Published online Apr 6, 2019. doi: 10.12998/wjcc.v7.i7.849
Peer-review started: November 14, 2018
First decision: December 22, 2019
Revised: February 24, 2019
Accepted: March 8, 2019
Article in press: March 9, 2019
Published online: April 6, 2019
Processing time: 142 Days and 14.9 Hours
Open dislocation of the glenohumeral joint is a very rare complication with only six cases described in the literature. Most cases resulted in severe complications like avascular necrosis of the humeral head or septic arthritis with poor functional results. The “mandatory” treatment of choice is surgery, with accurate debridement and reconstruction of the damaged soft tissues. However, the results in these cases do not approach those seen in classical dislocations.
This case report is the first description of an anterior open glenohumeral dislocation without associated fractures, but with complete avulsion of the soft tissue envelope of the proximal humerus. Surgical treatment consisted of copious lavage with saline solution, meticulous debridement of the nonviable soft tissues, reduction of the dislocated humeral head and reconstruction of the soft tissue envelope of the humeral head. The selected surgical approach was an inferior extension of the wound at the level of the delto-pectoral groove, as the best choice to be able to perform an adequate debridement and capsulo-tendinous reinsertion. At 6 mo there were no clinical signs of instability of the glenohumeral joint, the functionality of the joint was restricted to 90º of anterior elevation, internal rotation to L2, with severe limitation of abduction (60º) and external rotation (0º) but without residual pain, with an Oxford shoulder Score of 28.
Thorough reconstruction of the soft tissues surrounding the shoulder joint and an early rehabilitation program are key points to a good functional result.
Core tip: Open dislocation of the scapulo-humeral joint is a very rare finding in the emergency department and is usually the result of a high velocity trauma. The “mandatory” treatment of choice is surgery, with accurate debridement and reconstruction of the damaged soft tissues. However, the results in these cases do not approach those seen in classical dislocations.
- Citation: Faur CI, Anglitoiu B, Ungureanu AM. Open anterior glenohumeral dislocation with associated supraspinatus avulsion: A case report. World J Clin Cases 2019; 7(7): 849-854
- URL: https://www.wjgnet.com/2307-8960/full/v7/i7/849.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i7.849
Shoulder dislocation is the most common dislocation seen in the emergency department, with up to 96 % of cases having traumatic origin[1]. The complication rate is quite high, especially in the young and active population, with recurrent dislocation occurring in up to 45 % of patients[1]. Nevertheless, other low incidence complications can occur such as axillary nerve palsy (with clinically a relevant incidence up to 10%[2]) shoulder instability, Bankart lesion, and humeral head fracture. The “mandatory” treatment of choice is surgery, with accurate debridement and reconstruction of the damaged soft tissues. However, the results in these cases do not approach those seen in classical dislocations.
A 64-year male pedestrian was hit by a motor vehicle.
Following impact, he felt down on his elbow, with the right arm in extension, external rotation and adduction, so that a direct postero-anterior and inferior-superior force was applied through the humerus to the humeral head.
There were no significant comorbidities at admission.
The patient was a non-smoker, without personal or family history of other diseases.
On initial examination, in the emergency room, the pulse to the radial artery was present and no neurological deficit was found. Inspection of the humeral head revealed almost complete avulsion of the soft tissues which normally insert on the humeral head. The supraspinatus muscle was the only preserved soft tissue attachment on the head of the humerus; the external rotators were torn at the level of the muscle belly near its scapular insertion. Inspection of the wound, on the anterosuperior aspect of the glenohumeral joint, revealed absence of foreign bodies with only moderate blood loss, suggestive of an inside-out mechanism of dislocation. The wound appeared quite clean. The patient underwent radiological examination in order to obtain a more accurate diagnosis - as an associated fracture could not be excluded solely by inspection.
Laboratory results including complete blood count, electrolytes, and coagulation panels were within normal limits, with a white blood count of 6.21 K/μL, red blood cell count of 4.8 × 1012/L, and hemoglobin of 145 G/L.
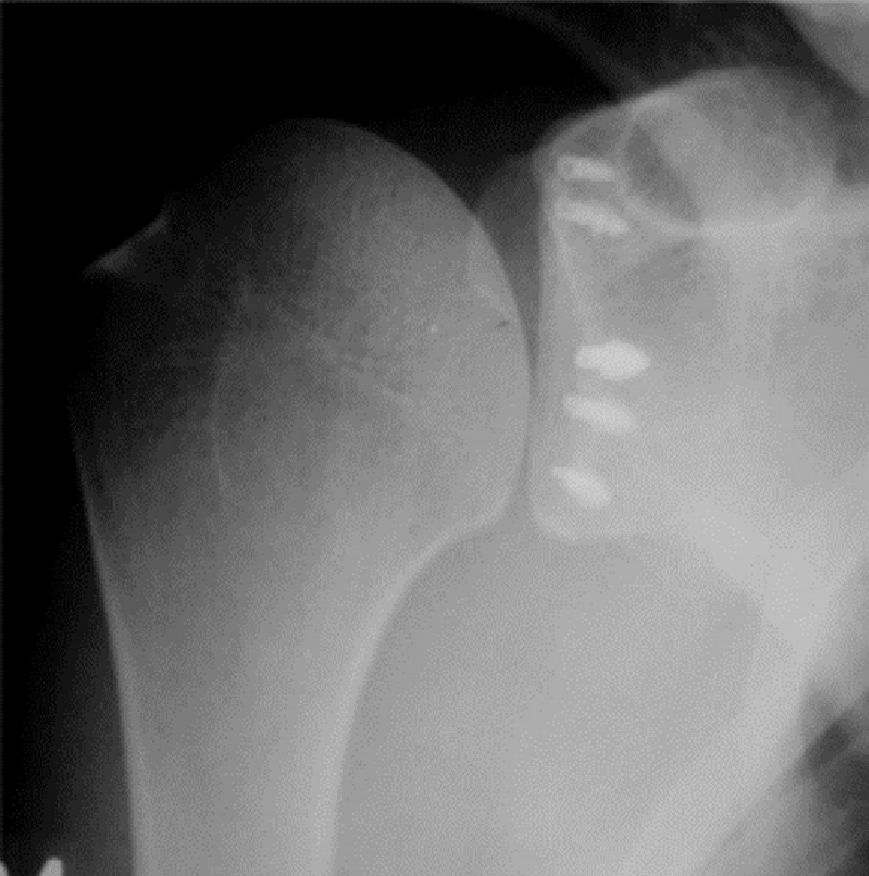
The anteroposterior position radiological view of the shoulder (Figure 1) demon-strated no fracture, and a definitive diagnosis of an open anterior dislocation of the left glenohumeral joint was established. After the radiological examination the patient was emergently taken to the operating room for surgical treatment, approximately 90 min from the time of the initial accident. The vital signs of the patient were stable - and the only other associated trauma was a displaced bimalleolar fracture of the contralateral ankle confirmed on X-ray.
After inspection of the injured extremity in the emergency room he was diagnosed with open dislocation of the right glenohumeral joint (Figure 2). The dislocated head was visible in the anterosuperior region of the shoulder joint, exactly at the level of the acromio-clavicular joint, with the apex of the humeral head resting 2 cm superior to the clavicle.
Surgical treatment consisted of copious lavage with saline solution (approximately 3000 mL), meticulous debridement of the nonviable soft tissues, and reduction of the dislocated humeral head and reconstruction of the soft tissue envelope of the humeral head. The selected surgical approach was an inferior extension of the wound at the level of the delto-pectoral groove, as the best choice to be able to perform an adequate debridement and capsulo-tendinous reinsertion.
The reinsertion of the subscapularis tendon at the level of the medial tubercle of the bicipital groove was performed by direct transosseous sutures along with the anterior ruptured portion of the capsule (with its superior, medial and inferior glenohumeral ligaments), followed by reattachment of the pectoralis major tendon to its anatomical position (Figure 3).
The ruptured long head of biceps brachialis tendon was fixed in the bicipital groove through a keyhole technique. The reinsertion of the capsulo-labral structures was performed from 1 to 5 o’clock using five 2.7 mm metallic anchors (Mini Corkscrew® FT suture anchor, Arthrex) (Figure 4).
The bimalleolar fracture was surgically stabilized three days after the initial surgical procedure, using one third semitubular plate on the peroneus and two 3.5 mm lag screws on the internal malleolus.
Postoperatively the patient was immobilized for three weeks in a shoulder orthosis, which allowed small movements of the elbow joint. The patient also received an antibiotic combination for 7 d (Gentamicin 3 × 80mg; Cetriaxonum 2 × 1g/d).
The local evolution was favourable with complete healing and removal of the skin sutures after 14 d.
After two weeks the patient started an aggressive program of rehabilitation consisting of passive ROM exercises, avoiding abduction and external rotation in order to protect the inserted soft tissues. After six weeks active full ROM of the shoulder joint was allowed including passive and active abduction and external rotation. Muscle strength exercises were permitted after 10 wk postoperatively. At 6 mo there were no clinical or radiological signs of infection with a good centration of the humeral head in the glenoid cavity and no signs of avascular necrosis. Although there were no clinical signs of instability of the glenohumeral joint, the functionality of the joint was restricted to 90º of anterior elevation, internal rotation to L2, with severe limitation of abduction (60º) and external rotation (0º) but without residual pain, with an Oxford shoulder Score of 28 at 6 months[3,4].
Open dislocation of the glenohumeral joint is a very rare, but extremely debilitating injury, due to involvement of the periarticular soft tissue envelope. In review of the literature, we found only six cases of patients with open dislocations of the shoulder.
Most open dislocations occur inferiorly (luxatio erecta). In 2011 Garrigues et al[5] reported an inferior open glenohumeral dislocation following a work-related injury. This was only the fourth case reported in the literature since 1800 and all resulted in significantly reduced function, infection and avascular necrosis of the humeral head.
Another case of inferior open luxatio erecta was reported in 1996 by Davison and Orwin[1] after a farm equipment accident. The humeral head penetrated the skin inferior to the pectoralis major muscle with avulsion of the greater tuberosity and tearing of the subscapularis tendon near its insertion into the lesser tuberosity. At 18 mo follow up despite rehabilitation attempts there was restriction of ROM without avascular necrosis of the humeral head.
A less common type of open glenohumeral dislocation is the posterior variety (2%-4%)[6]. Two cases of this type of humeral head dislocation were reported by Moeller[7] in 1975 and by Maroney and Devinney[8] in 2011. Both patients were involved in motor vehicle accidents and suffered complete skeletonization of the proximal humerus without any associated fractures of the upper limb. Moeller’s patient was treated by immediate irrigation, debridement, open reduction and reconstruction of the avulsed tendons followed by 2 mo of immobilization. The wound was complicated by a transient infection that required repeated irrigation and de-bridement. The functional results were unsatisfactory with only 70º of abduction, probably the result of damage to the suprascapular and axillary nerves, with residual pain secondary to avascular necrosis[7]. The second case (Maroney and Devinney) was treated using a staged procedure. Aggressive irrigation and debridement were first performed in the emergency room with closure of the initial wound followed by a second procedure two days later involving reconstruction of the soft tissue envelope via an anterior approach using bone anchors. The surgical treatment was followed by a three-week immobilization period followed by a rehabilitation program. The best functional result was obtained with this particular patient whose residual ROM at the glenohumeral joint was restricted to 120º of forward elevation, 90º of abduction and internal rotation to L4 without any signs of avascular necrosis[8].
The last variety of open glenohumeral dislocation is the anterior or anterosuperior type. Lucas and Peterson[9] in 1977 reported an anterior open shoulder dislocation without any mention of soft tissues injuries. The functional results were poor with loss of ROM of the shoulder joint and avascular necrosis of the humeral head.
A second case of anterior open glenohumeral dislocation was reported by Gregory and Lord[10] in 1996. A 15-year-old patient had a fair functional result but unfor-tunately developed avascular necrosis at radiological follow-up.
Our case report is the first description of an anterior open glenohumeral dislocation with complete avulsion of the soft tissue envelope of the proximal humerus without associated fractures of the shoulder bones. Another peculiarity unique to this case was the preservation of the humeral insertion of the supraspinatus muscle with avulsion of the scapular insertion.
In order to produce an open glenohumeral dislocation there are two conditions which must met. These include the position of the joint and a direct or indirect force transmitted to the joint that is severe enough to tear the soft tissues surrounding the shoulder. In our case, the right arm at the moment of impact with the ground was in extension, external rotation and adduction, which directed the humeral head to a space, just below the acromion, where there was no other bony protection. This lack of bony protection is likely responsible for anterior dislocation of humeral head without any associated fractures.
The preservation of the cartilage of the humeral head at the moment of injury, despite the devastating effect on the soft tissues of the shoulder joint, confirms the low osseous stability of the shoulder joint and the lack of bony obstacles to the humeral head during its dislocation from the joint at the moment of impact.
In conclusion this type of injury occurs during high velocity accidents and is almost always associated with other injuries. The most frequent complication involves avascular necrosis of the humeral head which occurs in over 60% of cases reported in the literature. Despite aggressive rehabilitation following reconstruction of the soft tissues of the shoulder joint, the functional results are almost always unsatisfactory with severe functional impairment of the glenohumeral joint.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Romania
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Noussios GI, Anand A S-Editor: Dou Y L-Editor: A E-Editor: Wu YXJ
| 1. | Davison BL, Orwin JF. Open inferior glenohumeral dislocation. J Orthop Trauma. 1996;10:504-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Haragus H, Prejbeanu R, Patrascu J, Faur C, Roman M, Melinte R, Timar B, Codorean I, Stetson W, Marra G. Cross-cultural adaptation and validation of the Romanian Oxford Shoulder Score. Medicine (Baltimore). 2018;97:e10926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Dawson J, Rogers K, Fitzpatrick R, Carr A. The Oxford shoulder score revisited. Arch Orthop Trauma Surg. 2009;129:119-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 255] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 5. | Garrigues GE, Nagda SH, Yu J. Open luxatio erecta: a case report and literature review. J Orthop Trauma. 2011;25:e34-e37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Sasashige Y, Kurata T, Masuda Y, Shimono K, Nagata Y. Dislocation of the shoulder joint with ipsilateral humeral shaft fracture: two case reports. Arch Orthop Trauma Surg. 2006;126:562-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Moeller JC. Compound posterior dislocation of the glenohumeral joint. Case report. J Bone Joint Surg Am. 1975;57:1006-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Maroney SS, Devinney DS. Open glenohumeral dislocation: skeletonization of the proximal humerus without associated fracture. Orthopedics. 2011;34:e776-e780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Lucas GL, Peterson MD. Open anterior dislocation of the shoulder. J Trauma. 1977;17:883-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Gregory PR, Lord M. Open anterior dislocation of the shoulder. J Orthop Trauma. 1996;10:128-130. [PubMed] |