Published online Jan 6, 2020. doi: 10.12998/wjcc.v8.i1.38
Peer-review started: August 20, 2019
First decision: September 9, 2019
Revised: October 15, 2019
Accepted: October 30, 2019
Article in press: October 30, 2019
Published online: January 6, 2020
Processing time: 139 Days and 22.8 Hours
Total cervical artificial disc replacement (TDR) has been considered a safe and effective alternative surgical treatment for cervical spondylosis and degenerative disc disease that have failed to improve with conservative methods. Positioning the surgical patient is a critical part of the procedure. Appropriate patient positioning is crucial not only for the safety of the patient but also for optimizing surgical exposure, ensuring adequate and safe anesthesia, and allowing the surgeon to operate comfortably during lengthy procedures. The surgical posture is the traditional position used in anterior cervical approach; in general, patients are in a supine position with a pad under their shoulders and a ring-shaped pillow under their head.
To investigate the clinical outcomes of the use of a modified surgical position versus the traditional surgical position in anterior approach for TDR.
In the modified position group, the patients had a soft pillow under their neck, and their jaw and both shoulders were fixed with wide tape. The analyzed data included intraoperative blood loss, position setting time, total operation time, and perioperative blood pressure and heart rate.
Blood pressure and heart rate were not significantly different before and after body positioning in both groups (P > 0.05). Compared with the traditional position group, the modified position group showed a statistically significantly longer position setting time (P < 0.05). However, the total operation time and intraoperative blood loss were significantly reduced in the modified position group compared with the traditional position group (P < 0.05).
The clinical outcomes indicated that total operation time and intraoperative blood loss were relatively lower in the modified position group than in the traditional position group, thus reducing the risks of surgery while increasing the position setting time. The modified surgical position is a safe and effective method to be used in anterior approach for TDR surgery.
Core tip: This article was designed to investigate the clinical outcomes of the use of a modified surgical position versus the traditional surgical position in anterior approach for total cervical artificial disc replacement (TDR). The clinical outcomes indicated that total operation time and intraoperative blood loss were relatively lower in the modified position group than in the traditional position group, thus reducing the risks of surgery while increasing the position setting time. The modified surgical position is a safe and effective method to be used in anterior approach for TDR surgery.
- Citation: Hou WX, Zhang HX, Wang X, Yang HL, Luan XR. Application of a modified surgical position in anterior approach for total cervical artificial disc replacement. World J Clin Cases 2020; 8(1): 38-45
- URL: https://www.wjgnet.com/2307-8960/full/v8/i1/38.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i1.38
Artificial cervical disc prosthesis was designed by utilizing bionics technology, thus preserving the activity of the treated segment, and its design was first reported by Goffin et al[1] in 2002. Total cervical artificial disc replacement (TDR) has been considered a safe and effective alternative surgical treatment for cervical spondylosis and degenerative disc disease that have failed to improve with conservative methods[2-9].
Positioning the surgical patient is a critical part of the procedure. Appropriate patient positioning is crucial not only for the safety of the patient but also for optimizing surgical exposure, ensuring adequate and safe anesthesia, and allowing the surgeon to operate comfortably during lengthy procedures[10,11].
The surgical posture is the traditional position used in anterior cervical approach; in general, patients are in a supine position with a pad under their shoulders and a ring-shaped pillow under their head[12,13]. The activity of the adjacent segment accelerates the degeneration of the adjacent layers and causes new symptoms[8,14-17].
To enable an improved TDR procedure, shorten the time of operation, reduce the incidence of perioperative complications, and improve the safety of the procedure, we planned to improve the traditional surgical position in anterior cervical approach.
In this study, a total of 48 cervical spondylosis patients who were treated by TDR with either the traditional or the modified surgical position were assessed. We comprehensively determined the clinical outcomes, including the blood pressure and heart rate before and after body positioning, position setting time, total operation time, and intraoperative blood loss.
All patients were initially assessed and treated by trained nurses before being enrolled in this study. Patients received a diagnosis of cervical spondylosis of one segmental level that was supported by clinical symptoms and imaging data and had poor clinical outcomes even after previously undergoing strict conservative treatment for at least three months.
Forty-eight patients were divided into a traditional position group and a modified position group, with 24 patients in each group (Table 1). Perioperative parameters were retrospectively analyzed.
| Modified group (n = 24) | Traditional group (n = 24) | P value | |
| Male/Female | 16/8 | 12/12 | 0.439 |
| Age (yr) | 46.7 (26-65) | 43.3 (25-61) | 0.998 |
| Level of surgery | 0.551 | ||
| C3/4 | 5 | 3 | |
| C4/5 | 11 | 11 | |
| C5/6 | 8 | 10 |
To assess the safety of the position setting process, blood pressure and heart rate were used, and these metrics were measured in all patients before and after the position setting process in both groups. In addition, the surgical position setting time was measured. After surgery, total operation time and intraoperative blood loss were recorded to evaluate the effects of surgical position on the safety of surgery.
Traditional position group: The traditional surgical position setting is shown in Figure 1A and B. After anesthesia intubation, the patient's head, neck, and shoulders were lifted, a shoulder pad was placed under the shoulders, and a ring-shaped pillow was placed under the head. Subsequently, the patient was positioned back on the table, and the height and position of the head, neck, and shoulder were checked until the neck was fully exposed.
Modified position group: The modified surgical position setting is shown in Figure 1C and D. After anesthesia intubation, a shoulder pad and a ring-shaped pillow were placed under the shoulder and head, respectively. Then, a soft pillow with a height of approximately 10 cm was placed under the patient's neck. The lower jaw was pulled in the rostral direction, both shoulders were pulled in the caudal direction, and tape was used to maintain the position.
Data are presented as the mean ± SD. Statistical analyses were performed by the independent-samples t-test between two groups using SPSS (version 22.0, Chicago, IL), and categorical variables were analyzed by the Mann-Whitney U test. Differences of P < 0.05 were considered significant.
All patients who underwent single-level Mobi-C artificial disc replacement from September 2014 to September 2015 were included (28 males and 20 females). The average age was 45.7 years (range, 25-65 years). Of the patients, 8 had C3-C4 replacement, 22 had C4-C5 replacement, and 18 had C5-C6 replacement.
There was no significant difference in sex, age, history, treated segment, anesthesia, or surgical staff between the two groups (P > 0.05).
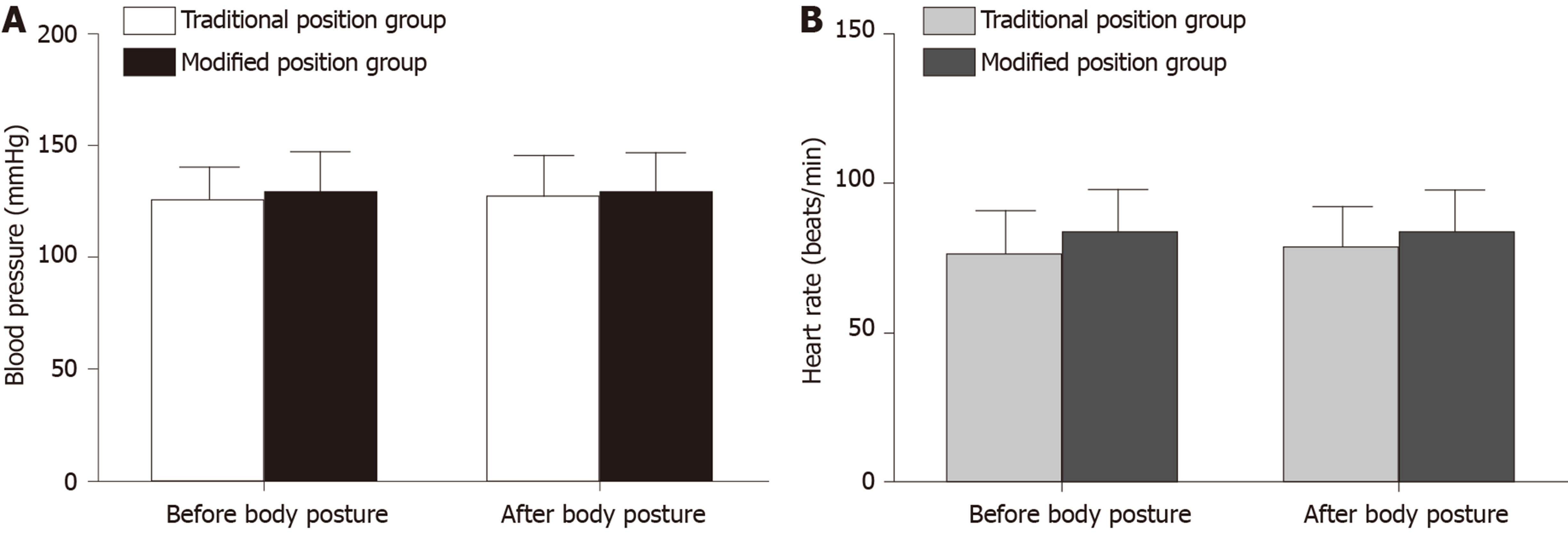
In the traditional position group, the blood pressure was 124.76 ± 15.3 mmHg before body positioning and 126.69 ± 18.7 mmHg after body positioning (Figure 2A). The average heart rate was 76.36 ± 14.2 bpm and 78.01 ± 13.8 bpm in the traditional position group before and after body posture, respectively (Figure 2B).
In the modified position group, the blood pressure before body positioning was 128.43 ± 18.8 mmHg, and it was 129.33 ± 17.1 mmHg after body positioning (Figure 2A). The average heart rate was shown to be 82.61 ± 15.0 bpm and 83.25 ± 14.4 bpm in the modified position group before and after body posture, respectively (Figure 2B).
Blood pressure and heart rate before and after body positioning were not significantly different within each group or between the two groups (P > 0.05).
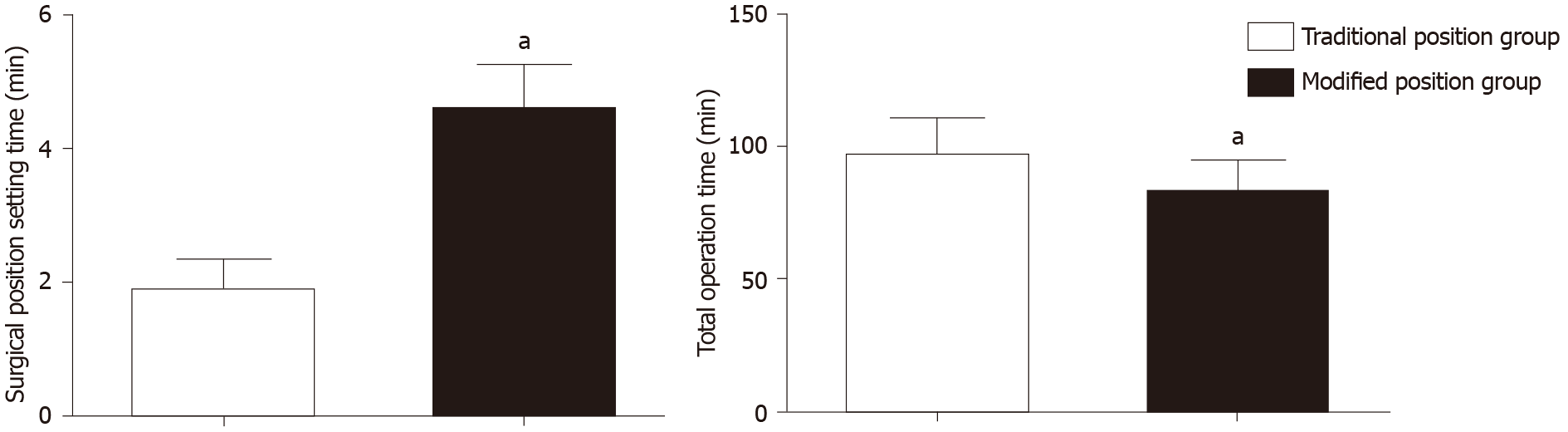
The surgical position setting time was 1.85 ± 0.49 min in the traditional position group, and it was 4.57 ± 0.67 min in the modified position group (Figure 3). A statistically significant increase was observed in the modified position group compared with the traditional position group (P < 0.05).
The total operation time was significantly shorter in the modified position group (82.05 ± 12.4 min) than in the traditional position group (95.78 ± 14.5 min) (P < 0.05) (Figure 3).
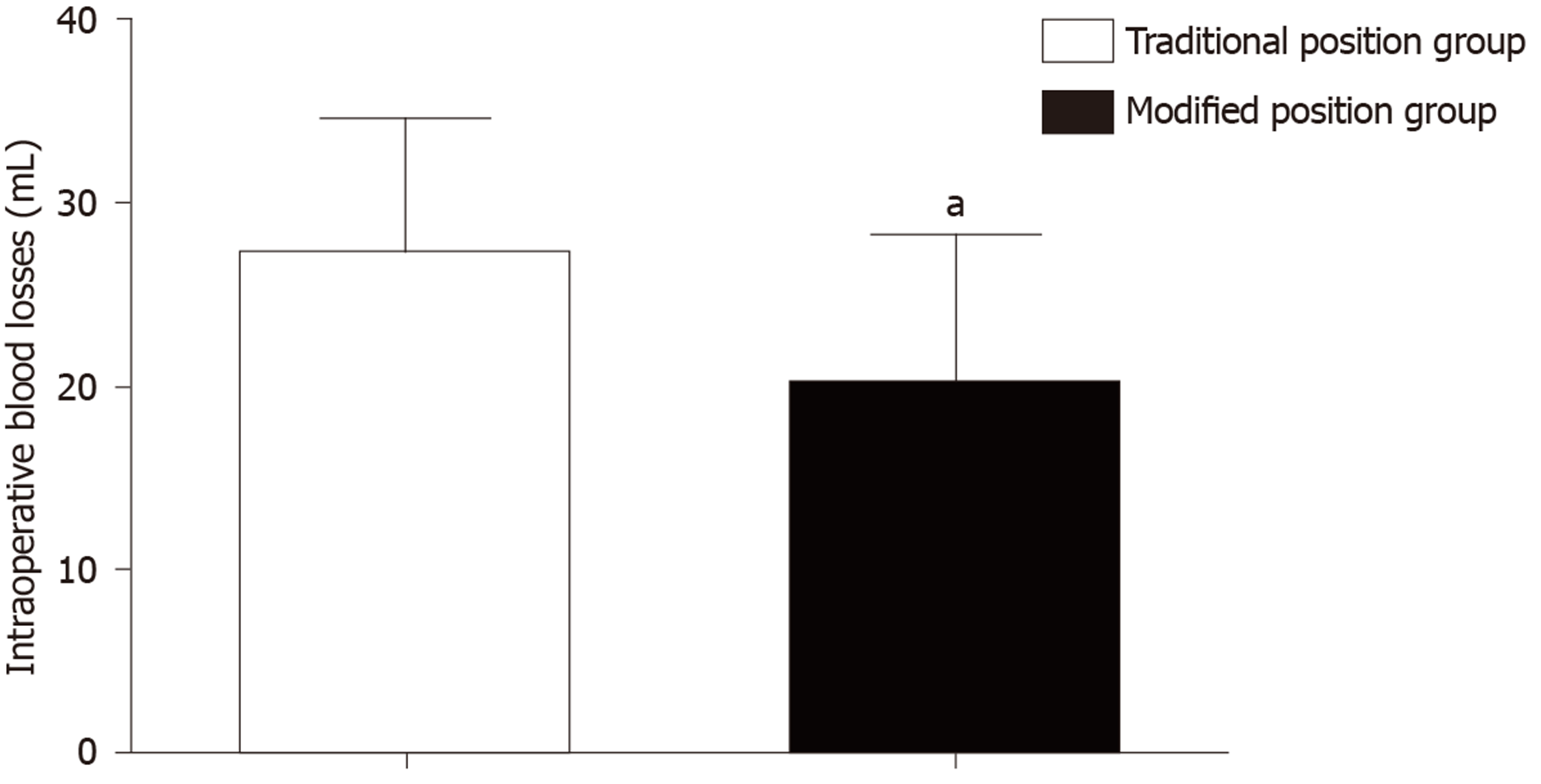
The intraoperative blood loss in the modified position group (20 ± 8.1 mL) was significantly lower than that in the traditional position group (27 ± 7.5 mL; P < 0.05) (Figure 4).
Artificial cervical disc prosthesis was designed to reconstruct or maintain the height of the intervertebral disc, maintain the regular activity of the cervical spine, and create favorable conditions for the recovery of function of the spinal cord after the spinal cord compression was removed[4,18-20].
An appropriate surgical position is crucial for the operation. Improvement in the patient's surgical status facilitates the surgeon’s procedure and reduces the amount of bleeding and the incidence of complications, thus creating essential conditions for successful implementation of the disc and recovery of the patient[10,11].
In this study, 48 cases of cervical disc replacement with Mobi-C prosthesis were included. Compared with patients in the traditional surgical position, patients in the modified surgical position had more satisfactory clinical outcomes, and the advantages are as follows.
To facilitate the operation and select the appropriate type of prosthesis in TDR, the patient is typically placed in the supine-neutral surgical position to maintain the natural curve of the cervical spine[8,21-27]. Because only the shoulder pad and ring-shaped pillow were placed under the shoulders and head, respectively, the neck of the patient was not supported in the traditional surgical position during anterior cervical approach. However, in the modified position, the shoulder pad and ring-shaped pillow were placed under the shoulders and head, respectively, and a soft pillow with a height of approximately 10 cm was placed under the patient's neck so that the patient was in the supine-neutral surgical position during the surgery.
During a cervical surgical procedure, slight activity of the patient can have serious consequences, including cervical displacement and injuries of the blood vessels and the spinal cord[15,23,28-32]. In the modified position, the lower jaw and both shoulders were pulled in the rostral and the caudal directions, respectively, and wide tape was used for auxiliary fixation. Thus, the cervical spine and other parts of the patient were securely fixed, allowing a successful surgery and guaranteeing the safety of the patients.
The total operation time was significantly shorter in the modified position group than in the traditional position group. Intraoperative blood loss in the modified position group was significantly lower than that in the traditional position group.
The modified surgical position needs more surgical position setting time. However, the total operation time was shortened, and intraoperative blood loss was reduced in patients with the modified surgical position compared with patients with the traditional position. A shorter operation time results in a lower operation risk, and a smaller amount of bleeding during the operation can not only help the surgeon's activity but also reduce the risk of injury in patients, which is beneficial to the healing process.
In this study, the modified surgical position in anterior approach was successfully designed for TDR. The results indicated that the modified surgical position had no adverse effects on the blood pressure and heart rate of the patient. The modified surgical position reduces the total operation time and intraoperative blood loss, although it consumes more surgical position setting time; these results suggest that the modified position is beneficial to the operation of the surgeons, and it is worthy of application and widespread use in TDR.
Total cervical artificial disc replacement (TDR) has been considered a safe and effective alternative surgical treatment for cervical spondylosis and degenerative disc disease that have failed to improve with conservative methods.
Positioning the surgical patient is a critical part of the procedure. Appropriate patient positioning is crucial not only for the safety of the patient but also for optimizing surgical exposure, ensuring adequate and safe anesthesia, and allowing the surgeon to operate comfortably during lengthy procedures. The surgical posture is the traditional position used in anterior cervical approach; in general, patients are in a supine position with a pad under their shoulders and a ring-shaped pillow under their head. The activity of the adjacent segment accelerates the degeneration of the adjacent layers and causes new symptoms.
To investigate the clinical outcomes of the use of a modified surgical position versus the traditional surgical position in anterior approach for TDR.
In the modified position group, patients had a soft pillow under their neck, and their jaw and both shoulders were fixed with wide tape. The analyzed data included intraoperative blood loss, position setting time, total operation time, and perioperative blood pressure and heart rate.
Blood pressure and heart rate were not significantly different before and after body positioning in both groups. Compared with the traditional position group, the modified position group showed a statistically significantly longer position setting time. However, the total operation time and intraoperative blood loss were significantly reduced in the modified position group compared with the traditional position group.
The clinical outcomes indicated that total operation time and intraoperative blood loss were lower in the modified position group than in the traditional position group, thus reducing the risks of surgery while increasing the position setting time.
The modified surgical position is a safe and effective method to be used in anterior approach for TDR surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kressel A, Kositamongkol P, Fires D S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Goffin J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Pointillart V, Van Calenbergh F, van Loon J. Preliminary clinical experience with the Bryan Cervical Disc Prosthesis. Neurosurgery. 2002;51:840-5; discussion 845-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Findlay C, Ayis S, Demetriades AK. Total disc replacement versus anterior cervical discectomy and fusion: a systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short- and medium- to long-term outcomes. Bone Joint J. 2018;100-B:991-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 107] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 3. | Verma K, Gandhi SD, Maltenfort M, Albert TJ, Hilibrand AS, Vaccaro AR, Radcliff KE. Rate of adjacent segment disease in cervical disc arthroplasty versus single-level fusion: meta-analysis of prospective studies. Spine (Phila Pa 1976). 2013;38:2253-2257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004;17:E9. [PubMed] |
| 5. | Di Martino A, Papalia R, Albo E, Cortesi L, Denaro L, Denaro V. Cervical spine alignment in disc arthroplasty: should we change our perspective? Eur Spine J. 2015;24 Suppl 7:810-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Badve SA, Kurra S, Nunley PD, Lavelle WF. The Mobi-C® cervical disc and other devices for two-level disc replacement: overview of its safety and efficacy. Expert Rev Med Devices. 2019;16:307-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Botelho RV. Preliminary clinical experience with the Bryan cervical disc prosthesis. Neurosurgery. 2003;53:785; author reply 785-785; author reply 786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Xu B, Ma JX, Tian JH, Ge L, Ma XL. Indirect meta-analysis comparing clinical outcomes of total cervical disc replacements with fusions for cervical degenerative disc disease. Sci Rep. 2017;7:1740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Yang SD, Zhu YB, Yan SZ, Di J, Yang DL, Ding WY. Anterior cervical discectomy and fusion surgery versus total disc replacement: A comparative study with minimum of 10-year follow-up. Sci Rep. 2017;7:16443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Burlingame BL. Guideline Implementation: Positioning the Patient. AORN J. 2017;106:227-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Obeid I, Boissière L, Yilgor C, Larrieu D, Pellisé F, Alanay A, Acaroglu E, Perez-Grueso FJ, Kleinstück F, Vital JM, Bourghli A; European Spine Study Group, ESSG. Global tilt: a single parameter incorporating spinal and pelvic sagittal parameters and least affected by patient positioning. Eur Spine J. 2016;25:3644-3649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 102] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 12. | Linhares D, Lobo J, Pinto R, Neves N. Atypical presentation of a cervical synovial cyst. Eur Spine J. 2017;26:2267-2271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Cornett CA, Kang JD, Lee JY, Devin CJ, Gannon E, Kim E, Esmende SM. Surgical Management of Cervical Spondylotic Myelopathy. Instr Course Lect. 2017;66:329-351. [PubMed] |
| 14. | Park CK, Ryu KS. Are Controversial Issues in Cervical Total Disc Replacement Resolved or Unresolved?: A Review of Literature and Recent Updates. Asian Spine J. 2018;12:178-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Kim CH, Park TH, Chung CK, Kim KT, Choi YH, Chung SW. Changes in cervical motion after cervical spinal motion preservation surgery. Acta Neurochir (Wien). 2018;160:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Wiedenhöfer B, Nacke J, Stephan M, Richter W, Carstens C, Eichler M. Is Total Disk Replacement a Cost-effective Treatment for Cervical Degenerative Disk Disease? Clin Spine Surg. 2017;30:E530-E534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Heo DH, Lee DC, Oh JY, Park CK. Bone loss of vertebral bodies at the operative segment after cervical arthroplasty: a potential complication? Neurosurg Focus. 2017;42:E7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Jackson RJ, Davis RJ, Hoffman GA, Bae HW, Hisey MS, Kim KD, Gaede SE, Nunley PD. Subsequent surgery rates after cervical total disc replacement using a Mobi-C Cervical Disc Prosthesis versus anterior cervical discectomy and fusion: a prospective randomized clinical trial with 5-year follow-up. J Neurosurg Spine. 2016;24:734-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 19. | Daentzer D, Welke B, Hurschler C, Husmann N, Jansen C, Flamme CH, Richter BI. In vitro-analysis of kinematics and intradiscal pressures in cervical arthroplasty versus fusion--A biomechanical study in a sheep model with two semi-constrained prosthesis. Biomed Eng Online. 2015;14:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Hisey MS, Bae HW, Davis RJ, Gaede S, Hoffman G, Kim KD, Nunley PD, Peterson D, Rashbaum RF, Stokes J, Ohnmeiss DD. Prospective, Randomized Comparison of Cervical Total Disk Replacement Versus Anterior Cervical Fusion: Results at 48 Months Follow-up. J Spinal Disord Tech. 2015;28:E237-E243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 21. | Siskey R, Peck J, Mehta H, Kosydar A, Kurtz S, Hill G. Development of a clinically relevant impingement test method for a mobile bearing lumbar total disc replacement. Spine J. 2016;16:1133-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Esmende SM, Daniels AH, Paller DJ, Koruprolu S, Palumbo MA, Crisco JJ. Cervical total disc replacement exhibits similar stiffness to intact cervical functional spinal units tested on a dynamic pendulum testing system. Spine J. 2015;15:162-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Kim JS, Dowdell J, Cheung ZB, Arvind V, Sun L, Jandhyala C, Ukogu C, Ranson W, Jacobs S, McAnany S, Cho SK. The Seven-Year Cost-Effectiveness of Anterior Cervical Discectomy and Fusion Versus Cervical Disc Arthroplasty: A Markov Analysis. Spine (Phila Pa 1976). 2018;43:1543-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 24. | Lavelle WF, Riew KD, Levi AD, Florman JE. Ten-year Outcomes of Cervical Disc Replacement With the BRYAN Cervical Disc: Results From a Prospective, Randomized, Controlled Clinical Trial. Spine (Phila Pa 1976). 2019;44:601-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 96] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 25. | Segal DN, Wilson JM, Staley C, Yoon ST. Outpatient and Inpatient Single-level Cervical Total Disc Replacement: A Comparison of 30-day Outcomes. Spine (Phila Pa 1976). 2019;44:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 26. | Chin KR, Pencle FJR, Seale JA, Pencle FK. Clinical Outcomes of Outpatient Cervical Total Disc Replacement Compared With Outpatient Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976). 2017;42:E567-E574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 27. | Chin KR, Pencle FJR, Benny A, Seale JA. Placing ball and socket cervical total disc replacement using instant center of rotation. J Orthop. 2019;16:390-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Kim SW, Paik SH, Oh JK, Kwak YH, Lee HW, You KH. The impact of coronal alignment of device on radiographic degeneration in the case of total disc replacement. Spine J. 2016;16:470-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Lanman TH, Burkus JK, Dryer RG, Gornet MF, McConnell J, Hodges SD. Long-term clinical and radiographic outcomes of the Prestige LP artificial cervical disc replacement at 2 levels: results from a prospective randomized controlled clinical trial. J Neurosurg Spine. 2017;27:7-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 30. | Loumeau TP, Darden BV, Kesman TJ, Odum SM, Van Doren BA, Laxer EB, Murrey DB. A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF). Eur Spine J. 2016;25:2263-2270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 31. | Chin KR, Lubinski JR, Zimmers KB, Sands BE, Pencle F. Clinical experience and two-year follow-up with a one-piece viscoelastic cervical total disc replacement. J Spine Surg. 2017;3:630-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 32. | Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H, Tsianaka E, Vagkopoulos K, Paterakis K, Fountas KN. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg. 2017;3:444-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |