Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4321
Peer-review started: August 17, 2019
First decision: September 23, 2019
Revised: October 17, 2019
Accepted: November 15, 2019
Article in press: November 15, 2019
Published online: December 26, 2019
Processing time: 130 Days and 6.3 Hours
The brown tumor is a kind of complication of hyperparathyroidism (HPT). The ultimate therapy usually is the resolution of HPT. We herein report an unlocatable HPT patient who received resection of a huge brown tumor of the rib, and experienced “self-recovery” of serum calcium and parathyroid hormone.
A 34-year-old female patient who suffered from a gradually increasing mass of the left chest wall since 2007 came to our hospital for treatment. The patient had a history of serum Ca and parathyroid hormone (PTH) increasing since June 2015 and received zoledronic acid treatment for 17 mo. When she came to our hospital in November 2017 after discontinuing medical treatment for 3 mo, the serum Ca and PTH levels were within normal ranges. The patient had no imaging abnormalities of parathyroid ultrasound or 99mTc-methoxyisobutyl isonitrile. Enhanced computed tomography revealed a local soft tissue mass of 96 mm × 113 mm with bone erosion of the left 8th rib, and the mass presented irregular enhancement with an unclear boundary between the mass and spleen. The mass was thought to likely be caused by HPT, but a malignancy could not be ruled out. Resection of the mass was performed, and the pathology proved that the mass was a brown tumor. A diagnosis of unlocatable HPT was considered. Since the serum Ca and PTH levels were both normal pre- and post-operation, the patient did not receive exploratory surgery for HPT, and received regular follow-up.
The huge brown tumor of the rib and “self-recovered” serum PTH and Ca levels are relatively rare in HPT patients. An exploratory operation may be deferred for these patients, and long-term follow-up should be performed.
Core tip: This is a very interesting case of unlocatable hyperparathyroidism (HPT). The patient presented a huge mass on her left chest wall. However, the serum Ca and parathyroid hormone levels were both normal pre- and post-operation, and the diagnosis was difficult to make. The mass was thought to be likely caused by HPT, but a malignancy could not be ruled out. Finally, the pathology proved that the mass was a brown tumor. Since the patient experienced serum calcium and parathyroid hormone “self-recovery”, she did not receive exploratory surgery for HPT, and received regular follow-up.
- Citation: Wang WD, Zhang N, Qu Q, He XD. Huge brown tumor of the rib in an unlocatable hyperparathyroidism patient with “self-recovered” serum calcium and parathyroid hormone: A case report. World J Clin Cases 2019; 7(24): 4321-4326
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4321.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4321
The brown tumor is a kind of complication of hyperparathyroidism (HPT), and it may sometimes be the initial symptom of HPT. The ultimate therapy is the resolution of HPT. Here, we reported an interesting case of unlocatable HPT that involved a resection of a huge brown tumor of the rib, and experienced “self-recovered” serum parathyroid hormone (PTH) and calcium.
A mass of the left chest wall for about 10 years.
A 34-year-old female came to the General Surgery Department of our hospital with the complaint of a mass of the left chest wall on November 6, 2017. The patient felt transient pain in the left libs in 2007 after delivery. Then the patient accidentally touched a mass in her left ribs with no special feeling. The patient went to a local hospital in June 2015 for a gradual enlargement in mass volume with epigastric discomfort. Upper abdominal computed tomography (CT) revealed that a 7.3 cm × 8.9 cm × 7.0 cm round low-density area might come from ribs that compress the stomach. They also found that serum PTH (162 pg/mL, normal range 12-88 pg/mL) and calcium (Ca, 2.71 mmol/L, normal range 1.8-2.6 mmol/L) levels were higher than normal ranges. A brown tumor of HPT was not excluded. Single photon emission computed tomography was further conducted, but no abnormality was found in the parathyroid glands of both sides. The patient was preliminarily diagnosed with HPT. However, the patient had no local evidence of primary HPT, and she had no history of chronic kidney disease (CKD). The patient received zoledronic acid for 17 mo and stopped in August 2017. The patient came to the Endocrinology Department of our hospital for further diagnosis on November 6, 2017.
A mass of the left chest wall could be touched with no pain, and the size was about 8 cm × 8 cm.
The retest of serum Ca was 2.14 mmol/L, P 0.90 mmol/L, ALP 72 U/L, PTH 59.5 pg/mL, and 1,25-dihydroxyvitamin D3 105.27 pg/mL, all of which were within normal range. The 24-h urinary calcium was 8.18 mmol/24 h and 24-hurinary phosphorus was 10.01 mmol/24 h, and both were also normal.
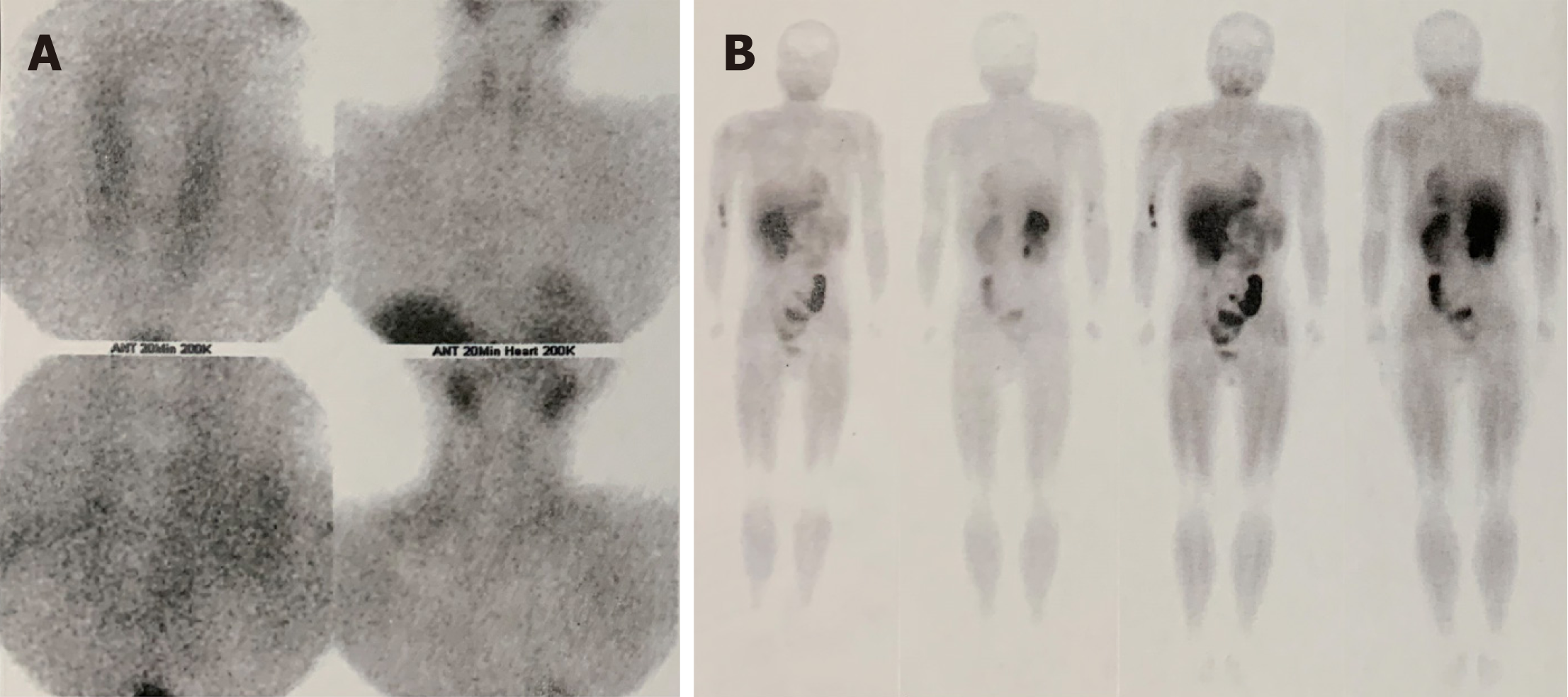
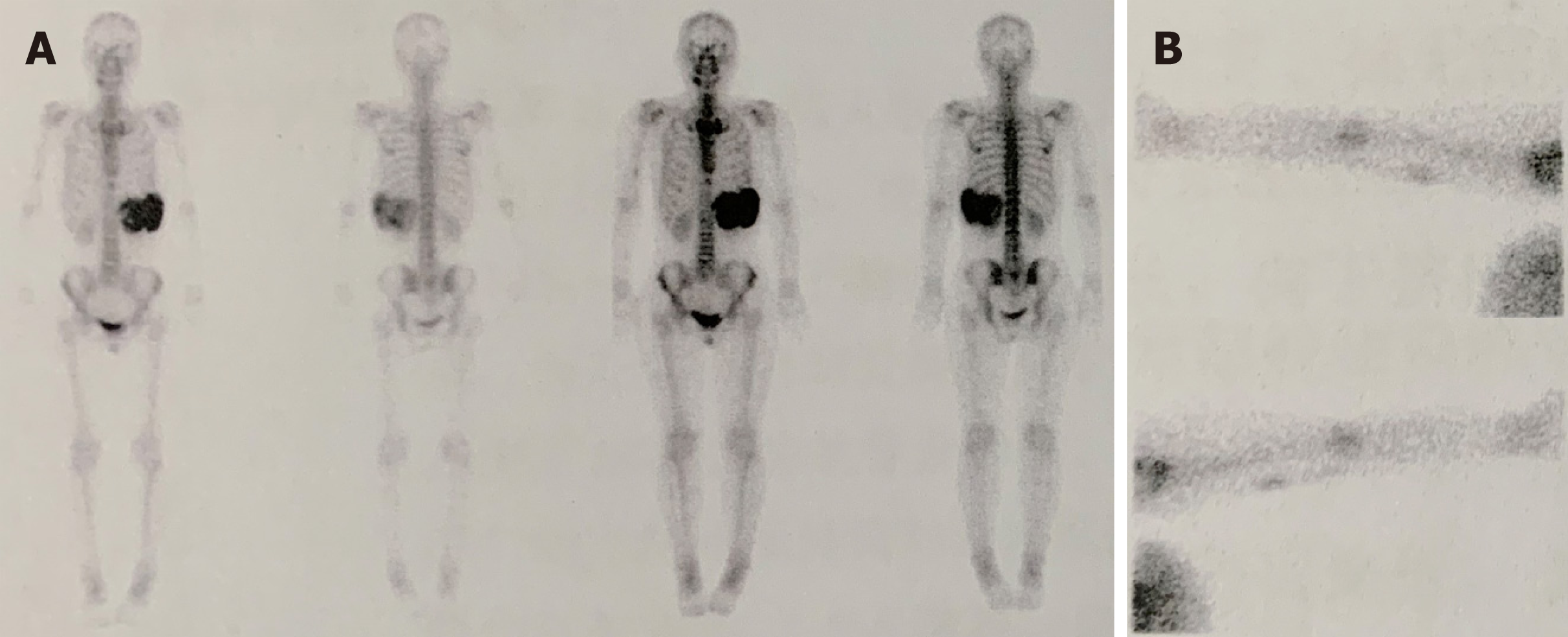
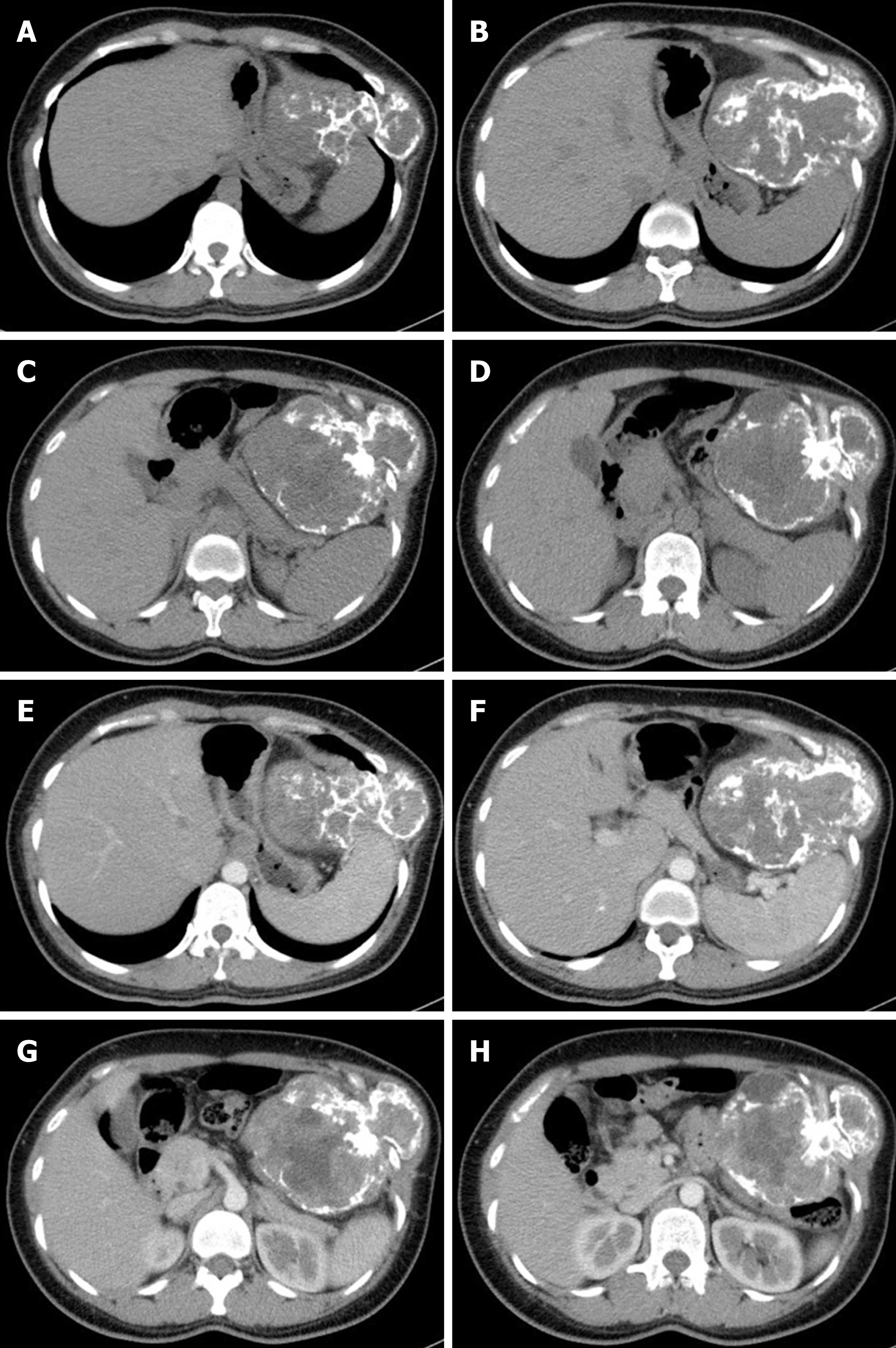
The test of bone mineral density revealed that there was no obvious osteoporosis. The ultrasound of the parathyroid revealed no abnormal changes in the parathyroid region, nor in 99mTc-methoxyisobutyl isonitrile (99mTc-MIBI) imaging (Figure 1). Radionuclide bone imaging presented a tumor likely originating from the 7-9th ribs (Figure 2). Re-examination of the chest and abdomen enhanced CT revealed bone erosion of the left 8th rib, and a local soft tissue mass of 96 mm × 113 mm with strip high density shadow inside. The mass presented irregular enhancement and an oppressed spleen, stomach, pancreas and colon. The boundary of the mass and spleen was unclear (Figure 3).
The diagnosis of a brown tumor was considered, but a malignancy could not be ruled out.
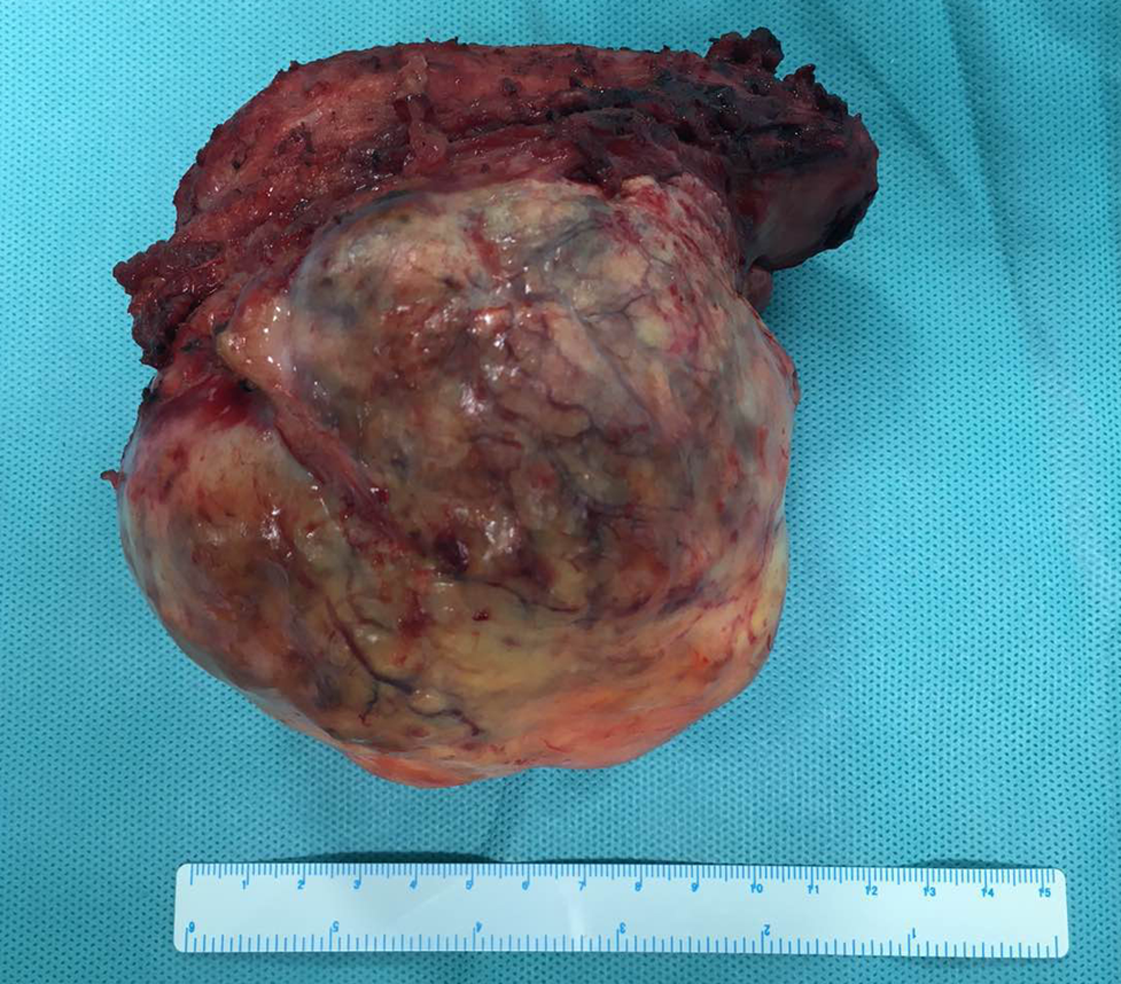
The patient was admitted into the General Surgery Department on December 25, 2017. A mass resection was performed. A thoracoabdominal incision was chosen, and the mass was found originating from the 9-10th ribs. The mass was separated from the compressed tissues, and was excised completely with part of the 9-10th ribs (Figure 4). Then the diaphragm was repaired and the incision was closed. The pathology was a brown tumor of HPT.
The patient did not receive medication after the surgery, and was discharged without complications on the 7th d after operation. Serum PTH (54.6 pg/mL) and Ca (2.28 mmol/L) were in the normal range on July 9, 2019.
Brown tumors are giant-cell lesions due to primary or secondary HPT, and may occur in about 4.5% of primary HPT patients and 1.5% of secondary HPT patients[1]. The common locations of brown tumors are pelvis, ribs, long bone shaft, clavicle, and jaw[2]. Brown tumors may sometimes be the first manifestation of HPT, and should be differentially diagnosed with solitary bone lesions, such as metabolic osteopathy, multiple myeloma, Langerhans’ cell histiocytosis, leukemia, multiple bone cysts, multiple non-ossifying fibroma, and fibrous dysplasia[2,3]. In our case, although the patient has a temporary increase of serum Ca and PTH, the serum or urinary Ca and serum PTH were normal when she came to our hospital. The results of cervical ultrasound and 99mTc-MIBI were also negative. Thus, the diagnosis should be made more prudently. The resection of the mass could not only relieve symptoms, but also exclude the possibility of malignancy.
However, the diagnosis of primary HPT may be inerrant when considering the pathology of the bone lesion and past medical history. The patient realized the mass of the left chest wall 10 years ago, but HPT was considered about 8 years later when high levels of serum Ca and PTH were found. She received zoledronic acid treatment for hypercalcemia for a period of time, which was then discontinued. The preoperative laboratory tests revealed normal serum/urinary Ca and PTH, with negative results from imaging examinations. For a suspicious primary HPT, cervical ultrasound and 99mTc-MIBI are usually used for location, and the sensitivities are 54% and 59%, respectively[2]. However, combined imaging of the two methods could reach a sensitivity of about 90%[2,4]. The main reasons for false-negative ultrasound include abnormal migration of the inferior parathyroid glands (substernal, retrotracheal or retroesophageal)[5], obesity[6], and interference of thyroid lesions[7]. The imaging of 99mTc-MIBI depends on the percentage of mitochondria-rich oxyphil cells, growth phase of glands, and P-glycoprotein levels[6]. PTH level and gland volume are important factors that influence imaging sensitivity[6,8].
When there are no positive results in all of the imaging examinations except for hypercalcemia, and high levels of PTH occur, surgical exploration may be tried. According to the study of Amin et al[2], hyperfunctioning glands are not more frequently located on a particular side or anatomical position. Therefore, intraoperative parathyroid hormone monitoring can be used to guide the resection. Considering that the serum Ca and PTH levels of our patient are within the normal ranges, the patient did not receive the exploratory surgery. However, she needs long-term follow-up to monitor laboratory tests and dynamic changes of primary lesions. The transient HPT with “self-recovery” of PTH is rare. Kim[9] reported an adult female patient with acute kidney injury (AKI) who experienced a transient elevation of PTH. However, the PTH elevation resolved after several weeks, in parallel with improving renal function, and the patient did not develop a brown tumor during this short time period. Our patient has no history of AKI or CKD, and the formation of the brown tumor suggests that the HPT may have existed for a long time. Thus, unlocatable primary HPT should be considered. There has been evidence that zoledronic acid could reduce the level of PTH in HPT of CKD[10], but a similar efficacy in primary HPT is unclear. Close follow-up should therefore be performed in case of recurrent elevation of PTH in the future.
Although there are some unlocatable HPT reports, cases involving a huge brown tumor of the rib and “self-recovered” serum PTH and Ca are relatively rare. An exploratory operation may be deferred for these patients, and long-term follow-up should be performed.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eleftheriadis T S-Editor: Wang J L-Editor: Filipodia E-Editor: Xing YX
| 1. | Mori H, Okada Y, Arao T, Shimaziri S, Tanaka Y. A case of multiple brown tumors with primary hyperparathyroidism. J Bone Miner Metab. 2013;31:123-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Amin AL, Wang TS, Wade TJ, Quiroz FA, Hellman RS, Evans DB, Yen TW. Nonlocalizing imaging studies for hyperparathyroidism: where to explore first? J Am Coll Surg. 2011;213:793-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Fraker DL, Harsono H, Lewis R. Minimally invasive parathyroidectomy: benefits and requirements of localization, diagnosis, and intraoperative PTH monitoring. long-term results. World J Surg. 2009;33:2256-2265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Zhou J, Lu DY, Xia L, Cheng XJ. Diagnosis performance of 99mTc-MIBI and multimodality imaging for hyperparathyroidism. J Huazhong Univ Sci Technolog Med Sci. 2017;37:582-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Erbil Y, Barbaros U, Tükenmez M, Işsever H, Salmaslioğlu A, Adalet I, Ozarmağan S, Tezelman S. Impact of adenoma weight and ectopic location of parathyroid adenoma on localization study results. World J Surg. 2008;32:566-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Berber E, Parikh RT, Ballem N, Garner CN, Milas M, Siperstein AE. Factors contributing to negative parathyroid localization: an analysis of 1000 patients. Surgery. 2008;144:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Kamaya A, Quon A, Jeffrey RB. Sonography of the abnormal parathyroid gland. Ultrasound Q. 2006;22:253-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Amin AL, Wang TS, Wade TJ, Yen TW. Normal PTH levels in primary hyperparathyroidism: still the same disease? Ann Surg Oncol. 2011;18:3437-3442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Lim AK. Transient secondary hyperparathyroidism in acute kidney injury. Intern Med J. 2016;46:857-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Moe SM, Chen NX, Newman CL, Gattone VH 2nd, Organ JM, Chen X, Allen MR. A comparison of calcium to zoledronic acid for improvement of cortical bone in an animal model of CKD. J Bone Miner Res. 2014;29:902-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |