Published online Jan 6, 2020. doi: 10.12998/wjcc.v8.i1.140
Peer-review started: September 22, 2019
First decision: October 24, 2019
Revised: November 3, 2019
Accepted: November 15, 2019
Article in press: November 15, 2019
Published online: January 6, 2020
Processing time: 106 Days and 8.1 Hours
Lymphangioma is a benign lesion that rarely involves the gastrointestinal tract, especially in adults. Small bowel lymphangioma is a rare cause of gastrointestinal bleeding. Here, we report a case of an adult diagnosed with jejunal lymphangioma presenting with melena, anemia and hypogammaglobulinemia. We also summarize and analyze all 23 reported cases from 1961 to 2019, and propose an algorithm for identification and management of small bowel lymphangioma.
A case of a 29-year-old woman presented with persistent melena and iron-deficiency anemia, accompanied by hypogammaglobulinemia. No lesions were found in the initial workup with esophagogastroduodenoscopy, colonoscopy and computed tomography (CT) enterography. Ultimately, capsule endoscopy and double-balloon enteroscopy revealed a 3 cm × 2 cm primary lesion with intensive white lymphatic dilatatory changes and visible fresh blood stains, accompanied by a small satellite lesion. The patient underwent complete surgical resection of these lesions, and histopathological examination confirmed a diagnosis of cavernous lymphangioma of the jejunum. The patient showed no evidence of disease at the time of this report.
We recommend CT, capsule endoscopy and enteroscopy to identify the lesions of lymphangioma. Laparoscopic surgery with histological diagnosis is an ideal curative method.
Core tip: Lymphangioma is a benign lesion that rarely occurs in the gastrointestinal tract of adults. Small bowel lymphangioma is an especially rare cause of gastrointestinal bleeding. We present a case of jejunal lymphangioma manifested as melena and anemia, accompanied by hypogammaglobulinemia. We also summariz and analyz all 23 reported cases from 1961 to 2019, and proposed an algorithm for identification and management of this disease.
- Citation: Tan B, Zhang SY, Wang YN, Li Y, Shi XH, Qian JM. Jejunal cavernous lymphangioma manifested as gastrointestinal bleeding with hypogammaglobulinemia in adult: A case report and literature review. World J Clin Cases 2020; 8(1): 140-148
- URL: https://www.wjgnet.com/2307-8960/full/v8/i1/140.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i1.140
Lymphangioma is a benign lesion of the lymphatic system that usually occurs in the head, neck and axillae in children, but rarely in adults. Gastrointestinal tract involvement of lymphangioma is especially rare within the small intestine, comprising less than 1% of all cases[1]. Small bowel and mesenteric lymphangiomas are rare causes of gastrointestinal bleeding[2]. Their etiology remains unclear, but is generally believed to be a developmental failure to establish normal communication with regional lymphatic drainage, resulting in dilatation of lymphatic channels[3]. Lymphangiomas are classified as simple capillary, cavernous and cystic types.
We present a case of small bowel lymphangioma manifesting as persistent gastrointestinal bleeding and iron-deficiency anemia in a young woman, accompanied by mild lymphopenia and hypogammaglobulinemia. We searched Medline and PubMed from inception up to September 1, 2019 for “lymphangioma”, “small intestine”, “small bowel”, “jejunum” and “ileum” as key words. Patients with mesenteric lesions were excluded, and no language limitation was set. We summarized and analyzed all 23 reported cases, and proposed an algorithm for identification and management of this disease.
A 29-year-old female patient presented with persistent mild melena for > 1 year.
The patient described melena once daily, with 50–100 mL per occurrence, without abdominal pain, hematochezia, or hematemesis. She experienced worsening fatigue and palpitations after activities. On initial evaluation, moderate to severe anemia and a positive fecal occult blood test were found. Hemoglobin was only transiently improved by oral supplementation with ferrous succinate 300 mg/d.
On admission, vital signs were stable and within normal limits. Physical examination revealed pallor and absence of abdominal signs. The rectal examination showed the presence of a small amount of tarry stool.
Laboratory data revealed iron deficiency anemia with hemoglobin level of 6.8 g/dL (normal range 11–15 g/dL), accompanied by elevation in reticulocytes to 7.32% (0.5–2.5%). Also notable were mild lymphopenia 0.75 × 109/L (0.8 × 109–4.0 × 109/L), decreased IgG 2.91 g/L (7.0–17.0 g/L), IgA 0.69 g/L (0.7–4.0 g/L) and normal IgM 0.69 g/L (0.40–2.30 g/L). Serum albumin was borderline low at 35 g/L (35–52 g/L). Serum tumor markers were unremarkable. Autoimmune antibodies were negative. The patient then underwent whole gastrointestinal tract assessment.
Although esophagogastroduodenoscopy (EGD) and colonoscopy did not reveal an obvious bleeding source, melenic liquid was seen in the terminal ileum. However, no lesion was found by abdominal/pelvic contrasted computed tomography enterography (CTE). 99mTechnetium-labeled red blood cell (99mTc-RBC) scintigraphy revealed a suspected bleeding site in the jejunum. Capsule endoscopy and double-balloon enteroscopy (DBE) were performed, revealing a 3 cm × 2 cm primary discoid elevated lesion in the middle jejunum, with intense white lymphatic dilatation and visible fresh blood stains. A small satellite lesion with the appearance of a white nodule was found 25 cm distal to the primary lesion (Figure 1A and B). Biopsies showed lymphatic hyperplasia with dilation. 18F-Fluorodeoxyglucose positron-emission tomography/computed tomography (18F-FDG PET/CT) did not reveal local uptake to suggest lymphoma.
Given the patient’s persistent gastrointestinal bleeding, and critical level of hemoglobin, the patient underwent small bowel segmental resection. The primary lesion was found 200 cm distal to the ligament of Treitz. The total length of resected small bowel was about 30 cm, including the small satellite lesion (Figure 1C).
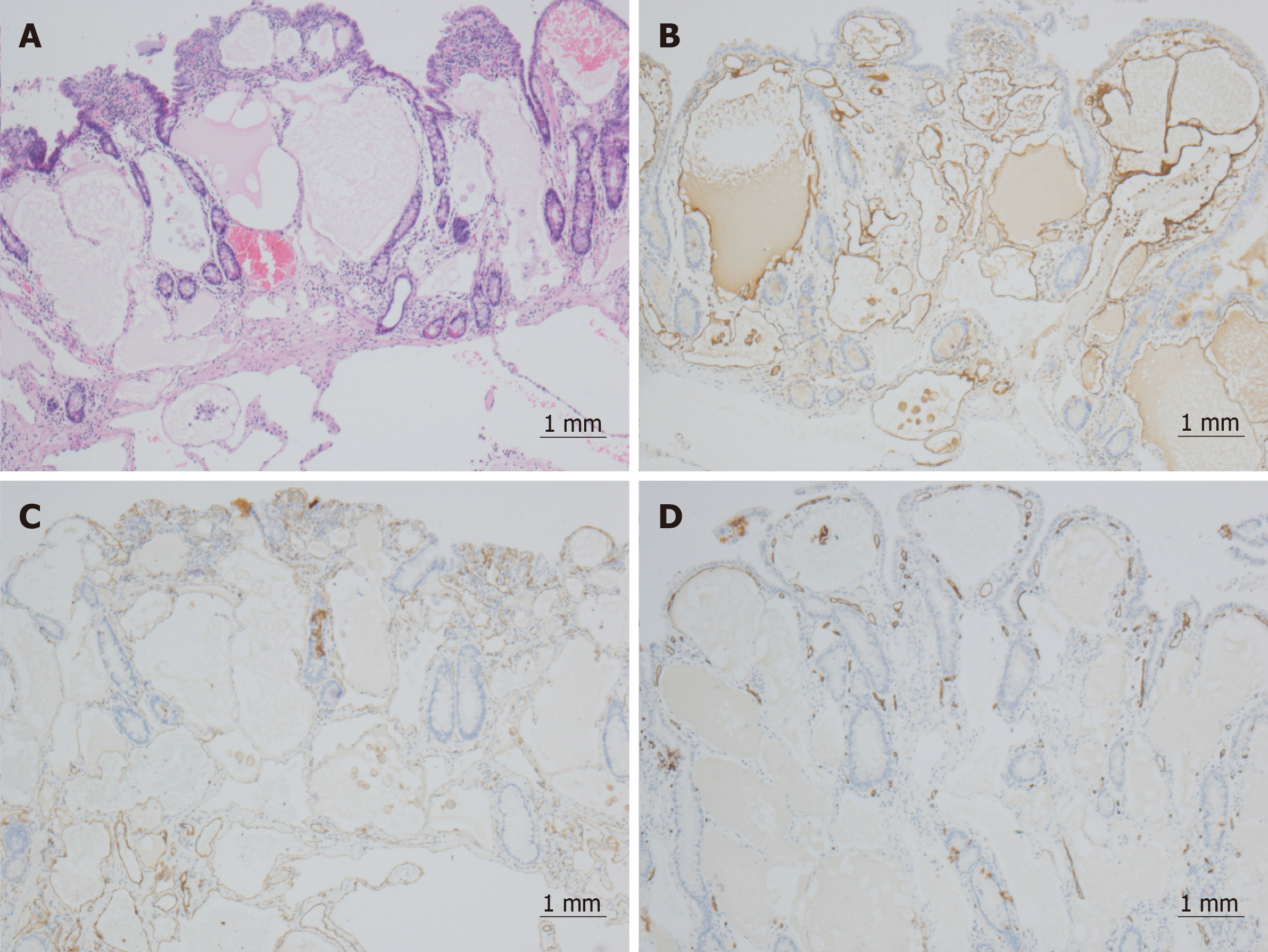
Microscopically, variably sized cysts were identified in both mucosal lamina propria and submucosa layers. The lumen was filled with lymphatic fluid and also contained RBCs and lymphocytes (Figure 2A). The cysts were lined by a single layer of flattened cells without atypia, which were positive for D2-40 and CD31 and negative for CD34 (Figures 2B-D) in immunochemical staining. A diagnosis of cavernous lymphangioma of the jejunum was made.
No further melena or anemia was noted after follow-up for 1 year, with hemoglobin (13.5 g/dL), lymphocytes (1.63 × 109/L) and immunoglobulins (IgG 8.63 g/L, IgA 1.10 g/L and IgM 1.77 g/L) values back to normal levels. As of this report, the patient was asymptomatic and showed no evidence of disease.
We present a case of a young female patient with persistent melena and moderate-to-severe iron-deficiency anemia, accompanied by mild lymphopenia and hypogammaglobulinemia. With the negative findings under EGD, colonoscopy and CTE, capsule endoscopy and DBE revealed a 3 cm × 2 cm primary lesion with a small satellite. She was diagnosed with cavernous lymphangioma of the jejunum with histopathological examination, and cured by surgical resection.
With rapid development in advanced endoscopic techniques, including enteroscopy, jejunal lymphangioma has become less rare than before. As a result, there is an unmet need for an algorithm for identification and management of this entity. However, evidence to date is limited to a small number of case reports. In the period from 1961 to September 1, 2019, only 22 adult cases of small intestinal lymphangioma were reported, when excluding patients with mesenteric lesions. We summarize and analyze these 22 cases alongside this current case report in Table 1[1,4-23].
| Ref. | Age/ gender | Ethnicity/ country | Symptoms | Laboratory results | Imaging/ endoscopy | Location | Layer/ appea-rance | Number/ size | Treatment | Pathology |
| Present case | 29/F | Asian/ China | Melena, fatigue, palpitations after activities | Anemia: Hgb 6.8 g/dL; IgG 2.91 g/L | Neg: EGD, CLS, CTE, PET/CT Pos: 99mTC-RBC-S, DBE | Mid-jej | SM/LP, elevated lesion with white lymphatic dilatation changes and fresh blood stains | 1/3 cm × 2 cm + 1/ satellite | Surgery | Cavernous Lpgm |
| Samuelson et al[4], 2018 | 70/M | Caucasian/American | Weight loss, hemate-mesis, abdominal pain, | — | Pos: CT (intussus-ception) | Jej | — | 1/2.5 cm | Surgery | Lpgm |
| Lim et al[1], 2018 | 70/M | Asian/ South Korea | Melena, dizziness | Anemia: Hgb 5.2 g/dL | Pos: ES | Prox-jej | SM; yellow-white polyploids with bleeding | Mu/small | Surgery (TT) | Lpgm |
| Huang et al[5], 2017 | 58/M | Asian/ Taiwanese | Melena/ dyspnea/ dizziness | Anemia: Hgb 3.5 g/dL | Neg: EGD, CLS; Pos: CT, SBE | 3rd Duo | Soft, yellow-pink, lobulated mass | 1/15 cm × 15 cm | Surgery (Lap) | Lpgm |
| Ng et al[6], 2016 | 33/M | Asian/ Singapore | Episodic melena, dyspnea, lethargy | Anemia: Hgb 3.9 g/dL | Neg: EGD, CLS; Pos: CT, SBE | Prox-jej | LP/SM; “strawberry” polyploids | 1/2.2 cm × 2.0 cm | Surgery (Lap, TT) | Cavernous Lpgm |
| Tseng et al[7], 2016 | 88/F | Asian/ China Taiwan | Episodic melena, fatigue, shortness of breath | Anemia: Hgb 8 g/dL | Neg: EGD, CLS; Pos: CE, SBE | Dis-Duo, Prox-jej | Lobular circumfe-rential | 1/2.8 cm × 2.4 cm+Mu/satellite | Surgery (Lap) | Cavernous Lpgm |
| Limaiem et al[8], 2015 | 22/F | Caucasian/Tunis | intermittent colicky abdominal pain, diarrhea | Anemia | Pos: CT/US (intussus-ception) | Jej | SM; peduncu-lated polyp | 1/2 cm | Surgery (Lap) | Lpgm |
| Bucciero et al[9], 2015 | 28/M | Caucasian/ Italy | Melena | Anemia: Hgb 4.0 g/dL | Pos: CT (inhomo-geneous mass) | 3rd Duo | Circumferential ulcerated with bleeding | Mu/small | Surgery | Lpgm |
| Antonino et al[10], 2014 | 24/F | Caucasian/ Italy | Melena | Anemia: Hgb 6.8 g/dL | Pos: EGD, MRI | 2nd Duo | Ulcerated polypoid | 1/5 cm | Surgery | Hemo-Lpgm |
| Kida et al[11], 2012 | 81/F | Asian/ Japan | Melena | Anemia:Hgb 5.0 g/dl | Neg: EGD, CLS, CT; Pos: CE | Prox-jej | SM/LP; white-yellowish peduncu-lated polyp | 1/2 cm × 1 cm | Polypec-tomy+hemoclipping+APC (DBE) | Lpgm |
| Fang et al[12], 2012 | 57/F | Asian/ China | Melena | Anemia | Neg: EGD; Pos: ES | Prox-jej | — | 1/5 cm × 4 cm | Surgery | Hemo-Lpgm |
| Mavrogenis et al[13], 2011 | 26/F | Caucasian/ France | Melena | Anemia | Neg: EGD, CLS, CT; Pos: CE | Prox-jej | Whitish carpet-like villi and superficial red spots | 1/ circumference 2/3 | Surgery (Lap) | Hemo-Lpgm |
| Mavrogenis et al[13], 2011 | 59/F | Caucasian/ France | Melena | Anemia | Neg: EGD, CLS; Pos: CE | Prox-jej | Polypoid covered whitish and red spots | 1/3.5 cm × 7 cm | Surgery | Hemo-Lpgm |
| Morris-Stiff et al[14], 2011 | 34/M | Caucasian/American | Dyspnea | Anemia: Hgb 6 g/dL | Pos: CT, CE, ES | Prox-jej | SM; lobular circumfe-rential | 1/5.3 cm × 4 cm × 1.5 cm | Surgery (TT) | Lpgm |
| Huang et al[15], 2009 | 57/M | Caucasian/American | Melena, shortness of breath | Anemia: Hgb 7.6 g/dL | Neg: EGD, CLS; Pos:CE, DBE | Mid-jej | Firm mass with central ulceration | 1/3.5 cm × 2.2 cm | Surgery (Lap) | Carvernous Lpgm |
| Hsu et al[16], 2007 | 75/M | Asian/ China Taiwan | Melena | Anemia | Neg: EGD, CLS, BR, CT; Pos: 99mTC-RBC-S, DBE | Dis-jej | SM; circumfe-rential | 1/6 cm × 4 cm | Surgery (Lap) | Lpgm |
| Griffa et al[17], 2006 | 54/M | Caucasian/ Italy | Episode of melaena | Anemia | Neg: EGD, CLS, US; Pos: CE | Mid-jej | SM; white-yellowish polypoid | 1/1.5 cm × 2 cm | Surgery (Lap) | Lpgm |
| Honda et al[18], 2003 | 31/F | Asian/ Japan | Melena | Anemia: Hgb 5.3 g/dL | Neg: EGD, CLS; Pos: BR, CT, ES | Prox-jej | Lobulated, yellowish-white surface with red and white specks | 1/3.5 cm × 3 cm | Surgery | Lpgm |
| Ishikawa et al[19], 1999 | 64/M | Asian/Japan | Melena | Anemia | Pos: BR,DBE | Upper-Ile | SM | 1/5.5 cm × 3 cm | Surgery | Cavernous Lpgm |
| Barquist et al[20], 1997 | 33/F | Caucasian/Panama | Chronic gastrointe-stinal blood | Anemia: Hgb 5.5 g/dL | Neg: EGD; Pos: ES | Mid-Jej | SM | 1/3.3 cm × 2.5 cm × 1.0 cm | Surgery (Lap) | Cavernous Lpgm |
| Hanagiri et al[21], 1992 | 53/M | Asian/ Japan | Bowel obstruction | Hgb 11 g/dL | Pos: CT | Jej | SM, smooth and yellowish | 1/2.5 cm × 2 cm | Surgery (Lap) | Cavernous Lpgm |
| Colizza et al[22], 1981 | 58/F | Caucasian/ Italy | Melena | Anemia: Hgb 7.5 g/dL | Neg: BR | SMH, Prox-jej | SM/LP | 2/4 cm × 5 cm | Surgery (Lap) | Cystic Lpgm |
| Ralston[23], 1961 | 58/M | Caucasian/Australian | Gastrointe-stinal bleeding | Anemia: Hgb 6.6 g/dL | Neg: BR,EGD | Prox-jej | SM | 1/1 cm × 0.5 cm | Surgery | Hemo-Lpgm |
Over the 58 years, nearly two-thirds of cases (18/23, 78.2%) were reported in the past 20 years. Among the 23 patients, Caucasians from Europe and the United States accounted for 52.2%, while Asians accounted for 47.8%, with most cases occurring in Japan. Among the 23 patients with detailed information, the male-female ratio was almost equal (52.2% vs 47.8%). In contrast to the predominance in young adults seen with congenital lymphatic dysplasia, the median age was 50 years, with a range of 22–88 years. Due to its slow-growing character, lymphangioma is often only diagnosed after the clinical symptoms appear with significantly increased size of the tumor.
The common clinical manifestations were persistent/episodic melena and refractory iron-deficiency anemia with average hemoglobin 6.18 ± 1.93 g/dL in the 15 patients with known complete blood counts. Depending on the size of the lesion, patients may present with a chief complaint of abdominal pain as a result of intussusception. One notable feature of this case was the rare finding of mild lymphopenia and hypogammaglobulinemia, which was not mentioned in any previous case. This is thought to be due to the excessive loss of lymphatic fluid containing lymphocytes and immunoglobulins into the intestinal lumen caused by local lymphatic dilatation of the lesions[24]. Leakage of these serum proteins occurs independently of their molecular weight. The reduction in serum levels is prone to occur for proteins with slow catabolic rate (e.g., IgG and albumin), since their loss is greater than their synthesis. These changes can be completely corrected after surgery.
Radiology and endoscopy are valuable methods for the diagnosis and management of the jejunal lymphangioma. Except in the case of intussusception, lymphangioma typically appears as well-defined, nonenhancing, homogeneous, low-attenuation cystic masses with intact overlying intestinal mucosa[25]. However, as a positive finding on CT only occurred in 39.1% of cases, use of capsule endoscopy and enteroscopy would minimize the risk of a missed diagnosis. 99mTc-RBC scintigraphy also played a role in confirming the existence and localization of unexplained gastrointestinal bleeding. Negative PET/CT can effectively exclude lymphoma from the differential diagnosis. All cases were located in the proximal small intestine, most commonly in the proximal jejunum (11/23, 47.8%), followed by middle jejunum (4/23, 17.4%) and duodenum (4/23, 17.4%). Most of the lymphangiomas were solitary (20/23, 87.0%), with a minority of cases reported with satellite lesions (13.0%, 3/23). The mean diameter of the primary lesion was 3.67 cm, and they mainly manifested as white–yellow polypoid (12/15, 80.0%) and circumferential (3/15, 20.0%) lesions with bleeding, all located in the submucosa or lamina propria. Comprehensive assessment of the whole gastrointestinal tract was critical.
All 22 patients with treatment records were cured with segmental intestinal resection, and more recent cases were successfully treated by laparoscopic surgery with tattooing markers. Only one patient was successfully treated with polypectomy under DBE, with hemoclipping combined with argon plasma coagulation for hemostasis. Lymphangioma was diagnosed by histological examination, and four patients were diagnosed with hemolymphangioma with positive CD31 and CD34.
Since lymphangioma in adults can be asymptomatic and varied, we need to distinguish it from lymphangiectasia. The superficial mucosal layers that consist of confluent dilated spaces with a smooth muscle component are more involved in lymphangioma. Lymphangiectasia consists of more widely spaced mucosal and submucosal cystic spaces, which lack smooth muscle and prominent endothelial lining. Hence, lymphangioma can be reliably distinguished from lymphangiectasia by pathological characteristics[26]. However, lymphangiosarcoma rarely involves the gastrointestinal tract in adults.
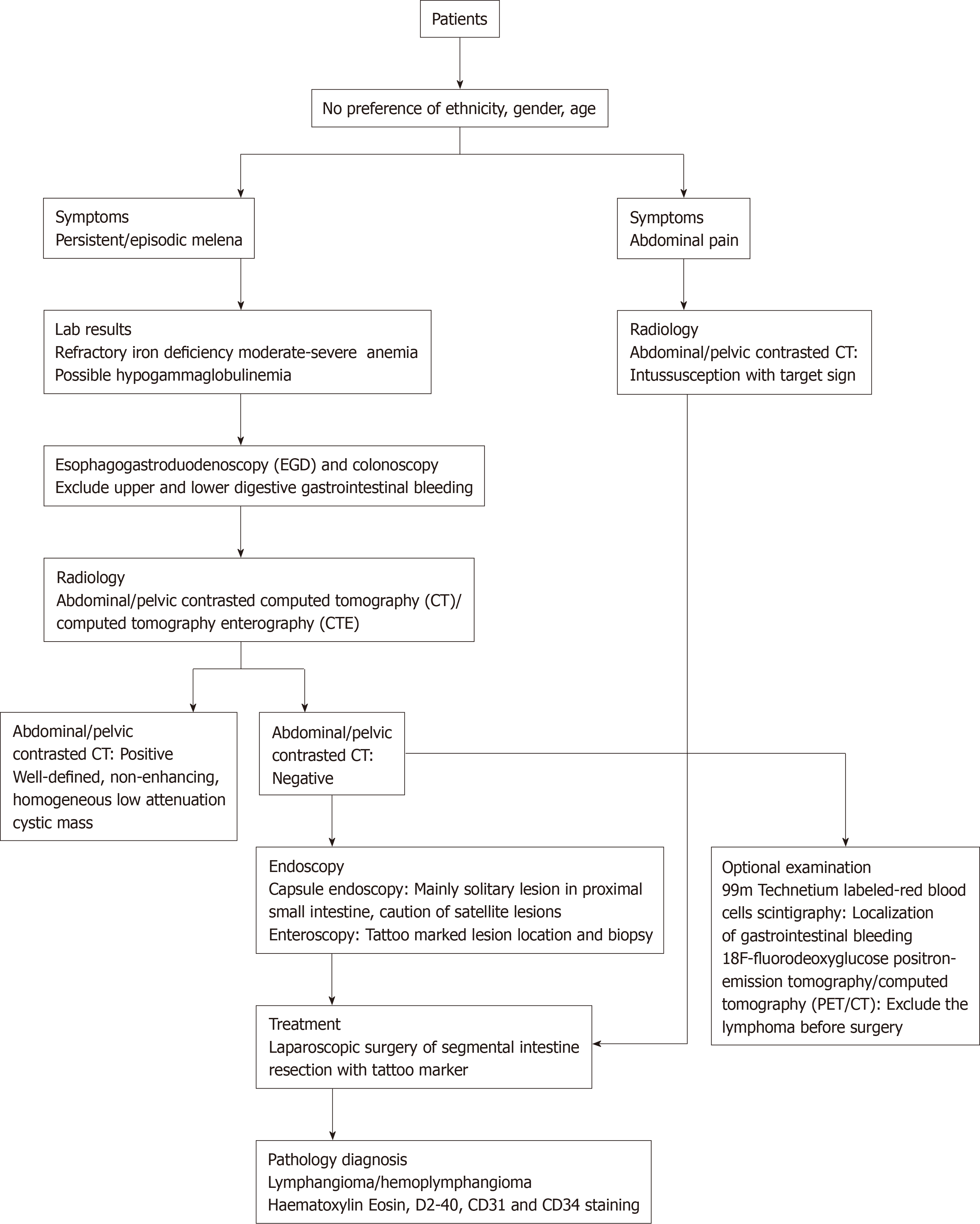
In summary, we propose an algorithm with a goal of timely identification and management of small intestine lymphangioma (Figure 3). For patients with melena and refractory iron-deficiency anemia, no gender and age preference, we first recommend EGD and colonoscopy to exclude the upper and lower digestive tract bleeding. Then, abdominopelvic contrasted CT was recommended to identify or exclude intussusception, as well as potential discovery of lesions in one-third of cases. With negative findings in CT, capsule endoscopy and enteroscopy are critical to assess all lesions with tattoo markers. Although most lymphangiomas present as solitary lesions in the proximal jejunum, attention must be paid to the possibility of satellite lesions. Finally, laparoscopic surgery with segmental intestinal resection with a tattoo marker remains the ideal curative method. The final diagnosis of lymphangioma/hemolymphangioma will be made by histological examination.
We would like to express our sincere gratitude to Dr. Ritchell van Dams, MD, MHS from Department of Radiation Oncology, University of California, Los Angeles, for his review and extensive editing of the manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rodrigo L, Tabibian J S-Editor: Ma YJ L-Editor: MedE-Ma JY E-Editor: Qi LL
| 1. | Lim DR, Kuk JC, Kim T, Shin EJ. Surgery of multiple lymphangioma in small bowel: a rare case report of chronic gastrointestinal bleeding. Ann Surg Treat Res. 2018;94:52-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Xu X, Liu W, Zheng C. A rare cause of repeated gastrointestinal bleeding. Mesenteric cavernous lymphangioma. Gastroenterology. 2014;146:e11-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Suthiwartnarueput W, Kiatipunsodsai S, Kwankua A, Chaumrattanakul U. Lymphangioma of the small bowel mesentery: a case report and review of the literature. World J Gastroenterol. 2012;18:6328-6332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 52] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Samuelson H, Giannotti G, Guralnick A. Jejunal lymphangioma causing intussusception in an adult: An unusual case with review of the literature. Ann Med Surg (Lond). 2018;34:39-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Huang MY, Chang HM, Gao HW, Huang TY. Small Intestinal Lymphangioma With Lymphangioectasia Causing Obscure Gastrointestinal Bleeding. Am J Gastroenterol. 2017;112:413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Ng JJ, Lau JW, Shabbir A. A Rare Cause of Obscure Gastrointestinal Bleeding. Gastroenterology. 2016;150:40-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Tseng CM, Su YC, Tai CM. An Unusual Cause of Obscure Gastrointestinal Bleeding. Gastroenterology. 2016;150:e9-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 104] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 8. | Limaiem F, Khalfallah T, Marsaoui L, Bouraoui S, Lahmar A, Mzabi S. Jejunal lymphangioma: an unusual cause of intussusception in an adult patient. Pathologica. 2015;107:19-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Bucciero F, Marsico M, Galli A, Tarocchi M. Small bowel lymphangioma: A rare case of intestinal bleeding. Dig Liver Dis. 2015;47:815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Antonino A, Gragnano E, Sangiuliano N, Rosato A, Maglio M, De Palma M. A very rare case of duodenal hemolymphangioma presenting with iron deficiency anemia. Int J Surg Case Rep. 2014;5:118-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Kida A, Matsuda K, Hirai S, Shimatani A, Horita Y, Hiramatsu K, Matsuda M, Ogino H, Ishizawa S, Noda Y. A pedunculated polyp-shaped small-bowel lymphangioma causing gastrointestinal bleeding and treated by double-balloon enteroscopy. World J Gastroenterol. 2012;18:4798-4800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Fang YF, Qiu LF, Du Y, Jiang ZN, Gao M. Small intestinal hemolymphangioma with bleeding: a case report. World J Gastroenterol. 2012;18:2145-2146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Mavrogenis G, Coumaros D, Lakhrib N, Renard C, Bellocq JP, Leroy J. Mixed cavernous hemangioma-lymphangioma of the jejunum: detection by wireless capsule endoscopy. Endoscopy. 2011;43 Suppl 2 UCTN:E217-E218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Morris-Stiff G, Falk GA, El-Hayek K, Vargo J, Bronner M, Vogt DP. Jejunal cavernous lymphangioma. BMJ Case Rep. 2011;2011:bcr0320114022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Huang Q, Minor MA, Weber HC. Clinical challenges and images in GI. Diagnosis: Cavernous lymphangioma of the jejunum. Gastroenterology. 2009;136:1170, 1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Hsu SJ, Chang YT, Chang MC, Yu SC, Lee JC, Shun CT, Wong JM. Bleeding jejunal lymphangioma diagnosed by double-balloon enteroscopy. Endoscopy. 2007;39 Suppl 1:E5-E6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Griffa B, Basilico V, Feltri M, Griffa A. [Submucosal jejunal lymphangioma: an unusual case with obscure gastrointestinal bleeding in an adult, detected by video-capsule endoscopy and treated by laparoscopy]. Minerva Chir. 2006;61:529-532. [PubMed] |
| 18. | Honda K, Ihara E, Ochiai T, Matsumoto M, Matsuda H, Nakashima A, Harada N, Kabemura T. Lymphangioma of small intestine. Gastrointest Endosc. 2003;58:574-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Ishikawa N, Fuchigami T, Tabata H, Kobayashi H, Sakai Y, Iizuka Y, Satou S, Nagae T, Kikuchi Y, Osamura S, Nakashima J, Yoshinaga H, Ishikawa T, Nakanishi M. [A case of lymphangioma of the small intestine]. Nihon Shokakibyo Gakkai Zasshi. 1999;96:959-963. [PubMed] |
| 20. | Barquist ES, Apple SK, Jensen DM, Ashley SW. Jejunal lymphangioma. An unusual cause of chronic gastrointestinal bleeding. Dig Dis Sci. 1997;42:1179-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Hanagiri T, Baba M, Shimabukuro T, Hashimoto M, Takemoto H, Inoue A, Sugitani A, Shirakusa T. Lymphangioma in the small intestine: report of a case and review of the Japanese literature. Surg Today. 1992;22:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Colizza S, Tiso B, Bracci F, Cudemo RG, Bigotti A, Crisci E. Cystic lymphangioma of stomach and jejunum: report of one case. J Surg Oncol. 1981;17:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Ralston M. Lymphangioma-haemangioma of the jejunum: a rare cause of alimentary tract bleeding. Aust N Z J Surg. 1961;30:209-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Amadori G, Micciolo R, Poletti A. A case of intra-abdominal multiple lymphangiomas in an adult in whom the immunological evaluation supported the diagnosis. Eur J Gastroenterol Hepatol. 1999;11:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Zhu H, Wu ZY, Lin XZ, Shi B, Upadhyaya M, Chen K. Gastrointestinal tract lymphangiomas: findings at CT and endoscopic imaging with histopathologic correlation. Abdom Imaging. 2008;33:662-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Lawless ME, Lloyd KA, Swanson PE, Upton MP, Yeh MM. Lymphangiomatous Lesions of the Gastrointestinal Tract: A Clinicopathologic Study and Comparison Between Adults and Children. Am J Clin Pathol. 2015;144:563-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |