Published online Feb 6, 2019. doi: 10.12998/wjcc.v7.i3.396
Peer-review started: November 21, 2018
First decision: December 9, 2018
Revised: December 27, 2018
Accepted: January 8, 2019
Article in press: January 8, 2019
Published online: February 6, 2019
Processing time: 69 Days and 1.6 Hours
Cardiac resynchronization therapy (CRT) can be used as an escalated therapy to improve heart function in patients with cardiac dysfunction due to long-term right ventricular pacing. However, guidelines are only targeted at adults. CRT is rarely used in children.
This case aimed to implement biventricular pacing in one child with heart failure who had a left ventricular ejection fraction < 35% at 4 years after implantation of an atrioventricular sequential pacemaker due to atrioventricular block. Postoperatively, echocardiography showed atrial sensing ventricular pacing and QRS wave duration of 120-130 ms, and cardiac function significantly improved after upgrading pacemaker.
Patients whose cardiac function is deteriorated to a level to upgrade to CRT should be upgraded to reverse myocardial remodeling as soon as possible.
Core tip: Current guidelines are based on adults, which do not enroll pediatric patients for recommendation of cardiac resynchronization therapy, making it more difficult to accurately assess its curative effects. Moreover, the physiological characteristics of children cause a higher risk in surgery compared with adults. In January 2015, the Cardiology Department of Guizhou Provincial People's Hospital implemented biventricular pacing for the first time in one child with heart failure due to right ventricular pacing. The cardiac function of the child improved significantly after upgrading the pacemaker.
- Citation: Yu S, Wu Q, Chen BL, An YP, Bu J, Zhou S, Wang YM. Biventricular pacing for treating heart failure in children: A case report and review of the literature. World J Clin Cases 2019; 7(3): 396-404
- URL: https://www.wjgnet.com/2307-8960/full/v7/i3/396.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i3.396
Atrioventricular block is a common bradyarrhythmia in childhood, which can be either congenital or acquired. The congenital atrioventricular block has an incidence of about 1/20000[1-3], and the resulting severe bradycardia not only affects the growth and development of children but also may cause sudden death[4-6]. Implantation of pacemakers is the only long-term, safe, effective measure for treating children with symptomatic atrioventricular block[7,8]. The improvement in pacemaker electrode leads has resulted in increased implantation of endocardial pacemaker electrode leads in children. The right ventricular apex is a common site of pacing due to easy implantation, unlikelihood of dislocation, stable threshold and so on. Pacing can be categorized as right ventricular single-chamber pacing or dual-chamber (right atrial and right ventricular) pacing. If pacemakers are implanted in children at a young age, they have a long-term pacing dependence and require multiple replacements. Therefore, the single-chamber pacing is often preferred. The right ventricular apical pacing alters the synchrony of ventricular activation sequence and cardiac conduction[9,10]. The right ventricular single-chamber pacing and atrioventricular sequential pacing can lead to a decline in cardiac function due to atrioventricular excitation asynchrony and delayed left ventricular contraction[11], resulting in an increased incidence of atrial fibrillation and heart failure[12]. The incidence of cardiac insufficiency in children receiving right ventricular single-chamber pacing is up to 7%-13%[13]. Cardiac resynchronization therapy (CRT) enhances left ventricular pacing on the basis of dual-chamber pacing in the right atrium and right ventricle, thereby restoring cardiac synchrony, improving cardiac function and quality of life, and reducing hospitalization and mortality[14]. However, current guidelines are based on adults, which do not enroll pediatric patients for recommendation of CRT[7,11,15], making it more difficult to accurately assess its curative effects. Moreover, the physiological characteristics of children cause a higher risk in surgery compared with adults. In January 2015, the Cardiology Department of Guizhou Provincial People's Hospital implemented biventricular pacing for the first time in one child with heart failure due to right ventricular pacing. The cardiac function of the child improved significantly after upgrading the pacemaker.
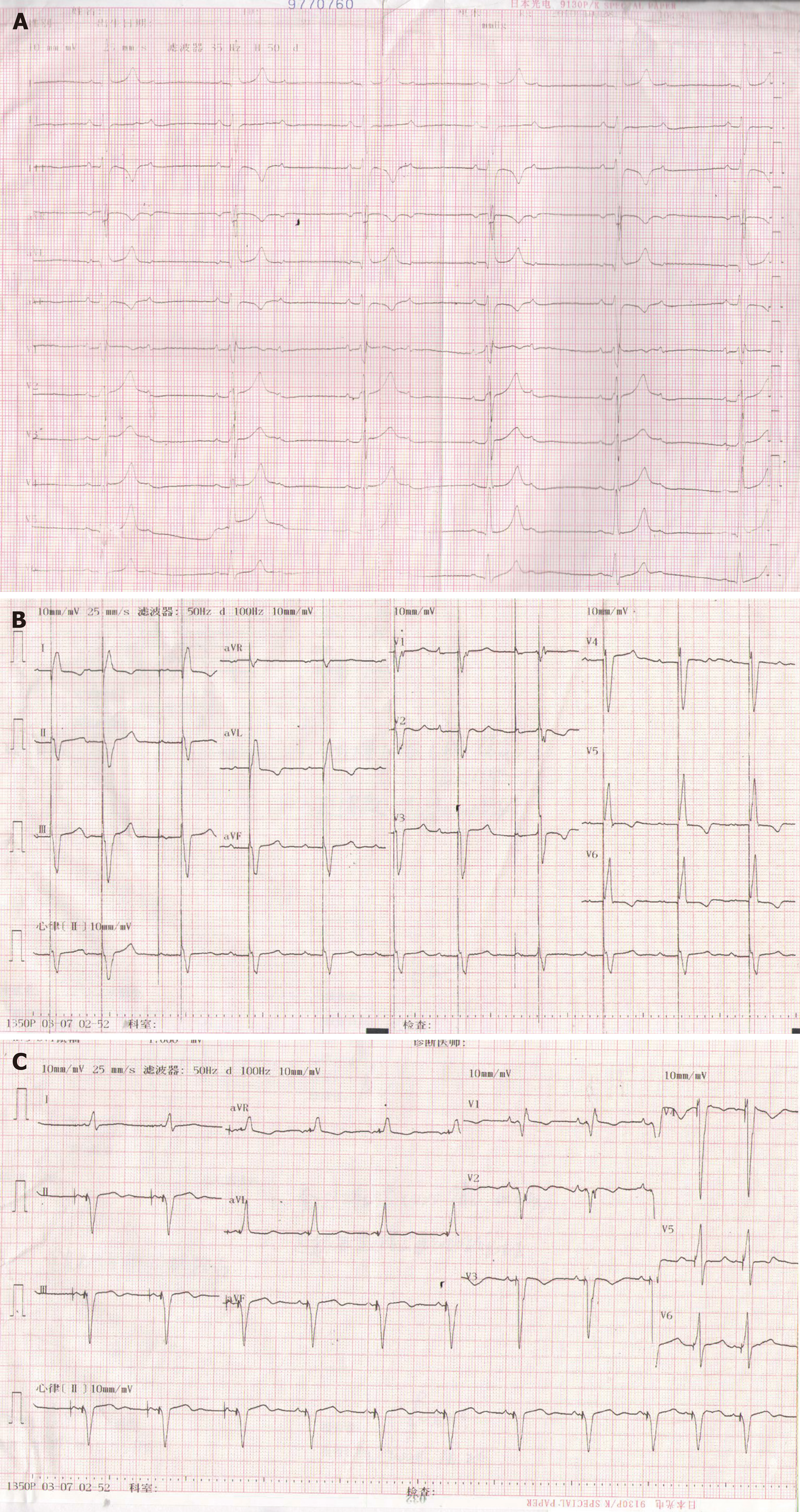
The patient was a 13-year-old boy (full-term birth) with normal development and no family history of genetic diseases or similar heart diseases. Four years ago, examination at admission revealed normal myocardial enzymes and thyroid, liver, and kidney functions. Echocardiography (ECG) showed normal cardiac structure. ECG (Figure 1A) revealed Mobitz II atrioventricular block, with a ventricular escape rate of 45 beats/min. He was not given drug treatment before admission. After admission, the patient was diagnosed as having arrhythmia with Mobitz II atrioventricular block. He was transferred to the Cardiology Department of Guizhou Provincial People's Hospital and implanted with an automatic atrioventricular sequential pacemaker (DDD pacemaker) despite huge risks and complications[16], because he had a history of recurrent syncope. The preoperative ECG showed full pacing rhythm, atrial sensing ventricular pacing, and atrial ventricular sequential pacing, with a QRS wave duration of 150 ms (Figure 1B). The patient was followed for a long time after surgery, during which no dislocation or rupture of the right ventricular electrode was seen. The pacemaker showed good pacing and sensing function, the atrial pacing ratio was 30%-40%, and the ventricular pacing rate was > 80%. Three years after surgery, he experienced chest tightness, fatigue, and other symptoms. ECG showed left atrium 40.0 mm, left ventricle 66.1 mm, moderate mitral and tricuspid regurgitations, and ejection fraction (EF) 32%. The patient was given oral administration of metoprolol 6.25 mg twice a day, digoxin 0.125 mg once a day (qd), furosemide 20 mg qd, spironolactone 20 mg qd, perindopril 2 mg qd, and other intensive medical treatment for 1 year. However, the improvement in cardiac function was not satisfactory, the symptoms still recurred, the ventricle gradually expanded, and the cardiac function progressively declined. The patient was admitted in January 2015 because of implantation of pacemakers for 4 years, fatigue for 1 year, and aggravation for 3 mo. In terms of physical examination at admission, ECG showed left atrium 42.4 mm, left ventricle 71.4 mm, moderate mitral and tricuspid regurgitation, and EF 19%. Programming revealed a right ventricular pacing rate > 99%. Chest X-ray showed a heart–chest ratio of 0.61. B-type brain natriuretic peptide (BNP) was 1023 pg/mL. Blood routine and blood biochemistry did not show obvious abnormalities. Referring to the 2013 ESC guidelines on cardiac pacing and CRT[7] (Referring to relative guidelines[7,8,17]), the patient underwent CRT for treating cardiac insufficiency.
A child with heart failure due to right ventricular pacing.
The left subclavian vein was punctured under local anesthesia, and retrograde coronary vein angiography was performed to reveal the main coronary vein and its branches. The lateral vein was selected as the target vein. A double guidewire (Ruinough, Pilot 50) was inserted at the distal part of the lateral vein and fixed, and then the left ventricular electrode (QUICKFLEXTMμ, 1258T, St. Jude Medical, United States) was delivered to the target vein and fixed using the protection sleeve. The threshold was 1.0 V (pulse width, 0.48 ms) and impedance was 839 Ω. No diaphragmatic stimulation occurred with 10 V pacing. The skin at the original pacemaker was cut open along the inferior part of the left clavicle, and the subcutaneous tissue was bluntly dissected up to the sac. Subsequently, the original right atrial electrode was tested, which showed a threshold of 0.9 V (pulse width, 0.48 ms), sensing of 5.0 mV, and impedance of 520 Ω. For the right ventricular electrode, the testing showed a threshold of 0.6 V (pulse width, 0.48 ms), sensing of 10.0 mV, and impedance of 600 Ω (because the child was pacing dependent, a left ventricular electrode was used for temporary pacing in the process of testing the right ventricular electrode). The lead was connected to the three-chamber pacemaker (FRONTIER II, 5596, St. Jude Medical) and embedded into the original sac. Postoperatively, Quick Optive (SJ) was combined with ECG to optimize the atrioventricular and ventricular intervals. When the atrioventricular interval was 130 ms and the left ventricle was advanced 20 ms, the mitral valve velocity time integral and aorta velocity time integral were the largest, and the QRS wave duration was the narrowest, which was shortened from 150 ms preoperatively to 130 ms (Figure 1C). The present study referred to the standards for adults because, currently, no standards and guidelines exist for pacemaker upgrades in children. Moreover, children are at a rapid stage of growth and development, which makes CRT implantation more difficult.
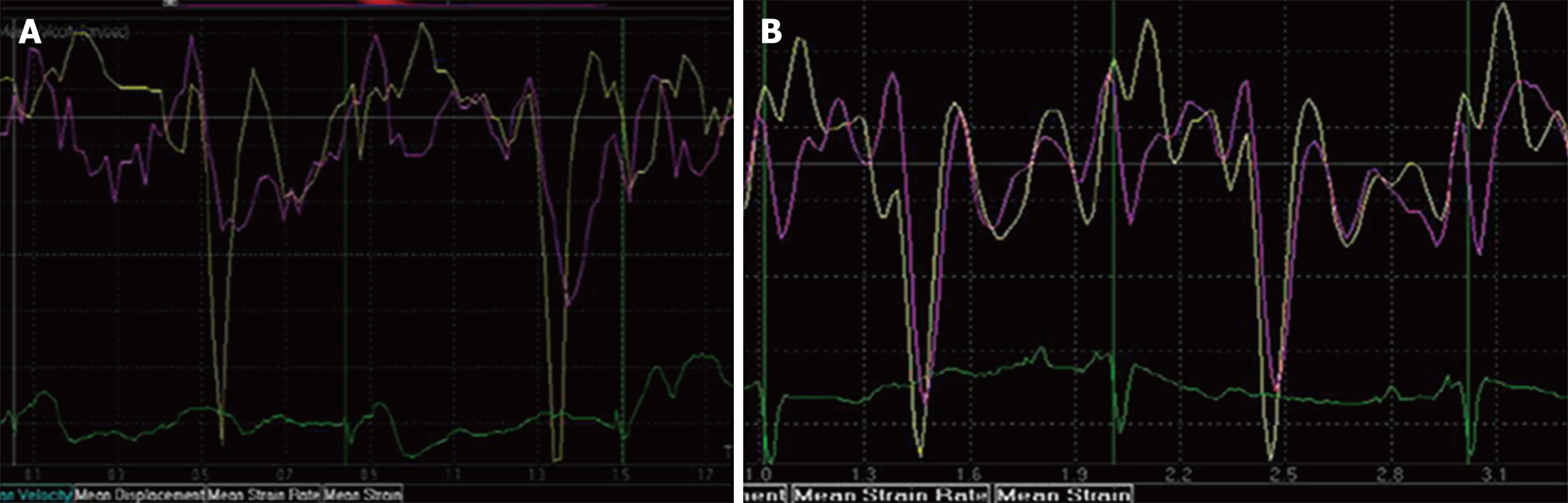
Postoperatively, the patient was regularly followed, during which no cardiac dysfunction or adverse cardiac events occurred. At postoperative 3 and 6 mo, ECG showed atrial sensing ventricular pacing and a QRS wave duration of 120-130 ms. Programming showed that the threshold of the right atrial electrode, right ventricular electrode, and left ventricular electrode was 0.75-1.0, 0.6-0.75, and 0.9-1.0 V (pulse width, 0.48 ms), respectively; the ventricular pacing rate was > 99%; and the atrial pacing rate was 32%. Although chest X-ray showed no significant reduction in the heart-chest ratio compared with that before surgery, ECG revealed the left atrium of 35.6 mm, left ventricle of 55.6 mm, mild mitral and tricuspid regurgitations, and an EF of 49%. Tissue Doppler echocardiography showed a significant improvement in ventricular synchrony compared with preoperative measurements [peak systolic velocity (Ts) and early peak diastolic velocity (Te) of the 12 segments] (Table 1 and Figure 2), and BNP decreased to 126.8 pg/mL. The exercise tolerance increased significantly, and the child could live a normal life and participate in appropriate physical activity, with a New York Heart Association (NYHA) functional class up to II.
| Anteroposterior diameter of left atrium (mm) | Left ventricular end-diastolic dimension (mm) | Left ventricular ejection fraction (%) | Left ventricular systolic peak time | Left ventricular diastolic peak time | |
| Before surgery | 42.4 | 71.4 | 19 | 39.8 | 38.5 |
| Postoperative 1 mo | 41.3 | 66.7 | 28 | 35.9 | 37.6 |
| Postoperative 3 mo | 36.1 | 60.8 | 32 | 32.7 | 35.3 |
| Postoperative 6 mo | 35.6 | 55.6 | 49 | 30.6 | 35.6 |
Right ventricular single-chamber pacing and atrioventricular sequential pacing can lead to a decline in cardiac function due to atrioventricular excitation asynchrony and delayed left ventricular contraction[11]. Hence, the present study used atrioventricular sequential pacing to reduce atrioventricular asynchrony due to single-chamber pacing. The pacing sites at the right ventricular outflow tract, septum, and beside the His bundle and other places were selected to reduce the adverse effects of long-term apical pacing of the right ventricle on the cardiac function in children. Nevertheless, some children still suffered from cardiac dysfunction caused by activation sequence asynchrony in the left ventricle and between the left and right ventricles due to right ventricular pacing[18]. Previous studies have reported that left ventricular pacing through the epicardial pathway can reverse cardiac dysfunction and loss of synchronism with a decline in EF caused by long-term right ventricular pacing, thus achieving better long-term echocardiographic cardiac function indexes compared with the right ventricular pacing[15,19]. However, this procedure requires surgical implantation of epicardial electrodes, which tends to cause a large trauma and a high surgical risk, and therefore is not widely accepted. Meanwhile, using biventricular pacing re-synchrony, CRT can regulate left and right ventricular pacing sequences, reverse left ventricular remodeling, delay the deterioration of cardiac function, and thus reduce hospitalization rate and mortality of heart failure[20]. The guidelines[7,21,22] recommend that patients with an EF < 35%, high ventricular pacing rate, NYHA class III, and ambulant IV should be upgraded to CRT treatment. However, no uniform standard exists for CRT in children; all refer to adult indications. The patient in the present study was first implanted with DDD, in which the right ventricular pacing electrode was placed in the right ventricular septum. However, he presented with progressive exertional dyspnea 3 years after operation, with a gradually increased left ventricular end-diastolic diameter and gradually decreased left ventricular ejection fraction. His symptoms did not improve significantly after receiving intensive medical treatment. Therefore, this case presumed the cause of heart failure in children as follows: (1) the right ventricular pacing leads to the widening of the QRS wave duration (> 120 ms). Consequently, the intraventricular conduction is delayed, the left lateral ventricular wall agitation is later than that of the septum, the agitation is transmitted from the right ventricular myocardium to the left ventricle via the ventricular septum and slowly transmitted in the left ventricular myocardium, and the left ventricular myocardium is changed from overall synchronic contraction to individual myocardial contraction. This ultimately leads to left and right ventricular contraction asynchrony, left intraventricular contraction asynchrony, and asynchrony of left ventricular and left atrial contractions, resulting in reduced effectiveness of left ventricular contraction and cardiac insufficiency[23]; and (2) adverse effects of long-term right ventricular pacing on cardiac function lead to the lack of myocardial perfusion[24], and even varying degrees of apoptosis of myocardial cells. These apoptotic cells are replaced by fibrous connective tissue, which causes a slower conduction velocity than normal myocardium and manifests as electrical and mechanical asynchrony in the heart, further aggravating the heart failure[25,26]. For the child in the present study, the cardiac function did not improve after intensive medical treatment, the left ventricular end diastolic diameter expanded progressively, and EF continued to decline. Referring to the adult guidelines, on the basis of right atrial and right ventricular sequential pacing, the left ventricular electrode was implanted into the lateral vein via the coronary sinus to restore the atrioventricular, left and right ventricular, and left intraventricular synchronicity; shorten QRS wave duration; and improve the child's heart function. After nearly a year of follow-up, the child’s exercise tolerance increased significantly, and EF values were close to the normal level.
In conclusion, CRT decreases to a IIb-type indication in patients with heart failure who experience worsening of symptoms following conventional pacemakers and a high rate of right ventricular pacing in the 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[27]. However, in the present study, the cardiac function recovered well after CRT, and the therapeutic effect was satisfactory. This might be because that the QRS duration was significantly widened after right ventricular pacing and presented as a “complete left bundle branch block[28,29].” The widening of the QRS wave was a sign of ventricular contraction asynchrony, and the worse the left ventricular asynchrony, the wider the QRS wave duration[30]. On the basis of solving atrioventricular asynchrony by DDD, CRT further restored the synchrony in the left ventricle and between the left and right ventricles, shortened QRS wave duration, and thus benefitted the cardiac function in the child. The cardiac function, QRS wave duration, and ECG of patients dependent on right ventricular pacing should be closely observed during follow-up. Patients whose cardiac function is deteriorated to a level that meets the criteria to upgrade to CRT should be upgraded to reverse myocardial remodeling as soon as possible.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sanchez-Beato M, Schievenbusch S, Czubkowski P S- Editor: Dou Y L- Editor: Wang TQ E- Editor: Song H
| 1. | Friedman RA, Fenrich AL, Kertesz NJ. Congenital complete atrioventricular block. Pacing Clin Electrophysiol. 2001;24:1681-1688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Michaelsson M, Riesenfeld T, Jonzon A. Natural history of congenital complete atrioventricular block. Pacing Clin Electrophysiol. 1997;20:2098-2101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 65] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Jaeggi E, Laskin C, Hamilton R, Kingdom J, Silverman E. The importance of the level of maternal anti-Ro/SSA antibodies as a prognostic marker of the development of cardiac neonatal lupus erythematosus a prospective study of 186 antibody-exposed fetuses and infants. J Am Coll Cardiol. 2010;55:2778-2784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 168] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 4. | Ho A, Gordon P, Rosenthal E, Simpson J, Miller O, Sharland G. Isolated Complete Heart Block in the Fetus. Am J Cardiol. 2015;116:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Jaeggi ET, Hamilton RM, Silverman ED, Zamora SA, Hornberger LK. Outcome of children with fetal, neonatal or childhood diagnosis of isolated congenital atrioventricular block. A single institution's experience of 30 years. J Am Coll Cardiol. 2002;39:130-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 259] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 6. | Udink ten Cate FE, Breur JM, Cohen MI, Boramanand N, Kapusta L, Crosson JE, Brenner JI, Lubbers LJ, Friedman AH, Vetter VL, Meijboom EJ. Dilated cardiomyopathy in isolated congenital complete atrioventricular block: early and long-term risk in children. J Am Coll Cardiol. 2001;37:1129-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 124] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 7. | Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, Cleland J, Deharo JC, Delgado V, Elliott PM, Gorenek B, Israel CW, Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA). 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013;15:1070-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 722] [Cited by in RCA: 764] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 8. | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147-e239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4116] [Cited by in RCA: 4653] [Article Influence: 387.8] [Reference Citation Analysis (1)] |
| 9. | Auger D, Hoke U, Marsan NA, Tops LF, Leong DP, Bertini M, Schalij MJ, Bax JJ, Delgado V. Effect of induced LV dyssynchrony by right ventricular apical pacing on all-cause mortality and heart failure hospitalization rates at long-term follow-up. J Cardiovasc Electrophysiol. 2014;25:631-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Zou C, Song J, Li H, Huang X, Liu Y, Zhao C, Shi X, Yang X. Right ventricular outflow tract septal pacing is superior to right ventricular apical pacing. J Am Heart Assoc. 2015;4:e001777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Dubin AM, Collins KK, Hare GFV, Reddy VM, Hanisch D, Chiesa N, Rosenthal DN. Abstract 2974: Midterm Results Of Resynchronization Therapy In Pediatrics: Do We Need New Guidelines? Circulation. 2018;116:II(664). |
| 12. | Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL, Lamas GA; MOde Selection Trial Investigators. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2003;107:2932-2937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1195] [Cited by in RCA: 1216] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 13. | Curtis AB, Worley SJ, Adamson PB, Chung ES, Niazi I, Sherfesee L, Shinn T, Sutton MS; Biventricular versus Right Ventricular Pacing in Heart Failure Patients with Atrioventricular Block (BLOCK HF) Trial Investigators. Biventricular pacing for atrioventricular block and systolic dysfunction. N Engl J Med. 2013;368:1585-1593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 520] [Cited by in RCA: 589] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 14. | Dickstein K, Vardas PE, Auricchio A, Daubert JC, Linde C, McMurray J, Ponikowski P, Priori SG, Sutton R, van Veldhuisen DJ; ESC Committee for Practice Guidelines. 2010 Focused Update of ESC Guidelines on device therapy in heart failure: an update of the 2008 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC Guidelines for cardiac and resynchronization therapy. Developed with the special contribution of the Heart Failure Association and the European Heart Rhythm Association. Europace. 2010;12:1526-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 118] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 15. | Tomaske M, Breithardt OA, Balmer C, Bauersfeld U. Successful cardiac resynchronization with single-site left ventricular pacing in children. Int J Cardiol. 2009;136:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Berul CI, Cecchin F; American Heart Association; American College of Cardiology. Indications and techniques of pediatric cardiac pacing. Expert Rev Cardiovasc Ther. 2003;1:165-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10348] [Cited by in RCA: 9348] [Article Influence: 1038.7] [Reference Citation Analysis (3)] |
| 18. | Janoušek J, van Geldorp IE, Krupičková S, Rosenthal E, Nugent K, Tomaske M, Früh A, Elders J, Hiippala A, Kerst G, Gebauer RA, Kubuš P, Frias P, Gabbarini F, Clur SA, Nagel B, Ganame J, Papagiannis J, Marek J, Tisma-Dupanovic S, Tsao S, Nürnberg JH, Wren C, Friedberg M, de Guillebon M, Volaufova J, Prinzen FW, Delhaas T; Working Group for Cardiac Dysrhythmias and Electrophysiology of the Association for European Pediatric Cardiology. Permanent cardiac pacing in children: choosing the optimal pacing site: a multicenter study. Circulation. 2013;127:613-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 19. | van Geldorp IE, Delhaas T, Gebauer RA, Frias P, Tomaske M, Friedberg MK, Tisma-Dupanovic S, Elders J, Früh A, Gabbarini F, Kubus P, Illikova V, Tsao S, Blank AC, Hiippala A, Sluysmans T, Karpawich P, Clur SA, Ganame X, Collins KK, Dann G, Thambo JB, Trigo C, Nagel B, Papagiannis J, Rackowitz A, Marek J, Nürnberg JH, Vanagt WY, Prinzen FW, Janousek J; Working Group for Cardiac Dysrhythmias and Electrophysiology of the Association for European Paediatric Cardiology. Impact of the permanent ventricular pacing site on left ventricular function in children: a retrospective multicentre survey. Heart. 2011;97:2051-2055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4673] [Cited by in RCA: 4548] [Article Influence: 227.4] [Reference Citation Analysis (0)] |
| 21. | Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, Cleland J, Deharo JC, Delgado V, Elliott PM, Gorenek B, Israel CW, Leclercq C, Linde C, Mont L, Padeletti L, Sutton R, Vardas PE, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Kirchhof P, Blomstrom-Lundqvist C, Badano LP, Aliyev F, Bänsch D, Baumgartner H, Bsata W, Buser P, Charron P, Daubert JC, Dobreanu D, Faerestrand S, Hasdai D, Hoes AW, Le Heuzey JY, Mavrakis H, McDonagh T, Merino JL, Nawar MM, Nielsen JC, Pieske B, Poposka L, Ruschitzka F, Tendera M, Van Gelder IC, Wilson CM; ESC Committee for Practice Guidelines (CPG) ; Document Reviewers. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013;34:2281-2329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1437] [Cited by in RCA: 1473] [Article Influence: 122.8] [Reference Citation Analysis (0)] |
| 22. | Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA, Ferguson TB, Hammill SC, Karasik PE, Link MS, Marine JE, Schoenfeld MH, Shanker AJ, Silka MJ, Stevenson LW, Stevenson WG, Varosy PD; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Heart Rhythm Society. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2013;61:e6-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 575] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 23. | Stevenson WG, Hernandez AF, Carson PE, Fang JC, Katz SD, Spertus JA, Sweitzer NK, Tang WH, Albert NM, Butler J, Westlake Canary CA, Collins SP, Colvin-Adams M, Ezekowitz JA, Givertz MM, Hershberger RE, Rogers JG, Teerlink JR, Walsh MN, Stough WG, Starling RC; Heart Failure Society of America Guideline Committee. Indications for cardiac resynchronization therapy: 2011 update from the Heart Failure Society of America Guideline Committee. J Card Fail. 2012;18:94-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 24. | Ten Cate TJ, Van Hemel NM, Verzijlbergen JF. Myocardial perfusion defects in right ventricular apical pacing are caused by partial volume effects because of wall motion abnormalities: a new model to study gated myocardial SPECT with the pacemaker on and off. Nucl Med Commun. 2009;30:480-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Thambo JB, Bordachar P, Garrigue S, Lafitte S, Sanders P, Reuter S, Girardot R, Crepin D, Reant P, Roudaut R, Jaïs P, Haïssaguerre M, Clementy J, Jimenez M. Detrimental ventricular remodeling in patients with congenital complete heart block and chronic right ventricular apical pacing. Circulation. 2004;110:3766-3772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 357] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 26. | Gebauer RA, Tomek V, Salameh A, Marek J, Chaloupecký V, Gebauer R, Matejka T, Vojtovic P, Janousek J. Predictors of left ventricular remodelling and failure in right ventricular pacing in the young. Eur Heart J. 2009;30:1097-1104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 84] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 27. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members; Document Reviewers. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4368] [Cited by in RCA: 4914] [Article Influence: 546.0] [Reference Citation Analysis (4)] |
| 28. | Lee KH, Cho JG, Park HW, Yoon NS, Kim SS, Kim MR, Kim MC, Cho KH, Kim HK, Kim CH, Kim KH, Jun SJ, Kim WJ, Lee KJ, Jeong HC, Cho JY, Park KH, Sim Ds, Yoon HJ, Kim KH, Hong YJ, Kim JH, Ahn Y, Jeong MH, Park JC. QRS morphology and ventricular dyssynchrony in patients with chronic right ventricular pacing. Int J Cardiol. 2014;176:962-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Sohn J, Lee YS, Park HS, Han S, Kim YN. Predictors of an adverse clinical outcome in patients with long-term right ventricular apical pacing. J Cardiol. 2017;70:420-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Bryant AR, Wilton SB, Lai MP, Exner DV. Association between QRS duration and outcome with cardiac resynchronization therapy: a systematic review and meta-analysis. J Electrocardiol. 2013;46:147-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |