Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.2028
Peer-review started: March 5, 2020
First decision: April 1, 2020
Revised: April 23, 2020
Accepted: April 27, 2020
Article in press: April 27, 2020
Published online: May 26, 2020
Processing time: 81 Days and 5 Hours
Because immediate implant surgery is not recommended for patients who have been diagnosed with periodontitis, researchers have treated these patients with a variety of methods, including combining orthodontic and periodontal surgeries as well as implantation. However, these treatments cost time and money for the patient. Although it has been reported that temporary implants released a severe gag reflex in 1 case, only a few studies have documented using temporary implants to treat patients diagnosed with severe periodontitis.
The patient was a 49-year-old female who was missing the majority of her teeth and had gingival atrophy and severe alveolar bone atrophy. After being diagnosed with severe periodontitis, the patient underwent staged load applied implant restoration therapy. The first load-bearing stage was carried out immediately by inserting temporary Osstem mini implants. Maxillary teeth were extracted by using the guided bone regeneration technique, and lateral maxillary sinus lifting was conducted on both sides. During the second load-bearing stage, temporary implants were removed, and permanent implants were placed. The resin bridge was segmented during the third load-bearing stage. During the fourth load-bearing stage, the permanent prosthesis was positioned in the patient’s mouth.
By conducting the load-bearing treatment in stages, the patient’s mouth contained restorations throughout the procedure, thus guaranteeing basic function and appearance.
Core tip: The advantages of the staged bone load-bearing treatment via temporary implants include: (1) A guarantee of the basic function and outward appearance; (2) Bone formation can occur rapidly and properly with temporary implants; and (3) Produces enough soft tissue to be reshaped.
- Citation: Wang SH, Ni WC, Wang RF. Treating severe periodontitis with staged load applied implant restoration: A case report. World J Clin Cases 2020; 8(10): 2028-2037
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/2028.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.2028
Oral implantation in patients with severe periodontitis is a controversial topic[1,2]. Though some cases[1-3] reported various treating methods (Table 1 and Table 2), one study[4] tried to skillfully use temporary implants in patients. There are two treatment methods available for patients with serious bone defects that require immediate dental implant surgery[5,6]. The indication to conduct All-on-4 implant surgery is relatively wide because longer implants could be used in minimum bone volume. However, the bone plates should be placed high enough because abrasion cannot occur[7]. Zygomatic implants can be used in patients if the zygomatic bone is stable enough for immediate restoration to be done[8]. Technical requirements are relatively high due to the risk factors of zygomatic implantation surgery. Additionally, All-on-4 and zygomatic implants might impose limitations on long-term oral health maintenance. Therefore, these two treatments might not be suitable for young patients.
| Case | Patient summary | Patient history | Intraoral examination | Radiological features | Final diagnosis |
| Combined periodontal and implant treatment of a patient with chronic periodontitis and severe alveolar bone loss | A 41-yr-old female whose upper front teeth were loose | Denied having systemic disease. The teeth have been filled with restorations at a different hospital | Teeth #21, #26, and #27 were missing and the patient had a deep overbite. The gap length of the missing teeth, located at the upper front part of the jaw, was 10 mm. The width of the alveolar ridge was 4 mm | Teeth #21, #26, and #27 were missing. In the area of tooth #21, the alveolar bone was absorbed. The entire alveolar bone was absorbed horizontally from 1/3 to 1/2 the depth of the root length | Moderate chronic periodontitis; severe prosthesis; dentition defect |
| Implant treatment of a case of severe chronic periodontitis | A non-smoking 51-yr-old female who only has a few maxillary teeth | Denied having systemic disease, drug allergies, and any infectious disease | Supragingival calculus was found in the mandibular anterior segment and pathologic tooth migration was found in teeth #11 and #12. Teeth #11, #12, and #21 exhibited class III mobility. Tooth #46 had a class III furcation lesion. Sixty-one percent of the teeth had a deep PPD of over 4 mm; 61% had BOP; and all teeth scored 101% on O’Leary’s plaque control record | In teeth #14, #16, #26, and #46, periodontal tissue destruction occurred. Horizontal bone resorption depth was 3 to 5 mm and, vertical bone resorption depth was 4 to 6 mm | Generalized moderate to severe chronic periodontitis |
| Treating severe periodontitis with staged load applied implant restoration | A 49-yr-old female who was missing most of her teeth and wanted implants immediately | Denied having systemic disease, drug allergies, and any infectious disease | The patient was missing the majority of her teeth and had gingival atrophy and severe alveolar ridge atrophy. There was a long PFM bridge on teeth #11-14 and #21-24 | Alveolar bone was absorbed to 1/3 of the root apex; the bond width of the maxillary anterior region was approximately 3 mm; the labial bone was absorbed; and the bone height in both posterior areas w approximately 2 mm | Dentition defect; Severe periodontitis |
| Case | Treatment step 1 | Treatment step 2 | Treatment step 3 | Treatment step 4 | Prognosis and follow-up |
| Combined periodontal and implant treatment of a patient with chronic periodontitis and severe alveolar bone loss | Basic periodontal treatment (non-surgical) and reassessment | In the area of tooth #21, conducted GBR tissue increment surgery and dental implantation simultaneously | Temporary restoration on the implant was made for gum shaping | Removed bad prosthesis in the area of tooth #11; permanent restorations were made | Received good feedback from patient; new therapy idea combined implantation, periodontal and restorations. This patient only has a limited number of bone defects |
| Implant treatment of a case of severe chronic periodontitis | Initial periodontal treatment: Oral hygiene instruction; scaling and root planning; tooth extraction (teeth #11, #12, #16, #21, #22, and #27); partial denture therapy (teeth #12-22); root canal treatment and hemisection (tooth #46); Occlusal adjustment (teeth #13 and #23) | Oral functional rehabilitation treatment: Implant prosthesis (in the areas of teeth #12, #16, #22, #36, and #41) | Temporary restoration: During the 5-mo relief period, a partial denture was placed in the maxillary anterior region | Permanent restoration: All custom abutments and porcelain fused to metal crowns were retained | The screw was restored after cleaning and occlusal adjustment. The patient’s oral hygiene has been well maintained. There has not been any recurrence nor has the patient's periodontal disease worsened among other natural teeth |
| Treating severe periodontitis with staged load applied implant restoration | First load-bearing stage: Removed the remaining teeth in the jaw; conducted immediate All-on-6 implant restoration and immediate loading | Second load-bearing stage: Inserted four temporary Osstem mini implants; performed immediate loading, maxillary GBR technique, and lateral maxillary sinus lifting on both sides | Third load-bearing stage: Four temporary implants were removed, and eight permanent implants were placed; performed immediate loading | Fourth load-bearing stage: The resin bridge was segmented for gingival repair | Restored with custom abutments and the zirconium crown-bridge prosthesis |
By using temporary implants for this case, transitional support was provided throughout the treatment. Studies have shown that temporary implants cause slight bone resorption but have little effect on the increment of bone mineral content.
A 49-year-old female patient was referred to the dental department of Zhejiang Chinese Medical University.
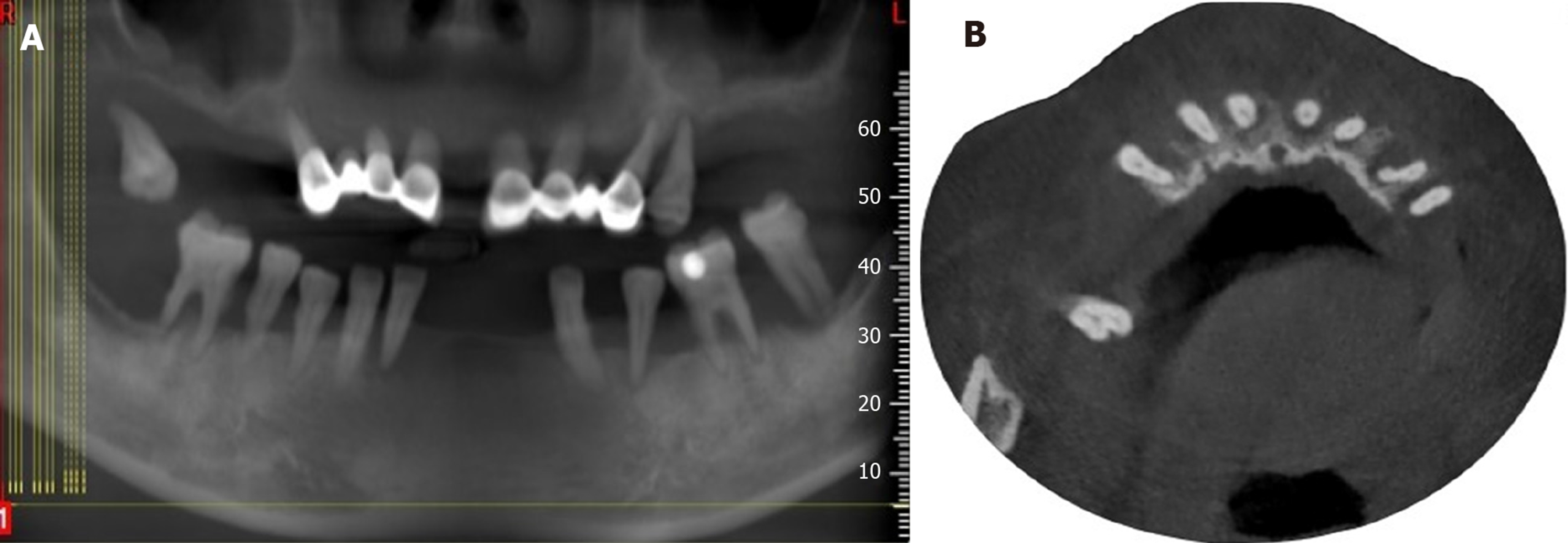
The patient was missing the majority of her teeth and had gingival atrophy and severe alveolar ridge atrophy. There was a long PFM bridge on teeth #11-14 and #21-24 (Figure 1).
Cone beam computed tomography showed that the alveolar bone was absorbed to 1/3 of the root apex; the bond width of the maxillary anterior region was approximately 3 mm (Figure 2A). The labial bone was absorbed, and the bone height in both posterior areas was approximately 2 mm (Figure 2B).
Dentition defect; Severe periodontitis.
Surgical procedures overview: (1) Extract teeth #11, #12, #14, #17, #21, #22, #24, and #25; (2) Perform lateral maxillary sinus lifting on both sides; and (3) Perform guided bone regeneration in the maxillary anterior tooth area, insert temporary implants in the anterior tooth area, and perform immediate loading.
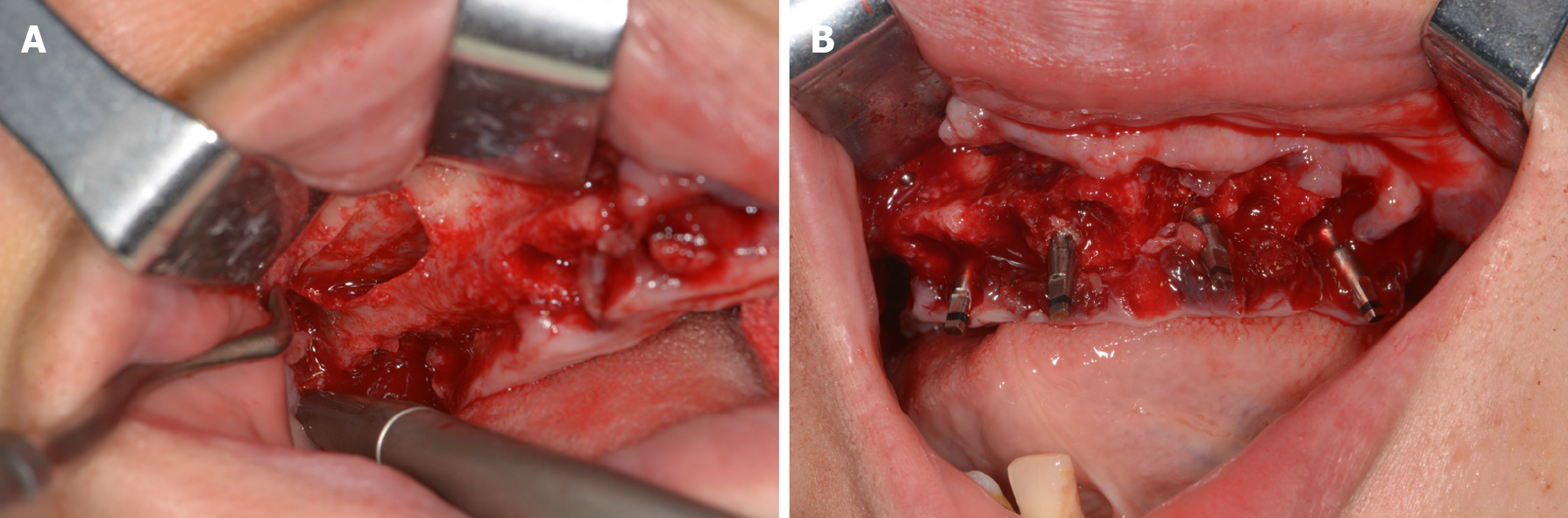
Before surgery, the patient received a Cefradine capsule to relieve inflammation, a dexamethasone acetate tablet to relieve swelling, and a compound paracetamol tablet to relieve pain. After conducting regular disinfection and administering anesthesia, teeth #11, #12, #14, #17, #21, #22, #24, and #25 were extracted. After the teeth extraction sockets were cleaned, an incision was made in the middle of the upper alveolar crest, and a relaxant incision was made on the buccal side. A 10 mm × 20 mm rectangular window was made at the maxillary sinus lateral wall (Figure 3A). The lowest margin of this window was 3-5 mm from the bottom of the maxillary sinus. The mucosa bottom of the maxillary sinus was turned inward and upward with a collagen membrane layer to make a new mucosa bottom. The bone augmentation material was put into the sinus floor making the lift height approximately 10 mm.
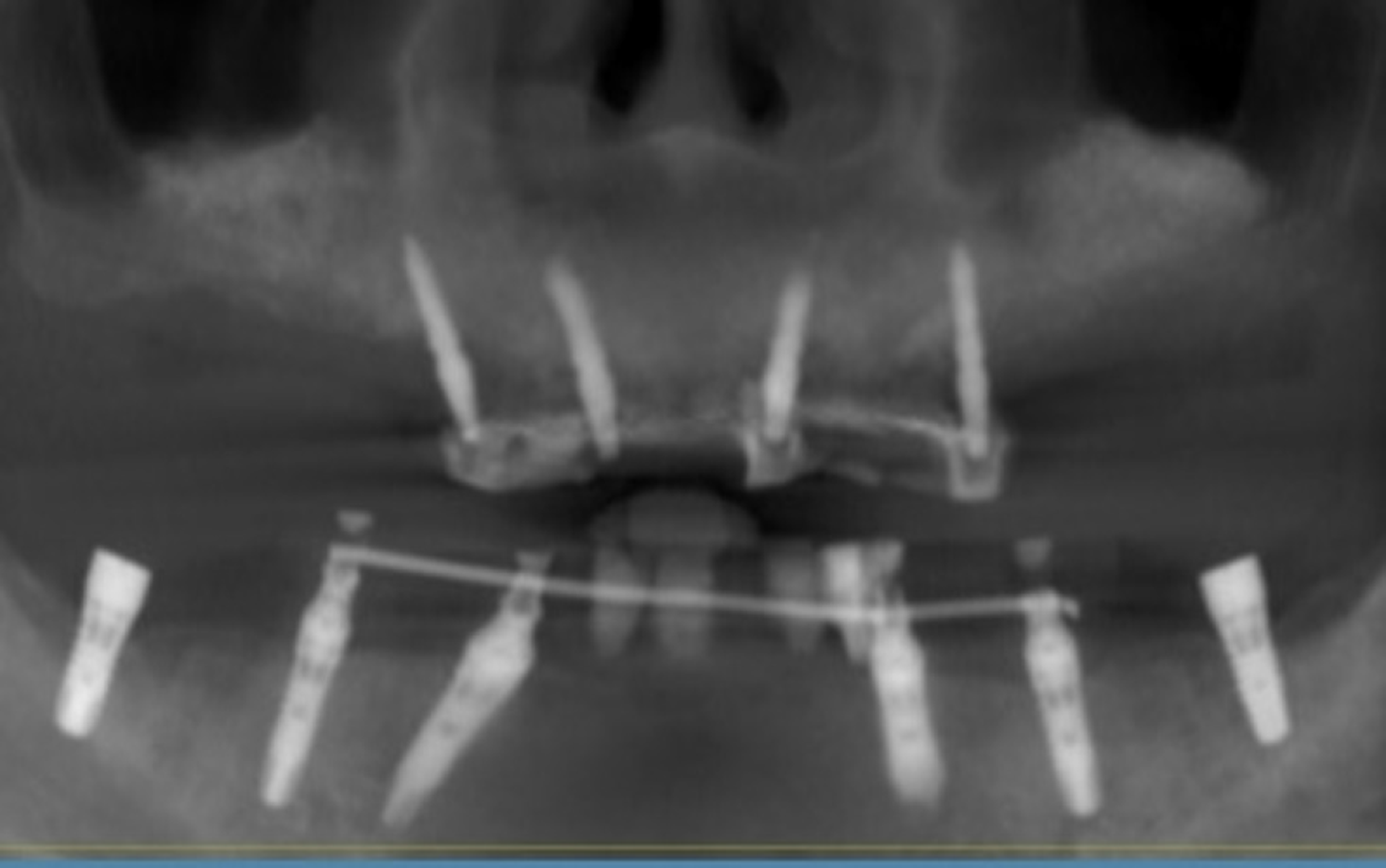
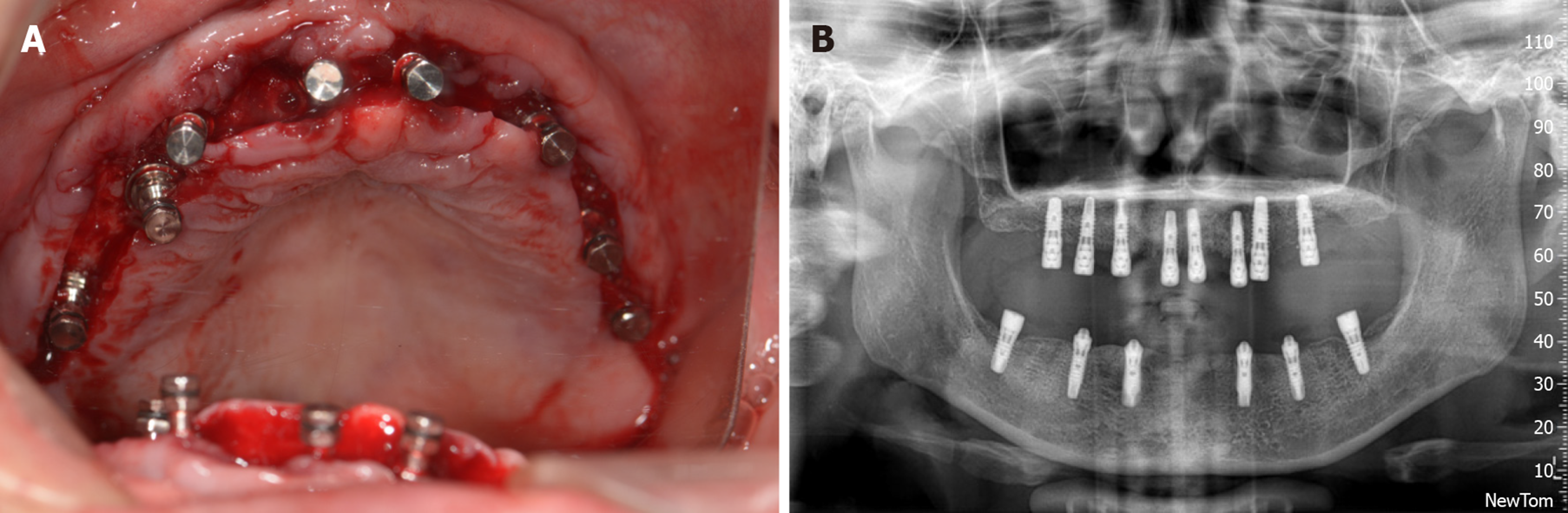
Four Osstem mini implants (Ms System Fixture, Osstem Implant Co. Ltd., Korea), which were used as a support temporary denture, were implanted into the areas of teeth #12, #14, #22, and #24 (Figure 3B). The temporary mini implants were inserted into alveolar bone instead of the bone graft. A 0.5 g autogenous bone mixed with Bio-Oss bone (Bio-Oss, Geistlich Pharma AG, Switzerland) filled the right maxillary anterior bone defect area. Then a 25 mm × 25 mm Bio-Gide periosteum (Bio-Gide, Geistlich Pharma AG, Switzerland) covered the top. Teeth #17 and #25 were each made into an auto-tooth bone, which filled the left maxillary anterior bone defect area, and were covered with 25 mm × 25 mm Bio-Gide periosteum. The collagen membrane was placed 1.5 mm away from the adjacent tooth in case the membrane was exposed and contaminated. The soft tissue was covered carefully with a relaxant notch via absorbed suture (4/0) to hold together the whole membrane. Temporary teeth #14-24 were placed in the maxillary anterior area. The postoperative X-ray showed that the temporary implants were placed properly (Figure 4).
Before surgery, the patient received a Cefradine capsule to relieve inflammation, a dexamethasone acetate tablet to relieve swelling, and a compound paracetamol tablet to relieve pain. After conducting regular disinfection and administering anesthesia, the periodontal flap procedure was done in the areas of teeth #16 and #17. Then maxillary sinus elevation surgery was conducted with 0.5 g Bio-Oss bone meal that filled the bone defected area. A 25 mm × 25 mm bone membrane covered the top, and an absorbed suture was used to close the wound carefully.
Examination: Some pigmentation was found on the maxillary CAD/CAM resin crowns. The implants were stable. There was not an uncomfortable feeling when the implants were tapped, and the surrounding gingiva had no abnormalities. Atrophied alveolar bone was found on teeth #32, #34, #36, #37, #42, #43, #44, #45, and #46. These teeth were severely loose. There was not an uncomfortable feeling when tapped, and oral hygiene was acceptable. The open range of the mouth was 3.5 fingers. There wasn’t any temporomandibular joint pain, bouncing, or noise. Cone beam computed tomography revealed the bone quality of the mandibular was still acceptable.
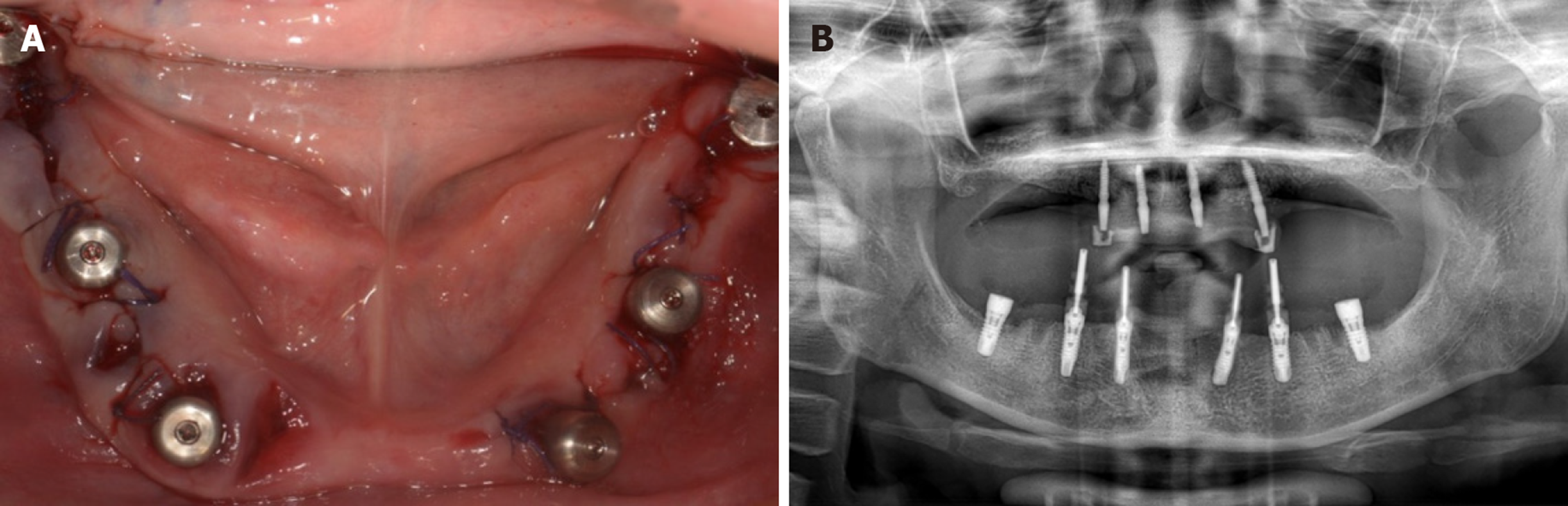
Surgical procedures: (1) Cleaned resin crowns and gum and removed pigment with a polishing needle; (2) Before surgery, the patient received a Cefradine capsule to relieve inflammation, a dexamethasone acetate tablet to relieve swelling, and a compound paracetamol tablet to relieve pain. The patient gargled chlorhexidine twice for 3-5 min each time; (3) After conducting regular disinfection and administering anesthesia, the gingiva was reconstructed. Teeth #32, #34, #36, #37, #42, #43, #44, #45, and #46 were extracted. Teeth extraction sockets were cleaned deeply, and granulation tissue was removed. An incision and an access flap were made in the mandibular region. After preparing the implant sockets, teeth #33, #35, #37, #43, #45, and #47 were implanted with SP 14.0 mm × 14 mm, 4.5 mm × 11 mm, 5.0 mm × 9.5 mm, 4.0 mm × 14 mm, 4.5 mm × 12.5 mm, and 5.0 mm × 9.5 mm permanent implants (Element Implant Mc Inicell, Thommen Medical AG, Switzerland) (Figure 5A). The torsion force was set at 35 Ncm. Teeth #33, #35, #43, and #45 were placed in multi-dental abutments, while teeth #37 and #47 were placed in abutments. Bio-Oss bone meal (Bio-Oss, Geistlich Pharma AG, Switzerland, 0.5 g) filled the areas of teeth #33, #43, and #45. Collagen plugs were placed in the areas of teeth #44 and #46. An absorbed suture was used to close the wound carefully; (4) After surgery, the abutments were removed and model transfer levers were placed in the areas of teeth #33, #35, #43, and #45. An X-ray showed that the implants were inserted in an acceptable position, and the implants combined with the model transfer levers firmly (Figure 5B). The models were copied and CAD/CAM resin crowns were made; and (5) We tried on CAD/CAM resin crowns, performed immediate loading, and polished and fixed resin crowns. Routine postoperative care and medical advice were provided after surgery.
Third subsequent visit (29 wk after the initial surgery): Removed temporary implants, performed immediate loading on the maxillary and permanent artificial teeth (with plastic base)
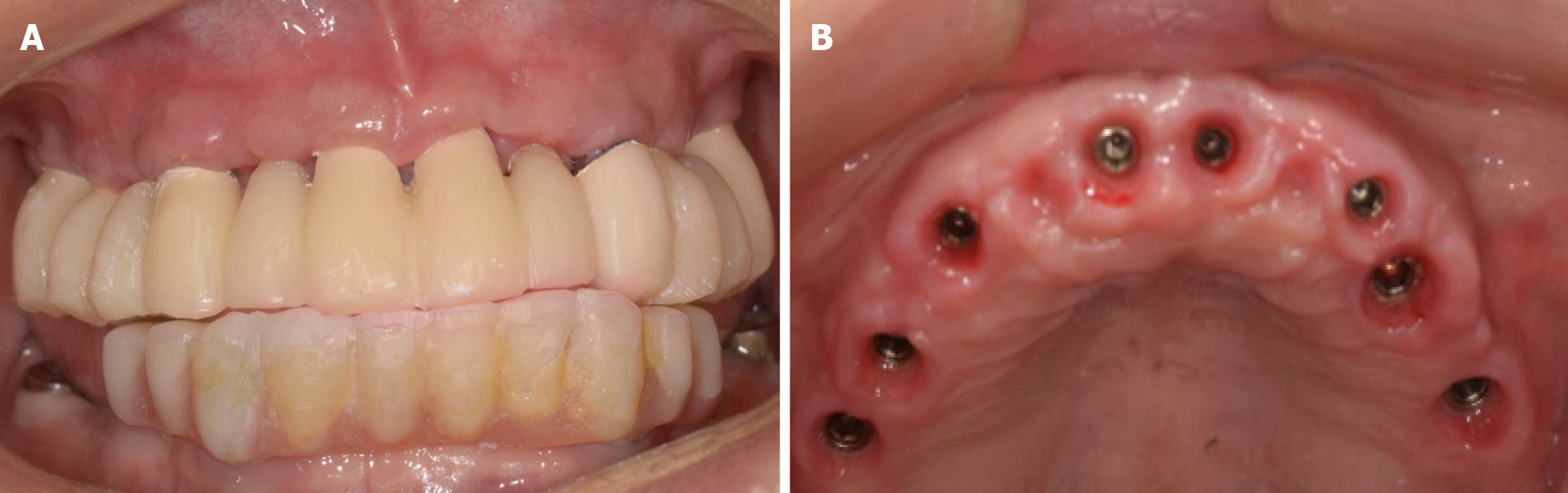
Treatment: (1) Before surgery, the patient received a Cefradine capsule to relieve inflammation, a dexamethasone acetate tablet to relieve swelling, and a compound paracetamol tablet to relieve pain. The patient gargled chlorhexidine twice for 3-5 min each time; (2) After removing the maxillary resin crowns, conducting regular disinfection, and administering anesthesia, the implant sockets were prepared, and the mini Osstem implant was removed. Implant surgery was performed in the areas of teeth #11, #13, #15, #16, #21, #23, #24, and #26, and we placed permanent implants (Element Implant Mc Inicell, Thommen Medical AG, Switzerland) with SP 14.0 mm × 11 mm, 4.0 mm × 11 mm, 4.5 mm × 11 mm, 5.0 mm × 9.5 mm, 4.0 mm × 11 mm, 4.0 mm × 11 mm, 5.0 mm × 12.5 mm, and 5.0 mm × 9.5 mm separately (Figure 6A). The abutments were placed carefully after implantation. The torsion force was set from 25 Ncm to 30 Ncm in the area of tooth #23, whereas in the areas of teeth #11, #13, #15, #16, #21, #24 and #26, the torsion force was 35 Ncm. An absorbed suture (4/0) was used to close the wound carefully; (3) The X-ray post-surgery showed that all implants were placed in an acceptable position as well as had satisfactory primary stability (Figure 6B); (4) The maxillary and mandibular were mocked up, and the resin crowns were worn until the next day; and (5) Routine postoperative care and medical advice were provided after surgery.
The protective caps were removed, and temporary dentures in the areas of teeth #11, #13, #15, #16, #21, #24, #26, #33, #35, #37, #43, #45 and #47 were tried on. The position was acceptable. We fixed the screw, blended, polished, and sealed the dentures.
The temporary dentures were removed to make final models. The permanent abutments with temporary crowns were made, and gingival repair will be conducted in the next stage. Patient wore temporary dentures that were sealed with resin.
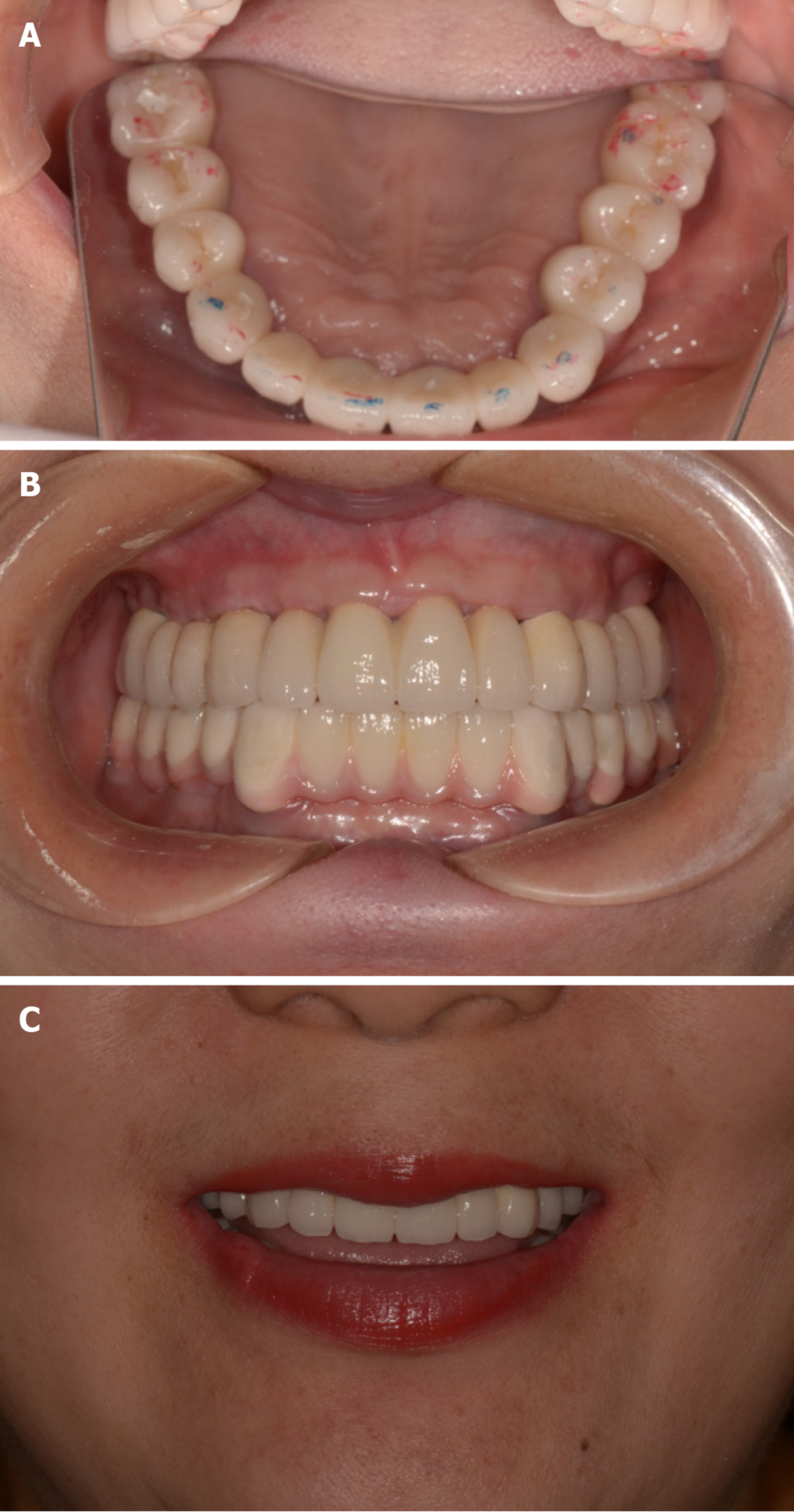
The temporary dentures, abutments in maxillary, and the healing caps in the areas of teeth #16 and #26 were removed. After placing permanent abutments and trying on the temporary prosthesis, the shape and the crown contour of the temporary prosthesis were restored. The height of the crown was adjusted and changed the placement. The temporary crown from the area of tooth #23 was removed (Figure 7). Then, the flow resin was used to recover the crown length of the anterior mandibular temporary zirconia prosthesis. As a result, occlusion of the maxillary and mandibular restorations was adjusted (Figure 8A), and maxillary temporary crowns were permanently cemented (Figure 8B).
The patient has a normal bite and has not complained about swelling, pain, food impaction, or discomfort. None of the dentures are loose. During the oral inspection and percussion test, both upper and lower jaws did not exhibit loose implants. Fracture phenomenon was not present in the upper crown, and none of the crowns were loose. The patient displayed excellent oral hygiene and is satisfied with her smile (Figure 8C).
In this case, the loss of the maxillary alveolar crest reached class V level, which means the patient was supposed to undergo incremental bone therapy before the implant procedure[9]. To speed up the rate of healing and maintain oral function as well as appearance, bone treatment therapy was performed throughout the implantation procedures.
The relationship between the maxilla and the mandible is similar to two conical columns, which taper off from the bottom to the top[10]. The basal bone is wider than the alveolar process in the mandible, and the bone resorption is in the direction of the vestibular groove after tooth loss[11]. As a result, the resorption of the vertical bone contributed to the increased width in the mandibular. Moreover, the proximal, medial and distance of the edentulous mandible also increased because the basal bone is located near the intermediate region. Bone absorption of alveolar processes can seriously affect the relationship in vertical, horizontal, and sagittal directions[12]. The edentulous jaw will cause a more severe maxillary and mandibular bone resorption disorder, usually includes a severe mismatch between the maxillary and mandibular bone, similar to class III mismatch in sagittal and horizontal directions[13].
Vertical bone augmentation has several advantages, one being the ability to achieve the natural perforation of the anterior maxillary short crown through the adherent mucosa[14]. Compared to removable dentures, fixed prosthesis is simple in design and fabrication. Additionally, it can be used to complete the superstructure with all-ceramic prostheses[15]. All of these advantages would make surgery more economically beneficial, minimize injuries, and provide a functional retainer that allows patients to sequence bone augmentation therapy.
To increase the success rate of implant surgery, a fixed prosthesis supported by simultaneous implants would release the patient's discomfort. Immediate loading of temporary implants not only allows patients to obtain a satisfactory occlusal recovery during immediate implantation but also plays an important role in avoiding mechanical loading in the incremental tissue area. Also, it is forbidden to wear a mucosa-supported removable partial denture after incremental tissue surgery.
In conclusion, indications for staged implant loading include: (1) Iinsufficient bone mass for immediate restoration; (2) Multiple disciplines required; (3) Occlusal retention or reconstruction; and (4) Necessity for temporary restoration of teeth.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ishizawa K, Isilk A S-Editor: Dou Y L-Editor: Filipodia E-Editor: Liu JH
| 1. | Seki K, Hagiwara Y. Implant Treatment with 12-Year Follow-Up in a Patient with Severe Chronic Periodontitis: A Case Report and Literature Review. Case Rep Dent. 2019;2019:3715159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Li Y, Xu L, Zhou YH, Ouyang XY, Cao T. Combination of periodontal, orthodontic and endodontic therapy in upper anterior teeth with hopeless prognosis and long-time follow-up: a case report. Beijing Da Xue Xue Bao Yi Xue Ban. 2017;49:740-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Lin ZK, Shu R. [Combined periodontal and implant treatment of chronic periodontitis patient with severe alveolar bone defects: a case report]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2018;53:164-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Stimmelmayr M, Edelhoff D, Schweiger J, Güth JF. Temporary Single Palatal Implant for Denture Stabilization During Augmentation and Implant Procedure: A Case Report. Int J Periodontics Restorative Dent. 2018;38:e105-e111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Hu C, Gong T, Lin W, Yuan Q, Man Y. Immediate implant placement into posterior sockets with or without buccal bone dehiscence defects: A retrospective cohort study. J Dent. 2017;65:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Li S, Di P, Zhang Y, Lin Y. Immediate implant and rehabilitation based on All-on-4 concept in patients with generalized aggressive periodontitis: A medium-term prospective study. Clin Implant Dent Relat Res. 2017;19:559-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Soto-Penaloza D, Zaragozí-Alonso R, Penarrocha-Diago M, Penarrocha-Diago M. The all-on-four treatment concept: Systematic review. J Clin Exp Dent. 2017;9:e474-e488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Davó R, Bankauskas S, Laurincikas R, Koçyigit ID, Mate Sanchez de Val JE. Clinical Performance of Zygomatic Implants-Retrospective Multicenter Study. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A. Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clin Oral Implants Res. 2015;26:e8-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | Genç T, Duruel O, Kutlu HB, Dursun E, Karabulut E, Tözüm TF. Evaluation of anatomical structures and variations in the maxilla and the mandible before dental implant treatment. Dent Med Probl. 2018;55:233-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Bertl K, Bertl MH, Heimel P, Burt M, Gahleitner A, Stavropoulos A, Ulm C. Alveolar bone resorption after primary tooth loss has a negative impact on straightforward implant installation in patients with agenesis of the lower second premolar. Clin Oral Implants Res. 2018;29:155-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Tan Z, Kang J, Liu W, Wang H. The effect of the heights and thicknesses of the remaining root segments on buccal bone resorption in the socket-shield technique: An experimental study in dogs. Clin Implant Dent Relat Res. 2018;20:352-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Zhang DZ, Xiao WL, Zhou R, Xue LF, Ma L. Evaluation of Bone Height and Bone Mineral Density Using Cone Beam Computed Tomography After Secondary Bone Graft in Alveolar Cleft. J Craniofac Surg. 2015;26:1463-1466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Elnayef B, Monje A, Gargallo-Albiol J, Galindo-Moreno P, Wang HL, Hernández-Alfaro F. Vertical Ridge Augmentation in the Atrophic Mandible: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2017;32:291-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 15. | Barenghi L, Barenghi A, Cadeo C, Di Blasio A. Innovation by Computer-Aided Design/Computer-Aided Manufacturing Technology: A Look at Infection Prevention in Dental Settings. Biomed Res Int. 2019;2019:6092018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |