Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.1966
Peer-review started: February 10, 2020
First decision: April 1, 2020
Revised: April 8, 2020
Accepted: April 17, 2020
Article in press: April 17, 2020
Published online: May 26, 2020
Processing time: 104 Days and 20.9 Hours
Recurrent hemarthrosis is a rare complication of total knee arthroplasty, and only a few cases have been reported; hence, it is hard to establish comprehensive diagnosis and treatment guidelines. We here report a case of recurrent hemarthrosis after total knee arthroplasty, and briefly review the literature.
A 50-year-old man, with a history of hypertension, presented to the Orthopedic Department of our hospital for non-traumatic acute left knee pain and swelling associated with a warmth sensation 14 mo after total knee arthroplasty. Investigations (ultrasound, aspiration, and arthroscopy) and managements (non-surgical, arthroscopy and open exploration) were performed, and the clinical effects of these interventions were analyzed separately. Clinical evidence indicates that the cause of this case was rupture of a pseudoaneurysm of the medial superior genicular artery.
The present case indicated that angiography is essential in cases of hemarthrosis after TKA; arthroscopy may not always be adequate as it may not provide a clear view; and traditional open exploration is still effective and sometimes necessary.
Core tip: Recurrent hemarthrosis is a rare complication of total knee arthroplasty, and only a few cases have been reported; hence, it is hard to establish comprehensive diagnosis and treatment guidelines. We present herein a rare case of recurrent hemarthrosis which occurred 14 mo after total knee arthroplasty. The patient underwent traditional investigations (ultrasound, aspiration, and arthroscopy) and managements (non-surgical, arthroscopy and open exploration), and the clinical effects of these interventions were analyzed separately. Clinical evidence indicated that the cause of recurrent hemarthrosis in this case was rupture of a pseudoaneurysm of the medial superior genicular artery.
- Citation: Geng X, Li Y, He X, Tian H. Traditional investigation and management for recurrent hemarthrosis after total knee arthroplasty: A case report. World J Clin Cases 2020; 8(10): 1966-1972
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/1966.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.1966
Recurrent hemarthrosis is a complication of total knee arthroplasty (TKA)[1], with an incidence of 0.3% to 1.6%, and appropriate management should be implemented as early as possible to minimize the risk of severe consequences[2-5]. No consensus is available on the criteria for diagnosis or treatment of this disease[6]. Kindsfater et al[7] described a case series of 30 patients and their findings were broadly reflective of the subsequent literature. In the present case, various investigations and managements were performed, and the clinical effects of these interventions were analyzed separately.
A 50-year-old man, with a history of hypertension, presented to the Orthopedic Department of our hospital for non-traumatic acute left knee pain and swelling associated with a warmth sensation 14 mo after TKA.
He had a history of hypertension, but was not regularly taking any anticoagulant or antiplatelet medication.
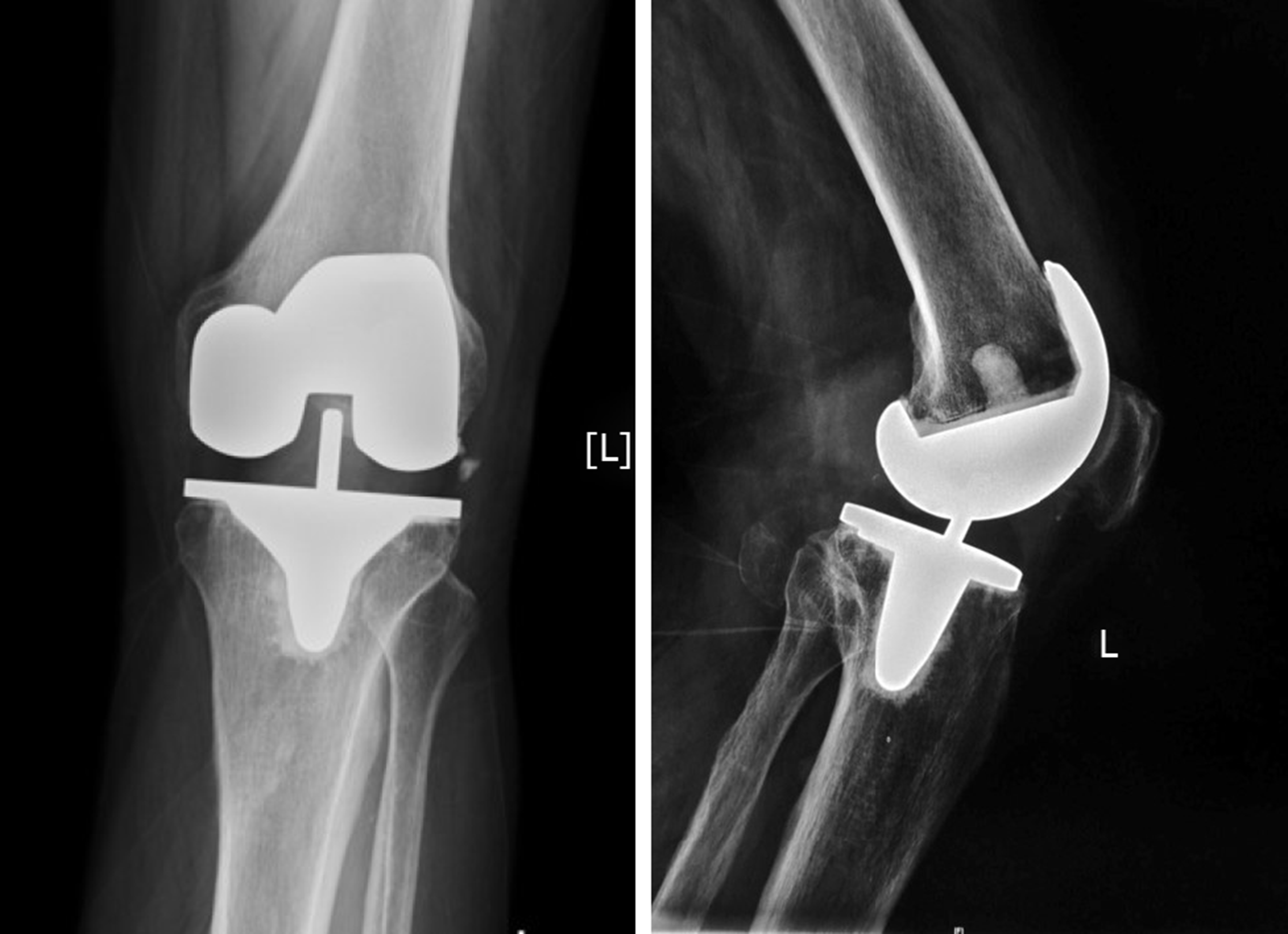
He had a bilateral knee pain due to end-stage primary knee osteoarthritis for over 10 years and underwent TKA of the left knee in 2013 after failure of conservative treatment. There were no complications intraoperatively. A pneumatic tourniquet was used during surgery at a pressure of 300 mmHg after exsanguination. The implant used was a Press Fit Condylar prosthesis P.F.C.® SIGMA® (DePuy Synthes, West Chester, United States). A single intra-articular drainage without blood recovery system was used, and was removed 24 h postoperatively. The drainage volume was 300 mL. Postoperative rehabilitation was uneventful, and the outcome was satisfactory. Thromboprophylaxis was administered with sodium enoxaparin (6100 IU per day), starting on the day of surgery and lasting 2 wk. The patient was discharged on postoperative day 7. Clinical tests and radiographs were normal 3 mo after TKA. The range of motion of the left knee was 0° extension to 125° flexion, and the femorotibial angle was 178°. The Hospital for Special Surgery Scoring System (HSS) score improved from 50 points to 96 points (with 30 points of pain, 20 points of function, 16 points of mobility, 10 points of force, 10 points of deformity and 10 points of stability). The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score reduced from 62 points to 7 points. However, 14 mo postoperatively, the patient experienced acute pain in the left knee while he was sleeping. This onset of pain was associated with immediate swelling of the knee and a sensation of warmth in the area of pain.
Local findings in the left knee showed that the range of motion was limited to 0° extension and 80° flexion, with positive patellar ballottement and no knee instability. The HSS score had decreased to 71 points and the WOMAC score was 55 points.
Aspiration of the knee joint yielded 40 mL of dark, bloody fluid (Figure 1). No organisms were isolated, and culture was negative for bacteria over a 72-h period. Culture was sent only once to microbiology because the patient’s symptoms were disappeared 10 h after non-surgical treatment was implemented.
The diagnosis of the presented case is hemarthrosis after TKA.
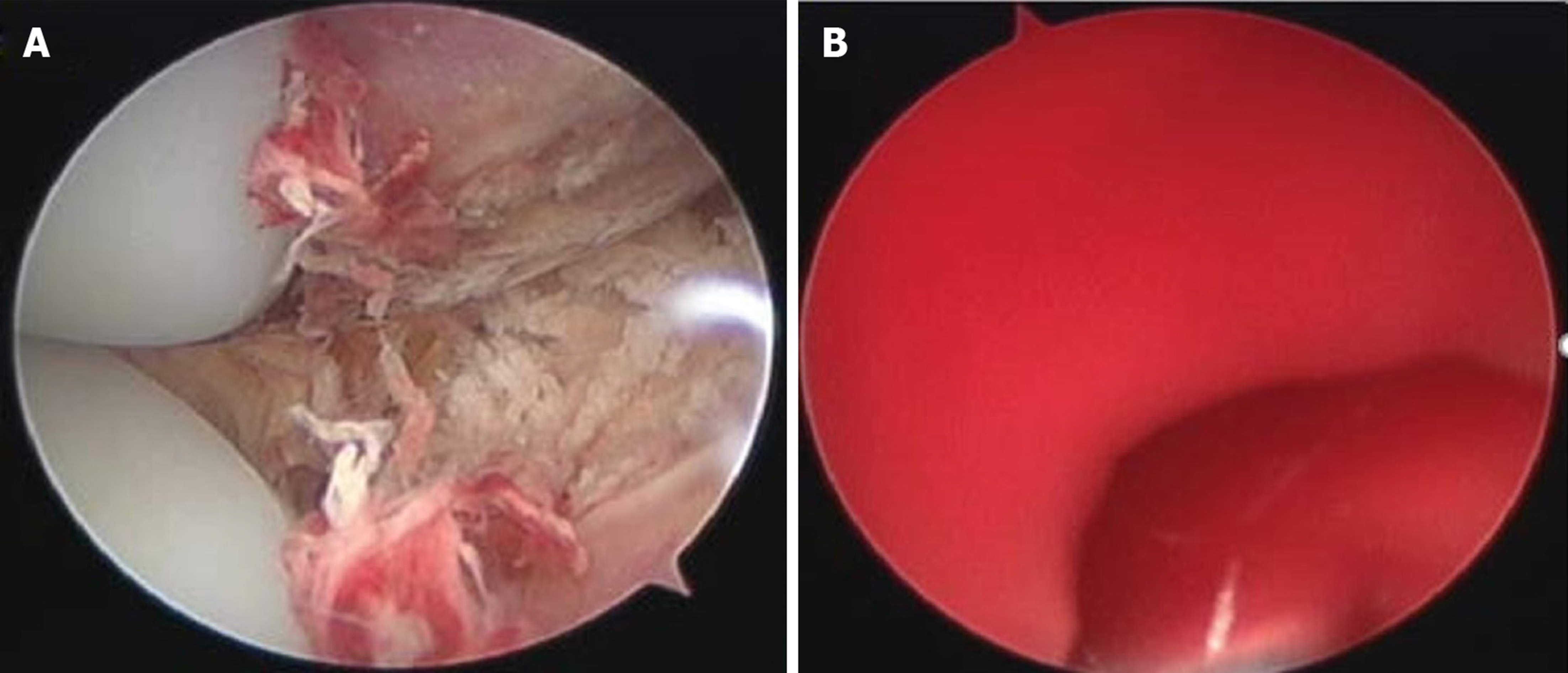
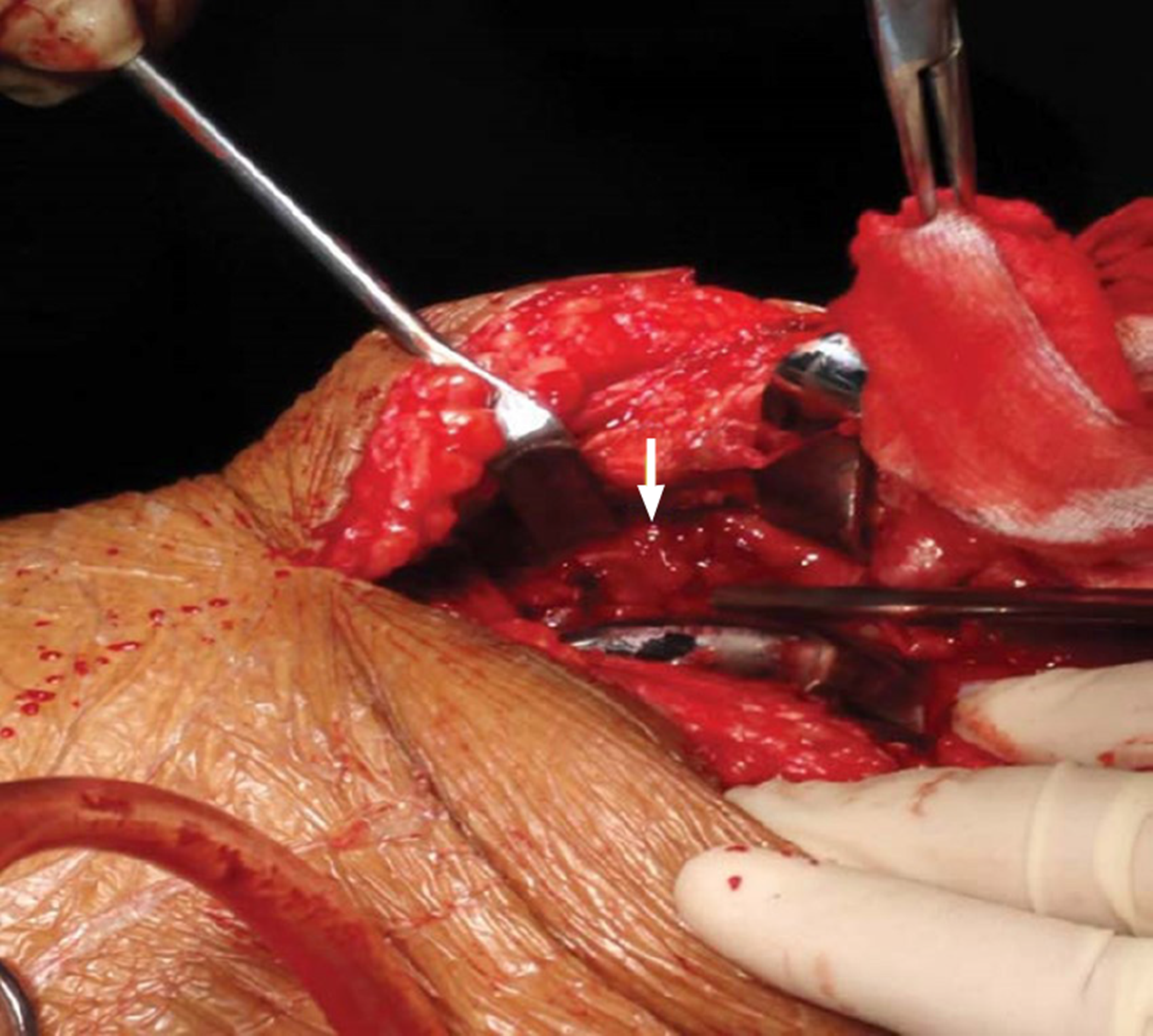
At the beginning, the patient received non-surgical treatment including compression, cryotherapy and immobilization was. The symptoms resolved 10 h later and he could walk home. But repeated similar episodes occurred in the following 2 mo. The patient was finally diagnosed with recurrent hemarthrosis after TKA. The patient presented to our department for definitive diagnosis and treatment, and arthroscopic exploration was performed. A tourniquet was initially used. After thorough lavage of the joint, there was no visible bleeding (Figure 3A). However, progressive hemorrhage blurred the view soon after releasing the tourniquet, and it was difficult to determine the source of the bleeding (Figure 3B). Therefore, open exploration was performed. Pulsatile bleeding was discovered in the medial sulcus close to the upper pole of the patella (Figure 4). The bleeding artery was about 1–1.5 mm in diameter. According to the anatomy of the knee and the structure of the blood vessel, the bleeding source was identified as the medial superior genicular artery. The artery was ligated with three sutures. There was no sign of bleeding during intraoperative flexion and extension of the knee.
The patient was symptom-free in the 15 mo after surgery. The left knee had a range of motion of 0° extension to 120° flexion, and the standing femorotibial angle was 177°. The HSS score returned to 92 points and the WOMAC score was 5 points in 24 mo after surgery. We also followed up the patient at 48 mo after surgery through video communication since he could not come back to our hospital. At that time, the WOMAC sore remained 5 points and knee function were perfect (Figure 5).
More recently, Ravi et al[6] reviewed previous literatures and suggested that the potential causes of recurrent hemarthrosis after TKA varied and involved systemic, local and iatrogenic etiologies. They also described an algorithm for the diagnosis and treatment of recurrent hemarthrosis after TKA. It was reported previously that the blood vessel could be directly injured during procedures such as resection of the proximal tibia or posterior femoral condyles, posterior capsule release, posterior cruciate ligament removal, and screw insertion[8]. In addition, a low power injury can cause the formation of an arteriovenous fistula, arterial aneurysm, or pseudoaneurysm, creating the potential for future blood vessel rupture[8-11]. Drexler et al[12] reported an atypical tibial defect in open surgery and biopsy results revealed high-grade epithelioid angiosarcoma, which was treated by amputation above the level of the knee. In addition, hemarthrosis may be caused by anticoagulation medication such as warfarin, aspirin, rivaroxaban, or clopidogrel[13]. Some rare causes like hemophilia, an inherited disease with a deficiency of factor VIII (hemophilia A) or factor IX (hemophilia B)[14,15], and PVNS, a proliferative tumor of synovial tissue, may also induce hemarthrosis[16-18]. Routine blood tests including inflammatory markers and a coagulation profile are essential in cases of swollen and painful knees after TKA[5]. In 1996, Worland et al[3] emphasized the necessity of aspiration as an important way to differentiate the cause of knee swelling after TKA. Ultrasound can present a luminal turbulence with a “Yin-Yang” sign which can easily detect arterial aneurysms, pseudoaneurysms, and arteriovenous fistulae[5]. Radiography can evaluate the position of components and determine whether the components are loose. Magnetic resonance imaging is valuable for detecting pathological changes of the synovium[19]. Angiography is a very useful method for diagnosing and treating recurrent hemarthrosis in both early and late cases. Vascularized synovium could present as a “tumor blush” sign in angiography[20]. All anticoagulant medication should be stopped after consultation with related experts. Cryotherapy, aspiration, and immobilization can resolve the symptoms and stop the bleeding temporarily or definitively[4,7]. Although some cases will fail in conservative therapy and require surgical therapy, non-surgical therapy should be given first[5]. Open surgical repair such as synovectomy is a direct approach to explore the bleeding area and ligate the blood vessel or remove the hypertrophic synovium[2,3]. However, open surgery is associated with operation-related complications such as iatrogenic injury, more blood loss, and longer rehabilitation. Arthroscopic synovectomy is a minimally invasive approach that allows dissection of hypertrophic synovium with less bleeding and trauma than open surgery. However, arthroscopic synovectomy is not always successful. Suzuki et al[21] reported a case of recurrent hemarthrosis in which the source of bleeding could not be determined in an unclear arthroscopic view, and was treated with open exploration, which was same as in our case. Therefore, angiographic embolization has been regarded as a more optimal choice in cases of vascular injury and of synovial impingement. Compared with open exploration and arthroscopic surgery, angiographic treatment is a less invasive therapy with lower risk of complications and easier rehabilitation[19,20]. In the present case, the patient did not undergo angiography, and the cause of the bleeding could not be determined preoperatively. In fact, the source of bleeding was suspected to be synovium impingement according to recently reported cases[5,7], and the ultrasound examination. However, open exploration revealed a bleeding artery, which strongly suggested that the cause of hemarthrosis was rupture of a pseudoaneurysm of the medial superior genicular artery. Arthroscopy was initially performed and was found to be inadequate compared with angiography. A clear scope is essential to determine the source of bleeding, unfortunately, it was difficult to visualize the effusion or jet point before the view became bloody.
The present case indicated the following perspectives. Firstly, angiography is essential in cases of hemarthrosis after TKA. Secondly, arthroscopy may not always be adequate as it may not provide a clear view. Lastly, traditional open exploration is still effective and sometimes necessary.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: De Martino I S-Editor: Wang JL L-Editor: Med-E Ma JY E-Editor: Liu JH
| 1. | Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61:173-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 448] [Cited by in RCA: 346] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Oishi CS, Elliott ML, Colwell CW. Recurrent hemarthrosis following a total knee arthroplasty. J Arthroplasty. 1995;10 Suppl:S56-S58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Worland RL, Jessup DE. Recurrent hemarthrosis after total knee arthroplasty. J Arthroplasty. 1996;11:977-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Ohdera T, Tokunaga M, Hiroshima S, Yoshimoto E, Matsuda S. Recurrent hemarthrosis after knee joint arthroplasty: etiology and treatment. J Arthroplasty. 2004;19:157-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Saksena J, Platts AD, Dowd GS. Recurrent haemarthrosis following total knee replacement. Knee. 2010;17:7-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Ravi B, Hosack L, Backstein D, Spangehl M. Recurrent Hemarthrosis After Total Knee Arthroplasty: Evaluation and Treatment. J Am Acad Orthop Surg. 2019;27:652-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Kindsfater K, Scott R. Recurrent hemarthrosis after total knee arthroplasty. J Arthroplasty. 1995;10 Suppl:S52-S55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Ibrahim M, Booth RE, Clark TW. Embolization of traumatic pseudoaneurysms after total knee arthroplasty. J Arthroplasty. 2004;19:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Sharma H, Singh GK, Cavanagh SP, Kay D. Pseudoaneurysm of the inferior medial geniculate artery following primary total knee arthroplasty: delayed presentation with recurrent haemorrhagic episodes. Knee Surg Sports Traumatol Arthrosc. 2006;14:153-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Cunningham RB, Mariani EM. Spontaneous hemarthrosis 6 years after total knee arthroplasty. J Arthroplasty. 2001;16:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Huang CH, Ho FY, Cheng CT, Ma HM. Hemarthrosis associated with failure of a mobile meniscal-bearing total knee arthroplasty. A case report. J Bone Joint Surg Am. 2003;85:2445-2448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Drexler M, Dolkart O, Amar E, Pritsch T, Dekel S. Late recurrent hemarthrosis following knee arthroplasty associated with epithelioid angiosarcoma of bone. Knee. 2010;17:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Takezawa Y, Arai Y, Fujita S, Yamagami T, Tanaka O, Kubo T. A case of selective arterial embolization for recurrent hemarthrosis after total knee arthroplasty. J Orthop Sci. 2013;18:679-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Silva M, Luck JV. Radial head excision and synovectomy in patients with hemophilia. Surgical technique. J Bone Joint Surg Am. 2008;90 Suppl 2 Pt 2:254-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Chin KR, Barr SJ, Winalski C, Zurakowski D, Brick GW. Treatment of advanced primary and recurrent diffuse pigmented villonodular synovitis of the knee. J Bone Joint Surg Am. 2002;84:2192-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 117] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 16. | Hamlin BR, Duffy GP, Trousdale RT, Morrey BF. Total knee arthroplasty in patients who have pigmented villonodular synovitis. J Bone Joint Surg Am. 1998;80:76-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Rukavina A, Kerkhoffs GM, Schneider P, Kuster MS. Recurrent hemarthrosis after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:898-900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Weidner ZD, Hamilton WG, Smirniotopoulos J, Bagla S. Recurrent Hemarthrosis Following Knee Arthroplasty Treated with Arterial Embolization. J Arthroplasty. 2015;30:2004-2007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Bagla S, Rholl KS, van Breda A, Sterling KM, van Breda A. Geniculate artery embolization in the management of spontaneous recurrent hemarthrosis of the knee: case series. J Vasc Interv Radiol. 2013;24:439-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Karataglis D, Marlow D, Learmonth DJ. Atraumatic haemarthrosis following total knee replacement treated with selective embolisation. Acta Orthop Belg. 2006;72:375-377. [PubMed] |
| 21. | Suzuki M, Kakizaki J, Tsukeoka T, Tsuneizumi Y, Miyagi J, Moriya H. A case of spontaneous hemoarthrosis after a total knee arthroplasty. Mod Rheumatol. 2006;16:248-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |