Published online Feb 26, 2019. doi: 10.12998/wjcc.v7.i4.482
Peer-review started: October 29, 2018
First decision: November 27, 2018
Revised: December 25, 2018
Accepted: January 8, 2019
Article in press: January 8, 2019
Published online: February 26, 2019
Processing time: 121 Days and 2.9 Hours
Chemotherapy is a standard strategy for stage IV gastric cancer patients. However, some cases cannot undergo conversion surgery because of their frailty, even if the patients had response to chemotherapy. For these patients, local tumor progression is a problem. We report here the case of a patient whose residual gastric cancer was resected through endoscopic submucosal dissection (ESD) after concomitant chemotherapy for metastatic gastric cancer.
An 85-year-old male complained of difficulty swallowing, and examination revealed gastric cancer with multiple liver metastases. Although he received concomitant chemotherapy, a residual tumor was observed in the primary lesion while the metastatic lesions disappeared completely. Conversion surgery was considered optional treatment; however, he could not undergo that because of advanced age and comorbidities. Thus, we performed ESD to treat the residual tumor. As a result, we resected the residual lesion completely. The patient has been alive for 29 mo since ESD, without recurrence.
We achieved local control using ESD, and these findings may provide therapeutic improvements both in local control and patient survival outcomes.
Core tip: Some cases cannot undergo conversion surgery because of their frailty, even if the patients had response to chemotherapy. For these patients, local tumor progression is a problem. We resected a residual tumor completely using endoscopic submucosal dissection (ESD) after chemotherapy in an elderly patient who was unable to undergo conversion surgery due to his age and comorbidities. The patient has been alive without recurrence for 29 mo after the ESD. ESD may provide therapeutic improvements in both local control and patient survival outcomes.
- Citation: Hayashi K, Suzuki S, Ikehara H, Okuno H, Irie A, Esaki M, Kusano C, Gotoda T, Moriyama M. Endoscopic resection for residual lesion of metastatic gastric cancer: A case report. World J Clin Cases 2019; 7(4): 482-488
- URL: https://www.wjgnet.com/2307-8960/full/v7/i4/482.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i4.482
For patients with stage IV gastric cancer, chemotherapy is a standard treatment option. Improvements in chemotherapy regimens have improved patient survival[1]; for example, patients’ median survival time is longer and the response rate continues to rise[2,3]. However, treatment outcomes for metastatic gastric cancer (mGC) remain unsatisfactory. Regardless, the improved efficacy of chemotherapy has led to the ability to perform surgery on tumors that were originally regarded as technically or oncologically unresectable or only marginally resectable. Conversion surgery is one treatment option with the potential to improve survival outcomes[4]. Yet, some factors prevent surgical resection, particularly advanced age, low performance status, and comorbidity, even if the patient achieves a complete response from chemotherapy. Many of these patients also experience difficulties with continuing intensive chemotherapy; thus, palliative treatment is often performed. Additionally, gastric stenosis and gastroparesis caused by local recurrence are major problems that decrease a patient’s quality of life.
Endoscopic submucosal dissection (ESD) is a common practice used to resect early gastric cancer. It is a minimally intensive procedure that can preserve quality of life. Moreover, the procedure can resect the whole specimen, which allows for correct histopathological assessment. We report herein a case of a patient with mGC that responded to chemotherapy and who underwent a complete resection of the residual tumor using ESD. Twenty-nine months after the ESD, no local recurrence or distant metastases have been found.
An 85-year-old Japanese male complained of difficulty swallowing and visited a hospital. He had a medical history of untreated abdominal aortic aneurysm and pulmonary phthisis. He underwent esophagogastroduodenoscopy to diagnose his symptoms, and a protruding lesion at the gastric cardia was found. Endoscopic biopsy confirmed a moderately differentiated adenocarcinoma. Abdominal computed tomography (CT) showed no evidence of the tumor invading the muscularis propria and serosa, enlarged lymph nodes, or distant metastases. Therefore, this lesion was diagnosed as stage IA gastric cancer (cT1N0M0, 7th edition of UICC TNM Classification of Malignant Tumors).
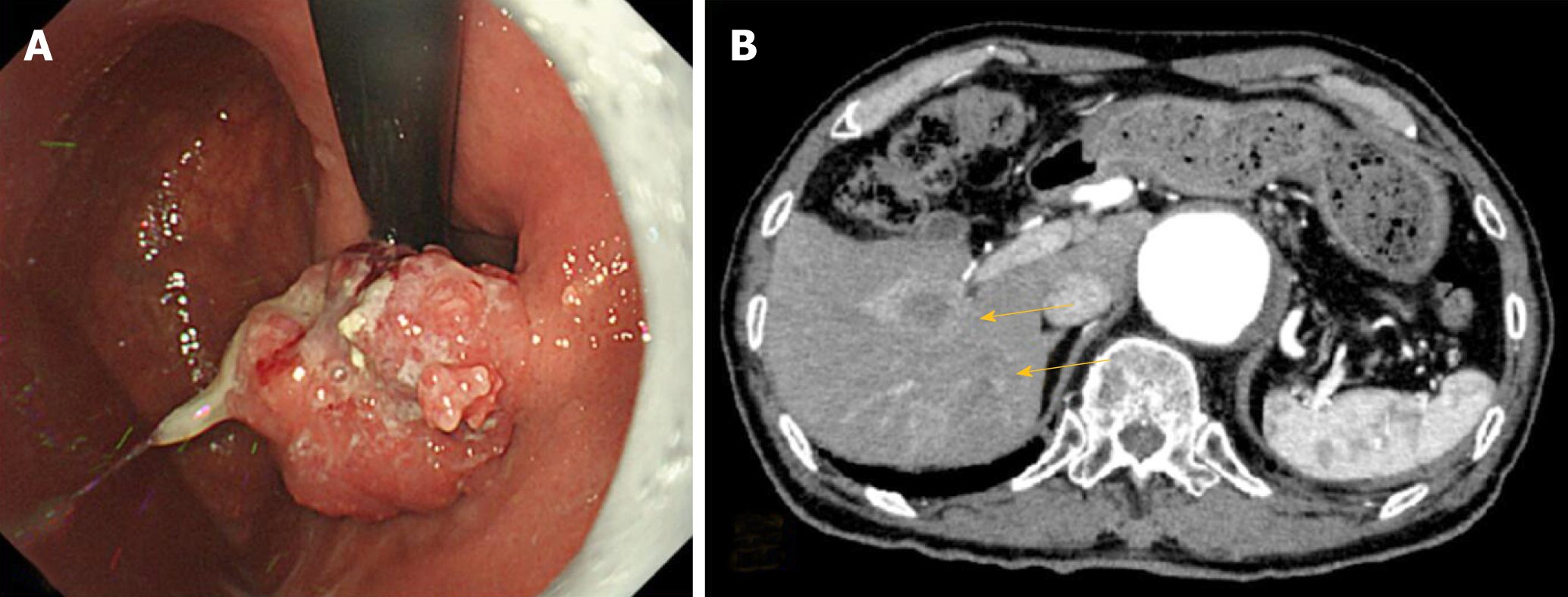
Four months after diagnosis, the patient visited our institution for treatment of this lesion. It took a long time for the patient to visit because he could not decide which treatment to take, with his options being surgery and endoscopic treatment. The tumor (Figure 1A) grew to 20 mm in size, and abdominal CT result showed clear evidence of multiple mass lesions (range: 10-30 mm) in the liver, suggesting metastases of his gastric cancer (Figure 1B); however, there was no evidence of the tumor invading the muscularis propria and serosa or of lymph nodes’ swelling. Therefore, the diagnosis was changed to stage IV gastric cancer.
The clinical diagnosis was gastric cancer with liver metastases; stage IV (cT1N0M1).
Although the patient was elderly, he was in the Eastern Cooperative Oncology Group performance status of 1 and had adequate organ functions; therefore, chemotherapy was deemed appropriate.
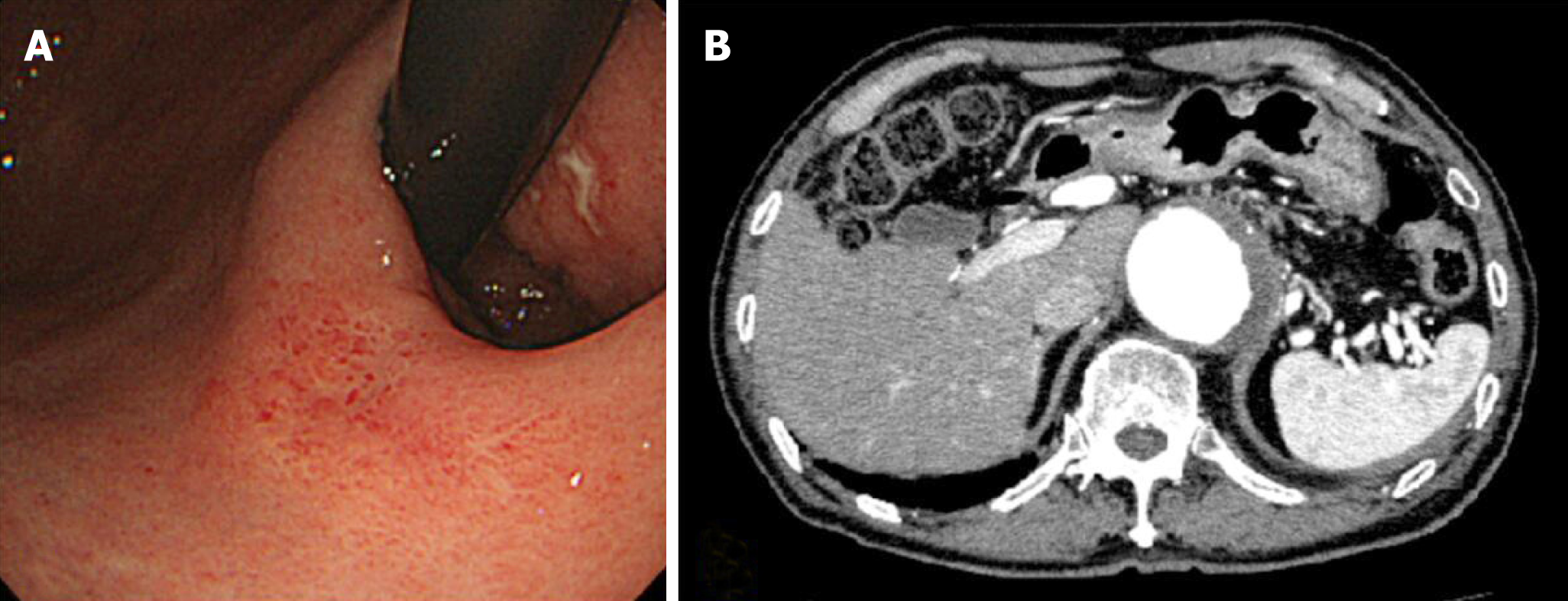
S-1 and oxaliplatin combination therapy (SOX) were administered. S-1 was administered orally (100 mg/d), and oxaliplatin was delivered via intravenous infusion (70 mg/m2 diluted in 500 mL of saline over 120 min). The patient underwent four cycles of SOX, beginning 1 mo after the diagnosis of mGC. Each SOX cycle lasted 3 wk, with S-1 administered daily on days 1 to 14 of each cycle, and oxaliplatin administered only on day 1 of each cycle. After SOX, the primary lesion decreased, although it was confirmed macroscopically, and endoscopic biopsy revealed no atypia. Additionally, CT confirmed no evidence of liver metastases. However, the patient had grade 3 sensory peripheral neuropathy (Common Terminology Criteria for Adverse Events version 4.0; CTCAE4.0); thus, oxaliplatin was discontinued and S-1 was continued for two additional cycles. Thereafter, the primary lesion macroscopically appeared smooth and protruded, and it appeared similar to a submucosal tumor (Figure 2A). The endoscopic biopsy still revealed no atypia. CT results showed no lymph node swelling or distant metastasis (Figure 2B). Therefore, we determined that the patient had had a complete response to the chemotherapy. At that point, the patient’s difficulty in swallowing had improved, but he had grade 3 anorexia and sensory peripheral neuropathy (CTCAE4.0); therefore, S-1 was discontinued.
Due to the patient’s response to chemotherapy, conversion surgery was considered. The patient’s liver metastases had completely disappeared and the primary lesion became unclear macroscopically; however, conversion surgery was difficult because of his advanced age and comorbidities. Although the biopsy specimen at the mucosa of the primary lesion revealed no atypia after chemotherapy, a residual tumor was suspected under the mucosal layer because it looked like there was submucosal tumor. Therefore, ESD was performed for the primary lesion. The lesion was resected with no complications.
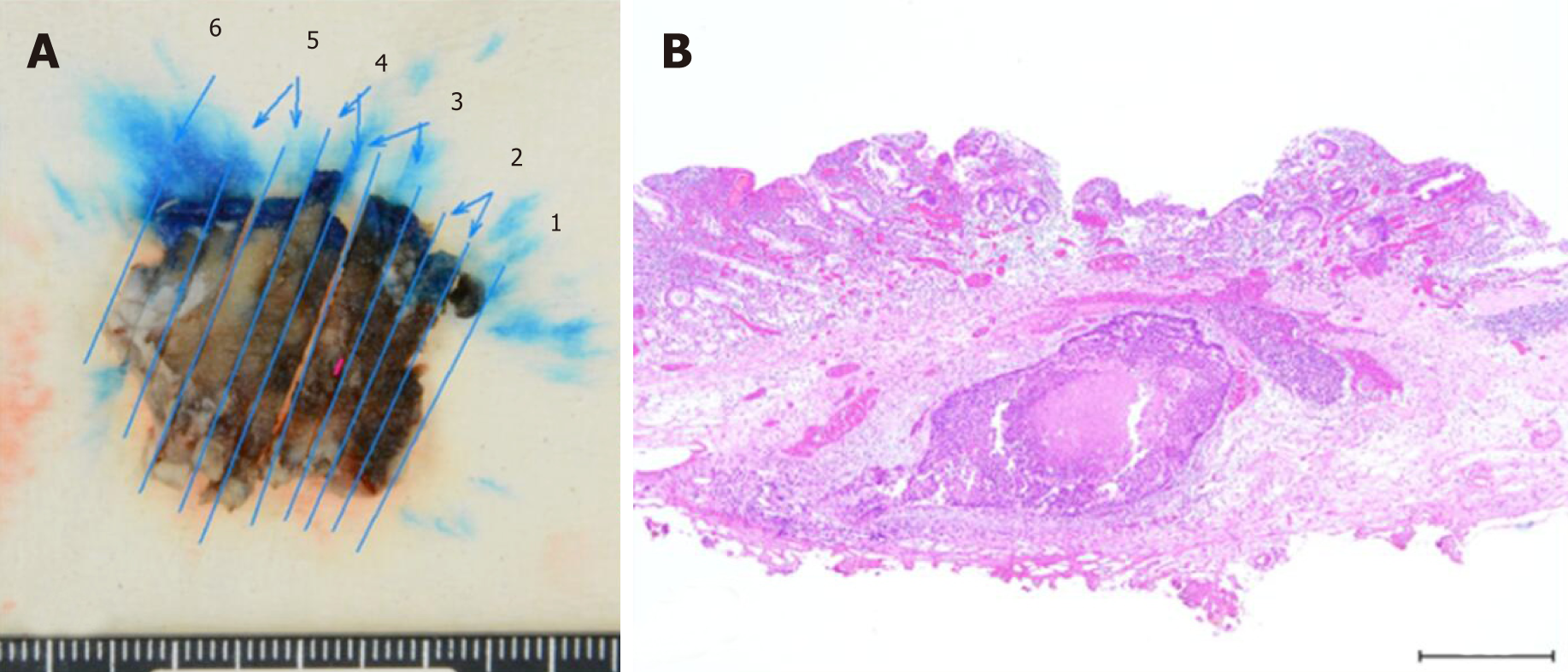
The pathological diagnosis of the specimen was 28 mm × 12 mm, U, type 0-IIc, 1.0 mm × 1.0 mm, well-differentiated tubular adenocarcinoma (tub1), ypT1b (SM), ly0, v0, pHM(-), and pVM(-) in the Japanese Classification of Gastric Cancer (Figure 3A and 3B). After ESD, no recurrence was observed during the 29 mo follow-up period.
To our knowledge, this is the first report describing the efficacy of ESD to prevent local recurrence and help maintain quality of life for a patient with mGC. Effective chemotherapy, followed by complete resection with negative margin using ESD, contributed to a good clinical course.
SOX was an effective and safe chemotherapeutic treatment in our patient’s case. A previous phase III study (G-SOX study) showed that SOX was not inferior to S-1 plus cisplatin therapy (CS) inefficacy[5]. Regarding safety, SOX has shown better tolerability than CS in elderly patients, with a lower frequency of grade 3 or worse adverse events, as well as lower occurrence of increased creatinine levels[6]. In clinical practice, SOX is administered more frequently than CS because of its feasibility.
In this case, the patient achieved a complete response for multiple liver masses, and the primary lesion size decreased from SOX, but it was difficult to continue chemotherapy due to adverse events (i.e., peripheral sensory neuropathy and anorexia). Recently, conversion surgery has been proposed and clinically performed following successful chemotherapy. Some studies showed that a microscopically margin-negative (R0) resection for a primary lesion after a good response to chemotherapy improved survival outcomes for mGC patients[7,8]. Additionally, cytoreductive or volume-reduction surgery has not shown survival benefits in similar patients[9,10]. Sato et al[11] reported a 5-year overall survival (OS) (median survival time of 47.9 mo) of 48.6% in patients with stage IV gastric cancer who had undergone R0 resection after chemotherapy. Additionally, R0 resection led to a significantly longer OS than did R1 (microscopic residual tumor) and R2 (macroscopic residual tumor) resections. Similarly, in patients with stage IV gastric cancer who had a gastrectomy after chemotherapy, OS was significantly longer from R0 resection only (median OS = 19.2 mo)[12].
Based on newly proposed classification categories for stage IV gastric cancer[13], our case was Category 2. Category 2 is indicative of the absence of macroscopic peritoneal dissemination, with marginally resectable metastatic lesions that are oncologically or technically unresectable. Furthermore, the proposed treatment strategy for Category 2 is conversion surgery, if the patient achieves a satisfactory response to chemotherapy. Therefore, our case was theoretically a good candidate for conversion surgery; however, the patient was elderly and had an untreated large abdominal aortic aneurysm. Moreover, the patient was concerned about decreased performance status due to total gastrectomy.
In cases in which the patient cannot undergo surgery and continue intensive chemotherapy, similar to the case of our patient, most patients shift to less-intensive chemotherapy or supportive care. In the current standard chemotherapy, subsequent chemotherapies are not always less-intensive. In clinical practice, some reports state that less intensive monotherapy was conducted for frail patients[14,15]. Nishimura et al[16] reported that irinotecan monotherapy after refractory response to fluoropyrimidine, platinum and taxanes showed modest activity. However, in these reports, even though most patients’ PS were 0-1, their prognoses were poor. For frail patients, if chemotherapy may decrease PS level and worsen prognosis, then supportive care is often chosen as the best alternative. Radiotherapy is one of the therapeutic strategies for these patients to manage localized tumors[17,18]. However, in this case, radiotherapy was not conducted due to comorbidity.
Local tumor progression is a problem in many of these patients. Gastric stenosis, obstruction, gastroparesis, bleeding, and pain are common conditions caused by local recurrence or advanced primary lesions that ultimately decrease a patient’s quality of life. For these cases, there are some available strategies, such as palliative gastrectomy, palliative gastrojejunostomy, or endoscopic stent. In this case, the patient did not suffer from obstruction at the end of chemotherapy. Although biopsy results both during and after chemotherapy were categorized as Group 1, the primary lesion appeared similar to a submucosal tumor. Considering that a lesion sometimes exists at the submucosa like an inverted polyp[19], a residual tumor was suspected. If the residual tumor had remained and grown, there would have been a risk of obstruction. Therefore, ESD was used to first confirm the residual tumor and then resect the lesion completely. The results of this case suggest that when clinically possible, conversion surgery is a better treatment option, because a tumor may remain even without macroscopic evidence of the disease.
ESD is a less-intensive treatment and common practice to resect early gastric cancer, rather than surgical resection[20,21]. ESD enables resection of the whole lesion, thereby allowing a correct histopathological assessment. Furthermore, the procedure is safe and effective in elderly patients. Abe et al[22] reported that the complication rate (bleeding and perforation rates of 3.2% and 2.8%, respectively) of ESD was similar in elderly (≥ 80 years) and non-elderly patients with early gastric cancer, indicating that ESD was a safe procedure, even for the elderly. Additionally, Watanabe et al[23] reported no significant differences in adverse events (i.e., rate of perforation, postoperative bleeding, aspiration pneumonia, or stricture) among patients with early gastric cancer, regardless of age. Several studies reported that endoscopic therapies, such as ESD, for locoregional recurrence of esophageal cancer after definitive chemoradiotherapy ensured safety. Furthermore, endoscopic therapy can be locally controlled and may improve both overall and disease-specific survival rates[24,25]. In the presented case, we achieved local control from the resection using ESD, which may provide therapeutic improvements in both local control and survival outcomes for the patient.
In conclusion, we presented a rare case of a complete resection with negative margins using ESD for a remnant submucosal lesion after chemotherapy for mGC. The patient has been alive for the past 29 mo after ESD, with no sign of local recurrence.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fogli L, Zhu YL, Kim JH S- Editor: Dou Y L- Editor: Filipodia E- Editor: Tan WW
| 1. | Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1575] [Cited by in RCA: 1912] [Article Influence: 239.0] [Reference Citation Analysis (1)] |
| 2. | Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, Aprile G, Kulikov E, Hill J, Lehle M, Rüschoff J, Kang YK; ToGA Trial Investigators. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010;376:687-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5541] [Cited by in RCA: 5305] [Article Influence: 353.7] [Reference Citation Analysis (3)] |
| 3. | Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, Miyashita K, Nishizaki T, Kobayashi O, Takiyama W, Toh Y, Nagaie T, Takagi S, Yamamura Y, Yanaoka K, Orita H, Takeuchi M. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1320] [Cited by in RCA: 1421] [Article Influence: 83.6] [Reference Citation Analysis (0)] |
| 4. | Schildberg CW, Weidinger T, Hohenberger W, Wein A, Langheinrich M, Neurath M, Boxberger F. Metastatic adenocarcinomas of the stomach or esophagogastric junction (UICC stage IV) are not always a palliative situation: a retrospective analysis. World J Surg. 2014;38:419-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Yamada Y, Higuchi K, Nishikawa K, Gotoh M, Fuse N, Sugimoto N, Nishina T, Amagai K, Chin K, Niwa Y, Tsuji A, Imamura H, Tsuda M, Yasui H, Fujii H, Yamaguchi K, Yasui H, Hironaka S, Shimada K, Miwa H, Hamada C, Hyodo I. Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naïve patients with advanced gastric cancer. Ann Oncol. 2015;26:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 398] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 6. | Bando H, Yamada Y, Tanabe S, Nishikawa K, Gotoh M, Sugimoto N, Nishina T, Amagai K, Chin K, Niwa Y, Tsuji A, Imamura H, Tsuda M, Yasui H, Fujii H, Yamaguchi K, Yasui H, Hironaka S, Shimada K, Miwa H, Hamada C, Hyodo I. Efficacy and safety of S-1 and oxaliplatin combination therapy in elderly patients with advanced gastric cancer. Gastric Cancer. 2016;19:919-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Fukuchi M, Ishiguro T, Ogata K, Suzuki O, Kumagai Y, Ishibashi K, Ishida H, Kuwano H, Mochiki E. Prognostic Role of Conversion Surgery for Unresectable Gastric Cancer. Ann Surg Oncol. 2015;22:3618-3624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (2)] |
| 8. | Yamaguchi K, Yoshida K, Tanahashi T, Takahashi T, Matsuhashi N, Tanaka Y, Tanabe K, Ohdan H. The long-term survival of stage IV gastric cancer patients with conversion therapy. Gastric Cancer. 2018;21:315-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 110] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 9. | Fujitani K, Yang HK, Mizusawa J, Kim YW, Terashima M, Han SU, Iwasaki Y, Hyung WJ, Takagane A, Park DJ, Yoshikawa T, Hahn S, Nakamura K, Park CH, Kurokawa Y, Bang YJ, Park BJ, Sasako M, Tsujinaka T; REGATTA study investigators. Gastrectomy plus chemotherapy versus chemotherapy alone for advanced gastric cancer with a single non-curable factor (REGATTA): a phase 3, randomised controlled trial. Lancet Oncol. 2016;17:309-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 534] [Cited by in RCA: 506] [Article Influence: 56.2] [Reference Citation Analysis (0)] |
| 10. | Mahar AL, Coburn NG, Singh S, Law C, Helyer LK. A systematic review of surgery for non-curative gastric cancer. Gastric Cancer. 2012;15 Suppl 1:S125-S137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Sato Y, Ohnuma H, Nobuoka T, Hirakawa M, Sagawa T, Fujikawa K, Takahashi Y, Shinya M, Katsuki S, Takahashi M, Maeda M, Okagawa Y, Naoki U, Kikuch S, Okamoto K, Miyamoto H, Shimada M, Takemasa I, Kato J, Takayama T. Conversion therapy for inoperable advanced gastric cancer patients by docetaxel, cisplatin, and S-1 (DCS) chemotherapy: a multi-institutional retrospective study. Gastric Cancer. 2017;20:517-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Satoh S, Okabe H, Teramukai S, Hasegawa S, Ozaki N, Ueda S, Tsuji A, Sakabayashi S, Fukushima M, Sakai Y. Phase II trial of combined treatment consisting of preoperative S-1 plus cisplatin followed by gastrectomy and postoperative S-1 for stage IV gastric cancer. Gastric Cancer. 2012;15:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Yoshida K, Yamaguchi K, Okumura N, Tanahashi T, Kodera Y. Is conversion therapy possible in stage IV gastric cancer: the proposal of new biological categories of classification. Gastric Cancer. 2016;19:329-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 166] [Cited by in RCA: 243] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 14. | Shirao K, Boku N, Yamada Y, Yamaguchi K, Doi T, Goto M, Nasu J, Denda T, Hamamoto Y, Takashima A, Fukuda H, Ohtsu A; Gastrointestinal Oncology Study Group of the Japan Clinical Oncology Group. Randomized Phase III study of 5-fluorouracil continuous infusion vs. sequential methotrexate and 5-fluorouracil therapy in far advanced gastric cancer with peritoneal metastasis (JCOG0106). Jpn J Clin Oncol. 2013;43:972-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 90] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Muranaka T, Yuki S, Komatsu Y, Sawada K, Harada K, Kawamoto Y, Nakatsumi H, Sakamoto N. Efficacy and Safety of Bolus 5-Fluorouracil and L-Leucovorin as Salvage Chemotherapy for Oral Fluoropyrimidine-Resistant Unresectable or Recurrent Gastric Cancer: A Single Center Experience. J Gastric Cancer. 2016;16:177-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Nishimura T, Iwasa S, Nagashima K, Okita N, Takashima A, Honma Y, Kato K, Hamaguchi T, Yamada Y, Shimada Y, Boku N. Irinotecan monotherapy as third-line treatment for advanced gastric cancer refractory to fluoropyrimidines, platinum, and taxanes. Gastric Cancer. 2017;20:655-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Hashimoto K, Mayahara H, Takashima A, Nakajima TE, Kato K, Hamaguchi T, Ito Y, Yamada Y, Kagami Y, Itami J, Shimada Y. Palliative radiation therapy for hemorrhage of unresectable gastric cancer: a single institute experience. J Cancer Res Clin Oncol. 2009;135:1117-1123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Asakura H, Hashimoto T, Harada H, Mizumoto M, Furutani K, Hasuike N, Matsuoka M, Ono H, Boku N, Nishimura T. Palliative radiotherapy for bleeding from advanced gastric cancer: is a schedule of 30 Gy in 10 fractions adequate? J Cancer Res Clin Oncol. 2011;137:125-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Odashima M, Otaka M, Nanjo H, Jin M, Horikawa Y, Matsuhashi T, Ohba R, Koizumi S, Kinoshita N, Takahashi T, Shima H, Watanabe S. Hamartomatous inverted polyp successfully treated by endoscopic submucosal dissection. Intern Med. 2008;47:259-262. [PubMed] |
| 20. | Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, Ohnita K, Mizuta Y, Shiozawa J, Kohno S. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 470] [Cited by in RCA: 520] [Article Influence: 32.5] [Reference Citation Analysis (1)] |
| 21. | Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225-229. [PubMed] |
| 22. | Abe N, Gotoda T, Hirasawa T, Hoteya S, Ishido K, Ida Y, Imaeda H, Ishii E, Kokawa A, Kusano C, Maehata T, Ono S, Takeuchi H, Sugiyama M, Takahashi S. Multicenter study of the long-term outcomes of endoscopic submucosal dissection for early gastric cancer in patients 80 years of age or older. Gastric Cancer. 2012;15:70-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Watanabe K, Hikichi T, Nakamura J, Takagi T, Suzuki R, Sugimoto M Md, Waragai Y, Kikuchi H, Konno N, Asama H, Takasumi M, Obara K, Ohira H. Endoscopic submucosal dissection for early gastric cancer in very elderly patients age 85 or older. Endosc Int Open. 2017;5:E17-E24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Koizumi S, Jin M, Matsuhashi T, Tawaraya S, Watanabe N, Sawaguchi M, Kanazawa N, Yamada Y, Onochi K, Kimura Y, Ohba R, Kataoka J, Hatakeyma N, Mashima H, Ohnishi H. Salvage endoscopic submucosal dissection for the esophagus-localized recurrence of esophageal squamous cell cancer after definitive chemoradiotherapy. Gastrointest Endosc. 2014;79:348-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Takeuchi M, Kobayashi M, Hashimoto S, Mizuno K, Kawaguchi G, Sasamoto R, Aoyama H, Aoyagi Y. Salvage endoscopic submucosal dissection in patients with local failure after chemoradiotherapy for esophageal squamous cell carcinoma. Scand J Gastroenterol. 2013;48:1095-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |