Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.1944
Peer-review started: April 17, 2020
First decision: April 24, 2020
Revised: April 30, 2020
Accepted: May 16, 2020
Article in press: May 16, 2020
Published online: May 26, 2020
Processing time: 37 Days and 19 Hours
Even at present, we are in the middle of the novel coronavirus disease 2019 (COVID-19) pandemic and are facing challenges in trial and error. Presently, emergency surgery for patients with suspected COVID-19 is burdensome not only for patients but also for healthcare workers. Therefore, we established a surveillance system in the emergency room and established principles for managing patients suspected of COVID-19 who require emergency surgery.
A 67-year-old man was diagnosed with appendicitis in March 2020. His wife was diagnosed with COVID-19 10 d earlier, and the patient was in close contact with her. The patient tested negative twice on an upper respiratory COVID-19 reverse transcription–polymerase chain reaction screening test, but chest X-ray and chest computed tomography revealed patchy ground-glass opacity in both upper lobes of the patient’s lungs. The same emergency surgery procedure for patients with confirmed COVID-19 was applied to this patient suspected of having the disease to ensure that surgery was not delayed while waiting for the reverse transcription–polymerase chain reaction results. A few hours after surgery, the upper respiratory tract specimen taken in the emergency room was negative for COVID-19 but the lower respiratory tract specimen was found to be positive for the disease.
When COVID-19 is suspected, emergency surgery should be performed as for confirmed COVID-19 without delay.
Core tip: During the novel coronavirus disease 2019 (COVID-19) pandemic, if emergency surgery is required, both emergency surgery and infection control should be performed using personal protective equipment and negative-pressure equipment and facilities without waiting for the results of COVID-19 reverse transcription–polymerase chain reaction. Even if the results of the reverse transcription–polymerase chain reaction test are negative, if the medical history, symptoms, and X-ray findings indicate suspected COVID-19, all medical activities should be performed as they would for a confirmed case and samples should be repeatedly tested using various methods and at different locations.
- Citation: Kim C, Kim JK, Yeo IH, Choe JY, Lee JE, Kang SJ, Park CS, Kwon KT, Hwang S. Appendectomy in patient with suspected COVID-19 with negative COVID-19 results: A case report. World J Clin Cases 2020; 8(10): 1944-1949
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/1944.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.1944
The novel coronavirus disease 2019 (COVID-19) began in Wuhan, China, at the end of 2019 and spread rapidly across the country and worldwide. Thereafter, the World Health Organization declared it to be a pandemic[1]. In South Korea, the first confirmed case was reported in January 2020. The 31st patient became a super-spreader, and group infection quickly occurred in Daegu Metropolitan City. Daegu became a major center for the epidemic, accounting for approximately 70% of all COVID-19 cases in South Korea[2]. The experience with Middle East respiratory syndrome (MERS) taught us that managing infections in the emergency room (ER) is crucial[3]. However, when patient numbers increase rapidly, the infection management system collapses, leaving the ER and healthcare workers vulnerable to contamination because of scarce medical resources.
Several studies published after the severe acute respiratory syndrome or MERS pandemics have investigated how to prevent the spread of infection during general surgery[4]. However, most studies have focused on the management of elective surgical procedures, whereas only a few reports of emergency surgery have been published in China since the outbreak of COVID-19[5,6].
The present study reports successful appendectomy and infection control in a patient with appendicitis who was strongly suspected of having COVID-19. The results of previous repeated reverse transcription–polymerase chain reaction (RT-PCR) tests for COVID-19 had been negative, and a positive result was obtained only after surgery.
In March 2020, a 67-year-old man presented with right lower quadrant (RLQ) pain and vomiting.
He had visited a local medical clinic after complaining of RLQ pain and vomiting for 2 d. He was referred by ambulance to our hospital to undergo a test for appendicitis. On March 19 (at 9 p.m.) upon arrival, he was fully conscious but complained of severe RLQ pain and tenderness. He had no respiratory symptoms or fever.
He had hypertension, diabetes mellitus, hyperlipidemia, and chronic kidney disease.
The patient’s wife had been diagnosed with COVID-19 10 d earlier, and the patient was in close contact with her. The patient tested negative twice (10 and 8 d earlier) in upper respiratory COVID-19 RT-PCR screens performed at the public health center.
He had localized tenderness in the RLQ.
His vital signs were as follows: Blood pressure, 150/80 mmHg; heart rate, 80 beats/min; respiratory rate, 20/min; and body temperature, 37.2 °C. Laboratory data showed a significant white blood cell count of 8.8 × 109 cells/L, containing 72.7% neutrophils. Both the C-reactive protein level and erythrocyte sedimentation rates were elevated: 6.5 mg/L (reference: < 0.5 mg/dL) and 48 mm/h (reference: 0–10 mm/h), respectively. The coagulation test results were normal.
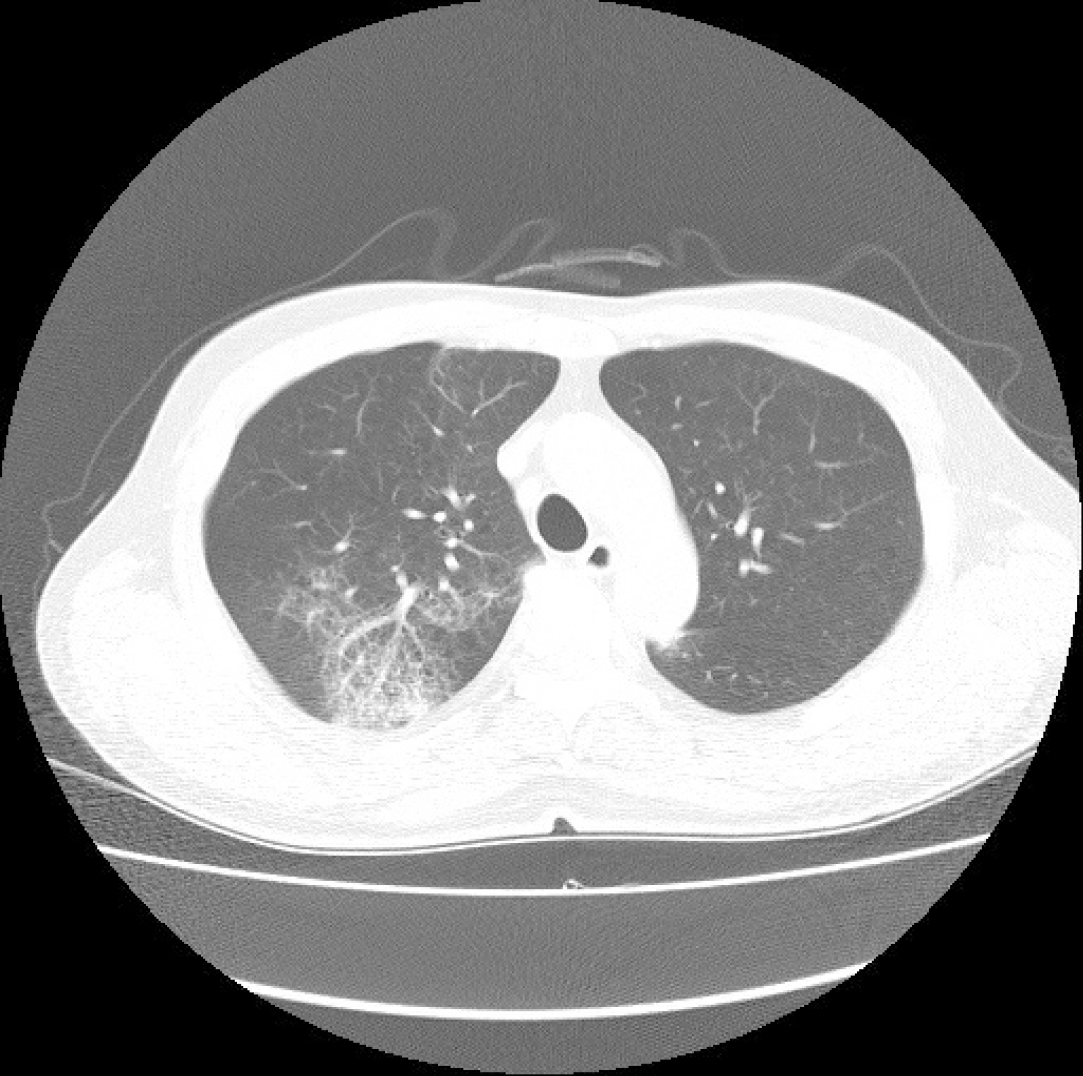
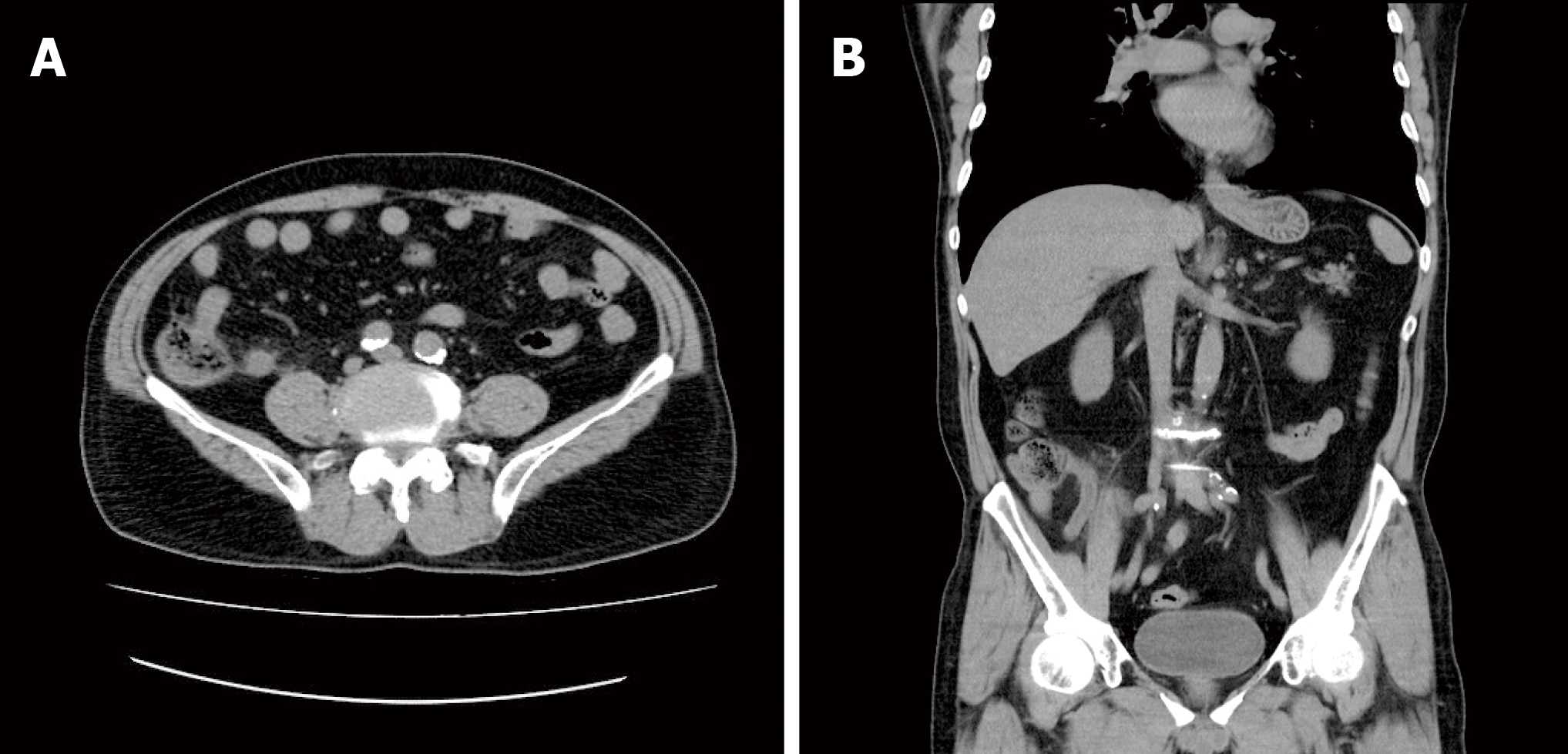
The patient had no respiratory symptoms, but COVID-19 RT-PCR screening and radiography of the chest were performed outside the ER according to the ER policy. The chest radiograph showed ground-glass opacity in the right upper lobe; therefore, the patient was immediately moved to an isolation room (Figure 1). Contrast-enhanced chest computed tomography (CT) revealed patchy ground-glass opacity in both upper lobes (Figure 2). An 11-mm dilatation of the appendix was confirmed on a non-contrast-enhanced abdomen CT image, and the patient was diagnosed with appendicitis (Figure 3).
The final diagnosis of the presented case was appendicitis with COVID-19 pneumonia. Histopathological analysis of the removed appendix revealed acute appendicitis.
Immediately after appendicitis was diagnosed, antibiotics - ceftriaxone and metronidazole - were administered intravenously. Although the patient’s previous COVID-19 RT-PCR test results were negative twice, he waited for surgery in an isolation room, and the surgeon wore personal protective equipment (PPE) comprising inner and outer gloves, an N95 respirator, eye shield/face shield/goggles, and a hooded coverall/gown before coming into contact with the patient to prepare for surgery. On March 20, 3 a.m., the patient was transferred to the operating room (OR) in a negative-pressure transfer device equipped with a negative-pressure air conditioning system. Two anesthesiologists, a nurse, and two surgeons wore PPE with powered air-purifying respirators. Endotracheal intubation was applied with a video-laryngoscope using rapid sequence induction. General anesthesia was maintained with desflurane and remifentanil. Laparoscopic appendectomy was performed to minimize patient fluid contact. The procedure was performed using three ports. According to the operative findings, the appendix was a pelvic type. Each procedure was performed carefully to avoid unnecessary scattering of fluid or aerosols. The peritoneal smoke generated during surgery was removed as much as possible using suction and air filters attached to the trocar. The entire appendix was extracted carefully and placed in a bag. We observed that the appendix was swollen and erythematous. However, there were no signs of perforation. Turbid peritoneal fluid was found near the appendix and in the pelvis. After surgery, the anesthesiologists planned to remove the endotracheal tube in the OR to minimize contamination, and the patient was extubated with continuous infusion of remifentanil to reduce coughing. Post-anesthetic care was performed in the OR for 30 min. The patient was placed in a negative-pressure transfer device and then admitted to a negative-pressure isolation facility in the intensive care unit (ICU). No personnel contacted the patient without wearing PPE between the quarantine area and ICU, and secondary transmission to the healthcare workers did not occur. On March 20, 10 a.m., a few hours after surgery, the samples taken in the ER were found to be negative for COVID-19 in the upper respiratory tract specimen (nasal and throat swab) but positive for COVID-19 in the lower respiratory tract specimen (sputum). Combinations of hydroxychloroquine, lopinavir/ritonavir, and darunavir/cobicistat were added to treat the COVID-19 infection.
The postoperative course was successful and without complication. There were no traces of fever or respiratory symptoms during hospitalization, and the patient was discharged 11 d after admission.
During the current COVID-19 outbreak, at-risk patients should be treated in the same manner as patients with confirmed infection. The experience and knowledge accumulated following the severe acute respiratory syndrome outbreak in 2003 and MERS in 2015 have ensured the safety of patients and medical staff and guided them in dealing with similar situations such as the COVID-19 pandemic[7]. However, it is very difficult to control and manage the escalating number of patients with relatively insufficient medical resources, and if all interest and resources are focused on COVID-19, a different emergency may be missed. However, because emergency cases cannot be treated in the same manner as they were before the COVID-19 outbreak, an approach appropriate to the type of emergency disease, the patient’s situation, and the hospital’s situation is necessary[8].
In accordance with hospital policy, regular non-emergency surgeries were delayed and these patients were required to visit a screening clinic 3 d before surgery to reduce the risk of nosocomial infection during the COVID-19 outbreak. Furthermore, all patients were required to undergo a COVID-19 RT-PCR screening test and chest radiography before entering the ER. If they had pneumonia, fever or respiratory symptoms, traveled abroad in the past 2 wk, or a history of contact with patients with COVID-19, they were quarantined until the RT-PCR results were obtained.
Clear guidelines are needed to prevent COVID-19 transmission and emergency surgeries; if the importance of either infection prevention or the requirement for emergency surgery is imbalanced, both can be missed. For patients in need of emergency surgery, a protocol has been established, i.e., to perform CT using a negative-pressure transport device even before COVID-19 is confirmed. The principles applied during the treatment of the patient with appendicitis were also applied while caring for patients with cerebral hemorrhage and intestinal perforation with suspected COVID-19 who visited the ER.
Recently, some guidelines for surgery complicated by COVID-19 have suggested that a trial of antibiotics can be considered for uncomplicated or early appendicitis based on the surgeon’s judgment and patient’s condition. However, operations should be performed if delaying the surgery is likely to prolong the hospital stay, increase the likelihood of later hospital admission, or cause harm to the patient[9,10]. Hospitalization was essential owing to the rapid progression of the COVID-19 pneumonia, the wide range of the pneumonia, and the distance between hospitals and homes. Furthermore, continuous self-isolation was necessary; hence, it was decided to perform emergency appendectomy considering that long-term hospitalization would be needed. Following receipt of the transfer inquiry, the departments of surgery, anesthesiology, emergency medicine, and infection control planned his isolation and postoperative ICU care in a meeting prior to the patient’s arrival. Because of the patient’s close contact with a COVID-19-positive patient and typical chest CT findings, the previous two negative COVID-19 results were ignored and the patient was treated as being COVID-19-positive. If COVID-19 is strongly suspected even if repeated upper respiratory tract test results are negative, it is necessary to repeat the test and obtain a different sample before releasing the person from quarantine because the result may be false negative.
In the early stages of COVID-19 infection, the virus primarily colonizes the upper respiratory tract but with time moves into the lower respiratory tract. Therefore, a lower respiratory tract examination using sputum should be performed as the infection progresses[11]. In addition, studies have shown that urine or stool samples are useful for testing pediatric patients or patients with no respiratory symptoms[12].
During the COVID-19 outbreak, the principles applied to emergency surgery for infected patients should be applied to both suspected and confirmed cases. In addition, emergency surgery should not be postponed due to a delay in obtaining COVID-19 test results. Prior consultation is required between experts in various fields, including infection control, surgery preparation, patient transfer, OR management, anesthesia, and surgery. Guidelines for emergency surgery in patients with COVID-19 should be prepared in advance according to the hospital environment and the patient’s special circumstances.
We thank Professor Gyu-Seog Choi for assistance with surgery arrangements.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Norčič G S-Editor: Wang JL L-Editor: A E-Editor: Wu YXJ
| 1. | Mahase E. Covid-19: WHO declares pandemic because of "alarming levels" of spread, severity, and inaction. BMJ. 2020;368:m1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 387] [Article Influence: 77.4] [Reference Citation Analysis (0)] |
| 2. | Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the Epidemiological Features of Coronavirus Disease 2019 (COVID-19) Outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35:e112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 276] [Cited by in RCA: 283] [Article Influence: 56.6] [Reference Citation Analysis (0)] |
| 3. | Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, Lee JY, Kim JM, Kang CI, Jo IJ, Ryu JG, Choi JR, Kim S, Huh HJ, Ki CS, Kang ES, Peck KR, Dhong HJ, Song JH, Chung DR, Kim YJ. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388:994-1001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 237] [Cited by in RCA: 246] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 4. | Park J, Yoo SY, Ko JH, Lee SM, Chung YJ, Lee JH, Peck KR, Min JJ. Infection Prevention Measures for Surgical Procedures during a Middle East Respiratory Syndrome Outbreak in a Tertiary Care Hospital in South Korea. Sci Rep. 2020;10:325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 5. | Kang X, Zhang R, He H, Yao Y, Zheng Y, Wen X, Zhu S. [Anesthesia management in cesarean section for a patient with coronavirus disease 2019]. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49. [PubMed] |
| 6. | Si Y, Sun XF, Zhong M, Yue JN, Fu WG. [Countermeasures and treatment for aortic acute syndrome with 2019 coronavirus disease]. Zhonghua Wai Ke Za Zhi. 2020;58:178-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Kim JY, Song JY, Yoon YK, Choi SH, Song YG, Kim SR, Son HJ, Jeong SY, Choi JH, Kim KM, Yoon HJ, Choi JY, Kim TH, Choi YH, Kim HB, Yoon JH, Lee J, Eom JS, Lee SO, Oh WS, Choi JH, Yoo JH, Kim WJ, Cheong HJ. Middle East Respiratory Syndrome Infection Control and Prevention Guideline for Healthcare Facilities. Infect Chemother. 2015;47:278-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 8. | Paek SH, Kim DK, Lee JH, Kwak YH. The Impact of Middle East Respiratory Syndrome Outbreak on Trends in Emergency Department Utilization Patterns. J Korean Med Sci. 2017;32:1576-1580. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | American College of Surgeons. COVID-19 Guidelines for Triage of Emergency General Surgery Patients. Available from: https://www.facs.org/covid-19/clinical-guidance/elective-case/emergency-surgery. |
| 10. | Royal College of Surgeons of England. Updated Intercollegiate General Surgery Guidance on COVID-19. Available from: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2. |
| 11. | To KK, Tsang OT, Chik-Yan Yip C, Chan KH, Wu TC, Chan JMC, Leung WS, Chik TS, Choi CY, Kandamby DH, Lung DC, Tam AR, Poon RW, Fung AY, Hung IF, Cheng VC, Chan JF, Yuen KY. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;ciaa149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1052] [Cited by in RCA: 1119] [Article Influence: 223.8] [Reference Citation Analysis (0)] |
| 12. | Tang A, Tong ZD, Wang HL, Dai YX, Li KF, Liu JN, Wu WJ, Yuan C, Yu ML, Li P, Yan JB. Detection of Novel Coronavirus by RT-PCR in Stool Specimen from Asymptomatic Child, China. Emerg Infect Dis. 2020;26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 323] [Cited by in RCA: 368] [Article Influence: 73.6] [Reference Citation Analysis (0)] |