Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.2044
Peer-review started: January 21, 2020
First decision: February 26, 2020
Revised: April 1, 2020
Accepted: April 15, 2020
Article in press: April 15, 2020
Published online: May 26, 2020
Processing time: 124 Days and 18.3 Hours
Ileocecal intussusception caused by two different tumors is rare, according to a literature review. We describe a case of a male patient with a cauliflower-like mass in the middle of the transverse colon observed by colonoscopy before surgery. It was considered to be intussusception caused by colon cancer. However, a substantial lipomatous mass was seen in the distal end of the intussusception by computed tomography before surgery, which posed a challenge in the preoperative diagnosis.
We report a 72-year-old male patient with intussusception. The patient underwent right hemicolectomy and cholecystectomy in our hospital on April 29, 2019. During operation, the ileum was inserted into the ascending colon by about 15 cm, and a tumor with a diameter of approximately 3.0 cm was observed in the distal part of the intestine. An atypical liposarcoma/highly differentiated liposarcoma in the adipose tissue was suspected in the postoperative pathology, and a lipoma was diagnosed after MDM2 gene testing. A 4.0 cm × 5.0 cm polypoid mass was seen immediately adjacent to the mass, and the postoperative pathology report suggested a high-level tubular adenoma. The patient was eventually cured and discharged with an uneventful follow-up.
Intussusception caused by two different types of masses is extremely rare. At present, surgery is the best treatment once intussusception is diagnosed.
Core tip: Ileocecal intussusception caused by two different tumors is rare. We report a 72-year-old male with intussusception. A cauliflower-like mass was observed in the transverse colon by colonoscopy before surgery. It was considered to be intussusception caused by colon cancer. However, a substantial lipomatous mass was seen in the distal end of the intussusception by computed tomography before surgery. The patient underwent a right hemicolectomy and cholecystectomy in our hospital. The benign and malignant fatty masses were sent for microscopic/immunohistochemical examination and MDM2 fluorescence in situ hybridization diagnosis after surgery. The patient was eventually cured and discharged with an uneventful follow-up.
- Citation: Fan WF, Ma G, Li GC, Long J, Xu YH, Guo KJ, Liu Z. Ileocecal intussusception caused by two different tumors - which is the culprit lesion? A case report. World J Clin Cases 2020; 8(10): 2044-2049
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/2044.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.2044
Intussusception is common in children but rare in adults[1]. It can be classified into four types: Enteric, ileocolic (without appendix invaginates), ileocolic (with ileocecal invagination), and colocolonic (including colorectal type). The etiology of adult intussusception is tumor- or surgery-related, idiopathic, and others. Benign or malignant tumors are the most frequent cause of intussusception in adults[1]. Any intestinal condition that changes the normal pattern of peristalsis increases the risk of intussusception[1,2]. Normal physiologic peristalsis along a bowel intussusception promotes extension of the invagination to involve longer segments of the intestine, mesentery, and mesenteric blood vessels[1,3]. In general, surgery is the best treatment once intussusception is diagnosed.
Abdominal pain accompanied by nausea, vomiting, and hematochezia for 1 d.
The patient was admitted to the emergency department of our hospital due to abdominal pain for 1 d, accompanied by diarrhea, nausea, vomiting, and black stool. The patient had been hospitalized in a local hospital at the early stage of the disease and was diagnosed with “intussusception, colonic mass, and gallbladder stone” by abdominal computed tomography (CT) and colonoscopy. After 1 wk of hospitalization, he was transferred to our hospital for surgical treatment. The patient had normal sleep, poor appetite, poor urination due to prostate stones, poor defecation, and significant weight loss.
Prostatitis, gallbladder stone, duodenal ulcer.
Sclera without yellow staining, no bleeding spots or petechiae in the skin mucosa, no liver palm or spider mole were observed. Superficial lymph nodes were not palpated, left epigastrium slightly distended, and no gastrointestinal type and peristaltic wave were noted. Abdomen was soft without tenderness, Murphy’s sign was negative, and the liver and spleen were not palpated below the costal margin. The mass, which was approximately 15 cm in diameter, was palpable in the right epigastric region. There was no muscle tension or rebound pain, and no percussion pain in the liver and spleen area, shifting dullness was negative, bowel sound was 3-4 times/min, no air to water sound or high-pitched bowel sound was observed.
White blood cell count was 11.84 × 109/L, neutrophils 9.86 × 109/L, red blood cells 5.00 × 1012/L, hemoglobin 156 g/L, platelets 482 × 109/L, direct bilirubin 4.5 μmol/L, and total bilirubin 13.2 μmol/L.
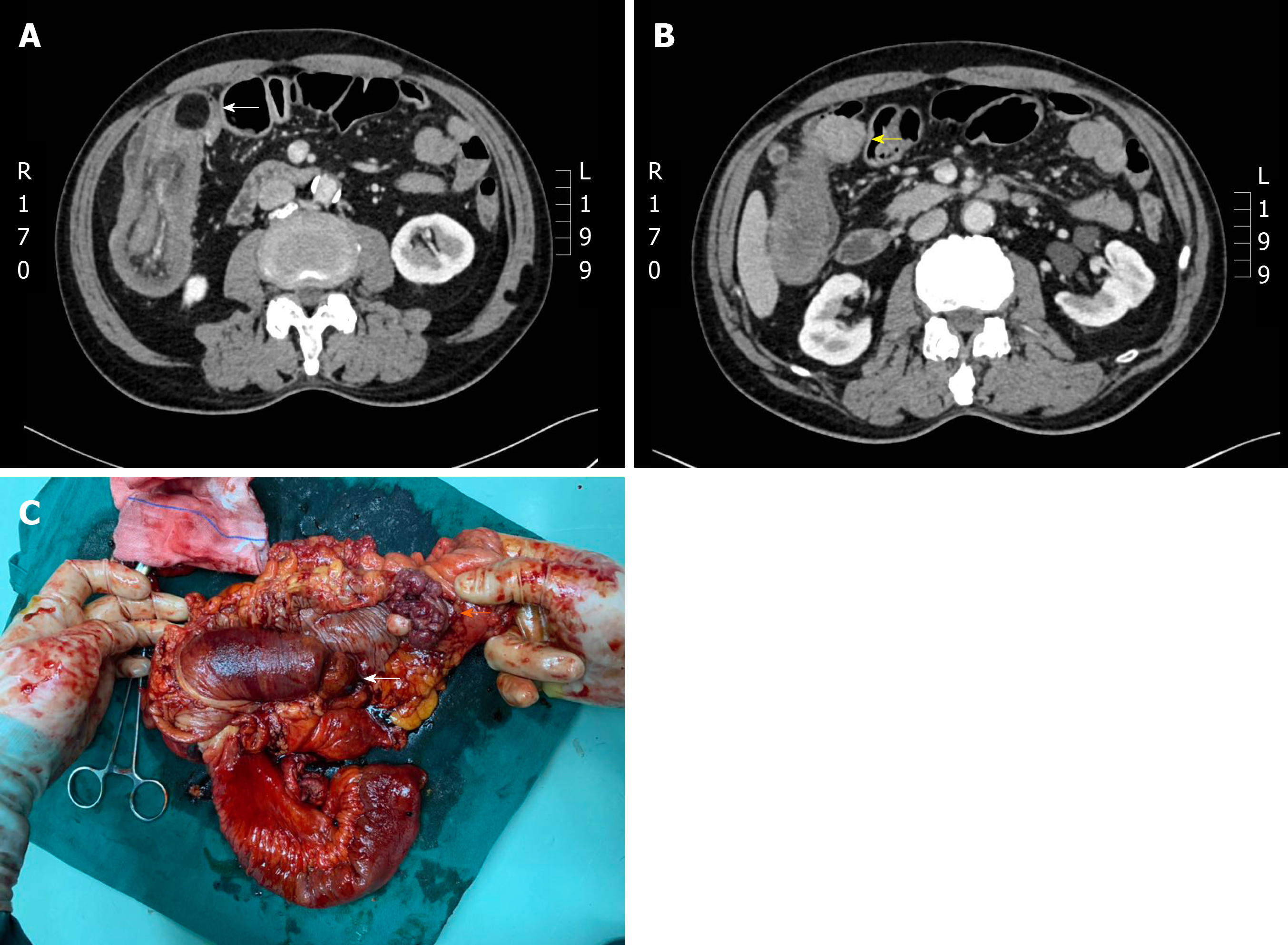
CT demonstrated an ileocecal bowel tube and mesangial membrane embedded in the ascending colon, showing a concentric circle sign. Eccentric thickening of the tube wall was seen in the colon-liver curvature, and enhancement was noted on the contrast-enhanced scan. The serous surface was slightly rough, herniated into the upper end of the intestinal loop, and there were round fat dense nodules, approximately 2.5 cm in diameter, suggesting a possible fat source of the tumor. Another solid mass, about 4.0 cm in diameter, was seen adjacent to this tumor and was suggestive of colon cancer. At the same time, thickening of the gallbladder wall, multiple dots of high-density shadows in the gallbladder, prostatic hyperplasia, chronic inflammation of the bladder and a small amount of pelvic effusion were noted (Figure 1A and 1B).
We considered the tumor to be the cause of intussusception before surgery; however, as two masses were found, it was uncertain which mass was the main cause of intussusception. We conducted an emergency surgical exploration. During the operation, the small intestine showed obvious dilatation, which is a manifestation of intestinal obstruction. Part of the ileum was inserted into the ascending colon up to the colon-liver curve, approximately 15 cm in length. A right hemicolectomy was performed, and the bowel was cut at the distal end of the tumor on the left side of the transverse colon (Figure 1C). The ileum was cut 15 cm from the ileocecal fold. The right hemicolon and the mesentery were completely removed and isolated. The gallbladder was removed due to gallstones. The ileum was inserted into the cecum up to the hepatic tract of the colon approximately 15 cm in diameter, and the intestinal wall showed necrotic changes. The insertion site showed a tumor in the ileocecum with a clear boundary and a diameter of 2.5 cm.
Postoperative pathology suggested that the ileocecal mass was a fatty dense mass and was suspected to be an atypical liposarcoma/highly differentiated liposarcoma that required MDM2 gene testing for diagnosis (Figure 2). The transverse colon mass was a high-level tubular adenoma, and the gallbladder showed chronic cholecystitis. Immunohistochemistry results were: CK (-), CDK4 (+), MDM2 (-), Vimentin (+), s-100 (+), CD34 (-), SMA (-), beta-catenin (-), Ki-67 (5%), CD117 (-), and DOG-1 (-). To confirm that the ileocecal mass was a lipoma or liposarcoma, the patient underwent MDM2 gene testing, and no MDM2 gene amplification was reported, which was consistent with the diagnosis of lipoma. The patient was diagnosed with ileocecal lipoma intussusception, transverse colon high-level tubular adenoma, and gallstones.
Ileocecal lipoma intussusception, tubular adenoma of the transverse colon, and gallstones.
Right hemicolectomy and cholecystectomy.
The patient had a good postoperative recovery, without fever or other symptoms, and wound healing was satisfactory without exudation. Postoperative CT examination indicated that the anastomosis was normal. The patient was finally discharged from hospital 16 d after surgery with normal diet, urination, and defecation.
Intussusception is defined as a long intestinal tube connected to the stomach or within the lumen, causing diversion of intestinal contents due to intestinal obstruction[4]. Intussusception can be divided into primary intussusception and secondary intussusception. More than 90% of primary intussusceptions are found in infants, while secondary intussusception in adult intussusception is clinically characterized by abdominal pain, vomiting, bloody stools, and abdominal mass. The causes of intussusception are diverse, and include ulcerative colitis[5], intestinal amoeba[6], intestinal allergic purpura[7], intestinal polyps[8], Meckel’s diverticulum[9], colon cancer[10], colonic lipoma[11], and colonic liposarcoma[12]. Intussusception is rare in adult intestinal obstruction[13]. In most intussusceptions, there is a starting site of organic lesion from which intussusception develops[14]. The types of intussusception are also diverse and include enteric, ileocolic, ileocecal, and colonic[15], and ileocecal intussusception is the most common type[16].
There are also rare causes of intussusception. Jin et al[17] reported cases of intussusception caused by para-duodenal hernia. Chaudhary et al[18] reported a case of colon-colon intussusception caused by primary liposarcoma of the colon. However, it would be interesting to dynamically observe cases of lipoma of the colon from asymptomatic to developing intussusception by colonoscopy[19].
In this case, the patient was admitted to our hospital due to abdominal pain and bloody stool for 1 d. CT showed a low-density tumor and solid dense tumor, which were adjacent to the distal end of the nested bowel. Two masses were also seen on colonoscopy at a local hospital, which caused difficulty in preoperative diagnosis. When the specimens were examined after right hemicolectomy, the adipose-derived neoplasm was found in the nested head. The intussusception continued to the substantial neoplasm, which appeared just before the nested head and played an important role in mechanical blocking of the intussusception. This suggested that the adipose-derived neoplasm was the cause of the intussusception and the substantial neoplasm stopped the advance of the intussusception, and the two masses together caused intestinal obstruction, intussusception and intestinal necrosis. The patient was cured and discharged from hospital after pathological confirmation of the lipoma and high-level tubular adenoma.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Goral V, Grawish M S-Editor: Gong ZM L-Editor: Filipodia E-Editor: Xing YX
| 1. | Honjo H, Mike M, Kusanagi H, Kano N. Adult intussusception: a retrospective review. World J Surg. 2015;39:134-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 169] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 2. | Weilbaecher D, Bolin JA, Hearn D, Ogden W 2nd. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121:531-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 213] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Brayton D, Norris WJ. Intussusception in adults. Am J Surg. 1954;88:32-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 98] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 666] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 5. | Esaki M, Matsumoto T, Fuyuno Y, Maehata Y, Kochi S, Hirahashi M, Iida M. Giant inflammatory polyposis of the cecum with repeated intussusception in ulcerative colitis: report of a case. Am J Gastroenterol. 2009;104:2873-2874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Steer D, Clarke DL, Buccimazza I, Thomson SR. An unusual complication of intestinal amoebiasis. S Afr Med J. 2005;95:845. [PubMed] |
| 7. | Lim CJ, Chen JH, Chen WL, Shen YS, Huang CC. Jejunojejunum intussusception as the single initial manifestation of Henoch-Schönlein purpura in a teenager. Am J Emerg Med. 2012;30:2085.e1-2085.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Ye W, Lu B, Liu H. A Rare Cause of Multiple Intestinal Mass Lesions. Gastroenterology. 2016;150:570-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Yu M, Fang Z, Shen J, Zhu X, Wang D, Shi Y. Double simultaneous intussusception caused by Meckel's diverticulum and intestinal duplication in a child. J Int Med Res. 2018;46:3427-3434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Martin P, Sklow B, Adler DG. Large colonic lipoma mimicking colon cancer and causing colonic intussusception. Dig Dis Sci. 2008;53:2826-2827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Gluskin AB, Singh NA. Gastrointestinal: A sigmoid lipoma as the cause of intussusception. J Gastroenterol Hepatol. 2017;32:292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Gomez G, Bilal M, Klepchick P, Clarke K. Rare case of entero-enteric intussusception caused by small bowel metastasis from a cardiac liposarcoma. World J Gastrointest Oncol. 2016;8:326-329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal Intussusception: Etiology, Diagnosis, and Treatment. Clin Colon Rectal Surg. 2017;30:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 194] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 14. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 428] [Cited by in RCA: 506] [Article Influence: 31.6] [Reference Citation Analysis (2)] |
| 15. | Yalamarthi S, Smith RC. Adult intussusception: case reports and review of literature. Postgrad Med J. 2005;81:174-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 137] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 16. | Rivkine E, Emmanuel R, Marciano L, Léa M, Polliand C, Claude P, Valenti A, Antonio V, Ziol M, Marianne Z, Poncelet C, Christophe P, Barrat C, Christophe B. Ileocolic intussusception due to a cecal endometriosis: case report and review of literature. Diagn Pathol. 2012;7:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Jin C, Mo J, Wang G, Jiang H, Feng Y, Wang S. Paraduodenal hernia complicated with intussusception: case report. BMC Surg. 2018;18:120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Chaudhary A, Arora R, Sharma A, Aggarwal S, Safaya R, Sharma S. Primary colonic liposarcoma causing colo-colic intusussception: a case report and review of literature. J Gastrointest Cancer. 2007;38:160-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Siu S, Oliphant R, Benstock S, Keshava A, Rickard MJFX. Colonic lipoma causing intussusception: a case for colonoscopic surveillance? ANZ J Surg. 2019;89:428-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |