Published online Jan 6, 2020. doi: 10.12998/wjcc.v8.i1.110
Peer-review started: September 25, 2019
First decision: November 11, 2019
Revised: November 18, 2019
Accepted: November 27, 2019
Article in press: November 27, 2019
Published online: January 6, 2020
Processing time: 103 Days and 16.1 Hours
Widening of the pubic joint of more than 10 mm is diagnostic and defined as pubic symphysis diastasis and is considered a complication of vaginal childbirth or pregnancy. As it is a rare pathology (ranging from 1 in 300 to 1 in 30000 pregnancies), no gold standard treatment has been defined.
This study examines two cases, a 27-year-old woman (gravida 1, para 1) and a 32-year-old woman (gravida 2, para 2), who presented to the clinic after uneventful vaginal deliveries. A normal pregnancy with no complications was observed in both patients. Severe pain in the pubic region occurred after labour and was accompanied by complicated locomotion. Pubic symphysis diastasis was confirmed radiologically and bed rest with lateral decubitus positioning was recommended. Oral non-steroidal antiinflammatory drugs were administered to relieve pain exacerbations. The symptoms decreased after treatment. Post-treatment magnetic resonance imaging (MRI) in the first case showed a reduction in symphyseal separation with no signs of osteitis. Three years later the symptoms recurred; MRI examination showed no further symphyseal widening or signs of osteitis. A relapse of symphyseal separation was diagnosed and conservative treatment was re-administered resulting in successful recovery. In the second case, pain recurred when the patient conceived for the second time. This time no benefit following conservative treatment was observed. Persistent pain and complicated locomotion led to scoliotic deformation of the lumbar part of the spine and leg length discrepancy, thus surgical treatment was chosen and internal pubic synthesis was performed.
Overall, surgical treatment resulting from insufficient conservative treatment showed a high risk of postoperative complications following the treatment of postpartum pubic symphysis diastasis.
Core tip: Widening of the pubic joint of more than 10 mm is diagnostic and defined as pubic symphysis diastasis and is considered a complication of vaginal childbirth or pregnancy. As it is a rare pathology and no gold standard treatment is defined, we present two cases with severe pain in the pubic region after labour, accompanied by complicated locomotion. Pubic symphysis diastasis was confirmed radiologically in both cases and conservative treatment was recommended. No benefit following conservative treatment was observed, thus surgical treatment was selected and internal pubic synthesis was performed. These cases show that standardisation of conservative and surgical treatment or studies of possible complications have not been defined; therefore, postoperative infections are likely to complicate surgical treatment. Overall, our findings demonstrate the significance of an accurate choice between conservative and surgical treatment due to possible complications after surgical intervention such as infection, loose screws, fistula and repeated surgical management.
- Citation: Norvilaite K, Kezeviciute M, Ramasauskaite D, Arlauskiene A, Bartkeviciene D, Uvarovas V. Postpartum pubic symphysis diastasis-conservative and surgical treatment methods, incidence of complications: Two case reports and a review of the literature. World J Clin Cases 2020; 8(1): 110-119
- URL: https://www.wjgnet.com/2307-8960/full/v8/i1/110.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i1.110
The pubic symphysis is a non-synovial joint that connects the right and left superior pubic rami with a normal radiographic separation width of 4 to 5 mm. Due to hormone-related changes and physiological alterations observed during pregnancy, the gap can increase by 2-3 mm and remain after delivery, such a separation is called physiological pubic symphysis diastasis. Infrequently vaginal delivery might lead to joint widening of > 10 mm which is diagnostic and defined as pathological pubic symphysis diastasis[1]. A physiological widening of the symphysis joint is based on normal endocrine changes during pregnancy; therefore, it does not depend on the mode of delivery, and the pathological diastasis is considered a complication of the vaginal method of childbirth and can be prevented by Cesarean delivery[2]. A separation larger than 25 mm involves damage of ligaments linked to the pubic bones; thus, pubic rupture can be determined[3]. This is a rare pathology found in postpartum women with an estimated prevalence ranging from 1 in 300 to 1 in 30000 pregnancies[4]. Possible predisposing factors involve the number of previous pregnancies, fetal macrosomia, narrow pelvic outlet or cephalo-pelvic disproportion, rapid and dense contractions during labour, epidural route of anaesthesia, previous trauma in the pelvic region, osteomalacia, chondromalacia, and infections[5,6]. Pubic symphysis diastasis can be symptomatic or asymptomatic. Although the exact number of women with an asymptomatic condition is unclear, literature reports show that postpartum patients with asymptomatic separation are at a higher risk of developing symptoms after secondary trauma or weight stress[7]. The leading symptom of symphyseal separation is pubic joint pain and inflammation. Pain can radiate to the abdominal or inguinal area, to lower extremities or to the back. The symptoms tend to worsen while moving, bearing a load, or raising a leg. Sometimes it may contribute to symphyseal or lower back discomfort or be followed by complicated locomotion leading to instability and incapacity while walking or standing[1]. Less common manifestations are urinary dysfunction and increased and/or uneven movement of the pelvic joints[8]. There are various non-operative and operative treatment options, but no gold standard treatment has been defined. The aim of this study was to review currently available approaches underlining pubic symphysis diastasis treatment indications, their effectiveness and complications. Two clinical cases of postpartum pubic symphysis diastasis are presented, and their postoperative conservative treatment, complications and outcomes are described.
Case 1: A 28-year-old patient (gravida 1, para 1) presented to the clinic 3 mo postpartum after an uneventful vaginal delivery with the complaint of a sharp, extremely intense pain in the pubic region.
Case 2: A 32-year-old woman (gravida 2, para 2) developed acute-onset anterior pubic pain during delivery. This anterior pubic pain radiated to the left buttock and thigh. The pain persisted postpartum and was exacerbated by any movement. Moreover, pain in the sacroiliac region contributed to the condition.
Case 1: The patient had a normal pregnancy until the last trimester when she started to complain of pain in the pubic region. She had an uneventful vaginal delivery of healthy twins. The pain increased after labour and became unbearable. Clinical and imaging examinations confirmed pubic symphysis diastasis with secondary pubic osteitis. Conservative treatment was administered for persistent pubic pain. The condition improved. Unfortunately, the pain recurred 3 mo later. The patient started to complain of severe pain accompanied by complicated locomotion. Progression of symphysial separation with expanded signs of osteitis and displacement of pubic bones were detected radiographically. Taking into account that the symptoms recurred after conservative treatment, surgical treatment was selected. Internal pubic synthesis under spinal anesthesia was performed. The pubic symphysis was reached layer by layer through a Pfannenstiel incision. Surgery revealed vertical and horizontal instability of the pelvis and the presence of 0.5 mm inflammatory fluid in the pubic symphysis. Debridement and repositioning were performed and a 6-hole plate and 6 screws were used for fixation of the superior symphysis diastasis. After the operation, the patient was allowed partial weight-bearing with the assistance of crutches for 3 mo. The postoperative period was without complications. However, several months later, a fistula appeared in the scar location. Diagnostic examination showed no pelvic instability or disruption of the inserted plate. Antibacterial therapy was administered and the fistula healed. However, the positive outcome was only temporary as the fistula recurred several times, causing severe aches in the region of the pubic joint. X-ray showed four loose screws, thus removal of the fixation plate was performed. The patient recovered well and one year later had no complaints. Furthermore, no radiological signs of skeletal instability or infection were detected.
Case 2: The patient with an uncomplicated prenatal course developed acute-onset anterior pubic pain during her first and otherwise normal delivery. This anterior pubic pain radiated to the left buttock and thigh. The pain persisted postpartum and was exacerbated by any movement. Radiographs confirmed pubic symphysis diastasis and conservative treatment was administered. The effect was only short-term and there were several periods of exacerbations of symptoms. When the patient conceived for the second time, acute-onset anterior pubic pain recurred and was accompanied by pain in the sacroiliac region. Symphysis diastasis and secondary pubic osteitis were confirmed, but this time no benefit following conservative treatment was observed. Persistent pain and complicated locomotion led to scoliotic deformation of the lumbar part of the spine and leg length discrepancy.
Case 1: The patient had no previous history of any major illness or any surgical interventions in the past.
Case 2: The patient had no previous history of any major medical illness or any surgical interventions in the past.
Case 1: No allergies, harmful habits or medicines taken were recorded.
Case 2: No allergies or harmful habits were recorded. The patient was taking vitamin D supplements.
Case 1: Clinical examination demonstrated painful palpation of the pubic region. Furthermore, pubic pain was provoked by pressure applied to the iliac crests in the antero-posterior and medial directions. There was no neurological pathology.
Case 2: Palpation of the anterior surface of the symphysis pubis elicited pain. Positive Trendelenburg’s sign was observed. Active straight leg raising was limited because of yielding pain. Bilateral trochanteric compression also induced pain.
Case 1: Leukocytosis (11 × 109/L) was detected during the first visit, which resolved during conservative treatment and was recorded again when the pain recurred. Neutrophilic leukocytosis (15 × 109/L) and elevation of C reactive protein (350 mg/L) were documented when the fistula occurred in the scar location. No other significant abnormalities in laboratory examinations were observed.
Case 2: No significant abnormalities in laboratory examinations were observed.
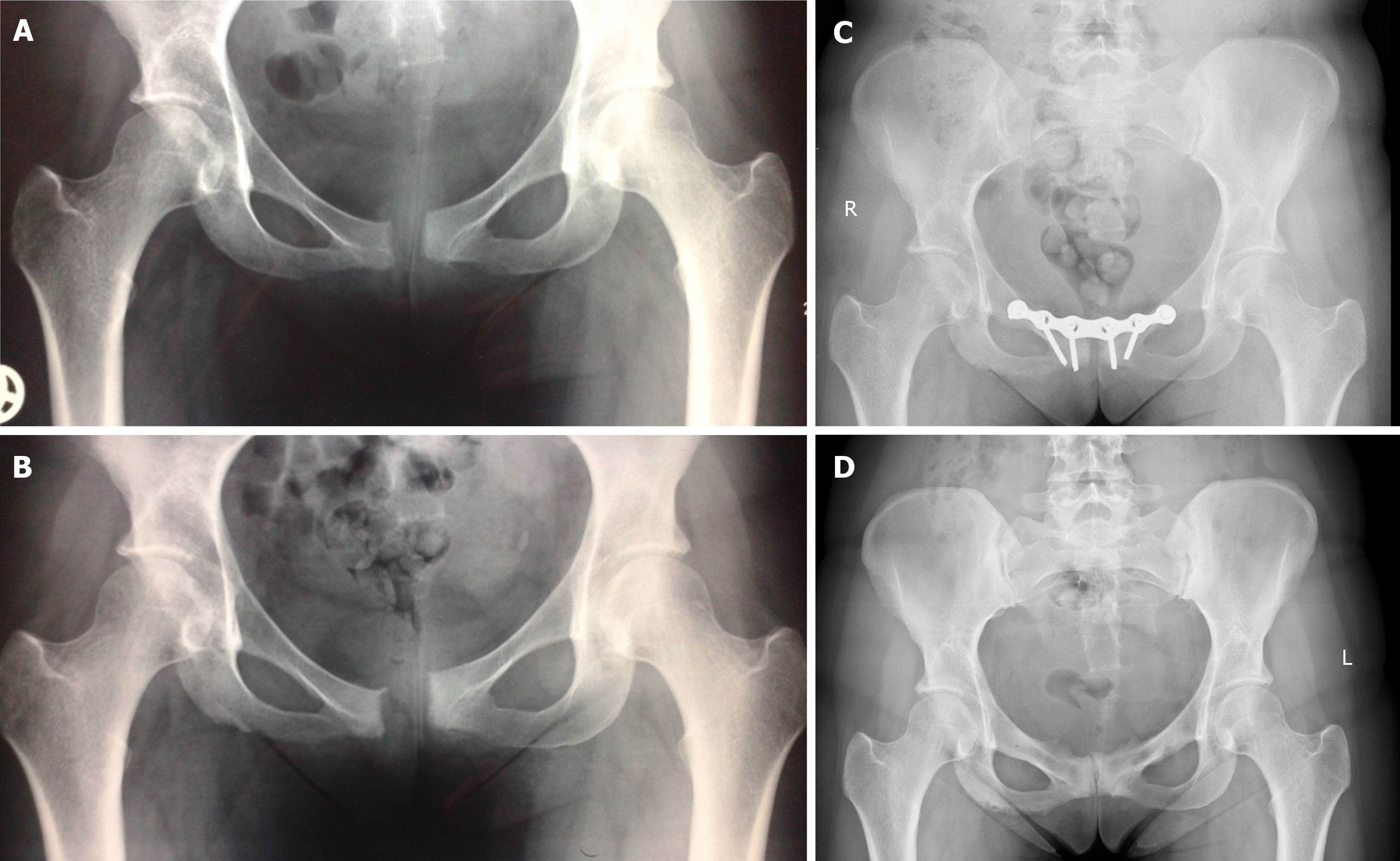
Case 1: On admission, pelvic X-ray showed a symphyseal gap of 1.5 cm with radiological characteristics of secondary pubic osteitis (Figure 1A). As the pain recurred 3 mo later, X-ray was repeated and a 2.5 cm symphysial separation with expanded signs of osteitis and displacement of pubic bones were detected (Figure 1B). After surgical treatment, the fistula in the scar location appeared several times; thus, X-ray was performed again and it showed four loose screws (Figure 1C). Removal of the fixation plate was performed and no radiological signs of skeletal instability or infection were detected (Figure 1D).
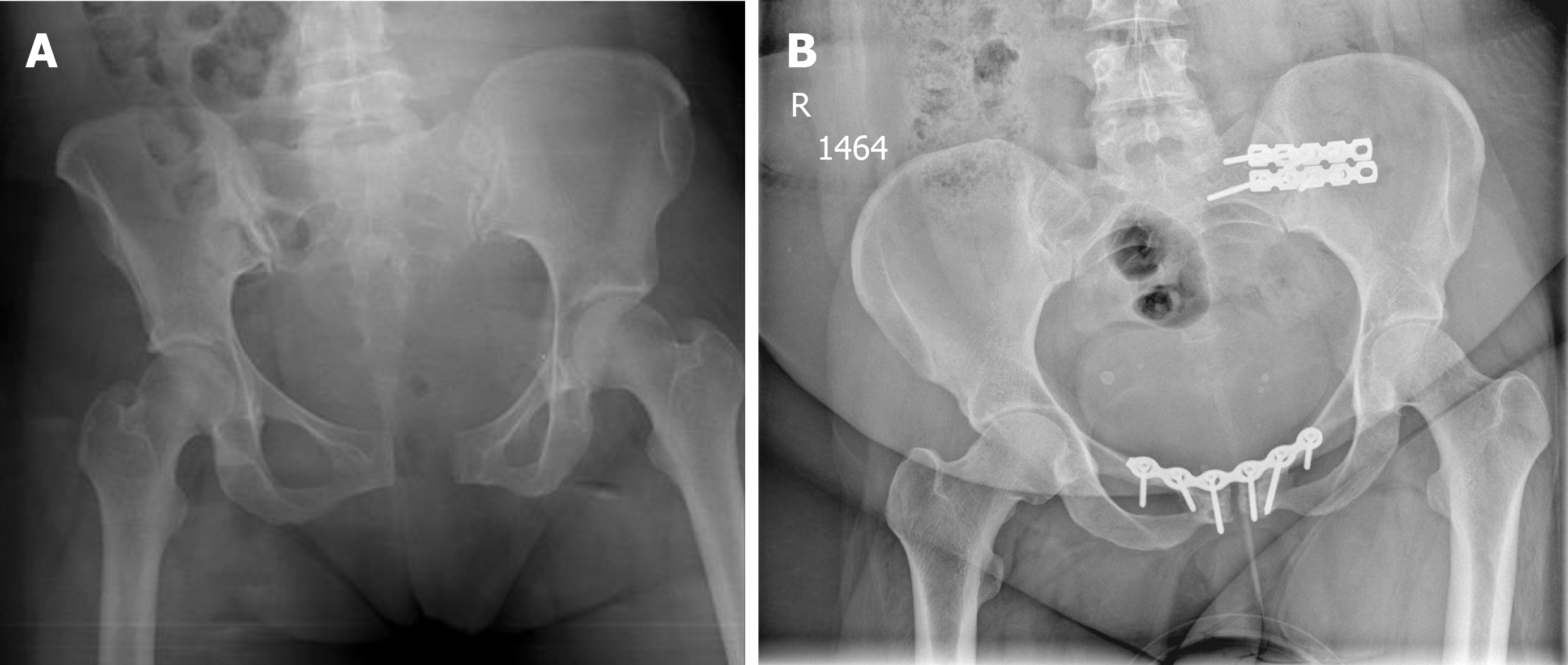
Case 2: On admission, radiographs confirmed pubic symphysis diastasis complicated by osteitis (Figure 2A). X-ray was repeated after repositioning and fixation of pubic symphysis diastasis with a plate and screws (Figure 2B).
Pubic symphysis diastasis and secondary pubic osteitis.
Oral non-steroidal antiinflammatory drugs (NSAIDs) and steroid injections into the symphysis pubis joint were administered for persistent pubic pain. Despite temporary improvement the symptoms recurred and surgical treatment was selected. Internal pubic synthesis under spinal anesthesia was performed. Pubic symphysis was reached layer by layer through a Pfannenstiel incision. Surgery revealed vertical and horizontal instability of the pelvis and the presence of 0.5 mm of inflammatory fluid in the pubic symphysis. Debridement and repositioning were performed and a 6-hole plate and 6 screws were used for fixation of the superior symphysis diastasis. After the operation, the patient was allowed partial weight-bearing with the assistance of crutches for 3 mo. The postoperative period was without complications. Several months later, a fistula appeared in the scar location and was successfully managed with antibacterial therapy. However, the positive outcome was only temporary as the fistula recurred several times and four loose screws were detected radiographically; thus, removal of the fixation plate was performed.
Following the occurrence of the first episode of pain, NSAIDs and acetaminophen were administered for pain management. However, analgesia was insufficient; thus, intrasymphyseal steroid injections in combination with local anaesthetics were administered. The effect was only short-term and there were several periods of exacerbations of symptoms. During the second pregnancy, the same medications were administered, but this time no benefit following conservative treatment was observed. Taking into account the complications (scoliotic deformation of the lumbar part of the spine and leg length discrepancy), surgery was indicated. The operation was performed in two stages, firstly, the left sacroiliac joint was fixed with a plate and screws, followed by the second stage of repositioning and fixation of pubic symphysis diastasis with a plate and screws.
The patient recovered well after surgery and one year later had no complaints. Furthermore, no radiological signs of skeletal instability or infection were detected.
Unfortunately, the symptoms remained after surgery. As the operative treatment was not effective, the pain was managed by analgesics, antidepressants and neuroleptics in combination with physiotherapy and pelvic binders. To correct leg length discrepancy, an insole was adjusted for the shorter leg.
Postpartum pubic symphysis separation is a clinical diagnosis based on clinical signs, of which the most common is pain in the symphyseal and sacroiliac joints, in some cases complicated locomotion or waddling gait is observed[1]. The literature mentions three clinical tests, highly ranked for their specificity and sensitivity, and used to evaluate symphysiolysis: tenderness in the particular joint area on palpation, positive Patrick’s (Faber) test, and positive Trendelenburg sign that showed the highest sensitivity[9]. Even though clinical assessment is sufficient to identify pubic symphysis diastasis[10], diagnostic imaging methods such as radiography, ultrasound, computed tomography and MRI are used for confirmation[11].
Prompt detection of the symptoms and establishment of the diagnosis are essential for early management strategies and may decelerate progression of the condition[1]. Although there are many treatment options varying from conservative to surgical methods, it is a rare pathology with insufficient evidence-based indications for each of them as well as a lack of studies highlighting the complications. A minimal widening of the symphyseal joint frequently has no clinical manifestations and requires no treatment at all[12]. Most symptomatic cases involve mild complaints and, as recommended in the literature, conservative treatment as an initial treatment option is sufficient. The selection between surgical or non-surgical strategies is significant as early operative treatment may not only have a faster beneficial effect on general health and pain reduction, but can also help to avoid incomplete healing or subsequent treatment difficulties[13].
In general practice, uncomplicated and mild cases are dealt with by conservative treatment. If conservative treatment fails or severe and/or complicated cases develop, surgery is performed. In general, uncomplicated cases and those with mild symptoms are more common. Many conservative methods are applied. Their efficiency has been discussed by many authors who are working on new non-interventional methods.
Conservative treatment is carried out to relieve pain and is usually combined with other methods to provide adequate analgesia. NSAIDs and acetaminophen as first-line analgesics for postpartum pain management are considered to be appropriate for pregnant and postpartum women and during lactation. Nevertheless, controversial results were observed in a meta-analysis, which reported similar effectiveness of Paracetamol and placebo in non-pregnant women[14,15].
NSAIDs therapy usually starts with ibuprofen ranging from 400 to 600 mg four times a day. Another option is naproxen varying from 250 to 500 mg twice a day. The doses can be adjusted per requirement and be reduced as tolerated[16].
In cases with a vicious cycle of pain accompanied by muscle spasms, lumbar epidural analgesia may be administered for 24 to 72 h, as several cases have reported good outcomes using epidural morphine, bupivacaine or fentanyl. A suggested dosage for lumbar epidural analgesia is bupivacaine 0.1% combined with 2 μg/mL of fentanyl for intermittent top-ups within 72 h[17].
There is research-based data of successful pain management with intrasymphyseal steroid injections in combination with local anaesthetics, particularly hydrocortisone, chymotrypsin and lidocaine[18]. Bonnin et al[19] suggested a protocol for local infiltration that consisted of 5 mL of lidocaine 1% and 40 mg of methylprednisolone. These authors presented a case report where infiltration with lidocaine alone was not as effective as lidocaine combined with methylprednisolone. An intracutaneous injection is inserted perpendicularly toward the pubic symphysis. When the needle reaches the fibroelastic cartilage it must be slightly withdrawn and the injection should be completed without resistance. Local infiltration is an easy and quick method with reported long-term effectiveness. Although this procedure demands the skills of an anaesthesiologist, the risk of developing an iatrogenic infection or an allergy to medications remains. Thus, these injections are contraindicated for patients with hypersensitivity to steroids or local anaesthetics[19]. In addition, external heat, ice or massage may aid in diminishing the symptoms. The administration of corresponding analgesia should be supported by bed rest, where the keystone is lateral decubitus positioning, or lying in a hammock is advised[1]. As an additional therapy, transcutaneous electrical nerve stimulation has also shown positive clinical outcomes[20]. There are several articles supporting the benefits of physiotherapy and acupuncture, as stabilising exercises show a significant improvement in functional status[21]. Physiotherapy focuses on strengthening muscles of the trunk and pelvis, and patients should learn how to avoid strain on the pelvis. These techniques combined with acupuncture are superior to traditional treatment alone and are recommended as an adjunct to standard treatment[22]. Nevertheless, effective pain management is necessary, as pain has a negative impact on patients’ psychological state. Taking into account that postpartum patients have a higher demand for emotional and social support, self-help group meetings are advantageous where helpful written information is available and practical solutions can be discussed between patients affected by the same problems[23].
In line with adequate analgesia, other techniques of conservative treatment are used to ensure effective healing. For example, pelvic ring integrity should be maintained and circular compression is necessary. To achieve this goal, supports or braces such as pelvic binders, belt braces or supportive pelvic/symphyseal belts are used. A brace or a girdle provides compression and stability to the sacroiliac joints and improves the disbursement of weight-bearing forces in the pelvis, back, hips and legs. Maintenance braces are beneficial for healing as they provide pelvic support in locomotion and reduce pain. A recent study on the effectiveness of pelvic binders applied multi-detector computed tomography and compared the treatment outcomes of diverse pelvic instability grades. The findings suggested that in globally unstable cases over-reduction of a binder may lead to overriding impacted symphysis[11,24]. Mulchandani and colleagues confirmed the efficiency of the pelvic binder in a review of four cases of conservative treatment with diastasis varying from 4 to 9.6 cm. A surgical waiver in those cases resulted in fast discharge postpartum and pain-free follow-up[8]. A novelty in this area is an elastic band device made from neoprene straps. It limits the contractility of the internal rotation muscles, movements of the pelvis and has proved to reduce the pathologic widening of the symphysial joint and minimise the pain syndrome. The elastic band is a European Conformity-certified medical device[25].
Conservative treatment consists of several different components and should be based on a multidisciplinary team approach.
Surgical treatment is rarely obligatory. Undoubtedly, an indication for operation is diastasis complicated by nerve compression, urogenital tract trauma or massive bleeding. Another indication is inefficient conservative treatment lasting from 1 to 1.5 mo; therefore, patients should be carefully followed-up after conservative treatment. Another indication is a large widening of the joint. A previous indication for surgery was a widening exceeding 2.5 cm[26], while recent studies suggest that conservative management has good outcomes and can be efficient in cases with wider separations. Therefore, surgery is now indicated only in cases where the diastasis is more than 4 cm[27]. On the other hand, anterior separation of the pubic symphysis of more than 2.5 cm causes progressive injury to the posterior pelvic ring, including disruption of the sacroiliac joint or sacral fracture, thus pain in the sacroiliac region might be indicative of further impairment[28].
An orthopaedic surgical correction in patients with a symphyseal gap over 4 cm was supported by the reduced duration of hospitalisation, a faster return to non-affected daily life, necessity for infant care, a shorter number of days in pain and no side effects on defecation[29]. The main surgical treatment methods are anterior cerclage wiring, anterior plating and external fixation[12]. The internal fixation procedure using a plate is reported to have fewer complications compared to fixations using only a wire or a screw alone. Therefore, this method is most commonly used in general practice. Some studies have compared the outcomes of using different types of plates[30], and in reduction of the diastasis, a two-hole plate technique is described as superior to a four-hole plate[31]. Beneficial outcomes of a complete symphysis disruption following internal fixation have been observed in acute, subacute and chronic cases[32].
Internal fixation is questionable in cases where organs of the reproductive system are damaged as it may increase the risk of infection in bones or soft tissues; therefore, in these cases external fixation should be considered as the method of choice[33].
On the other hand, surgical treatment with plate fixation is associated with frequently observed complications, the most common being contamination of the inserted pin or other infections, irritation of soft tissues, failure to fixate, loosening or replacement of screws, and recurrent widening that may require revision surgery[11,30]. One study retrospectively reviewed 148 patients treated with plate fixation and found that hardware breakage occurred in 43% of patients, although most were asymptomatic; therefore, the authors suggest that a high incidence of late fixation failure is clinically unimportant[34]. In this context, infectious complications are of primary concern, because any infection is more likely to have a severe course or lead to complications as immune insufficiency is observed during pregnancy and it was found that the Th1 axis and natural killer cytotoxicity suppression are also retained in the early postpartum. Complete immune recovery may take from 3 to 4 mo after delivery[35]. If posterior pelvic-arch instability is involved, open reduction and internal anterior-plate fixation of the pubic symphysis with posterior percutaneous screw fixation of the sacroiliac joints is a treatment option for simultaneous correction of symphyseal and sacroiliac joint instability[28].
Over the last 20 years, in many surgical specialties, the use of minimally invasive surgery has expanded widely as it is considered to be a safer and more effective technique to meet surgical needs than open surgery; therefore, laparoscopic techniques are increasingly used for this pathology. Considering that the main drawback of open surgery for a symphyseal diastasis is a high risk of infection, laparoscopic techniques may be beneficial due to smaller wounds and no need to remove the inserted plate. Moreover, a study demonstrating the repair of symphysis separation by Anchor and Suture Tape stabilisation also emphasises that such treatment has a reduced risk of hernia, decreased postoperative pain is observed and the absence of inserted rigid constructions such as plates or screws allows motion which is more physiological and more beneficial for healing. In the postoperative period, mobilisation with limitations of several activities for two weeks is promoted. However, despite the lack of studies on this method, several disadvantages have been demonstrated. Firstly, it demands a technically skilled general surgeon, and secondly, the operation might be unsuccessful and lead to sustained pain if the anchors are placed incorrectly or the suture is under-tensed[36]. Another minimally invasive technique is a pelvic bridge, a percutaneous method of subcutaneous fixation for the anterior pelvic ring, made through two incisions over each anterior iliac crest and one incision over the symphysis. A reconstruction plate or a spinal rod is placed through a subcutaneous tunnel overlying the external oblique fascia in the subcutaneous tissue, and fixation to the iliac crest and the pubis is achieved to ensure stability. This method is advantageous and includes fewer wound complications and less pain in the surgical site[37].
A rapid improvement in conservative and minimally invasive therapies suggests that surgical treatment is only necessary in very few cases. Surgery requiring open techniques is associated with a high rate of complications, especially infections; therefore, conservative therapy appears to be a better option in most pelvic symphysis diastasis cases. The possibility of persistent pain after surgery must be taken into account. Our clinical cases also support the opinion that the necessity of surgery should be strongly considered. In terms of surgical complications and improving the outcomes of non-interventional methods, some criticism may be referred to the indication for surgical treatment in cases of separation of less than 4 cm with the possibility of conservative treatment in even wider separations[8,27].
Pubic symphysis diastasis is a rare pathology mostly affecting postpartum women. A clear aetiology has not been defined, and only the predisposing factors are described in the literature. It can be symptomatic or asymptomatic. The main symptom is mild or severe pain which is managed by symptomatic or pathogenetic treatment. Taking into account that standardisation of conservative and surgical treatment or studies of possible complications were not found in the literature, we overviewed recent experiences and practical approaches as well as several new methods. After presenting our clinical cases of surgical treatment resulting from insufficient conservative treatment, we revealed a high risk of postoperative infections that are likely to trigger complications in treating postpartum symphysis pubis diastasis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Lithuania
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gao BL S-Editor: Zhang L L-Editor: Webster JR E-Editor: Liu MY
| 1. | Jain S, Eedarapalli P, Jamjute P, Sawdy R. Symphysis pubis dysfunction: a practical approach to management. Obstetrician Gynaecologist. 2006;8:153-158. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Heim J, Vang S, Thomas A, Ly T, Das K. Effect of Pregnancy, Labor, Delivery and Postpartum on Physiological Pubic Symphysis Diastasis [23I]. Obstet Gynecol. 2016;127:79S. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Nitsche JF, Howell T. Peripartum pubic symphysis separation: a case report and review of the literature. Obstet Gynecol Surv. 2011;66:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Parker JM, Bhattacharjee M. Images in clinical medicine. Peripartum diastasis of the symphysis pubis. N Engl J Med. 2009;361:1886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Kubitz RL, Goodlin RC. Symptomatic separation of the pubic symphysis. South Med J. 1986;79:578-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Yoo JJ, Ha YC, Lee YK, Hong JS, Kang BJ, Koo KH. Incidence and risk factors of symptomatic peripartum diastasis of pubic symphysis. J Korean Med Sci. 2014;29:281-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Bombaci H. Outcome of Internal Fixation and Corticocancellous Grafting of Symphysis Pubis Diastasis Which Developed after Malunion of Pubic Rami Fracture. Hip Pelvis. 2017;29:150-153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Mulchandani NB, Jauregui JJ, Abraham R, Seger E, Illica E. Post-partum management of severe pubic diastasis. Clin Exp Obstet Gynecol. 2017;44:464-466. [PubMed] |
| 9. | Albert H, Godskesen M, Westergaard J. Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. Eur Spine J. 2000;9:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 121] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Wellock VK. The ever widening gap-symphysis pubis dysfunction. Br J Midwifery. 2013;10:6. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Herren C, Sobottke R, Dadgar A, Ringe MJ, Graf M, Keller K, Eysel P, Mallmann P, Siewe J. Peripartum pubic symphysis separation--Current strategies in diagnosis and therapy and presentation of two cases. Injury. 2015;46:1074-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Hou Z, Riehl JT, Smith WR, Strohecker KA, Maloney PJ. Severe postpartum disruption of the pelvic ring: report of two cases and review of the literature. Patient Saf Surg. 2011;5:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Nayak SP, Panda CK. Comparison between conservative and surgical management in postpartum pubic symphysis diastasis: a randomized controlled trial. Int J Res Orthop. 2017;3:1211-7. [DOI] [Full Text] |
| 14. | Spigset O, Hägg S. Analgesics and breast-feeding: safety considerations. Paediatr Drugs. 2000;2:223-238. [PubMed] [DOI] [Full Text] |
| 15. | Saragiotto BT, Machado GC, Ferreira ML, Pinheiro MB, Shaheed CA, Maher CG. Paracetamol for low back pain. Cochrane Database Syst Rev. 2016;6:CD012230. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Knight CL, Deyo RA, Staiger TO, Wipf JE, Atlas SJ. Treatment of acute low back pain. Up To Date. Atlas SJ. Waltham, MA: Up To Date Inc 2017; Available from: https://www.uptodate.com/contents/treatment-of-acute-low-back-pain. |
| 17. | Scicluna JK, Alderson JD, Webster VJ, Whiting P. Epidural analgesia for acute symphysis pubis dysfunction in the second trimester. Int J Obstet Anesth. 2004;13:50-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Schwartz Z, Katz Z, Lancet M. Management of puerperal separation of the symphy-sis pubis. Int J Gynaecol Obstet. 1985;23:125-28. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Bonnin M, Bolandard F, Storme B, Sibaud F, Rabishong B. [Pelvic pain by acute symphysis pubis separation after vaginal delivery]. Ann Fr Anesth Reanim. 2006;25:644-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Ayeni GO, Oladire O, Jovita DA, Ethelbert OO, Chukwuemeka OC. Transcutaneous Electrical Nerve Stimulation (TENS) in the Management of Peripartum Diastasis Symphysis Pubis (DSP): Cases Report. Indian J Physiother Occup Ther. 2015;9. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Stuge B, Veierød MB, Laerum E, Vøllestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial. Spine (Phila Pa 1976). 2004;29:E197-E203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 128] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Elden H, Ladfors L, Olsen MF, Ostgaard HC, Hagberg H. Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. BMJ. 2005;330:761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 116] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 23. | Wainwright M, Fishburn S, Tudor-Williams N, Naoum H, Garner V. Symphysis pubis dysfunction: improving the service. Br J Midwifery. 2003;11:664-7. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Dreizin D, Bodanapally U, Mascarenhas D, O'Toole RV, Tirada N, Issa G, Nascone J. Quantitative MDCT assessment of binder effects after pelvic ring disruptions using segmented pelvic haematoma volumes and multiplanar caliper measurements. Eur Radiol. 2018;28:3953-3962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Lasbleiz J, Sevestre FX, Moquet PY. Using an Elastic Band Device After a Severe Obstetric Pubic Symphyseal Separation: Clinical and Imaging Evaluation. Obstet Gynecol. 2017;130:625-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 26. | Pauwels F. Beitrag zur Klarung der Beanspruchung des Beckens, insbesondere der Beckenfugen. In: Gesammelte Abhandlungen zur funktionellen Anatomie des Bewegungsapparates. Berlin: Springer 1965; 183-196. [DOI] [Full Text] |
| 27. | Kharrazi FD, Rodgers WB, Kennedy JG, Lhowe DW. Parturition-induced pelvic dislocation: a report of four cases. J Orthop Trauma. 1997;11:277-81; discussion 281-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Hierholzer C, Ali A, Toro-Arbelaez JB, Suk M, Helfet DL. Traumatic disruption of pubis symphysis with accompanying posterior pelvic injury after natural child-birth. Am J Orthop. 2007;36:E167-E170. |
| 29. | Dunivan GC, Hickman AM, Connolly A. Severe separation of the pubic symphysis and prompt orthopedic surgical intervention. Obstet Gynecol. 2009;114:473-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Park MS, Yoon SJ, Choi SM, Lee K. Is there a clinical benefit of additional tension band wiring in plate fixation of the symphysis? BMC Musculoskelet Disord. 2017;18:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Lange RH, Hansen ST. Pelvic ring disruptions with symphysis pubis diastasis. Indications, technique, and limitations of anterior internal fixation. Clin Orthop Relat Res. 1985;201:130-137. [RCA] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Najibi S, Tannast M, Klenck RE, Matta JM. Internal fixation of symphyseal disruption resulting from childbirth. J Orthop Trauma. 2010;24:732-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Chang JL, Wu V. External fixation of pubic symphysis diastasis from postpartum trauma. Orthopedics. 2008;31:493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 34. | Morris SA, Loveridge J, Smart DK, Ward AJ, Chesser TJ. Is fixation failure after plate fixation of the symphysis pubis clinically important? Clin Orthop Relat Res. 2012;470:2154-2160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 35. | Groer ME, Jevitt C, Ji M. Immune changes and dysphoric moods across the postpartum. Am J Reprod Immunol. 2015;73:193-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 36. | Arner JW, Albers M, Zuckerbraun BS, Mauro CS. Laparoscopic Treatment of Pubic Symphysis Instability With Anchors and Tape Suture. Arthrosc Tech. 2018;7:e23-e27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 37. | Hiesterman TG, Hill BW, Cole PA. Surgical technique: a percutaneous method of subcutaneous fixation for the anterior pelvic ring: the pelvic bridge. Clin Orthop Relat Res. 2012;470:2116-2123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |