Published online Apr 6, 2019. doi: 10.12998/wjcc.v7.i7.863
Peer-review started: November 22, 2018
First decision: January 19, 2019
Revised: January 29, 2019
Accepted: February 26, 2019
Article in press: February 26, 2019
Published online: April 6, 2019
Processing time: 135 Days and 0 Hours
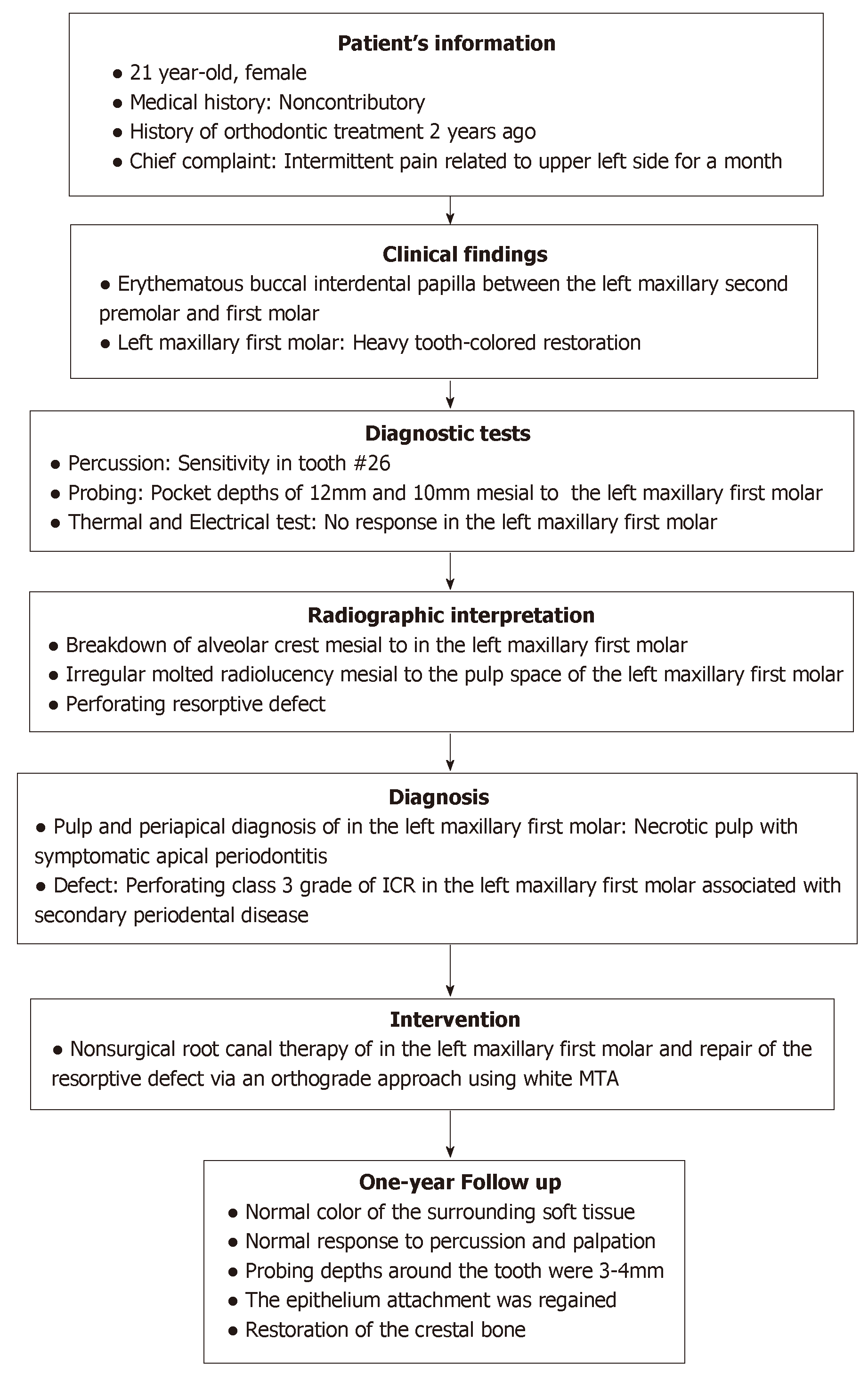
Invasive cervical resorption (ICR), a commonly misdiagnosed condition, is an aggressive form of external tooth resorption that contributes to periodontal tissue inflammation and deepening of the periodontal pockets. Herein we report the case of a patient, exhibiting ICR and elaborate the effects of a non-surgical approach in the amelioration of this condition.
A 21-year-old female reporting intermittent pain at the upper left side, multiple restorations, no trauma history, and having received orthodontic treatment was studied. Localized erythematous swelling was noted at the buccal interdental papilla between the left maxillary first molar and second premolar. The diseased pulp and tissue in resorption were removed and the root canal system including the defect were sealed using gutta percha/AH Plus and mineral trioxide aggregate (MTA). At the one-year recall, the tooth showed no symptoms and responded normally to percussion and palpation. The surrounding periodontium exhibited a normal color and the probing depth was normal. Radiographic examination showed a restoration of crestal alveolar bone and good adaption to MTA.
Non-surgical root canal treatment in conjunction with resorption defect orthograde repair with MTA was found to be an effective treatment option in the elimination of ICR. Early diagnoses are recommended in order to employ non-surgical approaches for management of ICR instead of surgical interventions.
Core tip: Invasive cervical resorption (ICR) denotes a particularly aggressive form of external tooth resorption that progressively destroys the tooth structure within the dentition. The outcome of the present case demonstrates the significance of early diagnoses of ICR; so that non-surgical approaches may be utilized instead of surgical interventions. This case study has explored the efficacy of non-invasive non-surgical approaches to treat ICR.
- Citation: Alqedairi A. Non-Invasive management of invasive cervical resorption associated with periodontal pocket: A case report. World J Clin Cases 2019; 7(7): 863-871
- URL: https://www.wjgnet.com/2307-8960/full/v7/i7/863.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i7.863
Invasive cervical resorption (ICR) denotes a particularly aggressive form of external tooth resorption that progressively destroys the tooth structure within the dentition[1,2]. This clinical condition serves the purpose of progressively destroying the tooth structure within the dentition. It is notable due to its position with regards to the cervical region of the tooth and its invasive properties and can be visualized as a pinkish color in the crown of the tooth[2]. This color occurs due to coronal dentin and enamel resorption, due to which the intensely vascular resorptive tissue can be visualized through the residual enamel[3]. A clinical classification of ICR has been proposed by Heithersay based on the extension of dentin destruction[2]. Class 1 demonstrates a small invasive resorption near the cervical area with shallow penetration into dentin. Class 2 demonstrates a well-defined, close to the coronal portion of the pulp cavity with little or no extension to the root dentin. Class 3 represents a deeper invasion of dentine by resorbtive defect and extending into the coronal third of the root. Class 4 corresponds to a large invasive resorption extending beyond the coronal third of the root[2].
Numerous complications surround the effective and accurate diagnosis of ICR primarily due to its consistent misinterpretation as a form of internal resorption[3]. Research indicates a lack of clarity surrounding the etiology of this condition. Moreover, various factors may predispose an individual to ICR. Literature noted that the primary contributing factor was intra-coronal bleaching, followed by orthodontics, trauma and other dentoalveolar surgery periodontal treatments[4].
ICR affects the periodontal tissues within the dentition and this clinical condition is considered as one of the primary factors due to which periodontal tissue in-flammation may arise[5]. However, ICR does not have any pulpal interaction, since the pulp is shielded by a predentin layer. Studies indicate the role of bacterial involvement in the gingival sulcus in sustaining the inflammation within the periodontal tissues[6-8]. Moreover, the occurrence of ICR was found to be extremely prevalent below the tooth’s epithelial attachment. Therefore, it is of great significance to take into consideration the fact that the location of ICR is not always cervical. This is because, the location is associated with the level of marginal tissues and the depth of the periodontal pockets[9]. It is critical that resorption be terminated via the utilization of suitable dental treatment. The present case study discusses the utilization of non-surgical root canal treatment in conjunction with mineral trioxide aggregate (MTA) to form the treatment of a patient with ICR associated with Periodontal Pocket.
A 21-year-old female patient presented to endodontic clinic at the University Dental Hospital at King Saud Dental University with the chief complaint of intermittent spontaneous pain related to upper left side.
Patient has recently noticed a small localized swelling between teeth in the maxillary left posterior region. The pain started at the same area a month ago. Patient reported no sensitivity to cold or heat stimulation.
The patient reported no history of trauma. However, she had received orthodontic treatment 2 years ago. The patient had multiple restorations mostly carried out by a pedodontist one year prior to her admittance at this hospital.
Patient medical history was noted to be noncontributory.
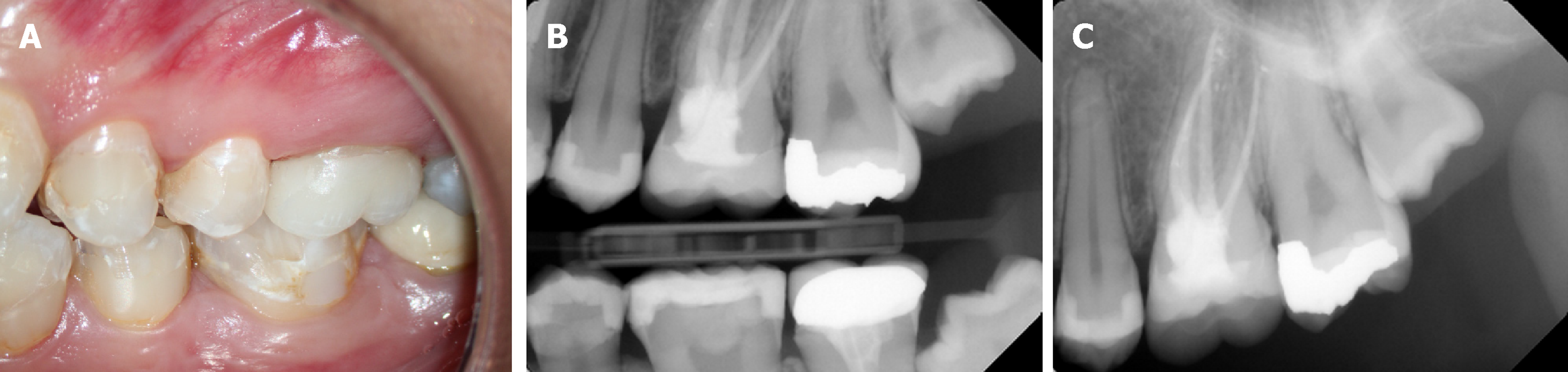
Clinical examination revealed the presence of localized erythematous swelling at the buccal interdental papilla between the left maxillary first molar and second premolars (Figure 1A and B).
It was noted that the left maxillary second premolar and first molar had MOD tooth-colored restorations. Meanwhile, the left maxillary second molar had MO amalgam restorations. The teeth were tested electrically and thermally. It was found that left maxillary first molar was not responsive to the thermal or electric pulp tests; whereas, the other tested teeth responded normally. Moreover, it was noted that this tooth was sensitive to percussion and tender to palpation. On probing, a respective pocket depth of 12 mm and 10 mm was detected in the mesiobuccal and mesiolingual regions of left maxillary first molar (Figure 1C and D).
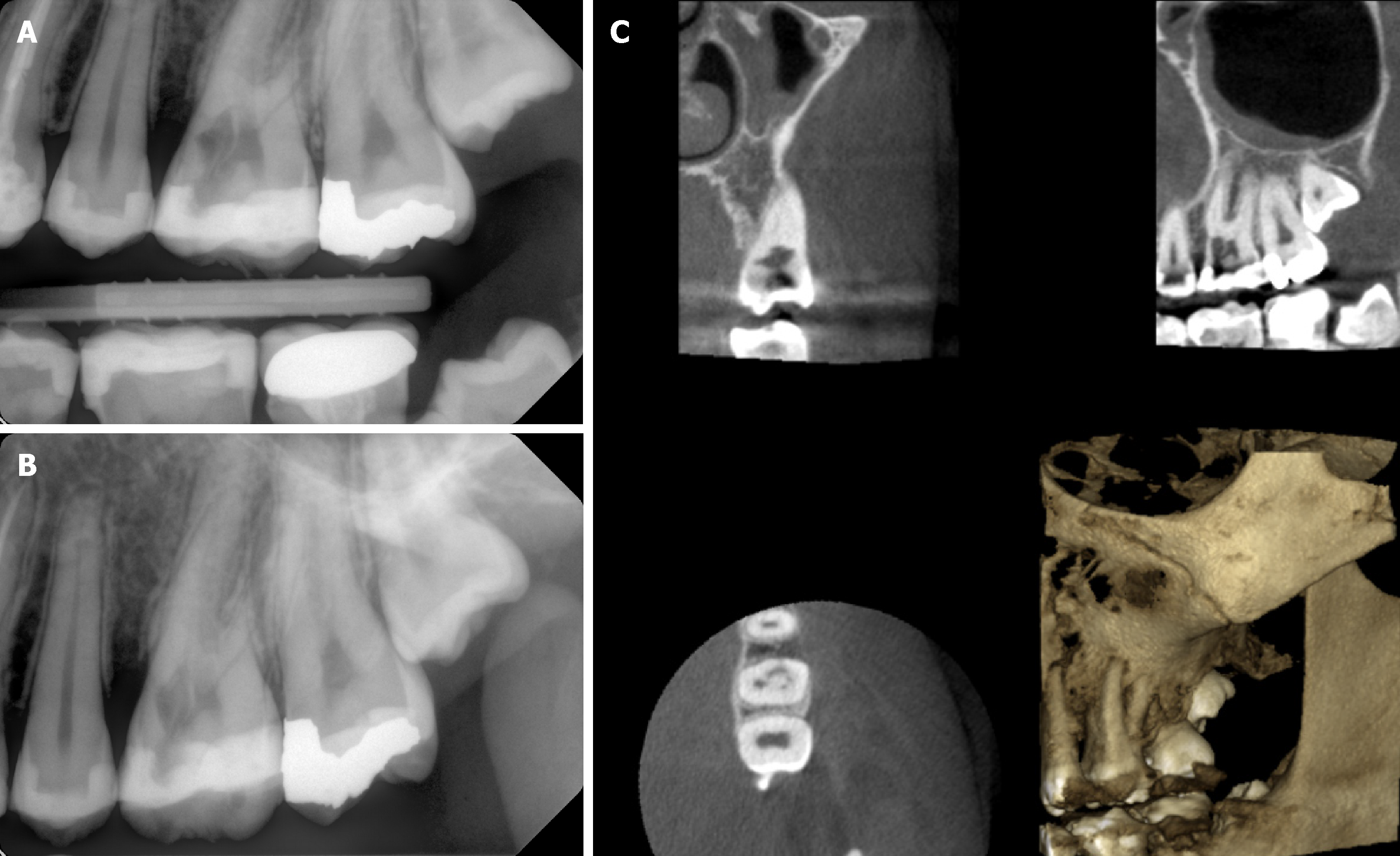
A two-dimensional radiographic examination was conducted that revealed the presence of a breakdown of the crest of alveolar bone mesial to left maxillary first molar and an irregular molted radiolucency mesial to the pulp space of left maxillary first molar but separated by radiopaque line, and extending into the radicular dentin (Figure 2A and B). Cone-beam computed tomography examination confirmed the size and the external perforation of the existing resorption defect (Figure 2C).
Based on the clinical and radiographic findings, the left maxillary first molar was diagnosed as necrotic pulp with symptomatic apical periodontitis. Furthermore, the resorptive lesion was diagnosed as a perforating class 3 grade of ICR that was associated with secondary periodental disease.
A treatment plan was presented to the patient that was inclusive of nonsurgical root canal therapy and the repair of the resorptive defect via an orthograde approach using white MTA. A questionable prognosis was considered due to the extension and location of the resorptive defect. Consent was obtained from the patient. The first treatment session incorporated the administration of local infiltration anesthesia and tooth isolation via rubber dam. Upon access cavity preparation, excessive bleeding was noted at the anticipated location of resorption defect. The defect was temporarily sealed with Oraseal (Ultradent Products Inc., South Jordan, Utah the United States) and complete access was performed. Mesiobuccal, distobuccal and palatal canals were located and negotiated to the full length, and their patency was established using a size 10 k-file (Dentsply/Maillefer, Ballaigues, Switzerland).
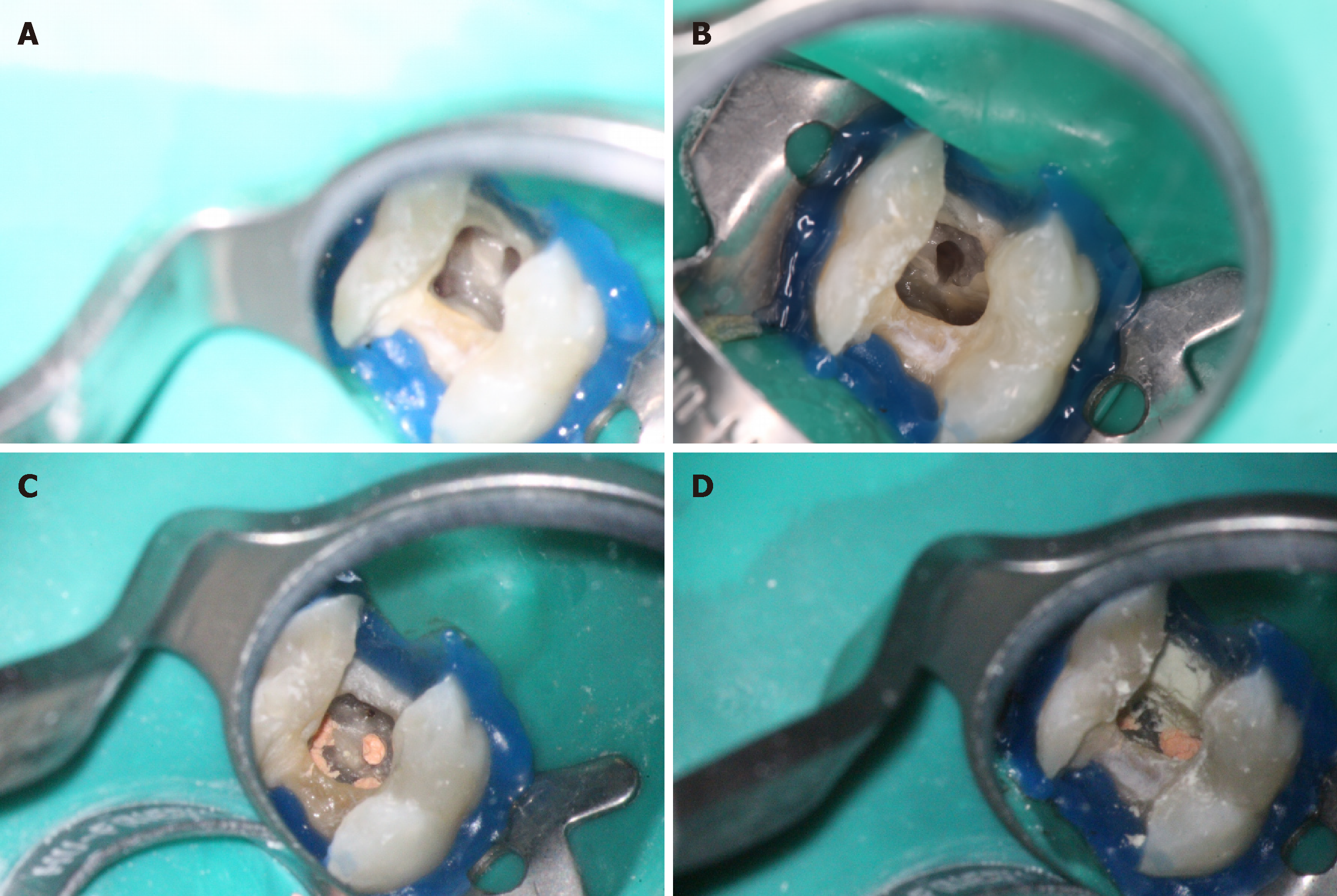
Following this, a chemo-mechanical preparation using a profile rotary system (Maillefer, Ballaigues, Switzerland) was carried out. Mesiobuccal and distobuccal canals were prepared to size 35/04, while the palatal canal was prepared to di-mensions of 40/06. The preparation of the canals was consistently carried out under irrigation using 5.25% sodium-hypochlorite solution. Subsequently, the resorption defect was exposed and the granulomatous tissue was removed using a spoon excavator instrument and a size 2 round carbide bur (Komet Dental, Lemgo, Germany). Two small perforations and the second mesiobuccal canal were located at the base of the resorptive defect. It is to be noted that the visibility was compromised due to the excessive bleeding. Therefore, the root canal system and the resorption defect were dressed with calcium hydroxide (Ultradent Products Inc., South Jordan, Utah the United States) and the tooth was then provisionally restored using cotton and cavit (coltene, Alstatten, Switzerland). One week later, the patient presented to the clinic and was found to be asymptomatic. The tooth was reopened and calcium hydroxide was removed. The bleeding due to the resorption defect was controlled and better visibility was achieved (Figure 3A and B). The second mesiobuccal canal was negotiated and prepared to size 30/04. The mesiobuccal root demonstrated type II root canal configuration according to the Vertucci classifications[10].
The canals were later irrigated using 17% EDTA (SybronEndo, Orange, Ca). Furthermore, 5.25% NaOCL was used as final rinse for the canals. Obturation of the root canal system was performed using the continuous wave of vertical condensation technique through the use of gutta percha and AH26 (Dentsply, Konstanz, Germany) (Figure 3C). The resorption defect and the two mesiobuccal canals orifices were sealed with white MTA (Dentsply/Maillefer, Ballagiues, Switzerland) (Figure 3D). The tooth was then provisionally restored with wet cotton and cavit. The postoperative radiograph revealed that there was adequate MTA filling of the perforation and resorption defect (Figure 4). One week later, the tooth was reopened, the setting of MTA was confirmed and the tooth was restored with bonded restoration using a multicore medium (Ivoclar Vivadent, Schaan, Liechtensien). Subsequently, the tooth was prepared and an impression was taken for the coronal overlay.
Two weeks later, clinical examination revealed the presence of normal color in the surrounding soft tissue and a normal response to percussion and palpation. Probing depths around the tooth were within normal limits (3-4 mm) and the epithelium attachment was regained. At the one-year recall, the tooth showed no symptoms and responded normally to percussion and palpation. It was noted that the surrounding periodontium exhibited a normal color and the probing depth was likewise noted to be normal. The radiographic examination showed a restoration of the crestal alveolar bone and good adaption to the MTA (Figure 5). Figure 6 represents the timeline from the patient’s presentation to the final outcome.
The case study has explored the efficacy of non-surgical approaches to treat ICR. A patient reporting intermittent pain at the upper left side, no history of trauma, with multiple restorations and having received orthodontic treatment previously was studied. It was noted that orthodontic treatment and restorations were the pre-disposing factors that heavily contribute to the development of ICR[4]. A non-surgical approach in the form of root canal treatment and orthograde repair via MTA was utilized to effectively manage ICR in the patient.
In the recent years, studies have highlighted the efficacy of non-surgical approaches in the effective management of ICR, associated with the periodontal tissues. It was noted that such non-surgical approaches combine root canal treatment with orthograde repair of the region, where there is the presence of resorptive defect[11]. Such studies conducted a removal of diseased tissue and orthograde repair via the use of materials; such as MTA, as in the present case study. Studies reported that this material demonstrated good sealing ability that can serve as repair material for perforations[12,13], and has excellent biocompatibility[7].
The use of MTA with regard to orthograde repair and as an obturation material was noted to be extremely advantageous in studies that discussed its applications as a hermetic seal in root end filling[9]. More recently, new bioceramic formulations, such as Biodentin, EndoSequence® BC Sealer™, Root Repair Material (RRM™), and Fast Set Putty (Brasseler the United States®), have been introduced as an alternative to MTA, due to their better physical, chemical, and biological properties, and to overcome the drawbacks associated with the use of MTA like handling properties, long setting time and tooth discoloration[14-17]. This study additionally incorporated the use of EDTA and NaOCl to irrigate and rinse the canals. This use of EDTA and NaOCl was further noted in additional studies that have conducted reviews of non-surgical management of ICR[10].
As discussed earlier, the results depicted that the use of non-surgical treatment aided in the normalization of response to percussion and palpation, as well as the normalization of color in the surrounding soft tissue. It was further seen that the probing depths around the tooth were normal, and the epithelial attachment was recovered. The normal color and response to percussion and palpation was further noted at the one-year recall. Furthermore, the probing depth was noted to be within the normal limits, and the surrounding periodontum was seen to be normal in color. This normal probing depth after non-surgical management via MTA was noted in other studies that conducted a 1-year follow up after the treatment[6]. Additionally, the radiographic examination depicted restoration of crestal alveolar bone and good adaption to MTA (Figure 5). The use of radiographic analysis to assess the level of ICR was highlighted by Heithersay. This restoration of the crestal bone was further noted in additional studies that conducted examinations of the effective management of ICR[8].
ICR is an uncommon type of tooth resorption that is commonly misdiagnosed as a form of internal resorption. This condition may further impact the periodontal tissues that result in the development of deep periodontal pockets. Non-surgical management of ICR was discussed in various studies as an effective way of managing this condition. This study made use of root canal treatment and orthograde repair via MTA to manage ICR. At two weeks and one-year follow-ups, normalcy with respect to color, probing depth, response to percussion, and palpation was recovered. Furthermore, the crystal alveolar bone structure was also restored. These results are in support of the effective role of non-surgical approaches in the management of ICR. It is recommended that early diagnoses should be carried out with regards to ICR; so that non-surgical approaches may be utilized instead of surgical interventions. Furthermore, it is highly recommended to make use of MTA as a sealing material in orthograde repair due to its excellent sealing capabilities and biocompatibility.
The author thanks King Saud University, College of Dentistry Research Center (CDRC No. FR 0430) for their assistance in conducting this study.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Saudi Arabia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kopljar M, Vieyra JP S-Editor: Dou Y L-Editor: A E-Editor: Wu YXJ
| 1. | Ellis RA. Invasive cervical resorption. J Endod. 1994;20:422-423. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 2. | Heithersay GS. Clinical, radiologic, and histopathologic features of invasive cervical resorption. Quintessence Int. 1999;30:27-37. [PubMed] |
| 3. | Patel S, Kanagasingam S, Pitt Ford T. External cervical resorption: a review. J Endod. 2009;35:616-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 136] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Heithersay GS, Dahlstrom SW, Marin PD. Incidence of invasive cervical resorption in bleached root-filled teeth. Aust Dent J. 1994;39:82-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Frank AL, Torabinejad M. Diagnosis and treatment of extracanal invasive resorption. J Endod. 1998;24:500-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Tronstad L. Root resorption--etiology, terminology and clinical manifestations. Endod Dent Traumatol. 1988;4:241-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 372] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 7. | Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993;19:591-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 603] [Cited by in RCA: 601] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 8. | Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol 2000. 2014;64:57-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 556] [Cited by in RCA: 858] [Article Influence: 85.8] [Reference Citation Analysis (0)] |
| 9. | Bergmans L, Van Cleynenbreugel J, Verbeken E, Wevers M, Van Meerbeek B, Lambrechts P. Cervical external root resorption in vital teeth. J Clin Periodontol. 2002;29:580-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1000] [Cited by in RCA: 1102] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 11. | Kqiku L, Ebeleseder KA, Glockner K. Treatment of invasive cervical resorption with sandwich technique using mineral trioxide aggregate: a case report. Oper Dent. 2012;37:98-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod. 1993;19:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 477] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 13. | Arens DE, Torabinejad M. Repair of furcal perforations with mineral trioxide aggregate: two case reports. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:84-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 72] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Kaup M, Schäfer E, Dammaschke T. An in vitro study of different material properties of Biodentine compared to ProRoot MTA. Head Face Med. 2015;11:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 15. | Ciasca M, Aminoshariae A, Jin G, Montagnese T, Mickel A. A comparison of the cytotoxicity and proinflammatory cytokine production of EndoSequence root repair material and ProRoot mineral trioxide aggregate in human osteoblast cell culture using reverse-transcriptase polymerase chain reaction. J Endod. 2012;38:486-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Chen CL, Kao CT, Ding SJ, Shie MY, Huang TH. Expression of the inflammatory marker cyclooxygenase-2 in dental pulp cells cultured with mineral trioxide aggregate or calcium silicate cements. J Endod. 2010;36:465-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Hung CJ, Kao CT, Shie MY, Huang TH. Comparison of host inflammatory responses between calcium-silicate base material and IRM. J Dent Sci. 2014;9:158-164. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |