Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3503
Peer-review started: May 8, 2020
First decision: June 2, 2020
Revised: June 3, 2020
Accepted: July 14, 2020
Article in press: July 14, 2020
Published online: August 26, 2020
Processing time: 106 Days and 22.7 Hours
Repeated endoscopic probe dilatation is the most preferred treatment for esophageal stenosis which may cause high levels of symptom distress in the patient's home rehabilitation stage.
To explore the changes in the symptom distress level and its correlation with the dilation effect in patients with esophageal carcinoma undergoing repeated dilations for lumen stenosis.
The difference (R2-R1) between the diameter of the esophageal stenosis opening (R1) of the patients before dilation (R1) and after dilation (R2) was calculated to describe the extent and expansion of the esophageal stenosis before and after dilation. The M.D. Anderson Symptom Inventory was used to describe the symptom distress level of patients with dilation intermittence during their stay at home and to explore the correlation between the dilation effect and symptom distress level.
The diameter of the esophagus (R1) increased before each dilation in patients undergoing esophageal dilation (P < 0.05). The diameter (R2) increased after dilation (P < 0.05); the dilation effect (R2-R1) decreased with the number of dilations (P < 0.05). The total symptom distress score significantly increased with the number of dilations (P < 0.05). The symptom distress scores of the patients were negatively correlated (P < 0.05) with the previous dilation effect (R2-R1) and the esophageal diameter (R2) after the previous dilation. After the 1st to 4th dilations, the patient's symptom distress score was negatively correlated with the esophageal diameter (R12) before the next dilation, while there was no significant correlation (P > 0.05) with the other dilations.
In patients who have undergone repeated dilations, better effect stands for lower symptom distress level and the increase in symptom distress has a prompt effect on the severity of the next occurrence of restenosis.
Core tip: Esophageal carcinoma ranks 6th in terms of the associated mortality rate and the incidence of complications after standardized comprehensive treatment of esophageal carcinoma is between 12.3% and 38%. Repeated endoscopic probe dilatation is the most preferred treatment for esophageal stenosis, which may cause high levels of symptom distress in the patient's home rehabilitation stage. This study explored the changes in the symptom distress level and its correlation with the dilation effect in patients with esophageal carcinoma undergoing repeated dilations for lumen stenosis. Based on these data, we can find the changes in the symptom distress level and its correlation with the dilation effect, which can contribute to patients’ symptoms management.
- Citation: Liu L, Liu QW, Wu XD, Liu SY, Cao HJ, Hong YT, Qin HY. Follow-up study on symptom distress in esophageal cancer patients undergoing repeated dilation. World J Clin Cases 2020; 8(16): 3503-3514
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3503.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3503
Esophageal carcinoma ranks 8th worldwide among other cancers in terms of incidence and 6th in terms of the associated mortality rate. The incidence rate of esophageal carcinoma in China is increasing, showing obvious regional differences[1-4]. The incidence of complications after standardized comprehensive treatment of esophageal carcinoma is between 12.3% and 38%, which is significantly higher than that of other digestive tract cancers[3-6]. Esophageal stenosis is one of the most common complications due to the particularity of the esophageal wall anatomy[7,8]. The causes of esophageal stricture include scars from anastomotic stoma, rigid mucosa after radiotherapy, and hyperplasia after endoscopic annular mucosal dissection[9]. According to the severity, esophageal stenosis can be classified as severe stenosis (diameter [R] = 0.10-0.39 cm), moderate stenosis (R = 0.40-0.69 cm), or mild stenosis (R = 0.70-1.00 cm). Patients often feel that they are unable to eat when the esophagus is mildly to moderately narrow[10].
Surgery, stent implantation, and endoscopic dilation are common methods for the treatment of esophageal stenosis. However, esophageal stenosis can easily relapse and requires repeated treatments. Repeated surgical operations for esophageal stenosis are traumatic and are generally rarely accepted by patients. The time required for stent placement is short, the cost is high, and restenosis can easily occur. Therefore, repeated endoscopic probe dilatation is still the most preferred treatment for esophageal stenosis[11]. Dilation for esophageal stenosis relies on the mechanical destruction of scar tissue by the dilation probe to dilate the stenosis. Patients with esophageal stenosis usually undergo dilation once every 2-4 wk. By comparing the diameter of the esophagus before and after dilation and food intake, we can determine whether the dilation is effective. If the dilation is effective and the esophagus is no longer narrow, complete remission is considered to have occurred[12]. Studies have shown that to achieve complete remission, approximately 41% of patients need dilations three times, approximately 20% need dilations three to five times, approximately 23% need dilations 5-10 times, and 12% need dilations more than 10 times[13]. During the dilation process, the endoscope and the dilation probe repeatedly enter and exit the esophagus entrance. Tearing and bleeding of the pharynx, pyriform fossa, and esophagus mucosa to varying degrees are inevitable, and even perforation occurs[14]. In addition, endoscopists generally do not recommend sedation or anesthesia for dilation so that they can better observe the presence or absence of complications, such as perforation, through the patient’s response during the operation. Patients usually feel severe pain and suffer great physical and mental pain during the operation process. Short-term treatment often causes high levels of symptom distress in the patient's home rehabilitation stage. Symptom distress refers to "the degree of distress caused by specific symptoms experienced by the patient" and can also be defined as "physical or mental pain or suffering caused by the occurrence of symptoms and/or emotional changes in the patient"[15]. Among cancer patients, an average of 35.1% have symptoms of varying degrees[16]. There are many research studies on symptom distress in tumor patients at home and abroad, but for esophageal carcinoma patients who need repeated esophageal dilation, the symptom distress levels and changes have not been mentioned in any research studies.
This study aimed to investigate the changes in the esophageal diameter and symptom distress level in patients during the interval of dilation as the number of dilations increased to explore the dilation effect and its correlation with symptom distress level. The results of this study will be helpful for clinical nursing staff to understand the impact of repeated invasive diagnoses and treatments in patients during the home rehabilitation period and to further understand the problems and needs of tumor patients in the disease treatment and rehabilitation stages. Moreover, the results from the study will provide a basis for the design and implementation of symptom management programs, help relieve pain caused by symptom distress, and help improve the quality of life of patients.
In this study, a convenient sampling method was used to identify patients who were diagnosed with esophageal carcinoma by a pathological examination from January 1, 2018 to October 31, 2019 and suffered from esophageal stenosis after operation, radiotherapy and chemotherapy, comprehensive treatment, or endoscopic resection. After an evaluation was performed by endoscopic physicians, patients underwent endoscopic dilation for esophageal stenosis at the Sun Yat-sen University Cancer Center. The inclusion criteria were as follows: Aged 18-75 years, completed primary school or a higher level of education, diagnosed with the disease condition, provided contact information, and agreed to participate in follow-ups. The exclusion criteria were as follows: History of mental illness or dyslexia, distant metastasis, history of other malignant tumors caused by esophageal carcinoma accidents, and serious complications. If esophageal stenosis was found during operation and the diameter was less than < 0.1 cm, it was difficult to pass the guide wire. If a patient could not tolerate the operation, did not participate in the follow-up, or exhibited recurrence, metastasis, complications of other tumors, or changes in other treatment methods during the follow-up period, the patient was excluded. A total of 105 patients were included in this study, including 64 males and 41 females, aged 43-72 years, with an average age of 51.48 ± 4.15 years. Sixteen (15.24%) patients suffered from esophageal stenosis after surgical treatment, 24 (22.86%) suffered from stenosis after radiotherapy and chemotherapy, 54 (51.43%) suffered from stenosis after comprehensive treatment, 8 (7.62%) suffered from stenosis after endoscopic mucosal stripping, and 3 (2.86%) suffered from other conditions (immunotherapy, etc.). In this study, there were no severe complications, such as perforation during expansion.
In this study, endoscopic probe dilatation for esophageal stenosis was performed as follows: An OLYMPUS GIF-XP260N ultrafine transnasal gastroscope was used according to the gastroscope examination routine, the gastroscope was inserted through the oral cavity under the awake state, the esophageal stenosis was observed and recorded, and a silica gel probe dilator was selected according to the stenosis severity. The sizes of the dilators included 0.5 cm, 0.7 cm, 0.9 cm, 1.1 cm, 1.28 cm, 1.4 cm, 1.5 cm, and 1.6 cm. First, the metal guide wire was introduced from the working channel of the gastroscope and passed through the narrow part. The guide wire was retained, and the ultrafine gastroscope was pulled out. The dilation was slowly inserted along the guide wire for mechanical dilation for 2 min at each dilation pass. After less than three-degree dilations, the dilation probe and the guide wire were withdrawn together, and then the gastroscope was inserted again to assess the dilation effect of the narrow part. Patients with esophageal stenosis underwent dilation every 3 wk until complete remission.
Endoscopic dilation of patient file: We designed an “Endoscopic Dilation of Patient File” for each esophageal cancer patient after surgery, radiotherapy and chemotherapy, or comprehensive treatment; the file included demographic characteristics, disease treatment characteristics, esophageal stenosis information, including the diameter of esophageal stenosis opening (R1) before each dilatation, registration of the operation process, and the diameter (R2) of the esophageal stenosis opening of the patient after expansion. Finally, (R2-R1) was calculated to describe the current expansion effect.
M.D. Anderson Symptom Inventory: The M.D. Anderson Symptom Inventory (MDASI) was first developed by American Scholar Cleeland in 2000[17]. The original version includes two parts, the symptom subscale and the distress subscale. There are 13 items in the MDASI. The physical and psychological symptoms in the past 24 h are evaluated. There are six items in the distress subscale that are used to evaluate the effect of the symptoms listed in the symptom subscale, and the items concern self-care activities, emotions, work or housework, interpersonal relationships with others, walking, and enjoying daily life. Each item was scored on an 11-point scale from 0 (no points at all) to 10 (the highest level of severity). Since an esophageal carcinoma-specific symptom distress inventory has not yet been developed, this study supplemented the Chinese version of the MDASI with the specific symptoms of esophageal stenosis patients after receiving treatment, namely, dysphagia, reflux, choking cough, weight loss, and hoarseness. Twenty patients were selected for the preinvestigation to assess internal consistency. After testing, the Cronbach's α coefficient of the complete inventory, the first part of the original inventory, and the summed items were 0.837, 0.799, and 0.734, respectively. According to the evaluation of five experts from the Thoracic Department, Department of Endoscopy, and School of Nursing of Sun Yat-sen University Cancer Center, the supplementary items have good content validity.
During the interval between two dilations, i.e., the 10th day after each dilation, the MDASI was administered to evaluate and describe the symptom distress level of patients with different dilations, and the changes were described considering the time effect. Then, we analyzed the correlation between the symptom distress score and esophageal diameter (R2) after the previous dilation, esophageal diameter (R1) before the next dilation, and the previous dilation effect (R2-R1).
With the consent of the relevant departments of the hospital where the research was being carried out, the data were collected at the endoscopy center and thoracic endoscopy room of Sun Yat-sen University Cancer Center.
Esophageal carcinoma patients who were diagnosed with esophageal stenosis by endoscopic physicians and were planning to undergo dilation of esophageal stenosis repeatedly were selected. The patients received dilation for esophageal stenosis once every 3 wk. The researchers conducted a longitudinal follow-up investigation from the beginning of the patient's first dilation operation until the patient achieved a marked effect and terminated treatment. The patients who refused to participate in the follow-up or could not participate in the follow-up for other reasons, such as a change in the treatment method, were recorded as patients lost to follow-up.
The participants completed the assessments anonymously and kept the condition confidential. The data obtained were only used for this study and not for profit.
The researchers provided uniform training and instruction to the data collectors. A questionnaire survey was conducted by adopting the “Endoscopic Dilation of Patient Files” and MDASI.
The diameter of the esophageal stenosis before and after dilation, the amount of bleeding, and the pain score of patients during dilation were recorded by the data collector during dilation. After the dilation was completed, the patient/family member completed the “Endoscopic Dilation of Patient File” independently, and the data collector gave unified guidance and collected the data on site to ensure that there were no missing items.
One week after the patient’s dilation, the patient was asked to return an MDASI survey to the hospital. The patients who were able to return to the hospital were reminded by the data investigator in advance by phone after they provided consent. The patients who were unable to return to the hospital were administered the questionnaire by the data investigator on site to ensure that there were no missing items in the questionnaire. The patients who could complete the investigation were given exquisite gifts and publicity materials by the project team to improve patient compliance.
The secretary was trained to properly arrange the data, sort the patients’ “Endoscopic Dilation of Patient Files”, and manage them properly.
SPSS13.0 was used for data analyses. Frequencies, standard deviations, percentages, and means were used to describe the patient’s general information, disease-related data, expansion-related records, and the total score and individual scores of each symptom of each expansion interval.
ANOVA was used to compare the scores corresponding to R1, R2, R12, and R2-R1 with symptom distress during the interval of dilation and to establish a linear model to explore the changes and time effects.
Pearson correlation analysis was used to analyze the correlation between the symptom distress score during each dilation interval and the esophageal diameter (R2) after the previous dilation, the esophageal diameter (R12) before the next dilation, and the effect of the previous dilation (R2-R1).
In this study, only three (2.86%) patients achieved a marked effect after one dilation, six achieved a marked effect after two dilations, and 40.95% (43 patients) achieved a marked effect after three dilations, which accounted for the largest proportion. Forty (38.10%) patients needed more than four dilations, among whom 13 (16.19%) failed to achieve significant effects after six dilations. The median number of dilations was three (Table 1)
| Achieved marked effect | Cumulative percentage | Did not achieve significant results | |||
| n | Percentage (%) | n | Percentage (%) | ||
| 1 time | 3 | 2.86 | 2.86 | 102 | 97.14 |
| 2 times | 6 | 5.88 | 8.57 | 96 | 94.12 |
| 3 times | 43 | 44.79 | 49.52 | 53 | 55.21 |
| 4 times | 5 | 9.43 | 54.29 | 48 | 90.57 |
| 5 times | 18 | 37.50 | 71.43 | 30 | 62.50 |
| 6 times | 17 | 56.67 | 87.62 | 13 | 43.33 |
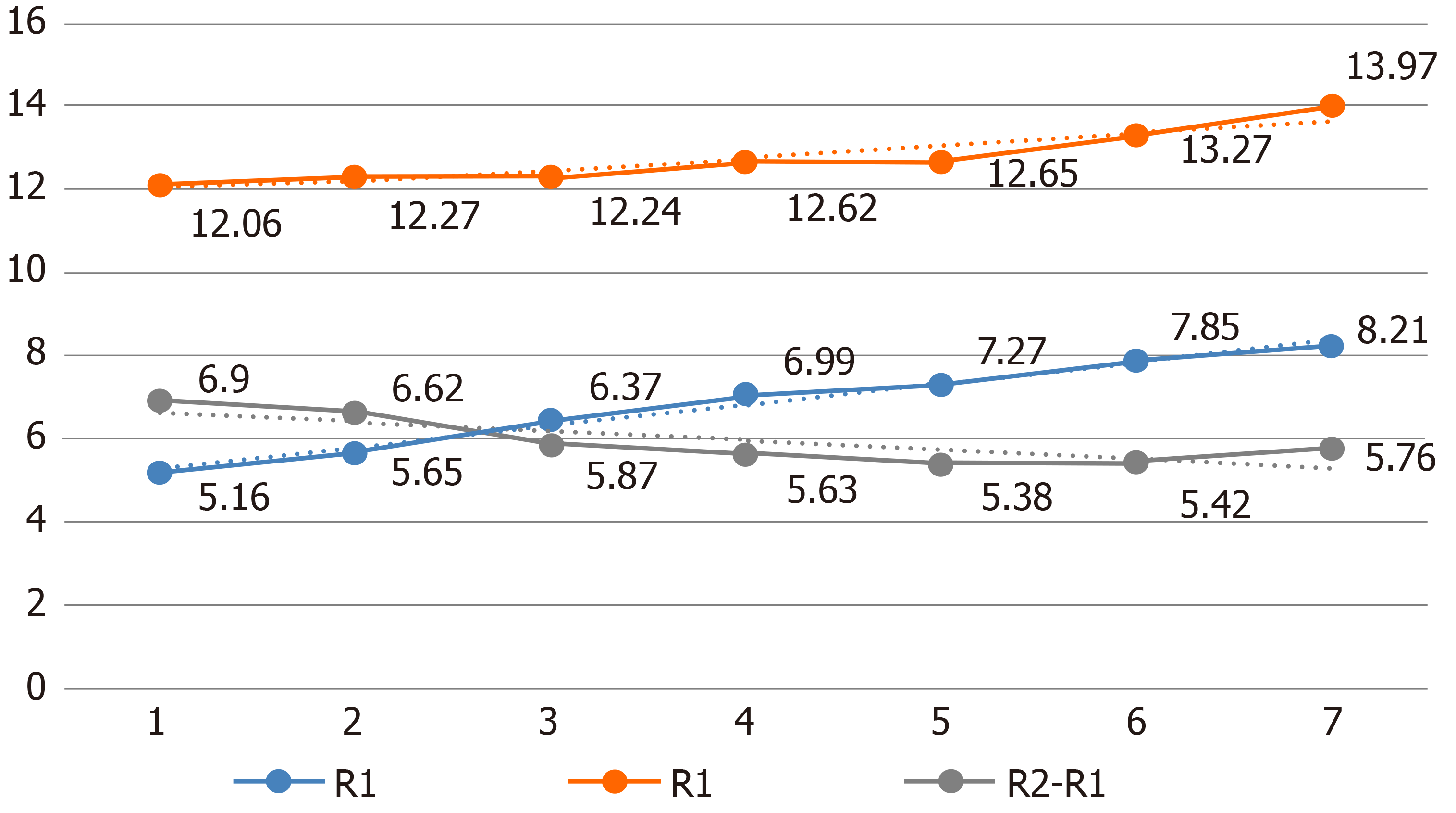
As the number of dilations increased, the esophageal diameter (R1) increased (P < 0.05) when the patient was recanalized, and the degree of stenosis improved from moderate stenosis (R11 = 5.16 ± 1.67 mm) to mild stenosis (R17 = 8.21 ± 3.41 mm). After dilation, the diameter (R2) increased (P < 0.05) and reached a level of no stenosis (> 10 mm) at the end of each dilation. The amount by which the esophageal diameter increased (R2-R1) gradually decreased with increasing dilation times, and the difference was statistically significant (P < 0.05), as shown in Table 2 and Figure 1.
| 1st time (n = 105) | 2nd time (n = 102) | 3rd time (n = 96) | 4th time (n = 53) | 5th time (n = 48) | 6th time (n = 30) | 7th time (n = 13) | F/P value | |
| R1 (mm) | 5.16 ± 1.67 | 5.65 ± 0.99 | 6.37 ± 0.67 | 6.99 ± 1.18 | 7.27 ± 2.10 | 7.85 ± 2.74 | 8.21 ± 3.41 | 34.71/ |
| R2 (mm) | 12.06 ± 2.92 | 12.27 ± 2.13 | 12.24 ± 1.69 | 12.62 ± 1.44 | 12.65 ± 2.39 | 13.27 ± 1.63 | 13.97 ± 2.11 | 16.95/ |
| R2-R1 (mm) | 6.90 ± 1.03 | 6.62 ± 0.99 | 5.87 ± 1.54 | 5.63 ± 0.89 | 5.38 ± 1.41 | 5.42 ± 1.10 | 5.76 ± 0.84 | 3.29/0.00a |
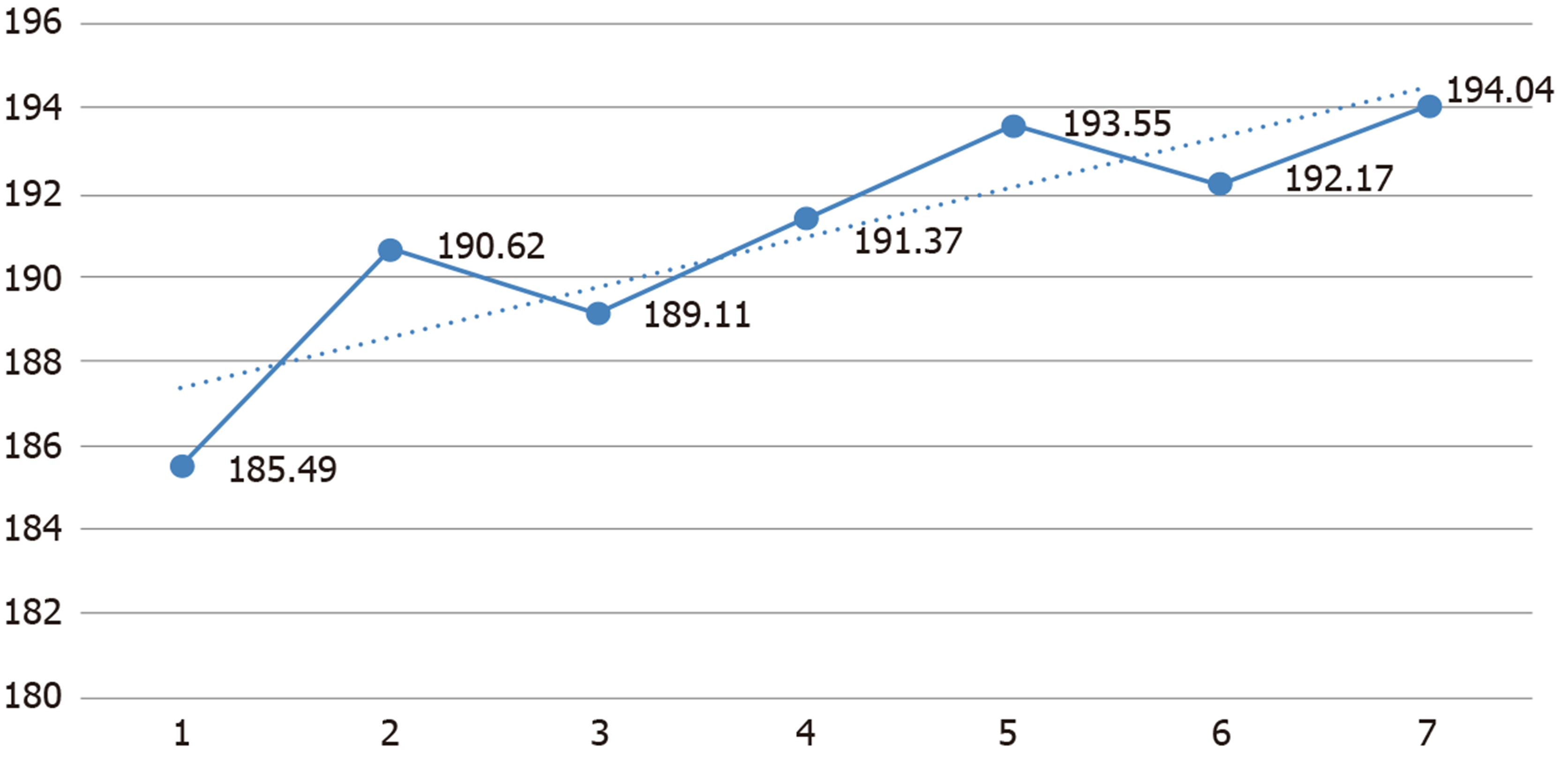
The total symptom distress score in patients with esophageal carcinoma who underwent repeated esophageal stenosis and dilation was significantly increased with the number of dilations (P < 0.05). The symptom dimension and distress dimension scores were significantly increased with the number of dilations (P < 0.05), as shown in Table 3 and Figure 2. Dysphagia and pain were the most common symptoms after the 1st to 4th dilations. Sadness, fatigue, and weight loss were the most common symptoms after the 5th to 7th dilations. In the investigation of patients' distress after each dilation, the most common types of distress were work-related, emotional, general activity-related, and general life-related distress (Table 4 and Table 5).
| After the 1st dilation (n = 105) | After the 2nd dilation (n = 102) | After the 3rd dilation (n = 96) | After the 4th dilation (n = 53) | After the 5th dilation (n = 48) | After the 6th dilation (n = 30) | After the 7th dilation (n = 13) | F/P value | |
| Total score | 185.49 ± 15.04 | 190.62 ± 14.83 | 189.11 ± 12.76 | 191.37 ± 14.20 | 193.55 ± 12.37 | 192.17 ± 15.10 | 194.04 ± 11.21 | 38.97/ |
| Symptom dimension | 106.37 ± 8.79 | 111.08 ± 5.99 | 108.39 ± 4.11 | 110.35 ± 8.37 | 114.70 ± 6.81 | 110.24 ± 7.28 | 112.33 ± 9.10 | 14.24/ |
| Distress dimension | 79.12 ± 2.66 | 79.54 ± 1.09 | 80.72 ± 1.37 | 81.02 ± 1.57 | 78.85 ± 1.98 | 81.93 ± 2.19 | 81.71 ± 6.68 | 17.64/ |
| After the 1st dilation (n = 105) | After the 2nd dilation (n = 102) | After the 3rd dilation (n = 96) | After the 4th dilation (n = 53) | After the 5th dilation (n = 48) | After the 6th dilation (n = 30) | After the 7th dilation (n = 13) | ||||||||||||||
| Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD |
| Dysphagia | 63.2 | 6.4 ± 1.8 | Dysphagia | 58.9 | 6.2 ± 1.6 | Dysphagia | 69.1 | 6.7 ± 2.4 | Distress | 78.4 | 7.3 ± 2.6 | Sadness | 77.4 | 7.5 ± 3.1 | Cough | 78.1 | 7.3 ± 1.9 | Sadness | 79.6 | 7.9 ± 2.8 |
| Pain | 61.1 | 5.8 ± 2.3 | Cough | 56.6 | 6.1 ± 2.3 | Weight loss | 69.3 | 7.1 ± 1.8 | Dysphagia | 70.6 | 6.9 ± 3.1 | Cough | 73.9 | 6.6 ± 2.4 | Sadness | 77.5 | 7.3 ± 2.6 | Fatigue | 70 | 7.1 ± 1.7 |
| Distress | 57.3 | 6.1 ± 2.1 | Pain | 51.2 | 6.6 ± 1.4 | Pain | 67.9 | 6.8 ± 2.1 | Fatigue | 68.3 | 7.6 ± 2.2 | Weight loss | 70.1 | 7.1 ± 3.6 | Fatigue | 73.1 | 7.6 ± 2.7 | Weight loss | 69.5 | 6.9 ± 2.4 |
| After the 1st dilation (n = 105) | After the 2nd dilation (n = 102) | After the 3rd dilation (n = 96) | After the 4th dilation (n = 53) | After the 5th dilation (n = 48) | After the 6th dilation (n = 30) | After the 7th dilation (n = 13) | ||||||||||||||
| Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD | Item | % | mean ± SD |
| Work | 49.3 | 4.7 ± 1.1 | Work | 56.7 | 4.8 ± 1.4 | Emotion | 56.2 | 4.7 ± 2.3 | Emotion | 57.3 | 5.1 ± 2.4 | Life fun | 49.6 | 4.7 ± 2.2 | Life fun | 51.4 | 5.2 ± 3.0 | General activities | 54.8 | 5.2 ± 2.4 |
| Emotion | 49 | 4.2 ± 1.2 | Emotion | 52.5 | 4.6 ± 2.2 | General activities | 40.6 | 4.2 ± 1.6 | Life fun | 40.7 | 4.5 ± 1.8 | 2 Emotion | 48.1 | 4.9 ± 1.3 | General activities | 37.2 | 5.0 ± 2.9 | Emotion | 43.7 | 5.3 ± 1.7 |
| General activities | 32.1 | 3.8 ± 0.9 | Life fun | 50.9 | 3.9 ± 1.7 | Life fun | 37.3 | 4.1 ± 2.0 | General activities | 40.7 | 4.1 ± 2.3 | 3 General activities | 31.7 | 4.9 ± 2.4 | Emotion | 37 | 4.9 ± 1.8 | Life fun | 42.9 | 3.9 ± 1.1 |
In the correlation scores between symptom distress and dilation effect of esophageal carcinoma patients who repeatedly undergo dilation for esophageal stenosis, the symptom distress scores of the patients were negatively (P < 0.05) correlated with the previous dilation effect (R2-R1) and the esophageal diameter (R2) after the previous dilation. After the 1st to 4th dilations, the patient’s symptom distress score was negatively correlated with the esophageal diameter (R12) before the next dilation, while there was no significant correlation (P > 0.05) with the other dilations (Table 6 and Table 7).
| Symptom distress after the 1st dilation (n = 105) | Symptom distress after the 2nd dilation (n = 102) | Symptom distress after the 3rd dilation (n = 96) | Symptom distress after the 4th dilation (n = 53) | Symptom distress after the 5th dilation (n = 48) | Symptom distress after the 6th dilation (n = 30) | Symptom distress after the 7th dilation (n = 13) | |
| R2-R1 | -0.356a | -0.332a | -0.665a | -0.157a | -0.675a | -0.293b | -0.273a |
| R2 | -0.185a | -0.257a | -0.392a | -0.366a | -0.119 | -0.665a | -0.227a |
| Symptom distress after the 1st dilation | Symptom distress after the 2nd dilation | Symptom distress after the 3rd dilation | Symptom distress after the 4th dilation | Symptom distress after the 5th dilation | Symptom distress after the 6th dilation | |
| R12 | 0.304b | -0.306a | -0.311b | -0.565b | -0.198 | -0.278 |
In patients with esophageal stenosis, restenosis can easily occur. In this study, only three (2.86%) patients achieved a remarkable effect after one dilation operation. In total, 87.62% (102 cases) of the patients received four dilation operations to achieve complete remission of symptoms. Among them, more than half (57 cases, 54.29%) of the patients achieved a marked effect within four times, and 17 (16.19%) patients still had no marked effect after seven dilations. In clinical practice, there are also patients with such refractory esophageal stenosis. Repeated mechanical dilations cannot achieve the goal of a complete resolution of symptoms. The treatment outcome may be related to the patient's individual anatomical characteristics, disease pathogenesis, treatment mechanism, or other factors. Additional discussion on the mechanism is needed with the support of clinical experiments[18].
The degree of stenosis usually reaches the level of moderate stenosis (R11 = 5.16 ± 1.67 mm) when patients seek medical treatment for the first time, which seriously affects patients' intake of food and water. Adequate nutritional support is an important aspect to ensure proper postoperative rehabilitation of esophageal carcinoma patients[19]. Therefore, esophageal stenosis not only seriously affects the quality of life of patients but also affects the rehabilitation outcome and disease prognosis of patients. After endoscopic treatment of esophageal stenosis, the esophageal diameter of the patient can reach a nonstenosis state (> 10 mm) immediately, ensuring that the patient can obtain timely nutritional support after dilation. Due to the anatomical features of the esophagus, patients with an immediate effect of dilation still have the possibility of restenosis, so it is necessary to perform dilation again when food intake is affected after restenosis. In this study, the severity of esophageal restenosis (R1) of the patients after treatment was somewhat less than that before treatment. Before the 7th dilation, the average severity of esophageal stenosis was mild stenosis (R17 = 6.31 ± 3.41 mm). This result indicates that dilation for esophageal stenosis can continuously improve the severity of esophageal stenosis in patients and alleviate the severity of restenosis. The diameter of the esophagus (R2) increased after dilation, but judging from the trend chart, the growth trend of R2 was moderate. As the number of dilations increased, the esophageal diameter difference (R2-R1) before and after dilation decreased compared with that before dilation. The marked reduction in the effect of dilation on esophageal stenosis may be related to the reduction in elasticity and toughness of the esophageal wall caused by the disease characteristics of some patients, repeated mechanical injury-hyperplasia trauma processes, and limited expansion effects.
The symptom distress levels of esophageal carcinoma patients who have undergone repeated dilation of esophageal stenosis increase with the number of dilations. In this study, more than half (57 cases, 54.29%) of the patients were able to achieve a marked effect within four times, three achieved a marked effect after one dilation operation, and six achieved a marked effect after two dilation operations. Therefore, for these patients, the curative effect of dilation was remarkable and timely, and the experience of physical symptoms, such as dysphagia and pain, and the experience of distress in aspects such as work, emotions, and life enjoyment were relatively low. Moreover, due to an obvious relief in esophageal stenosis and lower levels of distress in the patients’ life, a lower number of dilations corresponded to a lower average level of disease uncertainty during the patient's stay at home. Forty patients (38.10%) who needed more than four dilations, 17 (16.19%) of them failed to achieve significant effects after seven dilations. For these patients, repeated and continuous symptoms, such as pain, hemorrhage, and fear, caused by treatment methods leading to multiple mechanical injuries last for a long time. Repeated esophageal narrowing affects the intake of food and water for the patients, and the inability to eat food leads to difficulties in the life of the patients during the recovery period, which further affects the symptom distress level of the patients at home.
In terms of the incidence of symptoms, dysphagia and pain were among the three most common symptoms after the first to third dilations, while after the fourth to seventh dilations, sadness, fatigue, weakness, weight loss, and cough were more frequent. The results show that when patients experience fewer dilations, swallowing obstruction caused by the disease itself and pain caused by dilation therapy are more significant. With an increase in the number of dilations, the severity of esophageal restenosis in patients decreases, dysphagia improves, and patients experience less pain and other symptoms. The incidence rate of the corresponding symptoms is significantly reduced compared with those of other symptoms. However, the cost associated with patients' diseases and treatment for patients is increasingly prominent. Among the symptoms experienced by patients, weight loss and fatigue are very important. Repeated treatment often makes patients feel uncertain about the treatment and thus feel sad. Repeated mechanical injuries may cause damage to the mucosa, muscles, and nerves in the esophageal wall, and patients with more dilations are more likely to choke.
Judging from the incidence rate of various distress items, diseases and treatments continue to negatively affect patients’ emotions, enjoyment in life, and general activities. During the first and second dilations, distress from the disease and treatment most affected the patient’s work, which may be related to the fact that some patients felt more strongly that the disease caused them to stop/give up their work at the early stage of stenosis.
Correlation between symptom distress and dilation effect (R2-R1) and esophageal diameter (R2) after the previous dilation in patients undergoing esophageal stenosis dilation: In the correlation scores between symptom distress and the dilation effect of esophageal cancer patients who underwent repeated dilation of esophageal stenosis, the symptom distress scores of the patients were negatively (P < 0.05) correlated with the previous dilation effect (R2-R1) and the esophageal diameter (R2) after the previous dilation. The better the patient’s current expansion effect, the greater the difference in (R2-R1), and the lower the symptom distress level during the patient's stay at home. Endoscopic esophageal stenosis dilation can immediately enlarge the esophageal diameter. Therefore, patients can eat a warm and cool liquid diet 2 h after dilation. The improvement in a patient’s ability to feed himself or herself can greatly reduce the symptoms and severity of dysphagia, eating obstruction, and similar issues. Therefore, the better the dilation effect, the larger the diameter of the esophagus, the lower the symptom distress score, and the lower the level of symptom distress during the patient's stay at home.
Correlation between symptom distress and esophageal restenosis degree (R12) in patients undergoing esophageal stenosis dilatation: After the 1st to 4th dilations, the patient’s symptom distress score was negatively correlated with the esophageal diameter (R12) before the next dilation, while there was no significant correlation (P > 0.05) with the other dilations. During the home rehabilitation period, the higher the symptom distress level, i.e., the more severe the symptoms experienced by the patient, such as dysphagia and eating obstruction, the higher the level of distress in the patient’s life. This association may be related to the presence of the patient's esophageal restenosis during his or her stay at home, or it may be related to the patient’s personal emotional characteristics. This study indicated that the higher the symptom distress level of the patient before the previous dilation, the higher the esophageal restenosis degree before the next dilation, i.e., R12 is smaller. It was shown that the symptom distress level of patients in this study is obviously related to the progression of esophageal restenosis, suggesting that nursing staff should pay close attention to the symptom distress level of patients during home rehabilitation and suggest patients to receive endoscopic reexaminations in a timely manner. If esophageal restenosis has occurred, it is recommended that the next esophageal dilation be performed at an earlier time.
In conclusion, for esophageal carcinoma patients who have undergone repeated dilation of esophageal stenosis, the dilation effect and the diameter of the esophagus after dilation are closely related to the degree of symptom distress during the patient’s stay at home. The higher the degree of symptom perplexity, the more obvious the degree of esophageal stenosis in patients who underwent dilation in the early stage. As the number of dilations increases, the effect of dilations decreases significantly, and the level of symptom distress during the patient’s stay at home also increases. The results of this study suggested that the formulation of intraoperative nursing programs and the improvement in patients’ adherence can yield a better dilatation effect, which can help reduce the level of symptoms and distress in patients during their stay at home. Moreover, strict follow-ups and home symptom management are helpful for timely assessments of the patient’s symptom distress level, indirect assessments of the degree of esophageal restenosis before the next dilation, and timely suggestions for the patient’s dilation schedule. For patients who have failed to achieve the ideal effect after repeated dilations for esophageal stenosis, especially for patients who have undergone dilation more than four times, nursing workers should pay more attention to the level of symptom distress and strengthen symptom management.
There are many research studies on symptom distress in tumor patients at home and abroad, but for esophageal carcinoma patients who need repeated esophageal dilation, the symptom distress levels and changes have not been mentioned in any research studies.
The results can be used as a basis for symptom management.
This study aimed to investigate the changes in the esophageal diameter and symptom distress level in patients during the interval of dilation as the number of dilations increases to explore the dilation effect and its correlation with symptom distress level.
The difference between the diameter of the esophageal stenosis opening of the patients before dilation and the diameter of the esophageal stenosis opening after dilation was calculated to describe the extent and expansion of the esophageal stenosis before and after dilation.
The diameter of the esophagus (R1) increased before each dilation in patients undergoing esophageal dilation. The diameter (R2) increased after dilation, and the dilation effect (R2-R1) decreased with the number of dilations. The total symptom distress score increased with the number of dilations, and the difference was statistically significant. After the 1st to 4th dilations, the patient's symptom distress score was negatively correlated with the esophageal diameter (R12) before the next dilation, while there was no significant correlation with the other dilations.
For esophageal carcinoma patients who have undergone repeated dilation of esophageal stenosis, the dilation effect and the diameter of the esophagus after dilation are closely related to the degree of symptom distress during the patient's stay at home.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Campanale M, Orbell JH S-Editor: Wang JL L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Li S, Chung DC, Mullen JT. Screening high-risk populations for esophageal and gastric cancer. J Surg Oncol. 2019;120:831-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Modesto A, Carrère N, Guimbaud R, Rives M, Deutsch É, Quéro L, Créhange G. [Definitive or neo-adjuvant chemoradiation in esophageal carcinoma?]. Cancer Radiother. 2019;23:716-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Chen WQ, Zheng RS, Zhang SW, Zeng HM, Zou XN, He J. Report of Incidence and Mortality of Malignant Tumors in China in 2013. Zhongguo Zhongliu. 2017;29:1-7. [DOI] [Full Text] |
| 4. | Zheng RS, Sun KX, Zhang SW, Zeng HM, Zou XN, Chen R, Gu XY, Wei WQ, He J. Report of Epidemiology of Malignant Tumors in China in 2015. Zhonghua Zhongliu Zazhi. 2019;41:19-28. [RCA] [DOI] [Full Text] [Cited by in RCA: 276] [Reference Citation Analysis (0)] |
| 5. | Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11444] [Cited by in RCA: 13196] [Article Influence: 1466.2] [Reference Citation Analysis (3)] |
| 6. | Li DJ, Liang D, Jin J, Shi J, Qu F, He YT. Epidemiological Trend of Malignant Tumors in Upper Digestive Tract. Zhongliu Yufang Yu Zhiliao. 2018;31:62-68. [DOI] [Full Text] |
| 7. | Yoshida N, Morito A, Nagai Y, Baba Y, Miyamoto Y, Iwagami S, Iwatsuki M, Hiyoshi Y, Eto K, Ishimoto T, Kiyozumi Y, Yagi T, Nomoto D, Akiyama T, Toihata T, Imamura Y, Watanabe M, Baba H. Clinical Importance of Sputum in the Respiratory Tract as a Predictive Marker of Postoperative Morbidity After Esophagectomy for Esophageal Cancer. Ann Surg Oncol. 2019;26:2580-2586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Lin YH, Ou CY, Lee WT, Lee Y, Chang T, Yen YT. Treatment outcomes for one-stage concurrent surgical resection and reconstruction of synchronous esophageal and head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2019;276:2929-2940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Sunde B, Klevebro F, Johar A, Johnsen G, Jacobsen AB, Glenjen NI, Friesland S, Lindblad M, Ajengui A, Lundell L, Lagergren P, Nilsson M. Health-related quality of life in a randomized trial of neoadjuvant chemotherapy or chemoradiotherapy plus surgery in patients with oesophageal cancer (NeoRes trial). Br J Surg. 2019;106:1452-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Deng C, Zou XP. Prevention of Esophageal Stenosis after Endoscopic Submucosal Stripping. Guoji Xiaohuabing Zazhi. 2015;53:20-24. [DOI] [Full Text] |
| 11. | Song JU, Park HY, Kim H, Jeon K, Um SW, Koh WJ, Suh GY, Chung MP, Kwon OJ. Prognostic factors for bronchoscopic intervention in advanced lung or esophageal cancer patients with malignant airway obstruction. Ann Thorac Med. 2013;8:86-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Zu Y, Narayanan SS, Kim YC, Nayak K, Bronson-Lowe C, Villegas B, Ouyoung M, Sinha UK. Evaluation of swallow function after tongue cancer treatment using real-time magnetic resonance imaging: a pilot study. JAMA Otolaryngol Head Neck Surg. 2013;139:1312-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Spaander MC, Baron TH, Siersema PD, Fuccio L, Schumacher B, Escorsell À, Garcia-Pagán JC, Dumonceau JM, Conio M, de Ceglie A, Skowronek J, Nordsmark M, Seufferlein T, Van Gossum A, Hassan C, Repici A, Bruno MJ. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:939-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 207] [Article Influence: 23.0] [Reference Citation Analysis (1)] |
| 14. | Paul G, Bohle W, Zoller W. Risk Factors for the Development of Esophagorespiratory Fistula in Esophageal Cancer. J Gastrointestin Liver Dis. 2019;28:265-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Akin S, Can G, Aydiner A, Ozdilli K, Durna Z. Quality of life, symptom experience and distress of lung cancer patients undergoing chemotherapy. Eur J Oncol Nurs. 2010;14:400-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 130] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 16. | Wu XD, Jiang CN, Qin HY, Liu L, Feng GR, Zhang JE, Zhang MF. A study on the relationship between symptom distress and coping method in patients with esophageal carcinoma undergoing postoperative adjuvant chemotherapy. Huli Guanli Zazhi. 2014;14:77-79. |
| 17. | Wang XS, Wang Y, Guo H, Mendoza TR, Hao XS, Cleeland CS. Chinese version of the M. D. Anderson Symptom Inventory: validation and application of symptom measurement in cancer patients. Cancer. 2004;101:1890-1901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 169] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 18. | Valentino J, Freeman S, Nickl N. Retrograde esophageal dilation using Savary dilators. Laryngoscope. 2006;116:2227-2228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Sagar RC, Kumar KVV, Ramachandra C, Arjunan R, Althaf S, Srinivas C. Perioperative Artificial Enteral Nutrition in Malnourished Esophageal and Stomach Cancer Patients and Its Impact on Postoperative Complications. Indian J Surg Oncol. 2019;10:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |