Published online Jan 6, 2020. doi: 10.12998/wjcc.v8.i1.29
Peer-review started: October 9, 2019
First decision: November 13, 2019
Revised: November 28, 2019
Accepted: November 30, 2019
Article in press: November 30, 2019
Published online: January 6, 2020
Processing time: 89 Days and 19 Hours
Posterior malleolar fractures have been reported to occur in < 40% of ankle fractures.
To reveal the recurrent patterns and characteristics of posterior malleolar fractures by creating fracture maps of the posterior malleolar fractures through the use of computed tomography mapping.
A consecutive series of posterior malleolar fractures was used to create three-dimensional reconstruction images, which were oriented and superimposed to fit an ankle model template by both aligning specific biolandmarks and reducing reconstructed fracture fragments. Fracture lines were found and traced in order to generate an ankle fracture map.
This study involved 112 patients with a mean age of 49, comprising 32 pronation-external rotation grade IV fractures and 80 supination-external rotation grade IV fractures according to the Lauge-Hansen classification system. Three-dimensional maps showed that the posterior ankle fracture fragments in the supination-external rotation grade IV group were relatively smaller than those in the pronation-external rotation grade IV group after posterior malleolus fracture. In addition, the distribution analyses on posterior malleolus fracture lines indicated that the supination-external rotation grade IV group tended to have higher linear density but more concentrated and orderly distribution fractures compared to the pronation-external rotation grade IV group.
Fracture maps revealed the fracture characteristics and recurrent patterns of posterior malleolar fractures, which might help to improve the understanding of ankle fracture as well as increase opportunities for follow-up research and aid clinical decision-making.
Core tip: With increasing concern over the big data analytics, the distribution map of fracture lines (named fracture mapping) based on three dimensional computed tomography has also been widely used in the orthopedic field to characterize fractures. By creating fracture maps of the posterior malleolar fractures, the study revealed the fracture characteristics and recurrent patterns of posterior malleolar fractures.
- Citation: Su QH, Liu J, Zhang Y, Tan J, Yan MJ, Zhu K, Zhang J, Li C. Three-dimensional computed tomography mapping of posterior malleolar fractures. World J Clin Cases 2020; 8(1): 29-37
- URL: https://www.wjgnet.com/2307-8960/full/v8/i1/29.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i1.29
Ankle fractures account for roughly 10% of all fracture cases, indicating that they are one of the most common injuries in clinical practice and often require surgical intervention[1]. Posterior malleolar fractures have been reported to occur in < 40% of ankle fractures[2]. Numerous research findings have demonstrated that the presence of posterior malleolar fragment (PMF) is widely regarded as a critical prognostic factor or outcome indicator following ankle fracture treatment[2-5]. As previously reported, patients with PMF ankle fractures exhibit poor clinical outcomes in comparison with uni- or bi-malleolar ankle fractures[2].
Despite this, the optimal treatment procedures for posterior malleolar fractures remain controversial. The first treatment proposed by Regan et al[6] has been applied for decades, in which the fixation of coronoid fractures is based on size and articular involvement. More recently, it has been suggested that the patterns of coronoid fracture, especially their morphological features, are superior compared to the height of coronoid fracture[7-9]. Similarly, through the use of computed tomography (CT)-based PMF mapping in a subset of patients (n = 45), Mangnus et al[10] found that the morphology of PMF can be more crucial than fragment size alone for clinical decision making. Specifically, Haraguchi type II can be considered as an individual fracture pattern. Recently, there has been increasing interest in the morphological characterization of such fractures and reaching a consensus on surgical treatment.
To examine the pathoanatomical or morphological features of PMF, various studies have utilized plain radiograph[11], CT scan[12] and three-dimensional (3D) reconstruction CT[13]. Typically, the lateral view of plain radiograph can be used to assess PMF in ankle fractures. However, the plain radiographic assessment of PMF may be unreliable and inaccurate, even though the estimation of PMF size, including tibial articular surface, is feasible[14]. Given the rising concerns toward big data analytics, 3D CT-based fracture mapping has been commonly applied in orthopedic fields such as the characterization of scapular and thoracolumbar fractures[15,16], as initially described by Cole et al[17].
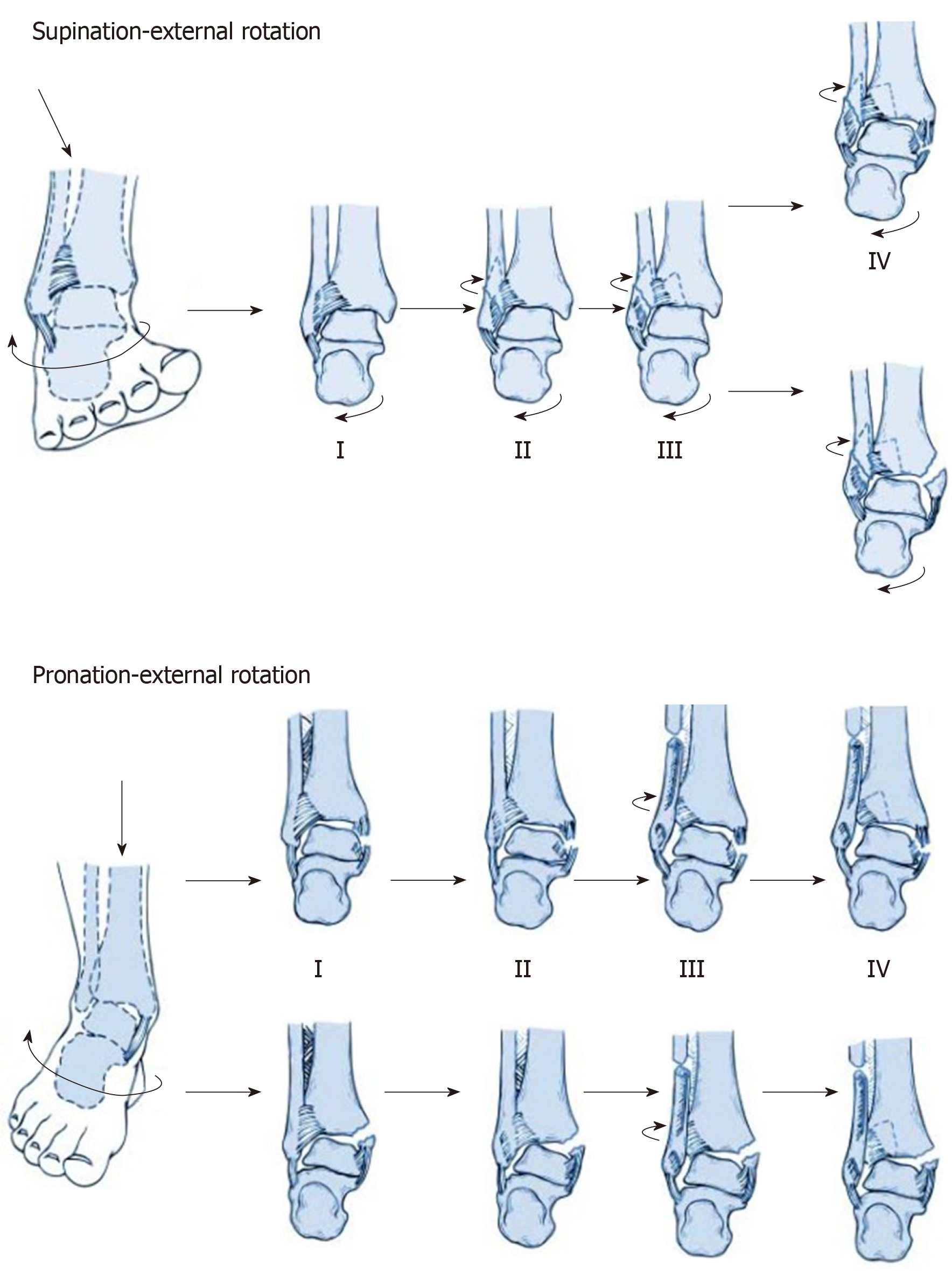
In the present study, our aims were to divide the position and prevalence of fracture lines of a series of posterior malleolar fractures into two groups: supination-external rotation grade IV (SER4) and pronation-external rotation grade IV (PER4) groups, as per the Lauge-Hansen classification system[18] (Figure 1) and to produce fracture maps through 3D CT mapping. We postulated that the 3D maps of posterior malleolar fractures would demonstrate the fracture lines, fracture characteristics and recurrent patterns of PMF, which would have the potential to enhance surgeons’ understanding and recognition of PMF during diagnostic intervention, preoperative planning, surgery and proper internal fixation. In addition, the 3D maps of medial malleolus and fibula were also obtained from the two groups.
A retrospective analysis was undertaken for the CT imaging data of patients diagnosed with PMF in our institution from January 2010 to December 2017. This data was obtained by searching the picture archiving and communication system database. All fractures were classified based on the Lauge-Hansen system[18], where the first term represents the position of the foot at the time of injury and the second term indicates the external force applied to the foot, in order to create specific fracture patterns. Inclusion criteria were as follows: (1) Participants must have either SER4 injuries or PER4 injuries; (2) Participants without pathological and osteoporotic posterior malleolar fractures; and (3) Good-quality CT images must be available. Participants were excluded if they: (1) Had fracture lines or anatomical landmarks obscured by foreign bodies; and (2) Had severe comminuted fractures in which the conditions of fracture lines were difficult to be determined. The data of participants were evaluated by a highly experienced orthopedic surgeon and senior investigator through the 3D CT rendering in the picture archiving and communication system database.
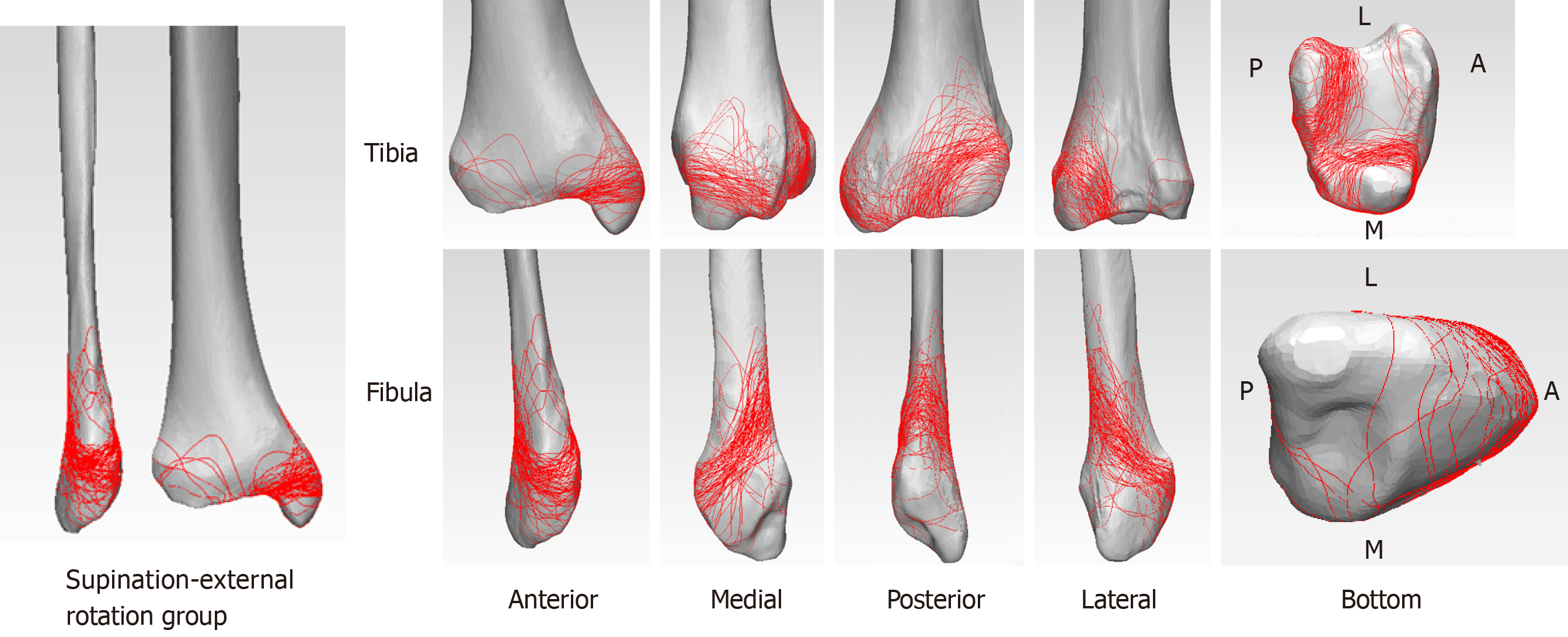
With increasing concern over the big data analytics, the distribution map of fracture lines (named fracture mapping) based on 3D CT has also been widely used in orthopedic fields to characterize fractures[16]. The raw data in digital imaging and communications in medicine format were recorded by a 64-channel CT scanner (Siemens Somatom Sensation, Siemens, Erlangen, Germany) with the following parameters: 0.5 mm interlayer spacing, 1 mm slice thickness, 200 mA tube current and 120 kV tube voltage. Subsequently, the digital imaging and communications in medicine data for all participants were inputted to Mimics 20.0 software (Materialise, Leuven, Belgium). Through threshold segmentation, the fragments of ankle joint were separated and reconstructed. Following this, the 3D reconstruction model of each fragment was generated using the STL file. The reconstructed model was then inputted to 3-matic 12.0 software (Materialise, Leuven, Belgium) in order to reposition the fragments. This was followed by overlapping and matching with the model of typical ankle through slight adjustment and standardization. Fracture lines were drawn on the typical ankle model in compliance with the existing fracture model, while the 3D maps were obtained by superimposing the fracture lines of all participants (Figure 2).
The fracture characteristics of patients were analyzed using the frequencies and percentages for categorical variables as well as arithmetic means for continuous variables. To compare whether gender is correlated with posterior malleolus fracture among SER and PER groups, a Pearson χ2 hypothesis test was conducted with the level of α = 0.05 (V20.0, SPSS, Chicago, IL, United States). Descriptive analyses were carried out for each group using a combination of 3D mapping generation.
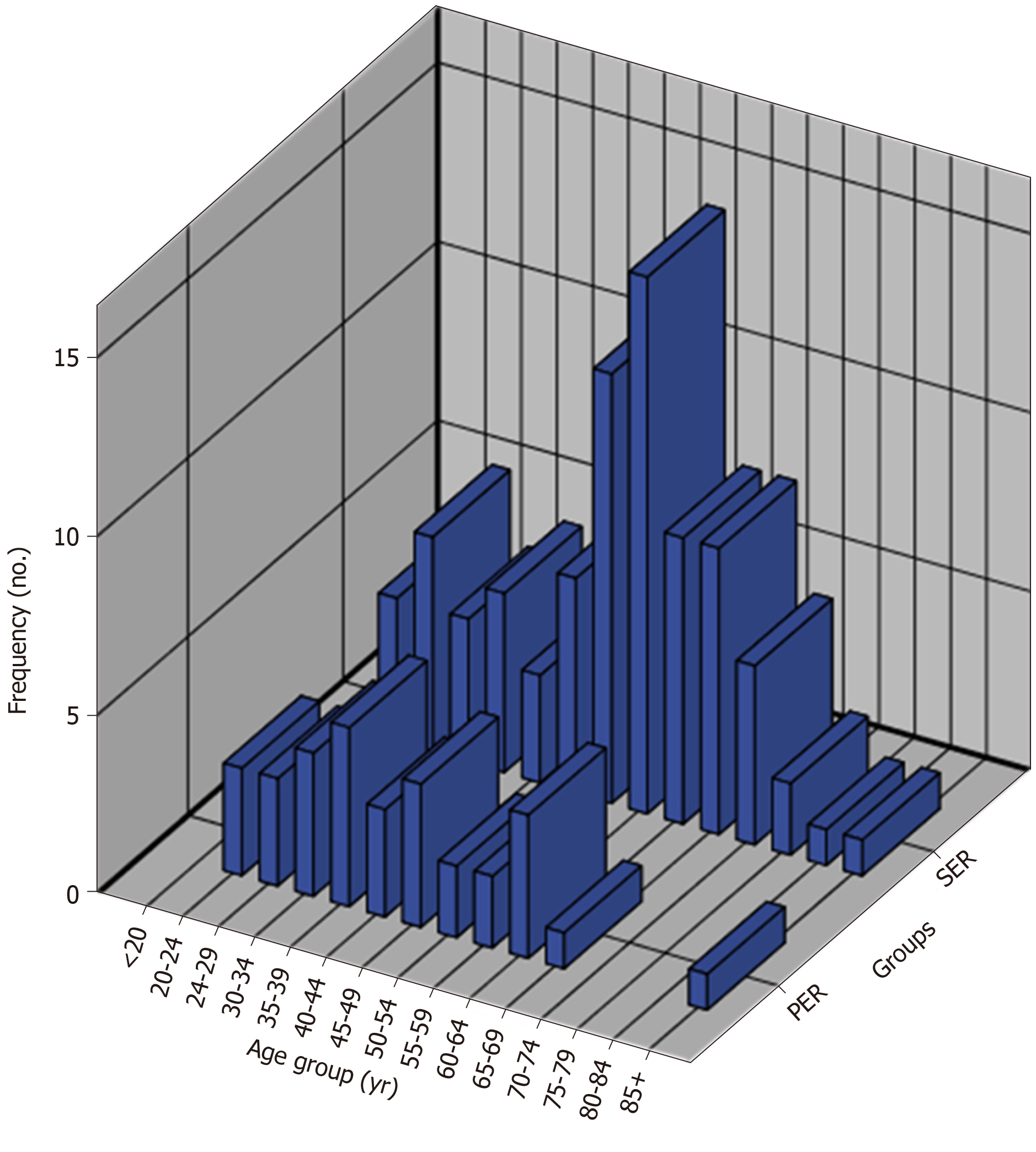
The present study enrolled 112 patients, of which 80 were in the SER4 group and 32 in the PER4 group. Participants had an average age of 49 (SD = 15.09 years; Figure 3). Patient demographics are summarized in Table 1. The results of Pearson χ2 hypothesis test demonstrated that the value of χ2 was 1.600 and P value was 0.206 (P > 0.05). This indicated that there was no statistically significant difference between gender in the two groups.
| Variables | |
| Age in yr, mean ± SD (range) | 49.0 ± 15.9 (20-89) |
| Supination-external rotation group | |
| Female | 48 |
| Male | 32 |
| Pronation-external rotation group | |
| Female | 15 |
| Male | 17 |
Comparison of the 3D maps of the two groups (SER group, Figure 4; PER group, Figure 5) revealed that the features shared by both groups was the presence of medial malleolus fractures and lateral malleolus fractures among all cases with posterior malleolus fracture. However, when compared to the PER4 ankle fracture, which demonstrated larger fragments following posterior ankle fracture, the posterior ankle fracture fragments resulting from SER4 ankle fractures exhibited relatively smaller fragments. In addition, distribution analyses on posterior malleolus fracture lines indicated that the SER group tended to have higher linear density but more concentrated and orderly distribution fracture lines compared to the PER group. This was supported by a number of posterior malleolus fracture lines extending to the medial malleolus. However, no significant difference in the distribution of medial malleolus fracture lines was found between the two groups.
In addition, an apparent difference was found in the distribution of lateral malleolus fracture lines between the two groups. Notably, the majority of lateral malleolus fracture lines in the SER group originated from the lower end of the fibula before extending upwards along the anterior-to-posterior portion at an oblique angle. Comparatively, the lateral malleolus fracture lines originated from a higher localization in the PER group, followed by generating a non-uniform random distribution. Most of them extended upwards along the anterior-to-posterior portion at an oblique angle with a spiral pattern, indicating that they tended to have a greater length.
Fractures of the posterior malleolar commonly occur and may result from a rotational injury. Although treatment for associated lateral and medial structures has been well founded, controversy exists regarding their management.
Typically, the fixation approach for posterior malleolus fracture is a precise reduction of bone fragment through ligament reconstruction, followed by fixation with screws along an anterior-to-posterior direction. Obviously, the advantage of this technique lies in the fact that patients remain in a supine position for a minimally invasive operation. However, its disadvantage is the high-failure rates of ligament reconstruction. In addition, it is impossible to remove the residual bone fragments in the joint. Some studies report the use of a posterolateral approach[19-23], which has gained considerable attention and recognition. The unique leverage of this method is its direct achievement of an anatomical reduction as well as a stable fixation along the posterior-to-anterior direction with screws or plates. This approach also enabled the removal of intra-articular loose bodies that may interfere with anatomic reduction. However, the drawback of this surgery is that it requires a prone or lateral position for patients. In addition, some retrospective clinical studies have demonstrated that the open posterolateral approach for fixing a posterior malleolus fracture is much greater than percutaneous anterior-to-posterior screw fixation. Nevertheless, these findings need to be further verified by prospective comparative trials[24].
Through the use of 3D-map analyses, our study clearly demonstrated the uniformity and enrichment of posterior malleolus fracture lines in the SER group. In spite of a less extensive distribution of corresponding fracture lines, several smaller fragments protruded easily into the joints between the tibia and fibula as well as the joints between the tibia and talus. It is worth noting that these fragments generally have a sizeable impact on ankle joint prognosis, given the difficulty of achieving a complete reduction indirectly by ligament repairing as well as the challenges of achieving stable fixation via screws. This indicates that the functional rehabilitation of the ankle joint has been compromised to a large extent. Distribution analyses of the 3D maps revealed a scattered, non-uniform pattern of fracture lines in the PER group, many of which had extended to the medial malleolus with more severe degrees of fracture. In addition, the fracture surfaces of corresponding fragments appeared to have rough edges. It is interesting that this particular type of fracture fragment exhibits a better chance of achieving a positive effect via indirect ligament reconstruction. Therefore, it is reasonable to believe that in most cases of SER4 injuries, it is possible to successfully apply the posterolateral approach for fracture reduction and fixation. In contrast, for PER4 injuries, screw fixation along the anterior-to-posterior direction can generally be applied, which leads to a great effect of reduction and fixation.
Several studies have reported a high rate (33.5%) of clinical- and/or radiologic-diagnosed osteoarthritis following posterior malleolar fractures. Besides, there is no significant effect of fragment size on long-term outcomes after conservative or surgical management of posterior malleolus fractures. However, Mingo-Robinet et al[25] and McDaniel et al[26] have demonstrated that the outcome of posterior malleolus fractures can be improved if the fracture size is less than or equal to 25% of total distal articular surface without affecting the quality of reduction. Additionally, they recommend that the anatomic reduction of PMF may be required for greater fracture size (≥ 25%) and that failure to achieve a considerable reduction and correction of PMF subluxation does not change the overall outcome. However, our results, based on morphological analysis, seem to suggest otherwise. It is noted that if screw fixation is applied along the anterior-to-posterior direction, small PMFs may exert a greater impact on the functional rehabilitation of the ankle joint, even though this method does not achieve better reduction and fixation because the fracture fragments are typically small.
Nevertheless, it is unlikely that one single factor plays a decisive role in the functional rehabilitation of the ankle joint following posterior malleolus fracture, especially as trimalleolar fractures involve both medial malleolus and lateral malleolus. Instead, it is necessary to comprehensively evaluate the impact of a diverse set of potential risk factors, including the size, shape and location of fragments and the smoothness of fracture surface as well as other elements of fracture fixation, surgical approach and post-surgical rehabilitation. After comprehensive assessment, we recommend that individualized treatment is the best option. Moreover, we believe that most single-factor assessments deviating from the inclusion of comprehensive factors are defective and unreliable. Overall, multi-factor analyses and assessments, larger sample size, prolonged follow-up period and multicenter prospective controlled trials are needed for future investigations.
Fracture maps revealed the fracture characteristics and recurrent patterns of the posterior malleolar fractures, which might help to improve the understanding of ankle fracture as well as increase opportunities for follow-up research and aid clinical decision-making.
Posterior malleolar fractures have been reported to occur in < 40% of ankle fractures, which is widely regarded as a critical prognostic factor or outcome indicator following ankle fracture treatment. The morphology of posterior malleolar fractures can be more crucial than fragment size alone for clinical decision making.
The optimal treatment procedures for posterior malleolar fractures remain controversial. The fracture characteristics and recurrent patterns of the posterior malleolar fractures are unclear.
In this study, the authors aimed to reveal the recurrent patterns and characteristics of posterior malleolar fractures by creating fracture maps of the posterior malleolar fractures through the use of computed tomography mapping.
A consecutive series of posterior malleolar fractures was used to create three-dimensional reconstruction images to produce the distribution map of fracture lines through three-dimensional computed tomography mapping in the Mimics and 3-matic software.
Three-dimensional maps showed that the posterior ankle fracture fragments in supination-external rotation grade IV fractures were relatively smaller than those in pronation-external rotation grade IV fractures after posterior malleolus fracture. In addition, the distribution analyses on posterior malleolus fracture lines indicated that supination-external rotation group tended to have higher linear density but more concentrated and orderly distribution fractures compared to pronation-external rotation group.
Fracture maps revealed the fracture characteristics and recurrent patterns of the posterior malleolar fractures, which might help to improve the understanding of ankle fracture.
Multifactor analyses and assessments, larger sample size, prolonged follow-up period and multicenter prospective controlled trials are needed for future investigations.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Emara KM, Spartalis E S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Qi LL
| 1. | Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures--an increasing problem? Acta Orthop Scand. 1998;69:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 449] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 2. | Jaskulka RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma. 1989;29:1565-1570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 205] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM. Results of ankle fractures with involvement of the posterior tibial margin. J Trauma. 2002;53:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 131] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Tejwani NC, Pahk B, Egol KA. Effect of posterior malleolus fracture on outcome after unstable ankle fracture. J Trauma. 2010;69:666-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Weber M, Ganz R. Malunion following trimalleolar fracture with posterolateral subluxation of the talus--reconstruction including the posterior malleolus. Foot Ankle Int. 2003;24:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71:1348-1354. [PubMed] |
| 7. | Doornberg JN, Ring D. Coronoid fracture patterns. J Hand Surg Am. 2006;31:45-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 8. | Doornberg JN, Ring DC. Fracture of the anteromedial facet of the coronoid process. J Bone Joint Surg Am. 2006;88:2216-2224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | O'Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113-134. [PubMed] |
| 10. | Mangnus L, Meijer DT, Stufkens SA, Mellema JJ, Steller EP, Kerkhoffs GM, Doornberg JN. Posterior Malleolar Fracture Patterns. J Orthop Trauma. 2015;29:428-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 11. | Büchler L, Tannast M, Bonel HM, Weber M. Reliability of radiologic assessment of the fracture anatomy at the posterior tibial plafond in malleolar fractures. J Orthop Trauma. 2009;23:208-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006;88:1085-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 193] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 13. | Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I. Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg. 2015;135:505-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 180] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 14. | Ferries JS, DeCoster TA, Firoozbakhsh KK, Garcia JF, Miller RA. Plain radiographic interpretation in trimalleolar ankle fractures poorly assesses posterior fragment size. J Orthop Trauma. 1994;8:328-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zlowodzki M, Cole PA. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am. 2009;91:2222-2228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 138] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Su Q, Zhang Y, Liao S, Yan M, Zhu K, Yan S, Li C, Tan J. 3D Computed Tomography Mapping of Thoracolumbar Vertebrae Fractures. Med Sci Monit. 2019;25:2802-2810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 17. | Cole PA, Mehrle RK, Bhandari M, Zlowodzki M. The pilon map: fracture lines and comminution zones in OTA/AO type 43C3 pilon fractures. J Orthop Trauma. 2013;27:e152-e156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 144] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 18. | Yin MC, Yuan XF, Ma JM, Xia Y, Wang T, Xu XL, Yan YJ, Xu JH, Ye J, Tong ZY, Feng YQ, Wang HB, Wu XQ, Mo W. Evaluating the Reliability and Reproducibility of the AO and Lauge-Hansen Classification Systems for Ankle Injuries. Orthopedics. 2015;38:e626-e630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Talbot M, Steenblock TR, Cole PA. Posterolateral approach for open reduction and internal fixation of trimalleolar ankle fractures. Can J Surg. 2005;48:487-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 20. | Tornetta P, Ricci W, Nork S, Collinge C, Steen B. The posterolateral approach to the tibia for displaced posterior malleolar injuries. J Orthop Trauma. 2011;25:123-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S. Management of Posterior Malleolar Fractures: A Systematic Review. J Foot Ankle Surg. 2016;55:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 128] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 22. | Fu S, Zou ZY, Mei G, Jin D. Advances and disputes of posterior malleolus fracture. Chin Med J (Engl). 2013;126:3972-3977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Irwin TA, Lien J, Kadakia AR. Posterior malleolus fracture. J Am Acad Orthop Surg. 2013;21:32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 24. | Verhage SM, Hoogendoorn JM, Krijnen P, Schipper IB. When and how to operate the posterior malleolus fragment in trimalleolar fractures: a systematic literature review. Arch Orthop Trauma Surg. 2018;138:1213-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 25. | Mingo-Robinet J, López-Durán L, Galeote JE, Martinez-Cervell C. Ankle fractures with posterior malleolar fragment: management and results. J Foot Ankle Surg. 2011;50:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 26. | McDaniel WJ, Wilson FC. Trimalleolar fractures of the ankle. An end result study. Clin Orthop Relat Res. 1977;37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |