Published online Jan 6, 2020. doi: 10.12998/wjcc.v8.i1.149
Peer-review started: October 13, 2019
First decision: November 13, 2019
Revised: November 17, 2019
Accepted: December 6, 2019
Article in press: December 6, 2019
Published online: January 6, 2020
Processing time: 85 Days and 11.3 Hours
A large cervical cyst with a cervical high-grade squamous intraepithelial lesion arising from the cervical stump is rare. After supracervical hysterectomy, there is a risk of various lesions occurring in the cervical stump. We review the types and characteristics of cervical stump lesions and compare total hysterectomy with subtotal hysterectomy. Gynecologists should choose the most suitable surgical method based on both the patient’s condition and wishes. If the cervix is retained, patients require a close follow-up.
A 57-year-old woman was admitted to the Gynecology Department for a large pelvic mass. Her chief complaint was abdominal distention for two months. She had undergone subtotal supracervical hysterectomy for leiomyoma 14 years prior. Abdominal ultrasonography detected a 9.1 cm × 8.5 cm × 8.4 cm anechoic mass with silvery fluid in the pelvic cavity and high-risk human papilloma virus 53 (HPV53) was positive. The admission diagnosis we first considered was a pelvic mass mimicking carcinoma of the cervical stump. We performed a laparotomy and a rapid frozen biopsy was suggestive of a fibrous cyst wall coated with a high squamous intraepithelial lesion. The pelvic mass was removed, and a bilateral adnexectomy was implemented. Final pathology confirmed that the pelvic mass was a large inflammatory cyst with a cervical high-grade squamous intraepithelial lesion. After successful intervention, the patient was discharged one week after surgery and there was no recurrence of the vaginal stump at 43 mo.
When addressing benign uterine diseases, gynecologists should pay adequate attention to retaining the cervix. If the cervix is retained, patients require a close follow-up.
Core tip: A large cervical cyst with a cervical high-grade squamous intraepithelial lesion arising from the cervical stump is rare. To the best of our knowledge, this is the first case about this rare cervical cyst with cervical high-grade squamous intraepithelial lesion, which indicates that it should take careful consideration when handling with a stump cervix lesion. Gynecologists should choose the most suitable surgical method based on the patient’s wishes and condition. In dealing with benign uterine diseases, we should pay adequate attention to retaining the cervix. If the cervix is retained, patients require a close follow-up.
- Citation: Zhang K, Jiang JH, Hu JL, Liu YL, Zhang XH, Wang YM, Xue FX. Large pelvic mass arising from the cervical stump: A case report. World J Clin Cases 2020; 8(1): 149-156
- URL: https://www.wjgnet.com/2307-8960/full/v8/i1/149.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i1.149
Supracervical hysterectomy has been a popular procedure for benign uterine diseases in the last two decades worldwide. Often, young and pregnant patients wish to retain a portion of the uterus for presumed benign disease. Therefore, there are still many patients with a retained cervical stump. After supracervical hysterectomy, there is a risk of various lesions occurring in the stump of the cervix, including cervical stump fibroids, cervical prolapse, cervical stump endometriosis, cervical stump precancerous lesions, and stump carcinoma. Among them, carcinoma of the cervical stump, according to the literature, has accounted for 2%-9% of all cervical carcinomas worldwide since 1970[1]. Leiomyosarcoma that arises in the uterine cervix stump after subtotal hysterectomy is also exceedingly rare[2]. However, based on a review of the literature with PubMed, a case of a pelvic mass comprising a rare large cervical cyst coated with a cervical high squamous intraepithelial lesion has not been reported until now.
Cervical cysts are a common disease and usually do not require special treatment. Large cervical stump cysts are a rare type of disease, as total hysterectomies are performed infrequently in patients with benign uterine diseases. However, it is rare when a cervical cyst is located in the pelvis, which manifests as a pelvic mass. Thus, we report this rare case, and a review of the literature is described. We hope that this report will benefit the fields of obstetrics and gynecology. After a patient has undergone supracervical hysterectomy, obstetricians and gynecologists should be aware of the possible common outcomes and rare diseases of the cervical stump and make appropriate treatment programs to avoid excessive and erroneous treatments for the patient.
A 57-year-old woman had been menopausal since the age of 52 years. Her chief complaint was abdominal distention for two months.
The patient had frequent urination, urgency, poor urination, and other compression symptoms for one year. Her symptoms worsened over the last three months. The patient’s daily bowel habits have changed considerably for half a year.
She had undergone subtotal supracervical hysterectomy for multiple leiomyoma 14 years prior and cold knife cervix conization because of a high-grade squamous intraepithelial lesion (HSIL) three years prior.
The patient did not have a history of smoking or drinking.
After a pelvic examination of the patient by two gynecologic oncologists, they found that the pelvic mass was similar to a 4-mo pregnant uterus. The mass was not as hard as a solid tumor and so we describe it as having a slightly hard texture. In addition, the mass with poor activity may be adhering to the tissue structure of the pelvic inner wall due to inflammation and infection. Vaginal examination indicated a normal vagina. Except for bloating and changes in bowel habits, the patient did not have any feeling of pain or other discomfort.
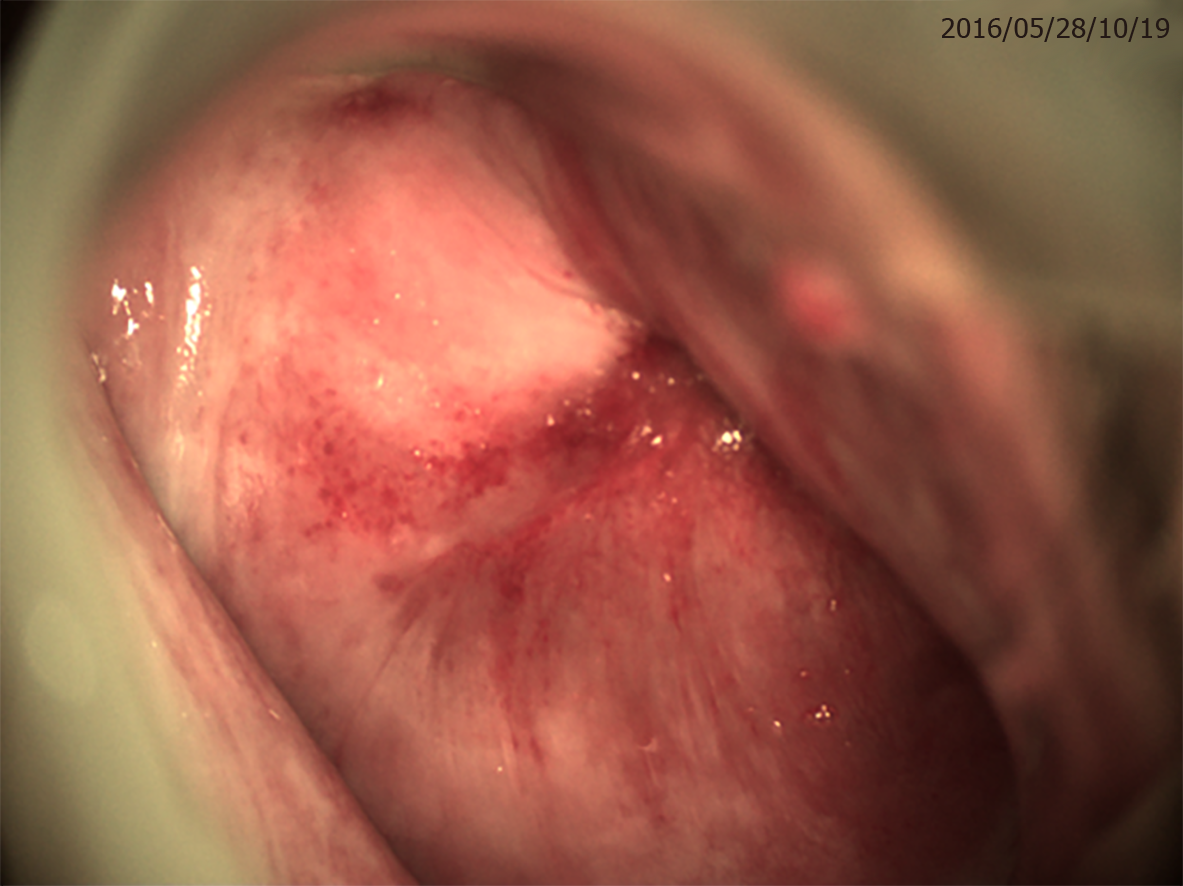
Cervical squamous cell carcinoma antigen (SCCA), a blood tumor marker of cervical cancer, was higher at 2.3 µg/L (reference range: <1.5 ng/mL). Other tumor markers, such as carbohydrate antigen 125 and human epididymal protein 4, were in the normal range (14.9 U/mL and 36.93 pm, respectively). Hormone test results were as follows: Estradiol 2, 33.87 pg/mL; testosterone, 33.58 ng/dL; follicle-stimulating hormone, 36.60 IU/L; prolactin, 7.08 ng/mL; and luteinizing hormone, 19.85 IU/L. In addition, human papilloma virus (HPV) genotypic test results showed that high-risk HPV53 was positive, and a subsequent colposcopy examination demonstrated no exact inner cervical orifice and that the cervical posterior fornix tension seemed strained. The surface of the cervix did not have a distinct acetowhite lesion or obvious anomalous vessels (Figure 1).
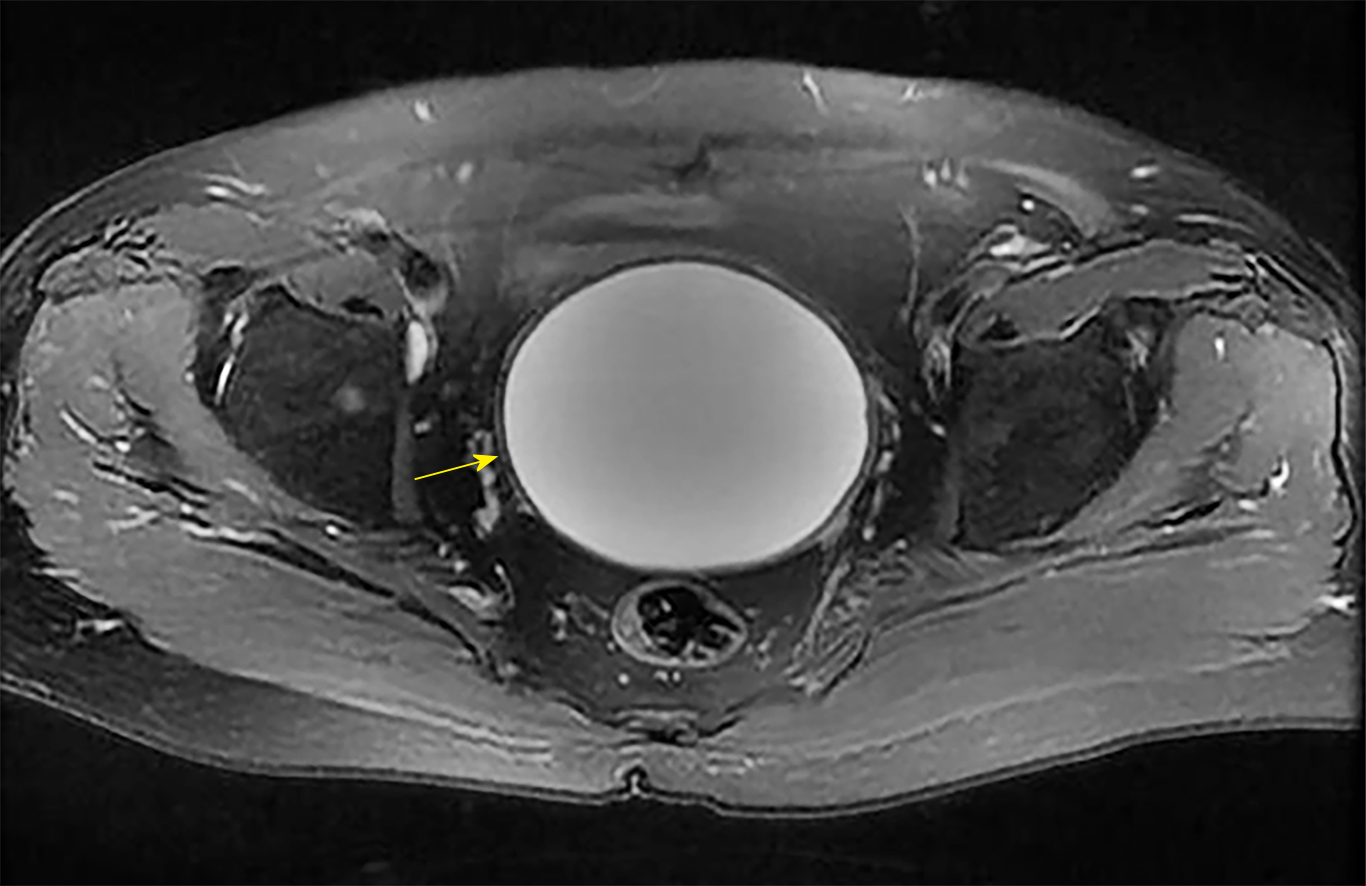
On auxiliary inspection, abdominal ultrasonography detected a 9.1 cm × 8.5 cm × 8.4 cm anechoic mass with silvery fluid in the pelvic cavity and dotted blood flow activity. Pelvic magnetic resonance imaging confirmed a large cystic mass and normal bilateral adnexa (Figure 2).
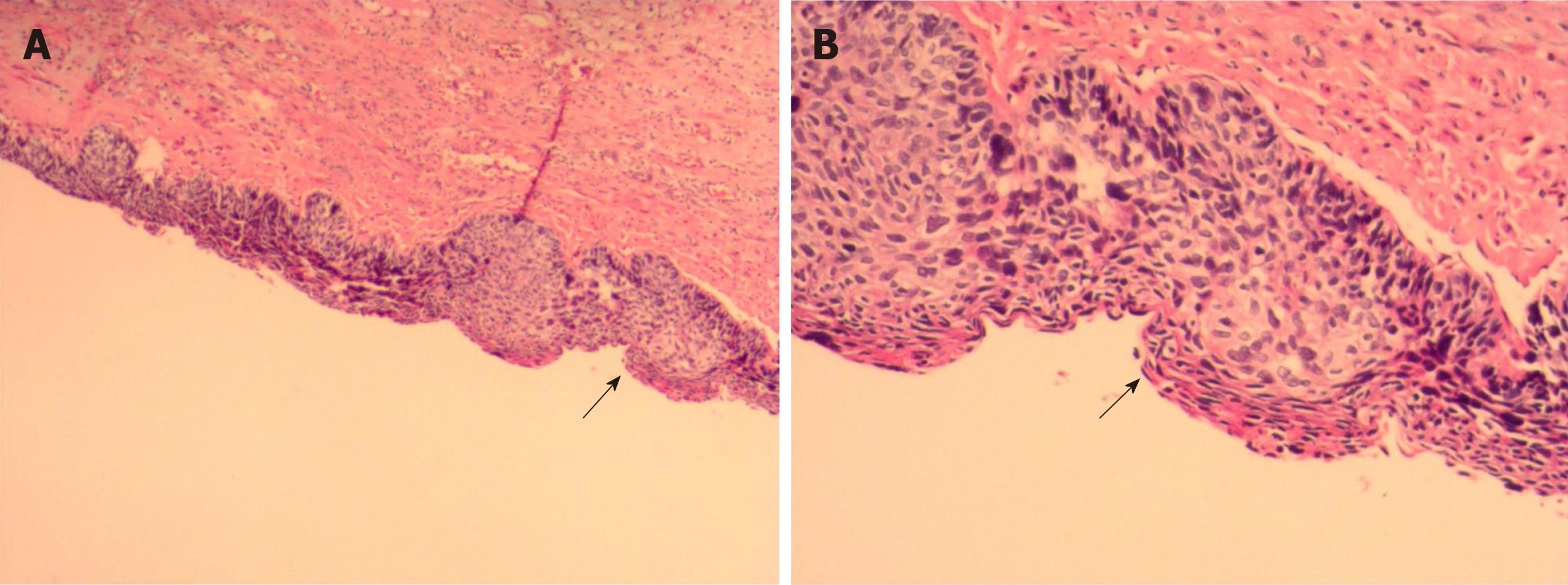
Final pathology confirmed that the pelvic mass was a large inflammatory cyst coated with a cervical high-grade squamous intraepithelial lesion (Figure 3). Dyskaryotic cells but no tumor cells were found in the cyst fluid.
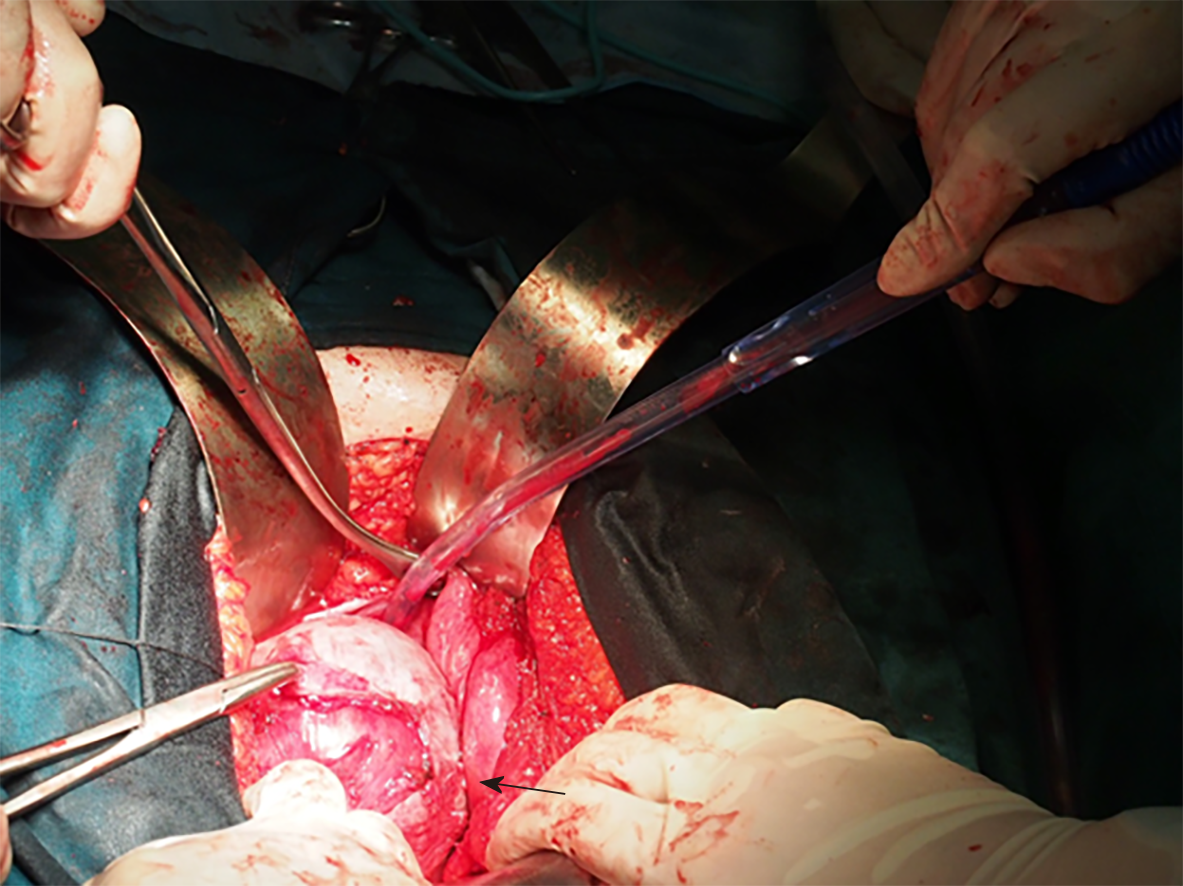
The admission diagnosis we first considered was a pelvic mass mimicking carcinoma of the cervical stump. Its main clinical manifestations are similar to those of cervical cancer. There are no specific early manifestations. However, such a large cervical stump lesion and the clinical manifestations of patients seem to be less supportive of this clinical diagnosis. Therefore, after a general discussion and family agreement, we decided to perform a laparotomy and made an appointment for a rapid frozen biopsy for the patient. A large mass adherent with peripheric tissue was observed during the abdominal operation (Figure 4). Bilateral salpingo-oophorons were atrophic with a smooth surface. The pelvic mass was removed, and a bilateral adnexectomy was implemented. Frozen sectioning was performed, and pathology was suggestive of a fibrous cyst wall coated with a high-grade squamous intraepithelial lesion. Bilateral oophorons showed corpus albicans.
The patient performed well after surgery, and the SCCA level returned to 0.3 µg/L as normal (reference range: <1.5 ng/mL). Outpatient management included close monitoring of the HPV test, SCCA level, and ultrasound. From the vaginal examination, there seemed to be no retained cervical tissue. The patient was discharged one week after surgery. The final follow-up was 42 mo. The patient was generally in good condition, with no recurrence of the vaginal stump.
Occurring during the process of cervicitis healing, secretion of the cervix gland causes hyperplasia in the squamous epithelium, blocking the cervical gland and forming a cystic mass[3]. Thus, primary cervical cysts are a very common gynecological disease. However, giant cysts that occur in the cervical stump are very rare.
Hysterectomy is one of the most basic and effective strategies for functional uterine bleeding, fibroids, and adenomyosis. According to the scope of surgery, hysterectomy can be divided into subtotal supracervical hysterectomy and total hysterectomy[4]. More than 90% of patients undergoing hysterectomy prefer supracervical hysterectomy, which has the advantages of maintaining pelvic support and sexual function, while surgical operators consider the advantages of less operative complications and a simple operation[5]. Therefore, to reduce the complications of hysterectomy associated with ureteral injury and a vaginal cuff abscess, subtotal or supracervical hysterectomy has been performed since the beginning of the last century. However, leaving the cervical stump increases the risks and problematic conditions, including stump carcinoma, which might occur several years after the initial cervical resection. As demonstrated by the pathology, the inner cyst wall was fibrous, and the outer wall was a squamous epithelium with an HSIL in our case. The mechanism by which the squamous epithelium climbed up and wrapped around the mass was unclear. These findings shed light on how to address cervical stump disease, especially precancerous lesions, after subtotal supracervical hysterectomy. It is better to conduct trachelectomy than conization. Vaginal trachelectomy is the preferable approach with the least complications[6]. The woman described herein rejected removal of her cervix and preferred cervical conization. She should be closely followed to monitor whether the vaginal cuff and/or pelvis develops carcinoma or a stump lesion after cervical conization.
Cause of the formation of a very large cyst at the cervical stump: Subtotal hysterectomy preserved the normal anatomy of the vagina for the patient, but the patient had a very large cervical cyst 14 years later. The main cause of the very large cervical cyst was the failure to remove all cervical glands when the cervical tissue was removed. Over the next few decades of chronic inflammatory irritation and subsequent HPV infection, no routine gynecological examination and timely treatment might have led to the development of a very large cervical cyst, which is consistent with literature reports on the reason for the development of primary cervical cysts[7]. Cervical cysts might have no symptoms in the early stages. Nonetheless, long-term cervical cysts could cause a vaginal bulge and compression symptoms, such as frequent urination, urgency, and poor urination, which could seriously affect the quality of life of patients.
For the occurrence of cervical cysts, we recommend that a serrated tube knife of the corresponding caliber, rather than a small serrated tube knife, be used for a loose uterine cervix with a conventional orifice to ensure that the more complete cervical tissue is cut. We should check again to determine whether the cut cervical tissue is integral. If absent, electrocoagulation remains to be conducted in the endocervical tissue. In this way, even if a small amount of gland remains after the cervical tissue is removed, it can become degenerated and necrotic by electrocoagulation, which would avoid the occurrence of postoperative cervical cysts.
Therefore, patients who have a preserved cervical stump should also be followed regularly to actively screen and treat cervical stump lesions. With the extensive development and application of ThinPrep liquid cytology for the screening, HPV testing, electronic colposcopy, etc., cervical stump lesions can be detected, prevented, diagnosed, and cured early.
Indications for residual cervical resection by trachelectomy: Due to benign alternations in the cervical stump, there is a significant risk of developing lesions, such as leiomyoma, even leiomyosarcoma, and stump carcinoma. Once a lesion occurs, further surgical treatment and even postoperative adjuvant therapy (e.g., chemotherapy and radiotherapy), with a much higher complication rate, will be required when the uterus is present[8]. Some studies have been carried out to explore the indications for and complications of removal of the retained cervical stump. Naja et al[9] clearly demonstrated that the indications for residual cervical resection were mainly prolapse, followed by pelvic masses and cervical precancerous lesions. After primary supracervical hysterectomy, 6.8%-19% of patients with periodic bleeding undergo cervical stump resection because they cannot accept more bleeding from the vagina. Kho et al[6] also reported that prolapse, pelvic masses, and abnormal bleeding were the most common indications for trachelectomy for a residual cervical stump after supracervical hysterectomy. Based on reports in the literature, cervical malignancy, a residual tumor, periodic vaginal bleeding, an abnormal pap smear, a pelvic mass, and pain are also indications for trans-abdominal resection of the retained cervical stump[10,11]. In addition, cervical intraepithelial neoplasia and cervical leiomyoma are indications for trans-vaginal surgery. Therefore, we conclude that prolapse of the cervical stump, as well as cervical neoplasia, is the most common reason for performing trachelectomy, which is preinvasive or invasive based on a review of the indications.
Comparison of subtotal hysterectomy and total hysterectomy: As mentioned above, preservation or removal of the uterine cervix has always been the focus of controversy among gynecologists during hysterectomy. Some studies argue that subtotal or supracervical hysterectomy better preserves bladder, sexual, and urinary function, but this hypothesis has not been proven[12,13]. Between 1843 and 1929, the first abdominal hysterectomy was completed by retaining the cervical stump in Manchester until total hysterectomy was performed by Richardson. With the rapid development of minimally invasive surgery, the first laparoscopic supracervical hysterectomy was introduced in 1991[14]. Thus, a growing minority of gynecologists preferred supracervical hysterectomy. From then on, studies on supracervical hysterectomy versus total hysterectomy have been performed. Rahn et al[15] compared the ability of the cervical stump with that of the vaginal cuff to resist downward traction. Their results revealed no difference in resistance to forces applied to the vaginal apex between the two procedures. Moreover, prospective randomized trials have indicated no benefits of supracervical hysterectomy on perioperative morbidity[16]. In a study by Ala-Nissilä et al[17], a comparison of long-term outcomes, including sexual symptoms, urinary incontinence, and genital prolapse, revealed no significant differences after supracervical and total abdominal hysterectomy during a follow-up period of 33 years.
However, supporters of supracervical hysterectomy demonstrated that operative morbidity could be decreased through laparoscopic supracervical hysterectomy for women with a large uterus (>500 g) but no contraindication for a residual cervix[18]. Currently, new cohort studies have shown that subtotal hysterectomy has less effect on the patient’s sexual function than total resection, which is beneficial to ensure the patient’s physical and mental health[19]. On the other hand, subtotal hysterectomy has less effect on supporting pelvic floor ligament tissue and can reduce the incidence of pelvic organ prolapse after total hysterectomy[20]. Furthermore, it can also avoid damage to the bladder, rectum, ureter, and nerves that control the bladder during surgery. A recent meta-analysis by Aleixo et al[21] in 2019 found that subtotal hysterectomy had less intraoperative blood loss, operative time, and hospital stay compared to total hysterectomy.
Opponents of subtotal hysterectomy claim that subtotal hysterectomy is faster, has less perioperative bleeding, and seems to have fewer intra- and postoperative complications. Nevertheless, the cervix does not show improved sexual functioning after surgery[22]. Women often believe that preserving the cervix means that they will retain satisfactory sexual function. Some studies have shown that total hysterectomy does not affect sexual satisfaction or libido[23,24]. Moreover, both laparoscopic total hysterectomy and subtotal hysterectomy induce a comparable improvement in long-term sexual functioning, especially in patients with impaired sexuality presurgery[25]. In addition, a residual cervix after subtotal hysterectomy may still require surgery again when a lesion occurs. Therefore, as the uterus has been resected, changes in the normal anatomical structure of the pelvis, the tight adhesion of tissues and organs, and intraoperative bleeding would greatly increase the difficulty of the second operation and challenge the surgeons. Additionally, for other reasons (e.g., infection control), supracervical or subtotal hysterectomy subsequently should not be recommended as a superior technique.
For patients who undergo subtotal or supracervical hysterectomy, attention should be paid to the exclusion of malignant diseases. The examination of a cervical smear and colposcopy can be performed to exclude cervical precancerous lesions and cervical cancer. Patients with irregular vaginal bleeding should be treated by segmental curettage or hysteroscopy to exclude endometrial lesions. The uterus should be dissected immediately after the uterus is removed during the operation. Suspected malignant disease should be examined by rapid frozen sectioning, and the scope of the operation should be determined according to the results to avoid the trauma of a reoperation after surgery[4]. However, for patients with endometriosis diagnosed before subtotal hysterectomy, endometriotic lesions are often located in the uterine ligament, uterine rectum, and posterior wall of the lower uterus, which preserves residual lesions in the cervix, leading to recurrence. Therefore, patients with endometriosis who need to have their uterus removed do not advocate for preservation of the cervix. Special attention should be also be paid to the anatomical relationship during the second operation for cervical stump lesions. The adhesion should be carefully separated, the bleeding should be completely stopped, the injury should be prevented, and the complications should be treated in a timely manner.
Cervical stump cysts are one of the most uncommon benign cervical lesions encountered by gynecologists. Due to their rarity, it is easy to escape a correct preoperative diagnosis, and these cysts are usually misdiagnosed as ovarian serous cystadenocarcinoma or ovarian mucinous cystadenocarcinoma. When addressing benign uterine diseases, gynecologists should choose the most suitable surgical method based on the patient’s condition and wishes. If the cervix is retained, patients require a close follow-up.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mrzljak A, Ozturk E S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Hannoun-Lévi JM, Peiffert D, Hoffstetter S, Luporsi E, Bey P, Pernot M. Carcinoma of the cervical stump: retrospective analysis of 77 cases. Radiother Oncol. 1997;43:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Zhiqiang L, Bin S, Min F, Yufang L. Leiomyosarcoma of cervical stump following subtotal hysterectomy: a case report and review of literature. Eur J Gynaecol Oncol. 2016;37:148-151. [PubMed] |
| 3. | Lee J, Kim S, Nam EJ, Hwang SM, Kim YT, Kim SW. Single-port access versus conventional multi-port access total laparoscopic hysterectomy for very large uterus. Obstet Gynecol Sci. 2015;58:239-245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Sloth SB, Schroll JB, Settnes A, Gimbel H, Rudnicki M, Topsoee MF, Joergensen A, Nortvig H, Moeller C. Systematic review of the limited evidence for different surgical techniques at benign hysterectomy: A clinical guideline initiated by the Danish Health Authority. Eur J Obstet Gynecol Reprod Biol. 2017;216:169-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Munro MG. Supracervical hysterectomy: ... a time for reappraisal. Obstet Gynecol. 1997;89:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Kho RM, Magrina JF. Removal of the retained cervical stump after supracervical hysterectomy. Best Pract Res Clin Obstet Gynaecol. 2011;25:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Donnellan NM, Mansuria S, Aguwa N, Lum D, Meyn L, Lee T. Obesity and older age as protective factors for vaginal cuff dehiscence following total hysterectomy. Gynecol Surg. 2015;12:89-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Petersen LK, Mamsen A, Jakobsen A. Carcinoma of the cervical stump. Gynecol Oncol. 1992;46:199-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Naja G, Mustin C, Volesky B, Berthelin J. Stabilization of the initial electrochemical potential for a metal-based potentiometric titration study of a biosorption process. Chemosphere. 2006;62:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | El-Zohairy MA. Trachelectomy: a review of 15 cases. J Egypt Natl Canc Inst. 2010;22:185-190. [PubMed] |
| 11. | Pratt JH, Jefferies JA. The retained cervical stump. A 25-year experience. Obstet Gynecol. 1976;48:711-715. [PubMed] |
| 12. | Maas CP, Kenter GG, Trimbos B. Outcomes after total versus subtotal abdominal hysterectomy. N Engl J Med. 2003;348:856-7; author reply 856-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Asnafi N, Basirat Z, Hajian-Tilaki KO. Outcomes of total versus subtotal abdominal hysterectomy. East Mediterr Health J. 2010;16:176-179. [PubMed] |
| 14. | Semm K. [Hysterectomy via laparotomy or pelviscopy. A new CASH method without colpotomy]. Geburtshilfe Frauenheilkd. 1991;51:996-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 124] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Rahn DD, Marker AC, Corton MM, Roshanravan SM, McIntire DD, Schaffer JI, Wai CY. Does supracervical hysterectomy provide more support to the vaginal apex than total abdominal hysterectomy? Am J Obstet Gynecol. 2007;197:650.e1-650.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 388 November 2007: supracervical hysterectomy. Obstet Gynecol. 2007;110:1215-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Ala-Nissilä S, Haarala M, Järvenpää T, Mäkinen J. Long-term follow-up of the outcome of supracervical versus total abdominal hysterectomy. Int Urogynecol J. 2017;28:299-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | McGurk L, Oliver R, Odejinmi F. Laparoscopic supracervical hysterectomy for the larger uterus (>500 g): a case series and literature review. Arch Gynecol Obstet. 2017;295:397-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Berlit S, Lis S, Jürgens S, Buchweitz O, Hornemann A, Sütterlin M, Tuschy B. Postoperative sexual functioning in total versus subtotal laparoscopic hysterectomy: what do women expect? Arch Gynecol Obstet. 2017;296:513-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Andersen LL, Alling Møller LM, Gimbel HM. Objective comparison of subtotal vs. total abdominal hysterectomy regarding pelvic organ prolapse and urinary incontinence: a randomized controlled trial with 14-year follow-up. Eur J Obstet Gynecol Reprod Biol. 2015;193:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Aleixo GF, Fonseca MCM, Bortolini MAT, Brito LGO, Castro RA. Total Versus Subtotal Hysterectomy: Systematic Review and Meta-analysis of Intraoperative Outcomes and Postoperative Short-term Events. Clin Ther. 2019;41:768-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Gimbel H. Total or subtotal hysterectomy for benign uterine diseases? A meta-analysis. Acta Obstet Gynecol Scand. 2007;86:133-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Okaro EO, Jones KD, Sutton C. Long term outcome following laparoscopic supracervical hysterectomy. BJOG. 2001;108:1017-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Nathorst-Böös J, Fuchs T, von Schoultz B. Consumer’s attitude to hysterectomy. The experience of 678 women. Acta Obstet Gynecol Scand. 1992;71:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 53] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Berlit S, Tuschy B, Wuhrer A, Jürgens S, Buchweitz O, Kircher AT, Sütterlin M, Lis S, Hornemann A. Sexual functioning after total versus subtotal laparoscopic hysterectomy. Arch Gynecol Obstet. 2018;298:337-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |