Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4307
Peer-review started: September 13, 2019
First decision: October 24, 2019
Revised: November 8, 2019
Accepted: November 15, 2019
Article in press: November 15, 2019
Published online: December 26, 2019
Processing time: 102 Days and 18.1 Hours
Fewer than 200 cases of diaphragmatic tumors have been reported in the past century. Diaphragmatic hemangiomas are extremely rare. Only nine cases have been reported in English literature to date. We report a case of cavernous hemangioma arising from the diaphragm. Pre-operative three-dimensional (3D) simulation and minimal invasive thoracoscopic excision were performed successfully, and we describe the radiologic findings and the surgical procedure in the following article.
A 40-year-old man was referred for further examination of a mass over the right basal lung without specific symptoms. Contrast-enhanced computed tomography revealed a poorly-enhanced lesion in the right basal lung, abutting to the diaphragm, measuring 3.1 cm × 1.5 cm in size. The mediastinum showed a clear appearance without evidence of abnormal mass or lymphadenopathy. A preoperative 3D image was reconstructed, which revealed a diaphragmatic lesion. Video-assisted thoracic surgery was performed, and a red papillary tumor was found, originating from the right diaphragm. The tumor was resected, and the pathological diagnosis was cavernous hemangioma.
In this rare case of diaphragmatic hemangioma, 3D image simulation was helpful for the preoperative evaluation and surgical decision making.
Core tip: Diaphragmatic hemangioma is rare, and its diagnosis is challenging. We present the case of a 40-year-old man with incidental abnormal findings in chest imaging studies. Contrast-enhanced computed tomography revealed a poorly-enhanced lesion in the right basal lung, abutting to the diaphragm. Three-dimensional (3D) image simulation revealed a supra-diaphragmatic tumor. Successful tumor resection followed by primary repair of diaphragm was performed via minimally invasive thoracoscopic surgery. The pathological findings confirmed a primary cavernous hemangioma of the diaphragm. In this rare case of diaphragmatic hemangioma, 3D image simulation was helpful for the preoperative evaluation and surgical decision making.
- Citation: Chu PY, Lin KH, Kao HL, Peng YJ, Huang TW. Three-dimensional image simulation of primary diaphragmatic hemangioma: A case report. World J Clin Cases 2019; 7(24): 4307-4313
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4307.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4307
Diaphragmatic tumors are very rare. Fewer than 200 cases have been reported in the past century[1]. Most diaphragmatic tumors are benign, including bronchogenic cyst, lipoma, and hemangioma. Diaphragmatic hemangiomas are extremely rare, and only nine cases have been reported in the English literature to date[2-10]. We report a rare case of cavernous hemangioma arising from the diaphragm. Pre-operative three-dimensional (3D) simulation and minimaly invasive thoracoscopic excision were performed successfully, and we describe the radiologic findings and the surgical procedure in the following article.
A mass over the right basal lung field was found incidentally.
A 40-year-old man presented to our hospital with a one-day history of hematuria that was diagnosed due to a ureteral stone after examination. Computed tomography (CT) of the abdomen revealed a mass over the right basal lung field found incidentally. He was referred to a chest surgeon. Contrast-enhanced CT of the chest was arranged for further evaluation.
The patient denied a history of hypertension, diabetes mellitus, or coronary artery disease. He had no known drug or food allergies. He also denied a history of operation, trauma, or blood transfusion.
The patient had no significant personal or family history.
The patient’s vital signs upon arrival were as follows: Body temperature 36.5°C, heart rate 74 beats/min, respiratory rate 18 times/min, blood pressure 156/84 mmHg, and oxygen saturation 98% on room air. He was alerted and oriented. The physical examination disclosed clean breathing sounds bilaterally, no chest tenderness, and no chest wall deformity. There was no specific finding of other systems.
A complete blood count was obtained showing a white blood cell count of 8.75 × 106/L, hemoglobin level of 15.7 g/dL, and platelet count of 222 × 109/L. Electrolyte, blood biochemistry, and coagulation tests were all in normal range.
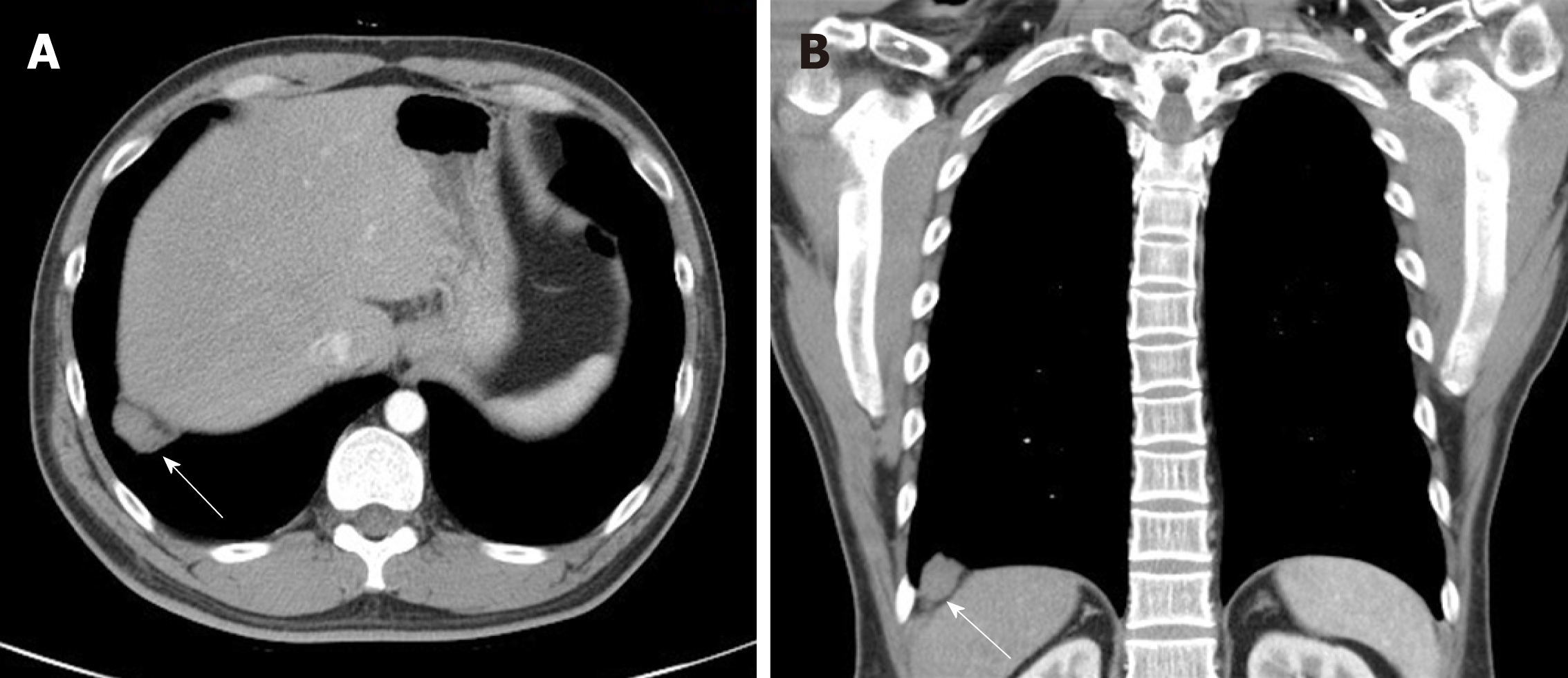
Contrast-enhanced CT of the chest revealed a poorly-enhanced lesion in the right basal lung, abutting the right diaphragm, measuring 3.1 cm × 1.5 cm in size (Figure 1). The mediastinum showed a clear appearance without evidence of abnormal mass or lymphadenopathy.
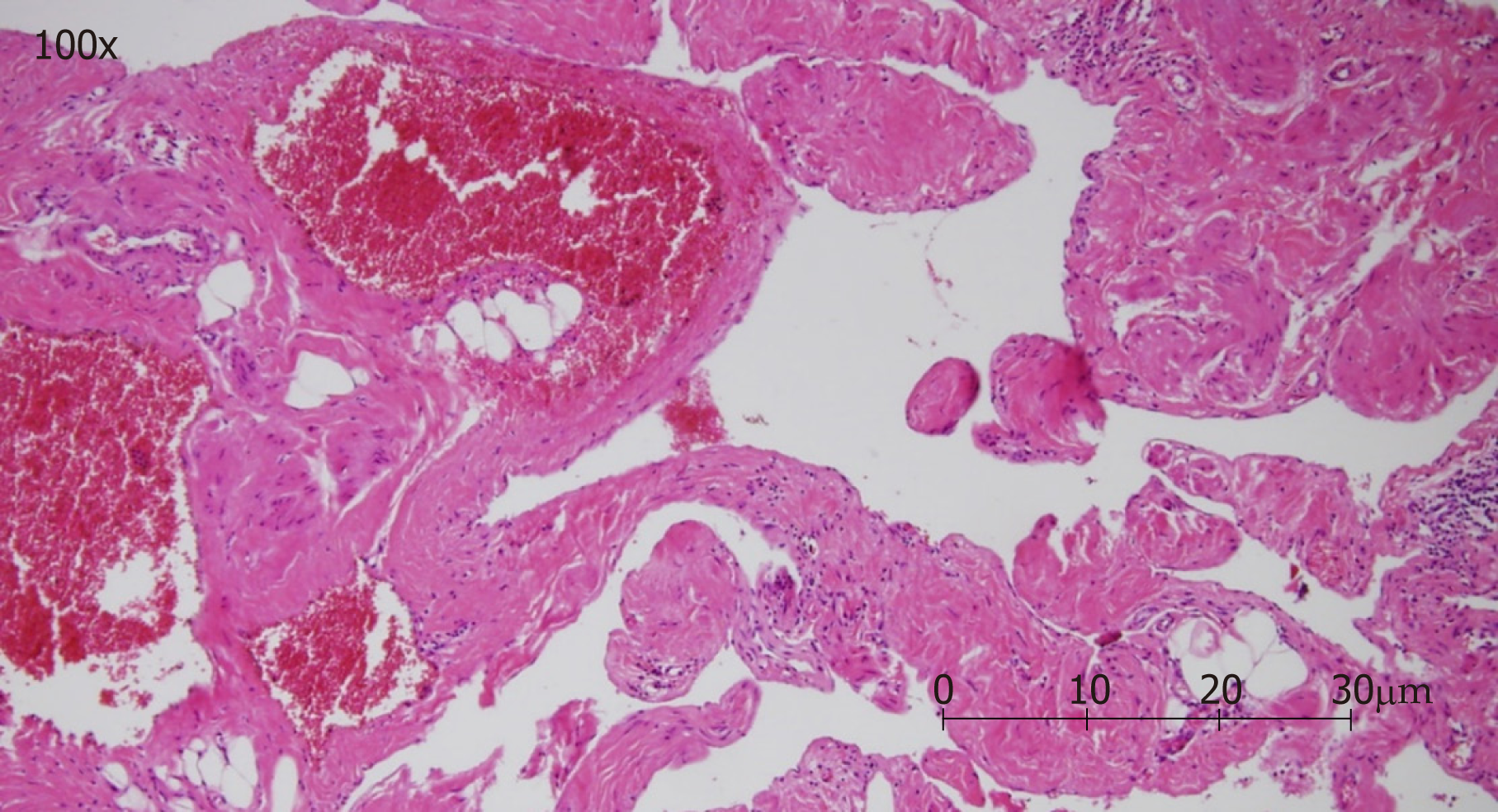
The resected tumor was sent for pathology examination after the operation. Grossly, the tumor was 3.5 cm × 1.5 cm × 1.3 cm in size and brown in color, with a soft consistency. Microscopically, the section showed a vascular lesion composed of dilated cavernous vascular spaces separated by irregular vascular walls (Figure 2). The pathological findings were compatible with those of cavernous hemangioma.
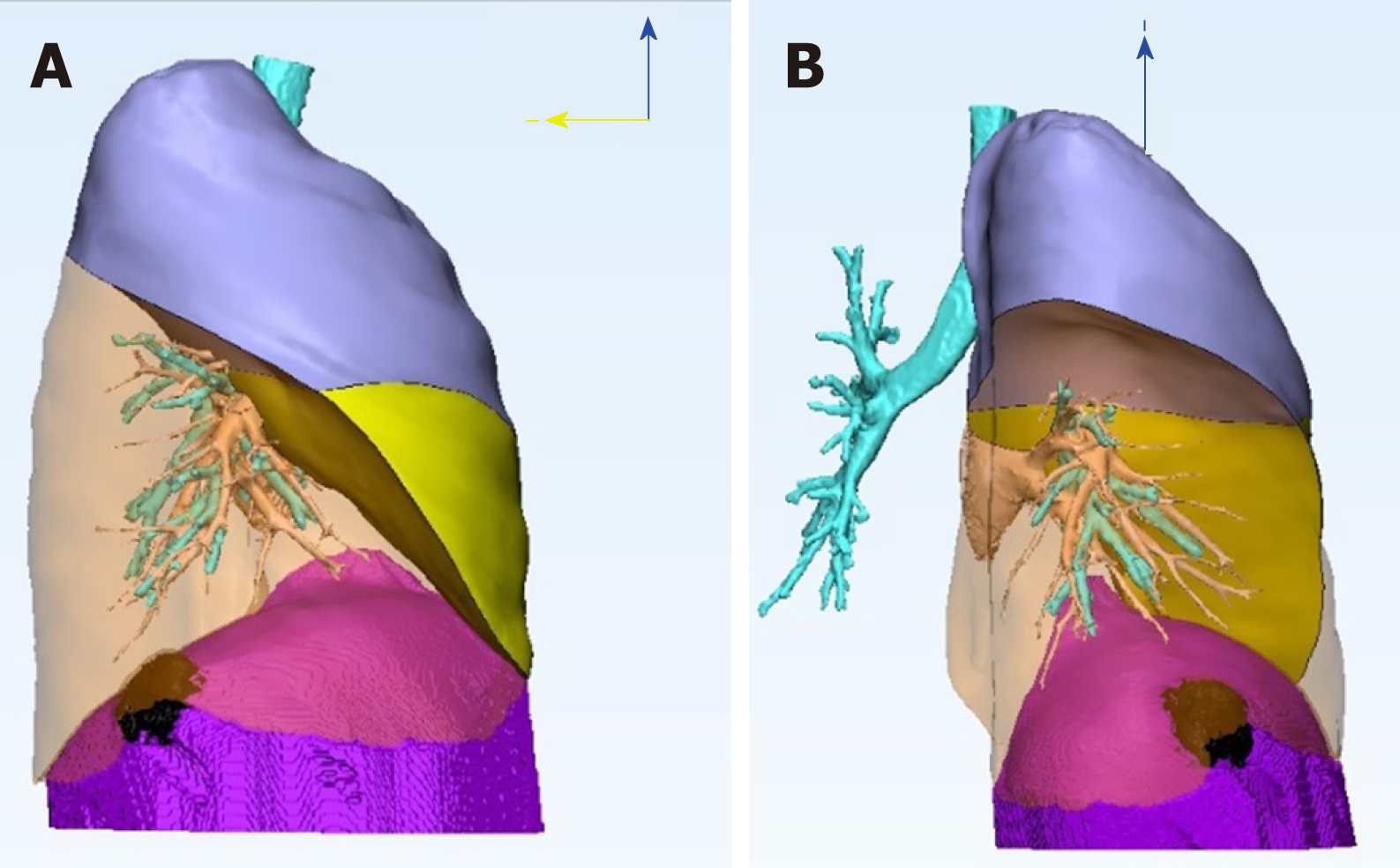
It was difficult to differentiate its origin from that of lung parenchyma or diaphragm tumor. A preoperative 3D image was reconstructed, which revealed a diaphragmatic lesion (Figure 3). The patient underwent video-assisted surgery. A thoracoscope was inserted into the thoracic cavity via an incision in the 8th intercostal space. Intraoperative findings revealed a lobulated reddish tumor located at the lateral aspect of the right diaphragm with a wide-based pedicle (Figure 4). The patient underwent a thoracoscopic procedure with tumor resection, followed by primary repair of the diaphragm. An energy device (LigaSure™ vessel sealing technology, Medtronic) was used because of the presence of an abundant feeding vessel which bled easily on touch.
The patient’s postoperative course was uneventful, and he was found to be tumor free during the 2-year follow-up.
Primary diaphragmatic tumors are very rare. In the past century, fewer than 200 cases have been reported[1]. Most diaphragmatic tumors are benign, including cystic mass (bronchogenic cyst, for example), lipoma, hemangioma, angiofibroma, neurofibroma, schwannoma, leiomyoma, teratoma, and endometrioma. Malignant diaphragmatic tumors include rhabdomyosarcoma, fibrosarcoma, sarcoma, hemangiopericytoma, germ cell tumors, pheochromocytoma, and leiomyosarcoma. Diaphragmatic hemangiomas are extremely rare, and only nine cases have been reported in the English literature to date[2-10] (Table 1).
| Ref. | Gender | Age (yr) | Clinical magnification | Diagnostic modality | Tumor location | Treatment | Outcome |
| Kaniklides et al[2], 1999 | Male | 4 | Large numbers of subcutaneous vessels over left upper abdominal wall | CT, MRI, angiography | Supraphrenic, left | Surgical resection with laparotomy plus thoracotomy | Good |
| Ohsaki et al[3], 2000 | Female | 31 | Chest pain on the deep inspirations | CT, MRI, bone scintigraphy (99mTc-hydroxymethylene diphosphonate) | Supraphrenic, right | Surgical resection via thoracic approach | Good |
| Cacciaguerra et al[4], 2001 | Female | 0 | Neonatal respiratory failure and hydrops fetalis | Cardiac sonography, CT | Supraphrenic, right | Surgical resection with median sternotomy | Good |
| Kono et al[5], 2006 | Female | 75 | No specific discomfort | CT, MRI | Supraphrenic, right | Surgical resection via thoracoscopic approach | good |
| Ino et al[6], 2010 | Male | 64 | No specific discomfort | CT, PET scan | Subphrenic, left | Surgical resection via laparoscopic approach | Good |
| Tsang et al[9], 2011 | Male | 0 | Massive pleural effusion, pericardial effusion with cardiac tamponade | Chest X ray, cardioechography | Supraphrenic and subphrenic, left | Surgical resection with median sternotomy, extended to upper abdomen | Good |
| Ueno et al[7], 2013 | Male | 51 | No specific discomfort | CT, PET scan | Supraphrenic, right | Surgical resection via thoracic approach | Good |
| Yao et al[8], 2013 | Unknown | 0 | Dyspnea | CT, MR | Supraphrenic, right | Interventional vascular embolization | Good |
| Wu et al[10], 2015 | Female | 0 | Progressive respiratory distress and massive right hydrothorax | Sonography, CT, MRI | Supraphrenic, right | Interventional vascular embolization | Good |
Most diaphragmatic tumors are asymptomatic and, therefore, often incidentally found. Associated symptoms are often related to the compression effect of huge tumors, including chest pain, shortness of breath, or abdominal pain. CT discloses more information about these tumors, such as size, location, and relationship with other structures. Using CT, we can also distinguish whether a diaphragmatic tumor is cystic or solid in nature. Magnetic resonance imaging (MRI) with contrast could help evaluate the internal components of the tumor without any concern of radiation dosage.
It is common to diagnose hepatic hemangioma by abdominal dynamic three-phase CT. Kono et al[5] reported a case of diaphragmatic hemangioma using dynamic imaging findings. On contrast-enhanced dynamic MRI images of T1-weighted imaging, the lesion showed a gradual enhancement pattern, which was maintained in the late phase. It describes the possibility of differentiating diaphragmatic hemangioma from other diaphragm tumors. In our case, two-phase contrast-enhanced CT of the chest disclosed a poorly-enhanced lobulated soft-tissue lesion, measuring 3.1 cm × 1.5 cm in size, in the right basal lung. Dynamic three-phase CT might provide more information. However, other vascular-rich tumors, such as hemangiopericytoma and angiofibroma, should be included in the differential diagnosis as well. Pathological examination is still required to confirm the diagnosis.
Benign diaphragmatic tumors could be observed. Image-guided needle biopsy is considered only for some patients because of limitations imposed by tumor size, diaphragm motion during inspiration and expiration, and risk of bleeding. Surgical treatment of a diaphragmatic tumor is indicated for patients with a symptomatic benign tumor or a resectable malignant tumor, or for patients requiring a definitive diagnosis. However, due to the small size of the tumor and risk of bleeding, we performed surgical intervention for our patient instead of biopsy.
Sometimes, it is difficult to distinguish between tumors originating from the lung, diaphragm, or intraabdominal organs using two-dimensional imaging. Their origin determines the surgical approach, which is either laparoscopy or thoracoscopy. Thapar et al[11] described a case of a diaphragmatic tumor that was thought to be an atypical hepatic mass preoperatively. 3D image simulation might be of help in such a situation.
The usefulness of 3D angiography using multiple detector CT in thoracic surgery was first reported by Watanabe et al[12] in 2003. Over the past decade, advanced software provides high-quality 3D models of the pulmonary vessels and the tracheobronchial tree. The clinical applications of 3D lung modeling in surgical simulation and navigation systems are safe and useful[13]. In this case, we built a 3D image simulation (Mimics Innovation Suite 21.0, Materialise) that clarified the relationship of the tumor and neighboring organs. The simulation revealed that it was a diaphragmatic tumor abutting the right basal lung, without any obvious extra blood supply. Thoracoscopic tumor resection was deemed suitable for this patient and it was performed smoothly.
3D image simulation clarified the relationship of the tumor and neighboring organs. In this rare case of diaphragmatic hemangioma, 3D image simulation was helpful for the preoperative evaluation of the tumor and surgical decision making.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A, Pandey A S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Kim MP, Hofstetter WL. Tumors of the diaphragm. Thorac Surg Clin. 2009;19:521-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Kaniklides C, Dimopoulos PA. Diaphragmatic haemangioma. A case report. Acta Radiol. 1999;40:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Ohsaki Y, Morimoto H, Osanai S, Nishigaki Y, Akiba Y, Hasebe C, Hirata S, Aburano T, Miyokawa N, Kikuchi K. Extensively calcified hemangioma of the diaphragm with increased 99mTc-hydroxymethylene diphosphonate uptake. Intern Med. 2000;39:576-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Cacciaguerra S, Vasta G, Benedetto AG, Bagnara V, Guarnera S, Bartoloni G, Patanè L. Neonatal diaphragmatic hemangioma. J Pediatr Surg. 2001;36:E21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Kono R, Terasaki H, Fujimoto K, Sadohara J, Oshita Y, Yano H, Hayabuchi N. Venous hemangioma arising from the diaphragm: a case report of computed tomography and magnetic resonance imaging findings. J Thorac Imaging. 2006;21:231-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Ino H, Naitou M, Hato S, Tomiyama K, Mandai Y, Hayashi T, Okada M, Doihara H. A rare primary diaphragmatic hemangioma successfully treated by laparoscopic surgery: report of a case. Surg Today. 2010;40:654-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Ueno K, Takeuchi E, Hino H, Kawashima M. Cavernous hemangioma arising from the diaphragm. Asian Cardiovasc Thorac Ann. 2013;21:735-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Yao Q, Hu X, Huang G, Pa M. A case of diaphragmatic infantile hemangioma. J Perinatol. 2013;33:576-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Tsang FH, Lun KS, Cheng LC. Hemangioma of the diaphragm presenting with cardiac tamponade. J Card Surg. 2011;26:620-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Wu L, Wang JM, Qiao ZW, Yan YL, Wang LS. Successful embolization and long-term follow-up of a rare neonatal diaphragmatic hemangioma. SAGE Open Med Case Rep. 2015;3:2050313X15615471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Thapar S, Ahuja A, Rastogi A. Rare diaphragmatic tumor mimicking liver mass. World J Gastrointest Surg. 2014;6:33-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Watanabe S, Arai K, Watanabe T, Koda W, Urayama H. Use of three-dimensional computed tomographic angiography of pulmonary vessels for lung resections. Ann Thorac Surg. 2003;75:388-92; discussion 392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 81] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Ikeda N, Yoshimura A, Hagiwara M, Akata S, Saji H. Three dimensional computed tomography lung modeling is useful in simulation and navigation of lung cancer surgery. Ann Thorac Cardiovasc Surg. 2013;19:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |