Published online Feb 26, 2019. doi: 10.12998/wjcc.v7.i4.532
Peer-review started: November 5, 2018
First decision: January 5, 2019
Revised: January 21, 2019
Accepted: January 26, 2019
Article in press: January 26, 2019
Published online: February 26, 2019
Processing time: 115 Days and 6.9 Hours
Spinal deformities in Ehlers-Danlos syndrome (EDS; type VI) are generally progressive and severe. Surgical treatment has been described for kyphoscoliosis in the thoracolumbar spine. However, there are few studies describing the consequences of an anterior approach in cervical kyphosis. An anterior approach may not be able to fully decompress the spinal canal and restore the normal curvature of the cervical spine. Therefore, the anterior approach for cervical kyphosis in young children is hard. We describe the first case in an EDS girl with cervical kyphosis who received satisfactory anterior cervical corpectomy decompression and fusion.
The chief complaints of a 16-year-old girl with EDS were double upper limb weakness for 7 years and double lower limb walking instability for 2 years. Moreover, the imaging results revealed that the degree of kyphosis from cervical vertebra 2 to 4 accompanying with spinal cord compression was 30°. An anterior cervical corpectomy involving cervical vertebra 3 and a titanium mesh implant were performed with internal fixation. The results at 3 mo after surgery demonstrated that the anterior fusion was solid, and the kyphosis of the cervical spine was corrected. Additionally, the power of all four extremities was significantly improved.
The incidence rate of cervical kyphosis in EDS is rare. The surgical treatment for these patients, especially an anterior approach, is challenging. Therefore, to develop safer and more effective strategies to treat cervical kyphosis in EDS, there is still much work to do.
Core tip: Ehlers-Danlos syndrome (ESD) is a rare inherited and clinically heterogeneous group of connective tissue disorders. We report a case diagnosed with ESD that was treated by anterior cervical surgery. The clinical outcome is satisfactory.
- Citation: Fang H, Liu PF, Ge C, Zhang WZ, Shang XF, Shen CL, He R. Anterior cervical corpectomy decompression and fusion for cervical kyphosis in a girl with Ehlers-Danlos syndrome: A case report. World J Clin Cases 2019; 7(4): 532-537
- URL: https://www.wjgnet.com/2307-8960/full/v7/i4/532.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i4.532
Ehlers-Danlos syndrome (EDS) is an inherited and clinically heterogeneous group of connective tissue disorders[1,2]. EDS is characterized by joint laxity and skin fragility[3]. Based on the degree of the clinical symptoms, the different biochemical and genetical defects, and the mode of inheritance, six major subtypes of EDS have been recognized since 1998. Among these subtypes, EDS VI (known as the kyphoscoliotic type) is extremely rare. In EDS VI, the kyphoscoliosis is progressive and accompanied with joint hypermobility and abnormal scarring[4]. Overall, the incidence rate of EDS is lower than 1 in 100000 live births[5,6]. The procollagen-lysine, 2-oxoglutatrate 5-dioxygenase (PLOD1) gene encodes lysyl hydroxylase (LH1) to catalyze the formation of hydroxylysine in collagen chains[7,8]. The kyphoscoliotic type with a deficiency of PLOD1/LH1 is of the most interest to a spinal specialist. Among the pediatric population diagnosed with EDS VI, the initial treatment focuses on physical therapy. However, the curve development of scoliosis is rapid. Therefore, once conservative treatment fails or neurologic defects occur because of spinal cord decompression, surgical treatment should be selected[9,10]. Many studies have demonstrated surgical treatment for adolescents with thoracolumbar kyphoscoliosis; however, reports involving cervical kyphoscoliosis are few[11]. Andrew J. Koberts reported a case where the anterior and posterior approaches were used to treat an infant with EDS type VI with symptomatic cervical kyphoscoliosis[12]. Herman and Sonntag reported 20 cases of cervical kyphosis treated by anterior cervical decompression, bone grafting, and anterior cervical plating. The average preoperative kyphosis was 38°, and the postoperative correction was 16°. In addition, 10% of patients had a complete remission of preoperative symptoms, and 55% had improved nerve function[13].
As we all know, because of the severe deformity associated with a significant risk of complications, surgery for these patients is extremely difficult. Moroever, it is difficult to develop a surgical standard of treatment for these diseases, so the individual approach may be advisable. This report concerns a 16-year-old girl with EDS VI with symptomatic cervical kyphosis who underwent anterior cervical corpectomy decompression and fusion (ACCF).
The chief complaints of a 16-year-old female with EDS were double upper limb weakness for 7 years and double lower limb walking instability for 2 years.
The patient developed limb weakness without obvious inducement for 7 years, and did not receive enough attention. She did not receive regular treatment else. And she gradually became unable to walk independently before one month.
She denied any history of trauma or surgery and did not have hypertension, diabetes, or cardiovascular and cerebrovascular diseases.
Her father and brother both had a blue tint to the sclera, joint hypermobility, abnormal scarring, and planovalgus feet.
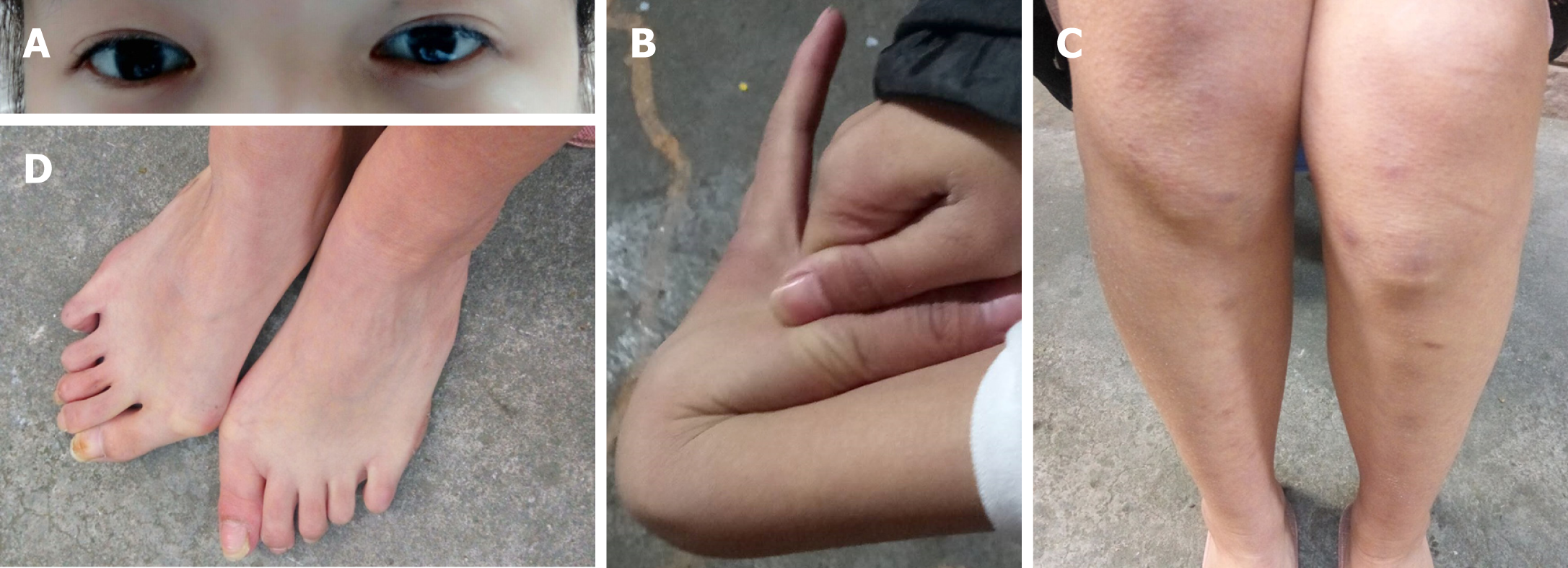
This patient was noted to have a blue tint to the sclera (Figure 1A), joint hypermobility (Figure 1B), abnormal scarring (Figure 1C), and planovalgus feet (Figure 1D). The power of main muscles in four extremities was approximately level III-IV.
Routine blood tests, routine urine tests and urinary sediment examination, routine fecal tests and occult blood test, blood biochemistry, immune indexes, and infection indexes were all normal.
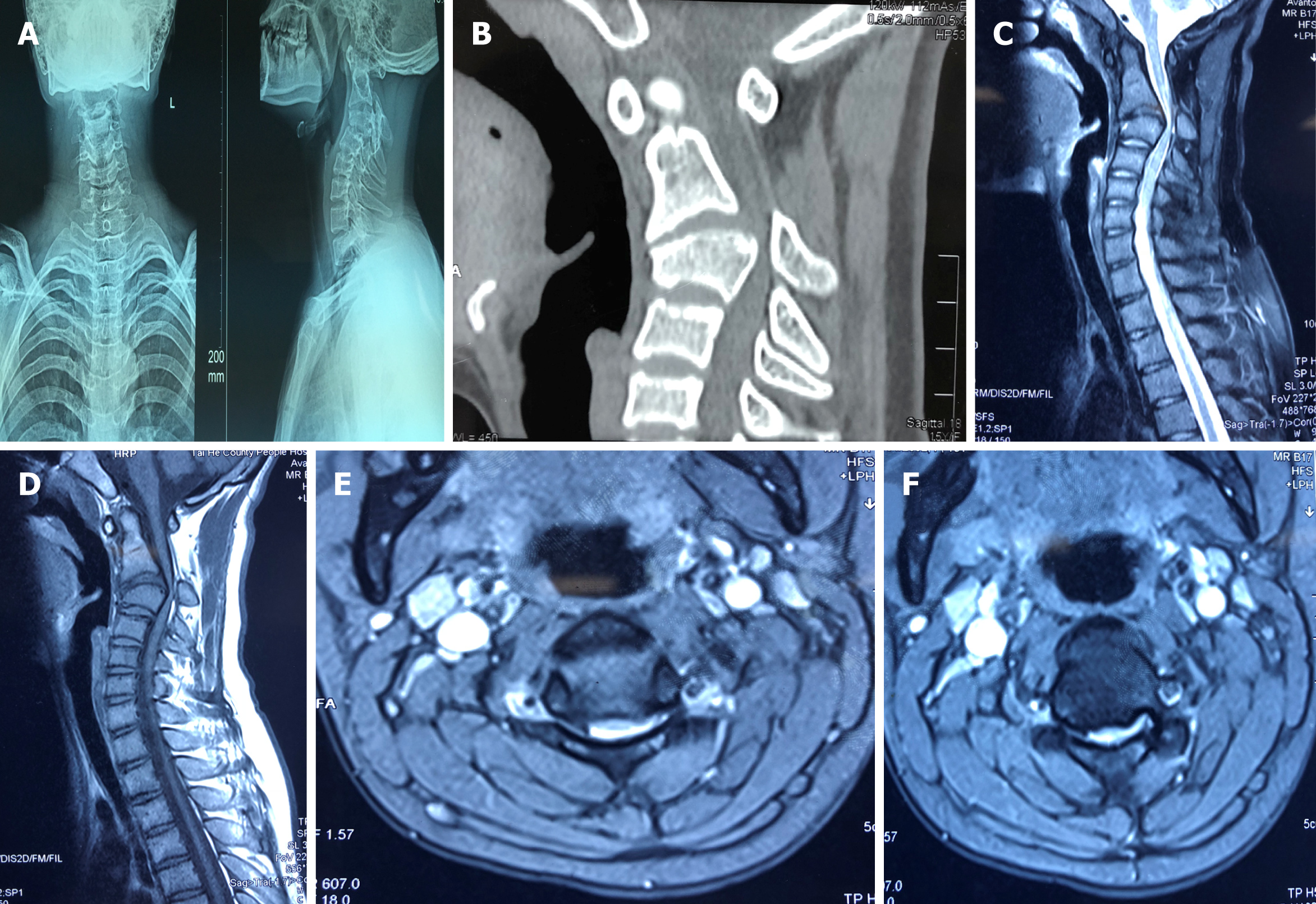
Imaging results (Figure 2) demonstrated that kyphosis at the C3 level was 30° and the cervical spinal cord was compressed from C2 to C4.
After satisfactory intratracheal anesthesia, the patient was intubated in an appropriate position to avoid excessive activity of the cervical spine. To expose enough field for surgery, a thin pillow was placed behind the shoulder to extend the neck. Through a right-side transverse incision, the cervical spine was exposed carefully. When the gap of C2/3 and C3/4 was certain, a spreader was mounted in the C2 and C4. The intervertebral discs of C3/C4 and C2/C3 were removed to expose the posterior edge of the vertebral body. The operator used rongeur and ultrathin pliers to remove the middle 2/3 of the C3 vertebral body, and the ossified posterior longitudinal ligament was bited. The cartilage surface of C2 and C4 was revealed; the length between C2 and C4 was measured. A titanium mesh was filled with bone from the C3 previously bited and then implanted into the gap between C2 and C4. Because the bone was enough, the iliac crest allograft was not selected. Finally, we used the appropriate titanium nails and plates for the anterior internal fixation. Moreover, during the operation, neuromonitoring was carried out, and no surgical complications were observed. Postoperatively, a satisfactory internal fixation was achieved, and a soft external neck brace was used.
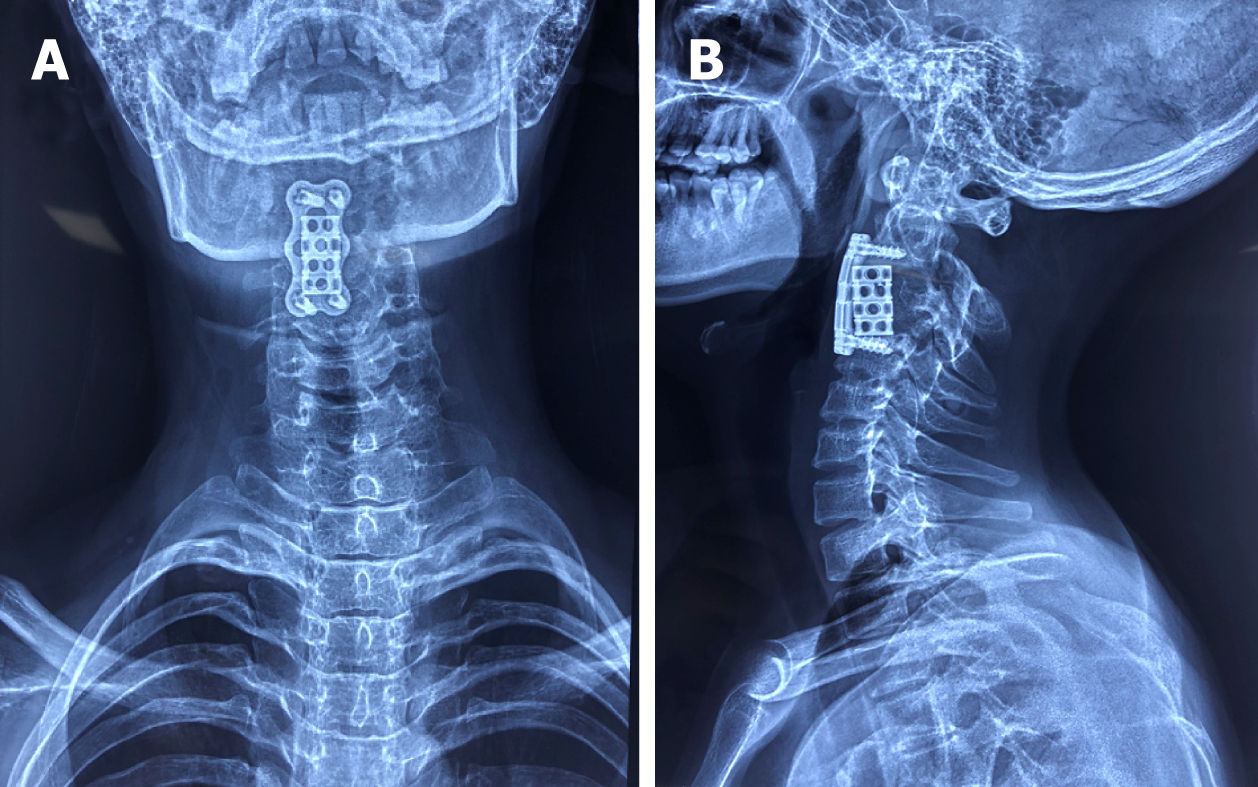
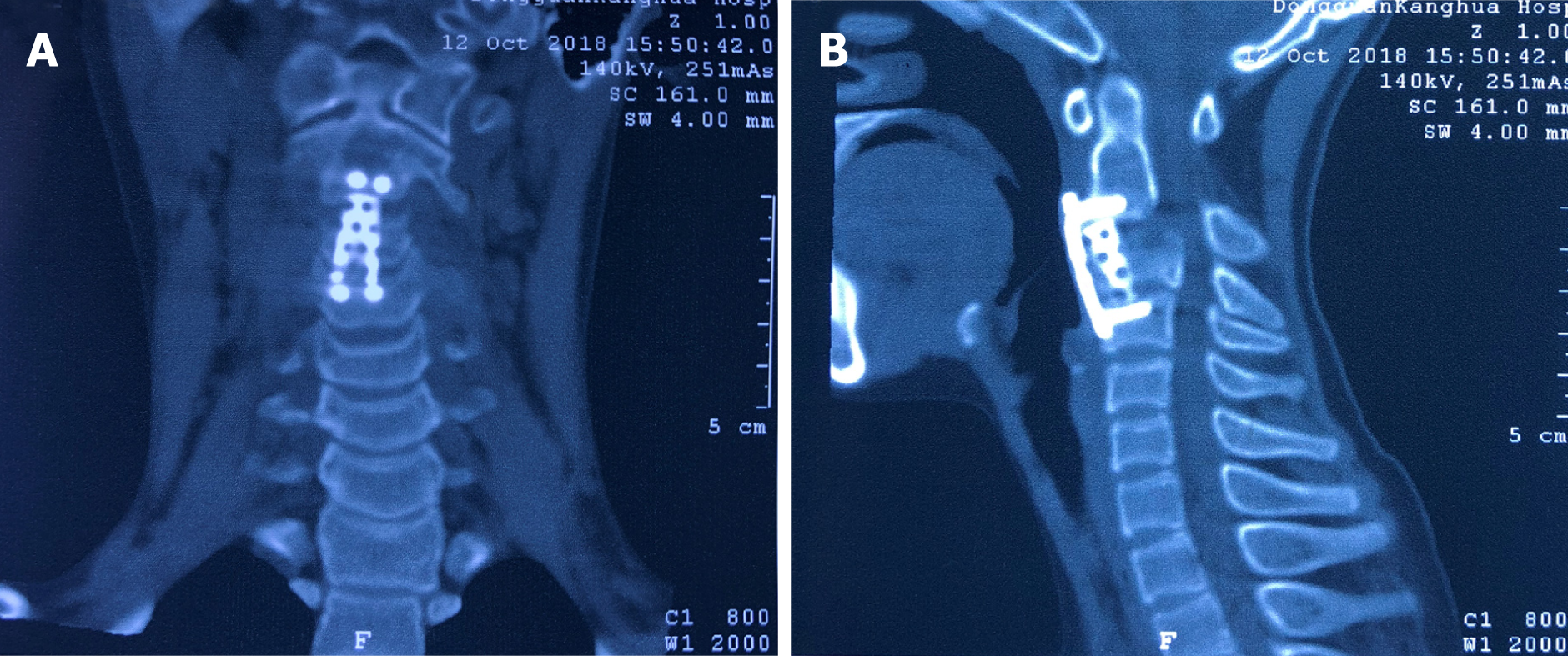
Radiographs 6 wk following anterior cervical corpectomy decompression and fusion showed that the preoperative kyphotic deformity in the cervical spine was significantly corrected (Figure 3). At the 3-mo follow-up, the patient showed significant neurological improvement, as she could walk independly and was able to perform fine movements with her double upper limbs. A computed tomography scan at 5 mo after surgery demonstrated a solid fusion of C2-4 with no displacement of internal hardware anteriorly (Figure 4). Moreover, the normal physiological curvature of the cervical spine was restored.
Villefranche Nosology demonstrated the major and minor diagnostic standards for the kyphoscoliosis type of EDS in 1998[4]. The major standards include joint hypermobility, decrease of muscle tension, and progressive scoliosis. The secondary standards include abnormal scarring and tissue fragility, osteopenia, miceocorneae, and arterial burst. Hypermobility of the cervical spine may lead to craniocervical unbalance and progressive cervical kyphoscoliosis, usually accompanied by motor disfunction, radiculopathy, myelopathy, and sensory disorders[5]. Some studies demonstrated that congenital severe hypotonia was always accompanied by a decrease in muscle power. Patients diagnosed with EDS VI may suffer from myopathy[14]. Yiş et al[15] revealed that the patients diagnosed with EDS VI were homozygous for PLOD1 mutations, leading to either loss of function of LH1 or to its deficit. Surgery may be selected when neurological changes or deformity are progressive. However, there is no article describing only anterior surgical management for patients with cervical kyphosis diagnosed with EDS VI.
The purpose of surgery is to relieve the compression of the cervical spinal cord, restore the normal curvature of the cervical spine, and stabilize the cervical vertebrae. However, internal fixation in underage girls is challenging due to the anatomy and lack of devices designed specifically for this patient. Moreover, in such limited space, when adequate decompression of the cervical spinal cord and restoration of the physiological curvature are performed, the risk of iatrogenic injury to the spinal cord is high. To prevent screw backout, anterior cervical plates need to be used individually. The autograft and allograft have been found to lead to clinical success, but the first is usually recognized as the gold standard[16]. Specifically, the bited bone from C3 is enough for grafting in this case, so we did not use any other materials. The external immobilization is an important process after surgery. Halo fixation may be a good choice, but due to the complications of pin loosening and infection, its use is sometimes limited[17]. Due to the reliable internal fixation, in this case, we only used soft fixation for 4-6 wk. Lacking of convincing materials, the long-term effect of internal fixation in pediatric patients is not fully clear. There is still much work to be done. However, many studies have found that few children achieve continued growth after fusion of the subaxial spine[18].
We report the first case of cervical kyphosis in a pediatric patient with EDS VI, who achieved a satisfactory clinical consequence only following ACCF. There is still some work needed to reveal the details about this case. In addition to some biomolecular and genetic experiments, we may need more time to follow her.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lakhdar F, Rodrigues-Lisoni FC S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Tan WW
| 1. | Giunta C, Superti-Furga A, Spranger S, Cole WG, Steinmann B. Ehlers-Danlos syndrome type VII: clinical features and molecular defects. J Bone Joint Surg Am. 1999;81:225-238. [PubMed] |
| 2. | Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ. Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK). Am J Med Genet. 1998;77:31-37. [PubMed] |
| 3. | Abdalla EM, Rohrbach M, Bürer C, Kraenzlin M, El-Tayeby H, Elbelbesy MF, Nabil A, Giunta C. Kyphoscoliotic type of Ehlers-Danlos Syndrome (EDS VIA) in six Egyptian patients presenting with a homogeneous clinical phenotype. Eur J Pediatr. 2015;174:105-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Giunta C, Randolph A, Al-Gazali LI, Brunner HG, Kraenzlin ME, Steinmann B. Nevo syndrome is allelic to the kyphoscoliotic type of the Ehlers-Danlos syndrome (EDS VIA). Am J Med Genet A. 2005;133A:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Henderson FC Sr, Austin C, Benzel E, Bolognese P, Ellenbogen R, Francomano CA, Ireton C, Klinge P, Koby M, Long D, Patel S, Singman EL, Voermans NC. Neurological and spinal manifestations of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175:195-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 143] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 6. | Porter DA, Glotzbecker MP, Timothy Hresko M, Hedequist DJ. Deep Surgical Site Infections Following Pediatric Cervical Spine Surgery. J Pediatr Orthop. 2017;37:553-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Hyland J, Ala-Kokko L, Royce P, Steinmann B, Kivirikko KI, Myllylä R. A homozygous stop codon in the lysyl hydroxylase gene in two siblings with Ehlers-Danlos syndrome type VI. Nat Genet. 1992;2:228-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 74] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Kivirikko KI, Pihlajaniemi T. Collagen hydroxylases and the protein disulfide isomerase subunit of prolyl 4-hydroxylases. Adv Enzymol Relat Areas Mol Biol. 1998;72:325-398. [PubMed] |
| 9. | McMaster MJ. Spinal deformity in Ehlers-Danlos syndrome. Five patients treated by spinal fusion. J Bone Joint Surg Br. 1994;76:773-777. [PubMed] |
| 10. | Vogel LC, Lubicky JP. Neurologic and vascular complications of scoliosis surgery in patients with Ehlers-Danlos syndrome. A case report. Spine (Phila Pa 1976). 1996;21:2508-2514. [PubMed] |
| 11. | Akpinar S, Gogus A, Talu U, Hamzaoglu A, Dikici F. Surgical management of the spinal deformity in Ehlers-Danlos syndrome type VI. Eur Spine J. 2003;12:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Kobets AJ, Komlos D, Houten JK. Congenital cervical kyphosis in an infant with Ehlers-Danlos syndrome. Childs Nerv Syst. 2018;34:1411-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Herman JM, Sonntag VK. Cervical corpectomy and plate fixation for postlaminectomy kyphosis. J Neurosurg. 1994;80:963-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 145] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Rohrbach M, Vandersteen A, Yiş U, Serdaroglu G, Ataman E, Chopra M, Garcia S, Jones K, Kariminejad A, Kraenzlin M, Marcelis C, Baumgartner M, Giunta C. Phenotypic variability of the kyphoscoliotic type of Ehlers-Danlos syndrome (EDS VIA): clinical, molecular and biochemical delineation. Orphanet J Rare Dis. 2011;6:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Yiş U, Dirik E, Chambaz C, Steinmann B, Giunta C. Differential diagnosis of muscular hypotonia in infants: the kyphoscoliotic type of Ehlers-Danlos syndrome (EDS VI). Neuromuscul Disord. 2008;18:210-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Betz RR, Lavelle WF, Samdani AF. Bone grafting options in children. Spine (Phila Pa 1976). 2010;35:1648-1654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Garfin SR, Roux R, Botte MJ, Centeno R, Woo SL. Skull osteology as it affects halo pin placement in children. J Pediatr Orthop. 1986;6:434-436. [PubMed] |
| 18. | Anderson RC, Ragel BT, Mocco J, Bohman LE, Brockmeyer DL. Selection of a rigid internal fixation construct for stabilization at the craniovertebral junction in pediatric patients. J Neurosurg. 2007;107:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |