Published online Jan 6, 2020. doi: 10.12998/wjcc.v8.i1.68
Peer-review started: August 8, 2019
First decision: October 14, 2019
Revised: November 10, 2019
Accepted: November 14, 2019
Article in press: November 14, 2019
Published online: January 6, 2020
Processing time: 151 Days and 20.5 Hours
Hilar cholangiocarcinoma is the most common malignant tumor of the extrahepatic bile duct. Until now, radical resection has been the most effective method for the long-term survival of patients with the disease. However, many problems have emerged in the field of hepatobiliary surgery for a long time, including complex surgical procedures, low resection rate, and postoperative complications. We have adopted the “multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a bile duct lake“ technique in the treatment of hilar cholangiocarcinoma since 2008, and obtained satisfactory short- and long-term results.
To examine the feasibility of the application of multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a bile duct lake in the operation of hilar cholangiocarcinoma.
A retrospective analysis was performed for the clinical data, surgical methods, and results of 76 patients with hilar cholangiocarcinoma who were treated with hilar bile duct lake-forming multiple Roux-en-Y hepaticojejunostomy reconstruction at Gansu Provincial Hospital.
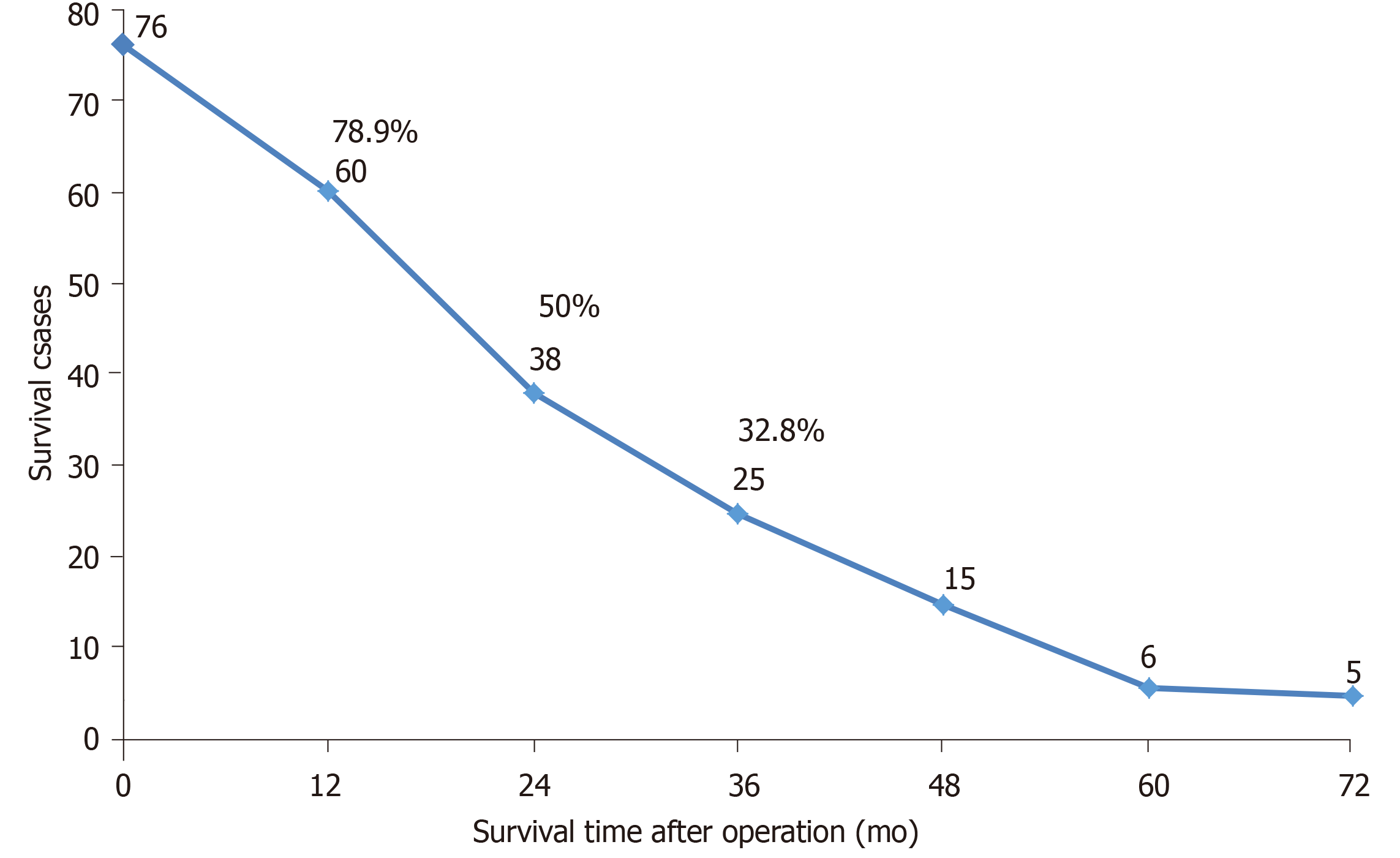
In all 76 cases, the operation was successful and no operative death occurred. The mean (range) operation time was 215.4 ± 53.5 min (124–678 min), and the amount of bleeding during the operation was 428.2 ± 63.8 mL (240–2200 mL). The overall 1-year survival rate was 78.9%, and the 3-year survival rate was 32.8%.
The multiple Roux-en-Y hepaticojejunostomy reconstruction technique with formation of a bile duct lake is safe and effective for the surgical treatment of hilar cholangiocarcinoma.
Core tip: Hilar cholangiocarcinoma accounts for approximately 50% of all cholangiocarcinomas. Until now, radical resection has been the most effective method for the long-term survival of patients with the disease. However, many problems have emerged in the field of hepatobiliary surgery over time, including complex surgical procedures, low resection rates, and postoperative complications. We have adopted the "multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a bile duct lake" technique in the treatment of hilar cholangiocarcinoma since 2008, and obtained satisfactory short- and long-term results.
- Citation: Yang XJ, Dong XH, Chen SY, Wu B, He Y, Dong BL, Ma BQ, Gao P. Application of multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of bile hilar duct lake in the operation of hilar cholangiocarcinoma. World J Clin Cases 2020; 8(1): 68-75
- URL: https://www.wjgnet.com/2307-8960/full/v8/i1/68.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i1.68
As the most common malignant tumor of the extrahepatic bile duct, hilar cholangiocarcinoma accounts for approximately 50% of all cholangiocarcinomas[1]. Until now, radical resection has been the most effective method for the long-term survival of patients with the disease. However, many problems have emerged in the field of hepatobiliary surgery over time, including complex surgical procedures, low resection rates, and postoperative complications. Besides radiological resectability assessment and preoperative biliary drainage, the primary problem that needs to be considered before and after tumor resection is the reconstruction of biliary intestinal anastomosis, in addition to vascular resection and reconstruction[2]. For most Bismuth type I hilar cholangiocarcinomas, anastomosis is relatively simple because of only one opening in the hilum; even if two openings are sometimes present, an opening can even form as a result of simple plastic surgery. However, this is different for type II, III, and IV hilar cholangiocarcinomas, as anastomosis is extremely difficult because as many as ten bile duct openings have been found in the hilum.
In this case, many surgeons use hilar plate-jejunum anastomosis, which sutures the jejunum with the liver tissue around the opening of multiple secondary or more bile ducts; however, the incidence rates of bile leakage, infection, and anastomotic stenosis are higher after this anastomosis is applied[3-5]. Some researchers use basin-like anastomosis; that is, they suture multiple bile duct openings to each other, forming a larger basin-like opening, which is then anastomosed with the jejunum[6,7]. Although anastomosis has few complications, it can only be applied to cases where only two or three bile duct openings are present in the portahepatis. If greater than four (even up to eight or nine) bile duct openings are present, suturing them together is almost impossible. In view of this situation, we have adopted the “multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a bile duct lake” technique in the treatment of hilar cholangiocarcinoma since 2008, and obtained satisfactory short- and long-term results. Herein, we present the results of our retrospective analysis.
The subjects included 76 patients with hilar cholangiocarcinoma, of whom 47 were men and 29 were women, who were hospitalized and underwent operation in the Department of General Surgery of Gansu Provincial Hospital between January 2008 and October 2016. The mean age was 56.3 ± 11.7 years (range, 39–84 years). Gross jaundice was found in 65 patients (85.5%), and upper abdominal discomfort was found in 43 patients (56.6%). Sixteen patients (21.1%) had asthenia and weakness, and eight (10.5%) had chills and fever. The serum total bilirubin level increased in 76 patients (100%), with a mean (range) of 238.3 ± 76.5 mmol/L (47–542 mmol/L). The mean preoperative jaundice time was 22.6 ± 5.4 d (9–87 d). Five patients had cirrhosis, eight had intrahepatic and extrahepatic stones and cholecystolithiasis, and five had a previous history of biliary tract surgery. All 76 patients were examined for tumor markers. Seventy patients (92.1%) had an abnormal CA199 level (>37 U/mL), which was >1000 U/mL in 51 patients (67.1%). All patients underwent B-mode ultrasonography, computed tomography (CT), and magnetic resonance cholangio-pancreatography (MRCP) examinations, showing intrahepatic bile duct dilatation in 63 patients (82.9%), and hilar and bile duct occupancy in 76 patients (100%). According to the Bismuth-Corlette classification, six cases were type I; 19, type II; 21, type IIIa; 16, type IIIB; and 14, type IV.
Preoperative jaundice reduction and supportive treatment: According to the severity of obstructive jaundice, the patients with preoperative total bilirubin levels of >200 mmol/L were routinely treated with PTCD. The reduction time was 5–15 d, with a mean of 10.2 ± 3.1 d. At the same time, jejunal nutrition tube bile transfusion and hepatoprotective treatment were administered, and if patients with gastrointestinal dysfunction were unable to eat, parenteral nutrition support was provided.
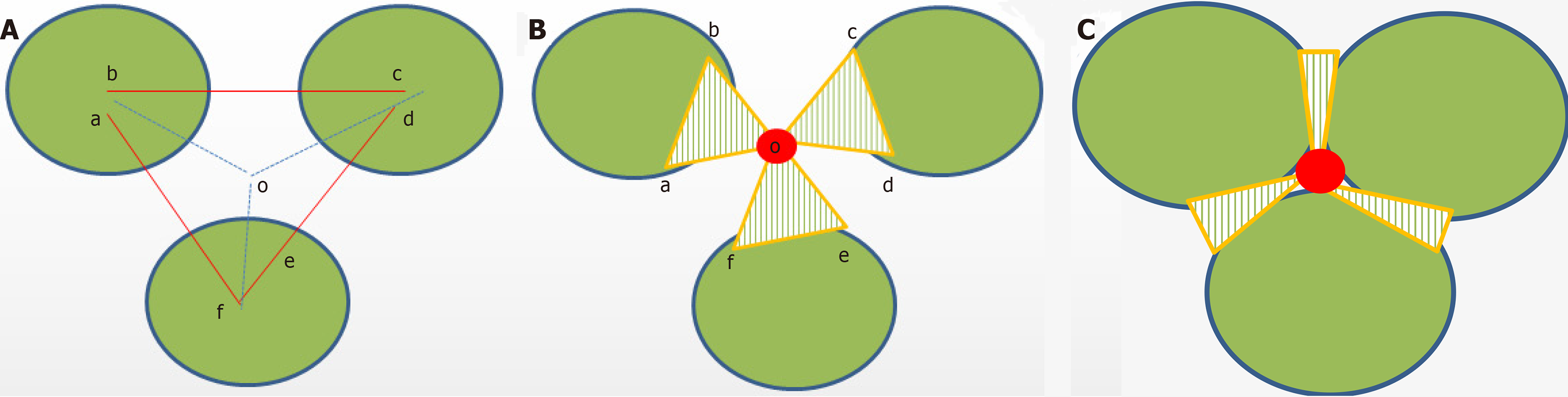
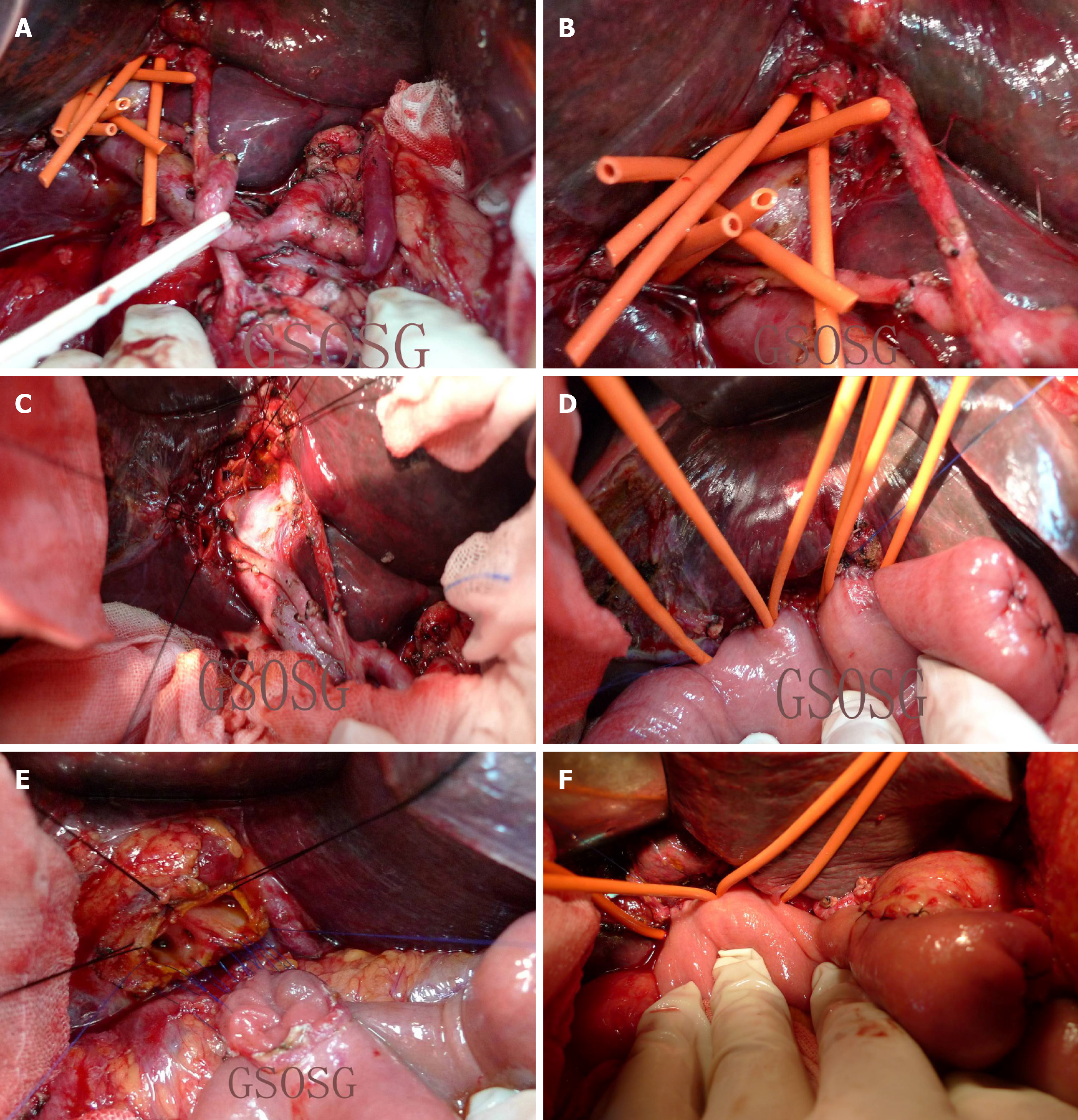
Surgical methods: Preoperative imaging data (including B-mode ultrasonography, CT, and MRCP) and intraoperative Bismuth-Corlette classification were used in combination with the patient’s general condition to determine the surgical method. The standard procedure was cholecystectomy + extrahepatic bile duct excision + hepatoduodenal ligament vascularized lymph node dissection + hilar cholangioplasty + bile duct-jejunum Roux-en-Y anastomosis. On this basis, 19 Bismuth type II cases and 16 type IIIB cases were treated with left hemihepatectomy or left caudate lobectomy; 21 type IIIa cases were treated with right hemihepatectomy or right caudate lobectomy; and 14 type IV cases were treated with left/right trilobectomy plus total caudate lobectomy. Hepatic artery reconstruction was performed in 24 patients; portal vein reconstruction, in 23 cases; and portal vein reconstruction, in 13 patients. Another six patients were treated with pancreaticoduodenectomy due to invasion of the pancreatic head. Cholangioplasty and reconstruction were performed after resection of the lesion and lymph node dissection, in which 2–4 hilar bile duct openings were formed into one bile duct lake; 3–7 bile duct openings into two bile duct lakes; and 6–9 bile duct openings into three bile duct lakes. Biliary duct formation and cholangiojejunal anastomosis were sutured continuously with 5–0 Prolene. The first step was to determine the number of bile duct lakes according to the number and location of the bile duct openings found on the section of the residual liver in the hilar region after R0 radical resection and lymph node dissection. Second, the end of the bile duct was trimmed, and the adjacent two or three bile duct intervals were wedged to maximize the opening of each branch of the bile duct, and then the adjacent bile duct openings were sutured with 5-0 Prolene (Figure 1). Finally, 1–3 common bile duct openings were assembled, and multiple Roux-en-Y hepaticojejunostomy reconstructions by formation of a bile duct lake were performed (Figure 2). The numbers of bile duct lake formations and vascular reconstructions in the different Bismuth type cases are shown in Table 1. Two of the latex tube drainages were placed behind the anastomosis and liver cut surface. The drainage tube was removed 3–7 d after the operation.
| Number of bile duct lakes | Number of bile duct openings | Bismuth type | Vascular reconstruction | ||||
| I | II | IIIa + IIIIb | IV | Portal vein | Hepatic artery | ||
| 1 | 2–4 | 6 | 9 | 7 | 0 | 6 | 8 |
| 2 | 3–7 | 0 | 10 | 21 | 3 | 8 | 10 |
| 3 | 6–9 | 0 | 0 | 9 | 11 | 9 | 6 |
All surgeries were performed after the patient or their relatives signed the informed consent form. This study was approved by the ethics committee of Gansu Provincial Hospital (2019-145).
Postoperative adjuvant chemotherapy: After 10–14 d of operation, 66 patients (86.8%) were treated with 4–6 cycles of the standardized therapy (oxaliplatin + gemcitabine) after the stitches were removed and gastrointestinal function had recovered.
All 76 cases were confirmed as hilar cholangiocarcinoma by pathological examination, including four cases of papillary carcinoma, 18 cases of well-differentiated adenocarcinoma, 45 cases of moderately and poorly differentiated adenocarcinoma, and nine cases of signet ring cell carcinoma. Postoperative pathological examination revealed that 53 cases (69.7%) were positive for lymph node metastasis of the hepatoduodenal ligament. The mean (range) number of lymph node metastasis was 4.6 ± 2.1 (3–16), and the remaining 23 patients had no lymph node metastasis. Of the cases, 49 had nerve involvement and 23 had an intravascular tumor thrombus. The mean (range) operative time was 215.4 ± 53.5 min (124–678 min). Intraoperative blood loss was 428.2 ± 63.8 mL (range, 240–2200 mL). Four cases of abdominal hemorrhage occurred after operation, of which three were treated conservatively with blood transfusions and hemostasis, and one was treated with a second operation (common hepatic artery hemorrhage). Nineteen cases with transient bile leakage were cured by peritoneal drainage for 9.4 ± 3.7 d (range, 7–21 d). Pleural effusion and/or ascites occurred in 35 cases (46.1%), all of which were cured after albumin infusion and diuretic treatment. No intraoperative deaths occurred, and three postoperative deaths occurred, including one patient with liver dysfunction, one patient with severe pulmonary infection, and one patient with systemic failure. Fifty-six patients had complete follow-up data. Survival curves are shown in Figure 3. The overall 1- and 3-year survival rates were 78.9% and 32.8%, respectively.
Like Goldbach’s conjecture, hilar cholangiocarcinoma is also known as the “pearl on the crown of the department of hepatobiliary surgery.” Therefore, surgeons who have the courage and ability to perform hilar cholangiocarcinoma surgery are worthy of respect. At present, the surgical procedures for hilar cholangiocarcinoma are basically in accordance with the principles of the academician Huang[8], including extrahepatic bile duct resection plus vascular skeletonization of the hepatoduodenal ligament for lymphoid tissue dissection, combined with left or right hepatic lobe (combined with caudate lobe) resection and hepatojejunostomy. If the portal vein or hepatic artery is invaded, it can be reconstructed by portal vein or hepatic artery R0 resection. The surgical procedure was based on the Bismuth classification as follows: The confluence of the left and right hepatic duct resections was performed for type I cases, combined with left and right hepatic duct formation plus Roux-en-Y hepaticojejunostomy reconstruction. For type II, IIIa, or type IV, right trilobectomy was necessary and combined with caudate lobectomy if the caudate lobe was invaded. For type IIIb, left hepatectomy was often required[9].
Resection and reconstruction are two basic components of radical resection of hilar cholangiocarcinomas, and both influence and restrain each other. In addition, to complete R0 resection of hepatic bile duct lesions and vascular skeletonization of the hepatoduodenal ligament for lymphoid tissue dissection, the difficulty of radical resection of the hilar cholangiocarcinoma is related to vascular resection and reconstruction, as well as bilioenteric anastomosis reconstruction. Nearly 80% of patients with hilar cholangiocarcinomas have vascular invasion, most of which are portal vein invasion, and some are combined with hepatic artery invasion[10]. With the advancement of surgical technology, especially vascular surgery techniques, the concept of surgery has also been updated. Several studies have confirmed that portal vein/hepatic artery resection and reconstruction can improve the R0 resection rate and prognosis of patients with hilar cholangiocarcinoma[11-16]. Of the 76 patients in this study, 24 underwent hepatic artery reconstruction; 23, portal vein reconstruction; and 13, hepatic artery combined with portal vein reconstruction.
In addition, owing to the deep location of the portahepatis, narrow space, and more ends of the bile duct on the residual liver surface after the lesion was resected at a high position, hepatic-jejunal anastomosis technology has become one of the greatest technical challenges in surgery. In this case, end-to-end anastomosis of all levels (2, 3, or even 4) of the bile duct and jejunal mucosa in each section was almost impossible. In view of this situation, professor Wu[6] established the basin-like Roux-en-Y cholangiojejunostomy for the radical resection of hilar cholangiocarcinoma in 1988. The grade 1–3 hepatic duct ends that had been cut were put together and reconstructed to form a wide hepatobiliary cavity, which was called “hepatobiliary duct basin,” and then anastomosed with the jejunum. Academician Chen Xiaoping improved the anastomosis method in 2008[4]. First, the posterior walls of the bile duct opening and jejunal loop incision were sutured intermittently. After suturing the posterior wall, the anterior wall of the jejunal loop incision was sutured with a U-shaped suture to the liver above the bile duct opening. Some scholars further simplify the operation method and adopt the method of suturing the jejunum loop to the hepatic capsule and hepatic portal vascular sheath. This method is simple and easy to master, but has also many shortcomings such as bile leakage, infection, and anastomotic stenosis[17,18].
Since 2008, we have made further improvements on the basis of the basin-like Roux-en-Y cholangiojejunostomy, and named it “multiple Roux-en-Y hepatico-jejunostomy reconstruction by formation of a hilar bile duct lake.” Thereby, a single “basin” is improved to 1–3 “lakes,” making cholangioplasty and biliointestinal anastomosis relatively easy. Furthermore, the tension formed by splicing and suturing can also make the broken end of the bile duct open, conducive to the smooth drainage of the bile, thus reducing the risk of late biliary stricture. At the same time, biliary plasty and continuous suture during the formation of a bile duct lake can also play a hemostatic role, reducing the incidence of postoperative biliary bleeding. The mean operation time in 76 patients was 215.4 min. Among the patients, 22 underwent one bile duct lake formation; 34, formation of two bile duct lakes; and 20, formation of three bile duct lakes. The intraoperative blood loss was 428.2 ± 63.8 mL. Postoperative complications occurred in 23 patients, including four with abdominal hemorrhage and 19 with bile leakage. No intraoperative death occurred. The overall 1- and 3-year survival rates were 78.9% and 32.8%, respectively. Therefore, the “multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a hilar bile duct lake” technique is safe and effective to use in the surgical treatment of hilar cholangiocarcinoma, which provides a reasonable choice for biliary surgeons to perform cholangio-jejunostomy reconstruction in the radical operation of hilar cholangiocarcinoma.
Hilar cholangiocarcinoma is the most common malignant tumor of the extrahepatic bile duct. Up to now, radical resection has been the most effective method for the long-term survival of patients with this disease. However, many problems have emerged in the field of hepatobiliary surgery over time, including complex surgical procedures, low resection rates, and postoperative complications. We have adopted the “multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of bile duct lake“ technique in the treatment of hilar cholangiocarcinoma since 2008, and obtained satisfactory short- and long-term results.
To provide a reasonable choice for biliary surgeons to perform cholangiojejunostomy reconstruction in the radical operation of hilar cholangiocarcinoma.
To examine the feasibility of the application of multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a bile duct lake in the operation of hilar cholangiocarcinoma.
A retrospective analysis was performed for the clinical data, surgical methods, and results of 76 patients with hilar cholangiocarcinoma who were treated with hilar bile duct lake-forming multiple Roux-en-Y hepaticojejunostomy reconstruction at Gansu Provincial Hospital.
All 76 patients were successfully treated surgically, and no operative death occurred. The mean (range) operation time was 215.4 ± 53.5 min (124–678 min), and the amount of intraoperative bleeding was 428.2 ± 63.8 mL (240–2200 mL). The overall 1- and 3-year survival rates were 78.9% and 32.8%, respectively.
Multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a bile duct lake is safe and effective to use in the operation of hilar cholangiocarcinoma.
The “multiple Roux-en-Y hepaticojejunostomy reconstruction by formation of a hilar bile duct lake” technique is safe and effective to use in the surgical treatment of hilar cholangiocarcinoma, and thus provides a reasonable choice for biliary surgeons to perform cholangiojejunostomy reconstruction in the radical operation of hilar cholangiocarcinoma.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mocchegiani F S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Xing YX
| 1. | DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, Choti MA, Yeo CJ, Schulick RD. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007;245:755-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 882] [Cited by in RCA: 1015] [Article Influence: 56.4] [Reference Citation Analysis (1)] |
| 2. | Yu XH, Liu C. Key Technologies of Surgical Treatment for Hilar Cholangiocarcinoma. Gandan Waike Zazhi. 2017;25:170-171. |
| 3. | Liu C, Jiang XQ. Possibility of Radical Resection of Hilarcholangiocarcinoma. Zhongguo Puwai Jichu and Linchuang Zazhi. 2016;23:1299-1303. [DOI] [Full Text] |
| 4. | Chen XP, Zhang ZW, Huang ZY, Chen YF, Zhang WG, Qiu FZ. Improvement of Biliary Reconstruction after Resection of Hilarcholangiocarcinoma. Zhonghua Waike Zazhi. 2008;46:634-635. [DOI] [Full Text] |
| 5. | He XD, Liu W, Tao LY, Zhang ZH, Cai L, Zhang SM. Clinical Value of Hilar Button Anastomosis in the Treatment of Type III and Type IV Hilarcholangiocarcinoma. Zhonghua Zhongliu Zazhi. 2009;31:626-629. [DOI] [Full Text] |
| 6. | Wu JS. Basin-like Biliary Enterostomy for Biliary. Yixue Linchuang Yanjiu. 2002;19:78-80. [DOI] [Full Text] |
| 7. | Chen DX, Xing GY, Liu Y. Hotspots in Surgical Treatment of Hilarcholangiocarcinoma. Zhonghua Qiangjing Waike Zazhi. 2017;10:196-199. [DOI] [Full Text] |
| 8. | Huang ZQ. The Present aituation of Surgical Treatment of Hilarcholangiocarcinoma and My Opinion. Zhongguo Shiyong Waike Zazhi. 2007;27:341-346. [DOI] [Full Text] |
| 9. | Zhao S, Wang X, Liu YB. Surgical Controversy and Perihepatichilar Resection of Hilarcholangiocarcinoma. Gandanyi Waike Zazhi. 2016;28:346-350. [DOI] [Full Text] |
| 10. | Wang JM, Jiang YQ, Zou SQ. Application of Combined Vascular Resection and Reconstruction in Resection for Advanced Hilar Cholangiocarcinoma. Zhongguo Puwai Jichu and Linchuang Zazhi. 2011;18:579-582. |
| 11. | Miyazaki M, Kato A, Ito H, Kimura F, Shimizu H, Ohtsuka M, Yoshidome H, Yoshitomi H, Furukawa K, Nozawa S. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery. 2007;141:581-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 176] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 12. | Song GW, Lee SG, Hwang S, Kim KH, Cho YP, Ahn CS, Moon DB, Ha TY. Does portal vein resection with hepatectomy improve survival in locally advanced hilar cholangiocarcinoma? Hepatogastroenterology. 2009;56:935-942. [PubMed] |
| 13. | Igami T, Nishio H, Ebata T, Yokoyama Y, Sugawara G, Nimura Y, Nagino M. Surgical treatment of hilar cholangiocarcinoma in the "new era": the Nagoya University experience. J Hepatobiliary Pancreat Sci. 2010;17:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 142] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 14. | Wang PF, Zhu ZM, Cai SW. Resection and Reconstruction of Hilarcholangiocarcinoma. Linchuang Waike Zazhi. 2017;25:177-177. [DOI] [Full Text] |
| 15. | Chen ZY, Beiping. Combined Vascular Aesection and Reconstruction in the Surgical Treatment of Hilarcholangiocarcinoma. Linchuang Gandanbing Zazhi. 2016;32:1277-1279. [DOI] [Full Text] |
| 16. | Bai XL, Ma T, Yu XZ, Liang TB. Evaluation of Radical Resection of Hilarcholangiocarcinoma Combined with Vascular Resection and Reconstruction. Zhonghua Puwaike Shoushuxue Zazhi. 2015;9:12-15. [DOI] [Full Text] |
| 17. | Nimura Y. Radical surgery of left-sided klatskin tumors. HPB (Oxford). 2008;10:168-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Yuan SG, Nong KT, Liu J, Lv J, Weng J, Yang JH, Chen Q, Mei MH. Propristine Continuous Hepaticojejunostomy for Advanced Hilarcholangiocarcinoma. Sichuan Yixue. 2011;32:73-75. [DOI] [Full Text] |