound repair, functional joint exercises, systematic anti-scar treatment and psychotherapy as key points in the late-term treatment of burn patients, and these four components formed an integrated treatment.
We used the combination of traditional Chinese and Western medicine to accelerate wound healing, reduce scar formation and relieve patients' pain. With the participation of professional rehabilitation therapists, individualized anti-scar and functional exercise schemes were provided according to the site of the scar, patients’ physical condition, and the nature of the scars. Psychological disorder screening and intervention should be carried out according to the symptoms of burn patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ayatollahi H S-Editor: Gong ZM L-Editor: Webster JR P-Editor: Li JH
| 1. | Hang H, Jianan W, Chunmao H. Experience in managing an urban massive burn incident: The Hangzhou bus attack on 5 July 2014. Burns. 2016;42:169-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Issler-Fisher AC, McKew G, Fisher OM, Harish V, Gottlieb T, Maitz PK. Risk factors for, and the effect of MRSA colonization on the clinical outcomes of severely burnt patients. Burns. 2015;41:1212-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Van Loey NE, Van Son MJ. Psychopathology and psychological problems in patients with burn scars: epidemiology and management. Am J Clin Dermatol. 2003;4:245-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 357] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 4. | Morton R, Gleason O, Yates W. Psychiatric effects of anabolic steroids after burn injuries. Psychosomatics. 2000;41:66-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Wiseman J, Ware RS, Simons M, McPhail S, Kimble R, Dotta A, Tyack Z. Effectiveness of topical silicone gel and pressure garment therapy for burn scar prevention and management in children: a randomized controlled trial. Clin Rehabil. 2020;34:120-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Karlsson M, Steinvall I, Sjöberg F, Olofsson P, Elmasry M. Burn scar outcome at six and 12 months after injury in children with partial thickness scalds: Effects of dressing treatment. Burns. 2020;46:546-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Lyu GZ, Xu LW. [Lay emphasis on early rehabilitation after extensive burn to prevent severe complications in late stage]. Zhonghua Shao Shang Za Zhi. 2017;33:257-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Lv G, Cai L, Yu J. [Effectiveness of traditional Chinese medicine and Western medicine in treating residual deep burn wound]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010;24:937-939. [PubMed] |
| 9. | Akita S, Hayashida K, Takaki S, Kawakami Y, Oyama T, Ohjimi H. The neck burn scar contracture: a concept of effective treatment. Burns Trauma. 2017;5:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Balumuka DD, Galiwango GW, Alenyo R. Recurrence of post burn contractures of the elbow and shoulder joints: experience from a Ugandan hospital. BMC Surg. 2015;15:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Schneider JC, Holavanahalli R, Helm P, O'Neil C, Goldstein R, Kowalske K. Contractures in burn injury part II: investigating joints of the hand. J Burn Care Res. 2008;29:606-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Willyard C. Unlocking the secrets of scar-free skin healing. Nature. 2018;563:S86-S88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 13. | Spronk I, Polinder S, Haagsma JA, Nieuwenhuis M, Pijpe A, van der Vlies CH, Middelkoop E, van Baar ME. Patient-reported scar quality of adults after burn injuries: A five-year multicenter follow-up study. Wound Repair Regen. 2019;27:406-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 14. | Lee SJ, Kim JH, Lee SE, Chung WS, Oh SH, Cho SB. Hypertrophic scarring after burn scar treatment with a 10,600-nm carbon dioxide fractional laser. Dermatol Surg. 2011;37:1168-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Hultman CS, Friedstat JS, Edkins RE. Efficacy of intense pulsed light for the treatment of burn scar dyschromias: a pilot study to assess patient satisfaction, safety, and willingness to pay. Ann Plast Surg. 2015;74 Suppl 4:S204-S208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Kono T, Groff WF, Sakurai H, Yamaki T, Soejima K, Nozaki M. Treatment of traumatic scars using plasma skin regeneration (PSR) system. Lasers Surg Med. 2009;41:128-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Gold MH, Berman B, Clementoni MT, Gauglitz GG, Nahai F, Murcia C. Updated international clinical recommendations on scar management: part 1--evaluating the evidence. Dermatol Surg. 2014;40:817-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 40] [Reference Citation Analysis (0)] |
| 18. | Gold MH, McGuire M, Mustoe TA, Pusic A, Sachdev M, Waibel J, Murcia C; International Advisory Panel on Scar Management. Updated international clinical recommendations on scar management: part 2--algorithms for scar prevention and treatment. Dermatol Surg. 2014;40:825-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 82] [Reference Citation Analysis (0)] |
| 19. | Monstrey S, Middelkoop E, Vranckx JJ, Bassetto F, Ziegler UE, Meaume S, Téot L. Updated scar management practical guidelines: non-invasive and invasive measures. J Plast Reconstr Aesthet Surg. 2014;67:1017-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 220] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 20. | Idrees S, Gul I, Faize FA, Akhtar M. Psychological Reactions, Social Support, and Coping Styles in Pakistani Female Burn Survivors. J Burn Care Res. 2017;38:e934-e943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Pallua N, Künsebeck HW, Noah EM. Psychosocial adjustments 5 years after burn injury. Burns. 2003;29:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Holt R, Kornhaber R, Kwiet J, Rogers V, Shaw J, Law J, Proctor MT, Vandervord J, Streimer J, Visentin D, Cleary M, McLean L. Insecure adult attachment style is associated with elevated psychological symptoms in early adjustment to severe burn: A cross-sectional study. Burns. 2019;45:1359-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Wiechman S, Saxe G, Fauerbach JA. Psychological Outcomes Following Burn Injuries. J Burn Care Res. 2017;38:e629-e631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Barnett BS, Mulenga M, Kiser MM, Charles AG. Qualitative analysis of a psychological supportive counseling group for burn survivors and families in Malawi. Burns. 2017;43:602-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Brown EA, De Young A, Kimble R, Kenardy J. Impact of Parental Acute Psychological Distress on Young Child Pain-Related Behavior Through Differences in Parenting Behavior During Pediatric Burn Wound Care. J Clin Psychol Med Settings. 2019;26:516-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |