Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4414
Peer-review started: September 24, 2019
First decision: November 11, 2019
Revised: November 26, 2019
Accepted: November 30, 2019
Article in press: November 30, 2019
Published online: December 26, 2019
Processing time: 92 Days and 6 Hours
Macro-aspartate aminotransferase (AST), a macroenzyme, is a high-molecular mass complex formed by self-polymerization or association with other serum components that are difficult for the kidney to clear, leading to the isolated elevation of serum AST activity. Cases of macro-AST formation are rare, with only 3 published in the English language literature up to September 2019 in China. In this paper, we present a case in which an asymptomatic woman with persistent isolated elevated AST was confirmed as having macro-AST by the polyethylene glycol precipitation method.
A 34-year-old woman was referred to our clinic for elevated AST levels with normal levels of other liver-associated enzymes on November 12, 2018. Her AST level of liver function test had been abnormal for 7 mo before she came to the clinic. The patient was asymptomatic with a normal physical examination. There was no relevant family history and no alcohol consumption or smoking. She had a several-month history of traditional Chinese medical taking and had stopped it 1 year prior. The laboratory tests in our clinic showed only the elevation of AST (89.5 U/L) with no other significant abnormalities. We performed the precipitation technique with polyethylene glycol to confirm the presence of macro-AST. Then for almost a year, her AST level still fluctuated in the abnormal range.
This case highlights that clinical physicians should be familiar with this rare condition of persistent isolated AST elevation due to the presence of macro-AST to avoid unnecessary investigation and patient anxiety.
Core tip: Here, we present a case in which an asymptomatic woman with persistent isolated elevated aspartate aminotransferase was diagnosed as having macro-aspartate aminotransferase, which was confirmed by the polyethylene glycol method; only 3 such cases have been published in the English language literature up to September 2019 in China. It is necessary for physicians to be sufficiently familiar with this condition to avoid repeated unnecessary check-ups.
- Citation: Zhan MR, Liu X, Zhang MY, Niu JQ. Isolated elevated aspartate aminotransferase in an asymptomatic woman due to macro-aspartate aminotransferase: A case report. World J Clin Cases 2019; 7(24): 4414-4419
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4414.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4414
The elevation of liver enzymes is usually associated with liver injury, and both elevated aspartate aminotransferase (AST) and alanine aminotransferase are observed in most situations. However, the isolated elevation of AST with an unexplained cause can be found in some rare instances. At such cases time, the presence of macro-AST should be the one of suspected diagnoses. Macro-AST is a high molecular mass complex formed by AST with immunoglobulin or other plasma components[1]. As a benign etiology of isolated AST elevation, it is often ignored in clinical practice, leading to costly, unnecessary, or even invasive tests before diagnosis. Macro-AST can be detected by gel filtration chromatography, ultracentrifugation and precipitation with polyethylene glycol (PEG) or simply storage at 4 °C[2]. Here, we report a woman in China with persistent isolated elevated AST due to the presence of macro-AST.
A 34-year-old previously healthy woman was referred to our clinic with isolated elevated AST but had no symptoms on November 12, 2018.
The patient was an infertile woman who found her liver function abnormal after a health examination for in vitro fertilization 7 mo before she came to our clinic. The liver function indicated that the only abnormal result was isolated elevated AST ranging from 76.2 to 170 U/L (reference range 13-35 U/L) with other liver-associated enzymes at normal levels during the past 7 mo. She had taken liver protection drugs intermittently but they had no effect.
The patient had no significant medical history.
She had a history of taking traditional Chinese medical for her infertility but had stopped 1 year prior. There was no relevant family history or alcohol consumption.
The physical examination of the patient showed no significant abnormality.
The laboratory tests showed only the elevation of AST (89.5 U/L), with normal levels of the other liver function tests and enzymes: Alanine aminotransferase: 16.1 U/L (7.0-40.0), alkaline phosphatase 47.6 U/L (35.0-100.0), γ-glutamyl transpeptidase 12.6 U/L (7.0-45.0), bilirubin 9.4 μmol/ (6.8-30.0), and total protein 74.9 g/L (65.0-85.0). Serologic testing for viruses was negative and just anti-hepatitis B surface antibody was positive, with a titer of 1300.973 IU/L (the patient had been vaccinated against hepatitis B 3 years prior). Regarding the autoimmune aspect, we did not find significant changes. Her ceruloplasmin, iron concentrations, and thyroid function test were also normal. The details and other laboratory data are shown in Table 1.
| Parameter | Result (normal range) | Parameter | Result (normal range) |
| AST in U/L | 89.5 (13.0-35.0) | WBC as × 109/L | 4.49 (3.5-9.5) |
| ALT in U/L | 16.1 (7.0-40.0) | RBC as × 109/L | 4.22 (3.8-5.10) |
| GGT in IU/L | 12.6 (7.0-45.0) | Hemoglobin in g/L | 123 (115-150) |
| ALP in IU/L | 47.6 (35.0-100.0) | Platelets as × 109/L | 187 (125-350) |
| ACHE in IU/L | 7194 (4300-12000) | Neutrophils as × 109/L | 2.69 (1.80-6.30) |
| TP in g/L | 74.9 (65.0-85.0) | Lymphocytes as × 109/L | 1.41 (1.10-3.20) |
| ALB in g/L | 44.9 (40.0-55.0) | Monocytes as × 109/L | 0.32 (0.10-0.60) |
| GLB in g/L | 30.0 (20.0-40.0) | ||
| TBIL in μmol/L | 9.4 (6.8-30.0) | ||
| DBIL in μmol/L | 2.8 (0.0-8.6) | CHOL in mmol/L | 4.39 (2.6-6.0) |
| IBIL in μmol/L | 6.6 (5.1-21.4) | TG in mmol/L | 0.62 (0.28-1.80) |
| Enzyme parameter | |||
| CK in U/L | 67 (40-200) | Virology test | |
| CKMB in U/L | 7.2 (0.0-25) | Anti-HAV-IgM | - (-) |
| LDH in U/L | 161 (120-250) | Anti-HEV-IgM | - (-) |
| α-HBDH in U/L | 116 (78.0-182.0) | HBsAg | - (-) |
| MAO in U/L | 3.4 (0.0-12.0) | Anti-HBsAb | + (-) |
| AFU in U/L | 21 (3.0-40.0) | HBeAg | - (-) |
| AMY in U/L | 90 (1-135) | Anti-HBeAb | - (-) |
| LPS in U/L | 46 (5.6-51.3) | Anti-HBcAb | - (-) |
| Anti-HCV | - (-) | ||
| Immunological test | Anti-HIV | - (-) | |
| Anti-dsDNA | - (-) | Anti-TP | - (-) |
| Anti-M2 | - (-) | ||
| Anti-gp210 | - (-) | ||
| Anti-SP100 | - (-) | Liver metabolism test | |
| Anti-SSA-52/Ro52 | - (-) | CER in g/L | 0.28 (0.2-0.6) |
| Anti-Sm | - (-) | SI in μmol/L | 15.6 (7.8-32.2) |
| Anti-nRNP/Sm | - (-) | SF in μmol/L | 43.5 (10-120.0) |
| Anti-LKM | - (-) | TIBC in μg/L | 62.0 (50.0-70.0) |
| Immunoglobulin A in g/L | 2.60 (0.7-4.0) | ||
| Immunoglobulin G in g/L | 15.1 (7.0-16.0) | ||
| Immunoglobulin M in g/L | 0.90 (0.4-2.3) | ||
| Complement C3 in g/L | 1.31 (0.9-1.8) |
The abdominal ultrasonography showed mild cholecystitis.
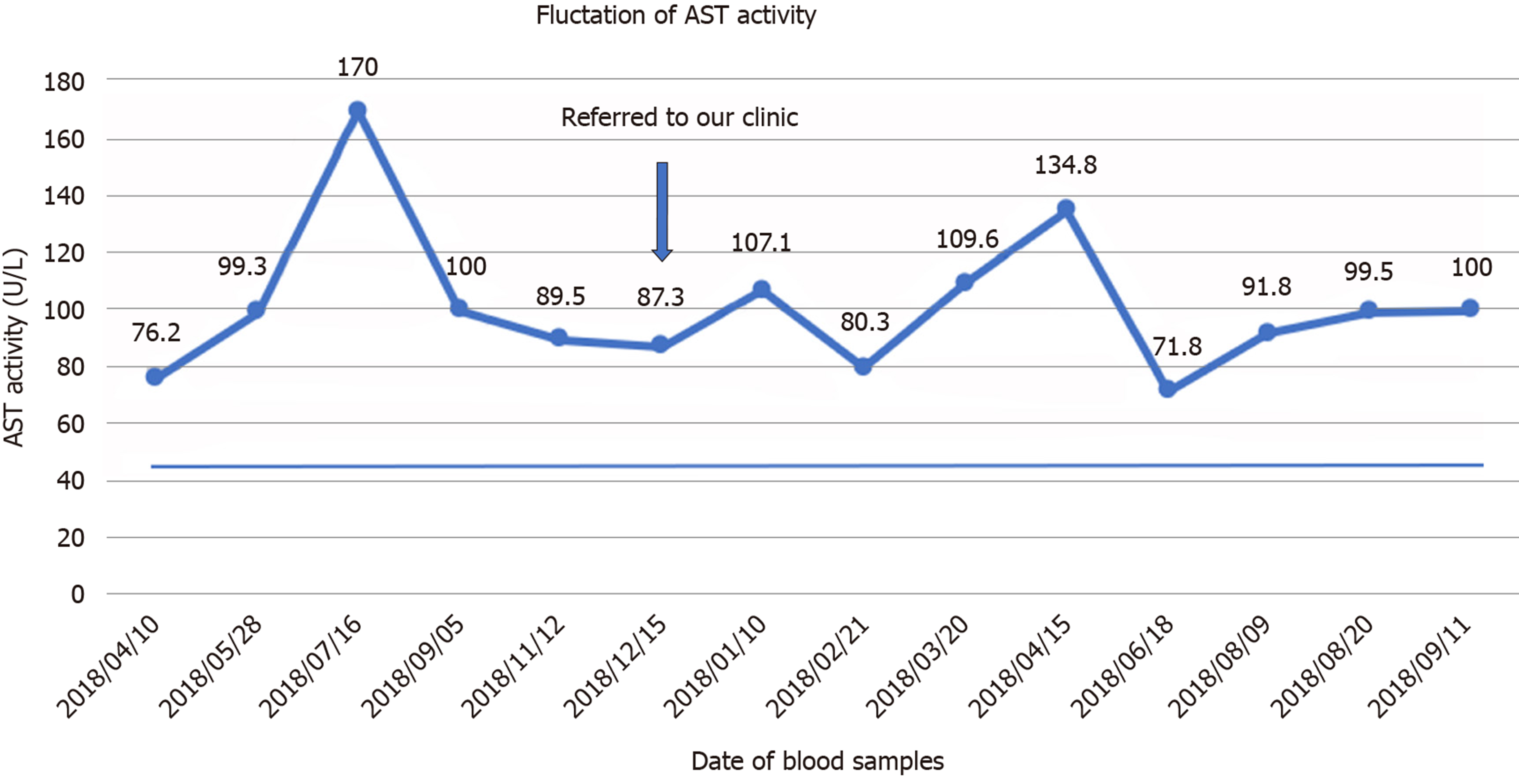
We told the patient to stop taking so-called “liver protectors” and undergo regular reexaminations. During the following 7 mo, there was still a persistent elevation of AST (Figure 1), with normal values for the other liver function tests. Because of the lack of symptoms and lack of evidence of underlying causes such as liver, muscle, or cardiac disease, we suspected the diagnosis of macro-AST formation.
Hence, we decided to confirm the presence of macro-AST in our hospital laboratory by measuring whether AST activity decreased in the sample after PEG precipitation. For the study, we requested a new sample from the patient and used two serum samples from other patients with elevated AST as controls. We conducted the precipitation with PEG following a previously described method[3,4]. The activity of AST dropped sharply to 1.4 U/L after the process (Table 2). After 2 mo, the patient had a reexamination of her liver function, which showed that the AST was still abnormal.
| AST origin | AST DIL1/2 | AST PEG | PPA (%) | AST recovery (%) | |
| Patient | 71.8 | 38.9 | 1.4 | 96.4 | 3.60 |
| Control 1 | 229 | 121.7 | 49.8 | 59.1 | 40.9 |
| Control 2 | 68 | 31 | 17.7 | 42.9 | 57.1 |
According to these results, we concluded that the isolated elevation of AST was most likely due to the presence of macro-AST.
There is no specific treatment for the patient because macro-AST is generally a benign condition.
The patient remained healthy without any abnormalities, except for the isolated elevated AST.
Macroenzymes are serum high molecular weight compounds formed by complexes of enzymes and their polymerization products. The enzymes are usually linked to immunoglobulins (mainly Ig G and Ig M) or other plasma components, which make their clearance slower and more difficult via urine, and ultimately lead to higher levels of their activity[3,5]. Macro-AST is one type of macroenzyme, which was first reported by Konttinen in 1978 in two healthy women[6]. This gradually led to the recognition that macro-AST may be one of the causes of elevated serum AST levels.
Macro-AST is rare, and the exact prevalence rate in the general population is unknown. There have been reports that the prevalence rate of macro-AST was 0.014% in 7273 patients who visited one hospital, while the prevalence was 9.09% in patients with isolated increased AST activity without liver abnormalities[4]. In addition, macro-AST seems to be more common in female patients < 60-years-old[7,8], which is also a high-risk group for autoimmune diseases. As described in the previous literature, the mechanism of the immune complex formation may be due to autoimmunity. The immune reaction or the dysregulation of immune tolerance seems to be associated with immune complex formation[9].
To the best of our knowledge, there are very few reports on macro-AST in China. Our patient is a female of child-bearing age who belongs to a high-risk group[8]. The increased serum activities of AST usually result from liver, heart, skeletal muscle, and erythrocyte injury. Our patient had no evidence of hepatic disease, skeletal muscle disorders, myocardial disease, or hemolysis according to the evaluations with abdominal imaging studies and laboratory examinations. Therefore, after a literature review, the presence of benign macroenzymes became suspected in the absence of organ-specific disease. Ultimately, we performed an experiment with PEG that clearly demonstrated the presence of macro-AST. Prior to being referred to our clinic, our patient underwent many repeated check-ups and was even advised to undergo a liver biopsy because elevated AST was observed. Moreover, she had been treated with various liver protective drugs that had no effect on her. She experienced significant psychological stress.
To date, whether macro-AST is related to disease is unsure and has attracted much attention. Although it has been reported that macroenzymes have been associated with various conditions, such as rheumatoid arthritis or other autoimmune conditions, allergen injection immunotherapy, monoclonal gammopathy, and chronic hepatitis C or possibly resolved acute hepatitis C[10], the majority of reported cases are asymptomatic. There is a report that the AST activity of a young woman with macro-AST for 12 years fluctuated between 163 and 500 U/L but she still remained healthy[8]. In addition, there have been 3 cases of macro-AST patients reported in China who remained healthy after 2-7 years of follow-up[11]. Two studies in children with macro-AST showed that all children remained healthy during long-term follow-up[12], and these studies have shown that macro-AST is a benign condition that needs no further work-up. In addition, a study showed that familial isolated elevated AST may be associated with a heterozygous mutation in glutamate oxaloacetate transaminase 1[13].
Macro-AST can be detected by multiple methods; the most common are precipitating the complexes of macroenzymes with PEG or simply storing the sample at 4 ºC, which is convenient and economical, although two cases reported by Chtioui et al[14] in 2010 and Maan et al[15] in 2017 showed no significant decrease in AST levels after 1 wk of being stored at 4 ºC. Ultracentrifugation and gel filtration chromatography, which constitute the standard reference method, require highly specialized chromatography, are complex and relatively expensive and are not available in most clinical laboratories. In the samples from our patient, we performed a precipitation technique with PEG to confirm the presence of macro-AST. After the patient’s serum was treated with PEG, immunoglobulins precipitated out, revealing the lower free AST concentration. PEG precipitation confirmed the presence of macro-AST with 96.4% polyethylene glycol precipitable activity, which was significantly greater than in the controls.
In conclusion, although macro-AST is rare, clinicians and laboratories should consider macro-AST as a cause of unexplained isolated AST elevations if the patients are asymptomatic and other diseases causing an increase in AST have been excluded. A high index of suspicion may help reduce costs and patient anxiety before performing additional tests.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sirin G, Tajiri K S-Editor: Zhang L L-Editor: Filipodia E-Editor: Liu JH
| 1. | Briani C, Zaninotto M, Forni M, Burra P. Macroenzymes: too often overlooked. J Hepatol. 2003;38:119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Davidson DF, Watson DJ. Macroenzyme detection by polyethylene glycol precipitation. Ann Clin Biochem. 2003;40:514-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | González Raya A, Coca Zúñiga R, Martín Salido E. Isolated elevation of aspartate aminotransferase (AST) in an asymptomatic patient due to macro-AST. J Clin Lab Anal. 2019;33:e22690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Patteet L, Simoens M, Piqueur M, Wauters A. Laboratory detection of macro-aspartate aminotransferase: case report and evaluation of the PEG-precipitation method. Clin Biochem. 2012;45:691-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Luk KHK, Hui YT, Lam JTW, Lai KY. Macro-aspartate aminotransferase is a possible cause of persistent isolated elevated aspartate aminotransferase level. Hong Kong Med J. 2019;25:337-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Konttinen A, Murros J, Ojala K, Salaspuro M, Somer H, Räsänen J. A new cause of increased serum aspartate aminotransferase activity. Clin Chim Acta. 1978;84:145-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Mrosewski I, Bredlau B, Öztürk Y, Switkowski R. Persistent Isolated Elevation of Aspartate Aminotransferase in an Asymptomatic Female Patient: a Case Report and Review of Current Literature. Clin Lab. 2019;65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Orlando R, Carbone A, Lirussi F. Macro-aspartate aminotransferase (macro-AST). A 12-year follow-up study in a young female. Eur J Gastroenterol Hepatol. 2003;15:1371-1373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Triester SL, Douglas DD. Development of macro-aspartate aminotransferase in a patient undergoing specific allergen injection immunotherapy. Am J Gastroenterol. 2005;100:243-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Lee M, Vajro P, Keeffe EB. Isolated aspartate aminotransferase elevation: think macro-AST. Dig Dis Sci. 2011;56:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Yu Z, Wang Y, Feng L, Jia J. Macro-aspartate aminotransferase: two-year follow-up of three patients in China. Dig Dis Sci. 2014;59:224-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Caropreso M, Fortunato G, Lenta S, Palmieri D, Esposito M, Vitale DF, Iorio R, Vajro P. Prevalence and long-term course of macro-aspartate aminotransferase in children. J Pediatr. 2009;154:744-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Kulecka M, Wierzbicka A, Paziewska A, Mikula M, Habior A, Janczyk W, Dabrowska M, Karczmarski J, Lazniewski M, Ginalski K, Czlonkowska A, Socha P, Ostrowski J. A heterozygous mutation in GOT1 is associated with familial macro-aspartate aminotransferase. J Hepatol. 2017;67:1026-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Chtioui H, Mauerhofer O, Günther B, Dufour JF. Macro-AST in an asymptomatic young patient. Ann Hepatol. 2010;9:93-95. [PubMed] |
| 15. | Maan W, Warsi AQ, Rashed A, Karjoo M. Unexplained High Activity of Aspartate Aminotransferase in an Asymptomatic Pediatric Patient. Int J Pediatr. 2017;5:5805-5808. [DOI] [Full Text] |