Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4245
Peer-review started: September 29, 2019
First decision: November 19, 2019
Revised: November 27, 2019
Accepted: November 30, 2019
Article in press: November 30, 2019
Published online: December 26, 2019
Processing time: 87 Days and 11.3 Hours
In recent years, with the popularity of laryngeal mask airway (LMA) for the management of clinical anesthesia, the influence of the LMA on the position and blood flow of the internal jugular vein (IJV) has attracted an increasing amount of attention.
To investigate the effect of placement of different types of LMA (Supreme LMA, Guardian LMA, I-gel LMA) on the position and blood flow of the right IJV.
This was a prospective randomized controlled trial. A total of 102 patients aged 18-75 years who were scheduled to undergo laparoscopic abdominal surgery with general anesthesia were randomly assigned to three groups: Supreme LMA (group 1), Guardian LMA (group 2), and I-gel LMA (group 3) groups. The main indicator was the overlap index (OI) of IJV and the common carotid artery (CCA) at the high, middle, and low points before and after the placement of the LMA. The second indicators were the proportion of ultrasound-simulated needle crossing the IJV and CCA, and the cross-sectional area and blood flow velocity of the IJV before and after placement of the LMA at the middle point.
Data from 100 patients were included in the statistical analysis. The OI increased significantly after placement of the LMA in the three groups at the three points (P < 0.01), except group 2 at the low point. In group 2 and group 3, the OI was lower than that in group 1 after LMA insertion at the high point (P < 0.0167). At the middle point, after LMA insertion, the proportion of simulated needle crossing the IJV significantly decreased in all three groups (P < 0.05), and the proportion in group 2 was higher than that in group 3 (P < 0.0167). The proportion of simulated needle crossing the CCA or both the IJV and CCA significantly increased in group 1 and group 2 (P < 0.05), which increased with no statistical significance in group 3. After LMA insertion, the cross-sectional area of the IJV significantly increased, while the blood flow velocity significantly decreased (P < 0.01). There was no significant difference among the three groups.
The placement of Supreme, Guardian, and I-gel LMA can increase the OI, reduce the success rate of IJV puncture, increase the incidence of arterial puncture, and cause congestion of IJV. Type of LMA did not influence the difficulty of IJV puncture. Therefore when LMA is used, ultrasound is recommended to guide the IJV puncture.
Core tip: The placement of laryngeal mask airway (LMA) may affect the position and blood flow of the internal jugular vein (IJV). The results of our study show that the placement of Supreme, Guardian, and I-gel LMA can increase the overlap index, reduce the success rate of IJV puncture, increase the incidence of arterial puncture, and cause congestion of IJV. Type of LMA did not influence the difficulty of IJV puncture. Therefore when LMA is used, ultrasound is recommended to guide the IJV puncture.
- Citation: Zhang JJ, Qu ZY, Hua Z, Zuo MZ, Zhang HY. Effect of different types of laryngeal mask airway placement on the right internal jugular vein: A prospective randomized controlled trial. World J Clin Cases 2019; 7(24): 4245-4253
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4245.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4245
Since the introduction of the laryngeal mask airway (LMA) into wide clinical practice, there has been a great expansion in its clinical applications. Patients receiving general anesthesia and endotracheal intubation can experience a stress response that produces clinical symptoms including sympathetic stimulation, tachycardia, and elevated blood pressure. And the LMA is preferred in airway management for improved hemodynamics and less difficulty in placement[1,2], especially for the benefit of a secure airway in patients with a potentially difficult intubation[3-6]. With the popularity of LMA, more and more types of LMA are being invented, and Supreme LMA, Guardian LMA and I-gel LMA are commonly used in our department at present.
In clinical anesthesia using LMA for airway management, central venous catheterization might be required in some patients. In order to avoid affecting the surgical operation, and because it’s easy to perform, the internal jugular vein (IJV) is a commonly used catheterization route, and the “central landmark” is generally used[7]. However, placement of the LMA may cause a change in the anatomy of the surrounding structures, especially the position relation of the IJV and common carotid artery (CCA). Previous studies have shown that when using the central landmark to catheterize the IJV after ProSeal™ LMA placement, medial deviation of the central landmark should be considered[8]. After placement of the LMA-Classic™, overlapping of the IJV and CCA increased at the high and middle points of the IJV while at the lower point the position of the vessels remained unaffected[9]. These anatomical changes may lead to failure of the catheterization of IJV based on the landmark technique. In addition, placement of the LMA may also cause venous congestion, which would have particular relevance in patients undergoing general anesthesia for eye or head and neck surgery, where raised venous pressure may lead to raised intra-ocular pressure or increased bleeding[10]. However, there are few studies on the influence of placement of LMA or type of LMA on the position of the IJV and CCA, and the changes in blood flow of IJV.
Therefore, we designed this prospective randomized controlled trial, to observe the effect of placement of different types of LMA on the position and blood flow of right IJV.
This study was a prospective randomized controlled trial. The protocol was approved by the Beijing Hospital Medical Ethics Committee (2012bjyyec-030-02). Informed consent was signed by the patient or legal guardian before enrollment. The study was conducted in the Departments of Anesthesiology of Beijing Hospital.
Patients were included if they met the following criteria: (1) Scheduled to undergo laparoscopic abdominal surgery with general anesthesia; and (2) Age ≥ 18 years and ≤ 75 years. Patients were excluded if they met any of the following criteria: (1) Refused to participate in the study; (2) Body weight of 30% more or less than the standard weight; (3) American Society of Anesthesiologists physical classification of III or higher; (4) Abnormal anatomy of the pharynx; (5) Head and neck movement disorder or restricted mouth opening; and (6) Other circumstances that the doctor or investigator believed not suitable for the study.
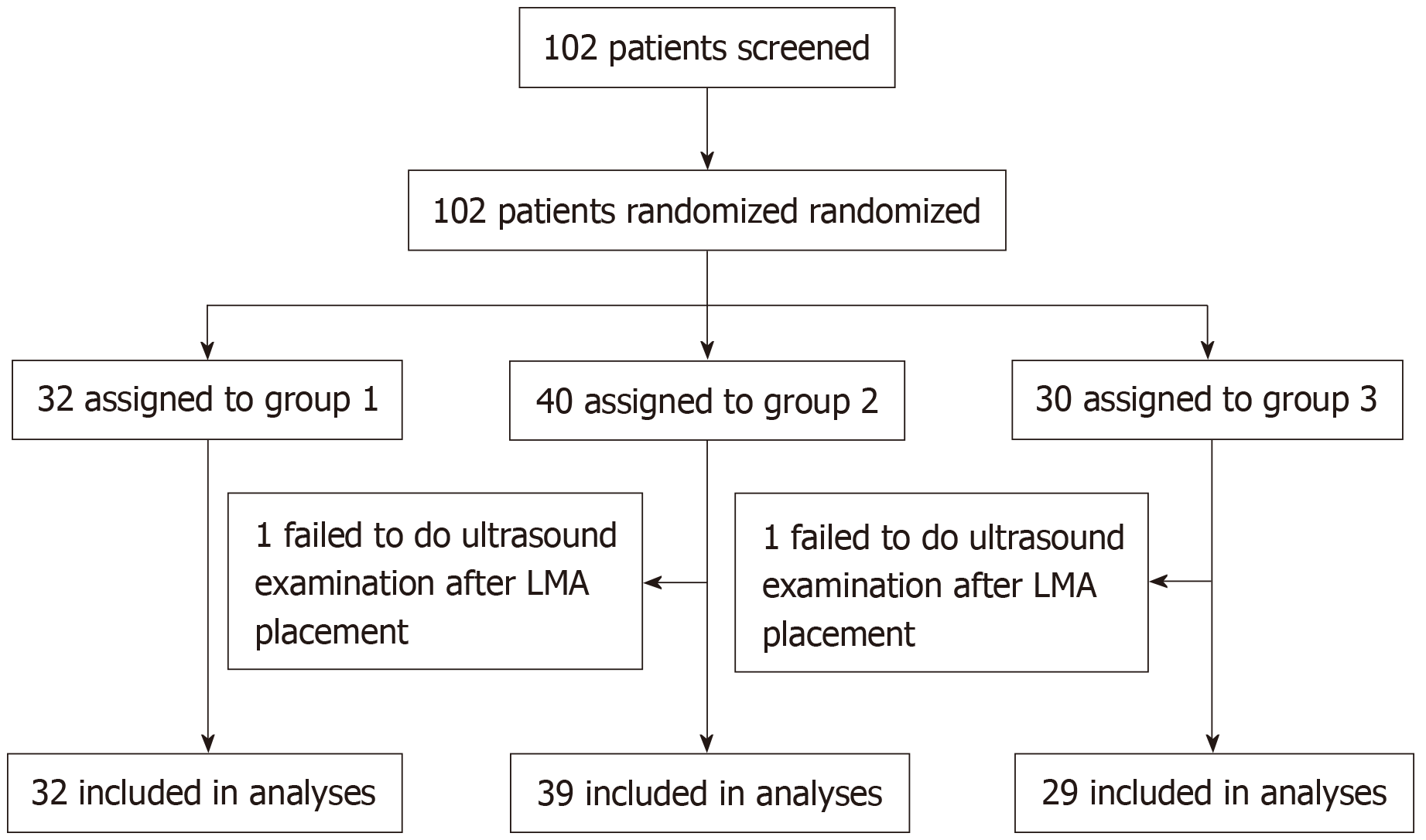
Random numbers were generated using Microsoft Excel software. The enrolled patients were randomly assigned to the Supreme LMA group (group 1), the Guardian LMA group (group 2), or the I-gel LMA group (group 3) (Figure 1). The results of randomization were sealed in sequentially numbered envelopes until the end of the study. The anesthesiologist used the corresponding type of LMA according to the randomization and selected a suitable size on the base of body weight. After rapid induction of general anesthesia, the LMA was inserted and the cuff was inflated until the LMA was just above airway leak pressure. A clear airway was confirmed using clinical signs and capnography.
During the measurement, an ultrasound scanner (M-Turbo, linear type,13-MHz probe; Sonosite, Seattle, WA, United States) was used. The measurement sites consisted of three points on the right side of the neck (high point: At the midpoint of the mastoid process and ramus clavicularis of the sternocleidomastoid muscle attach to the clavicle; middle point: At the intersection of the clavicular head and sternal head of the sternocleidomastoid muscle; low point: Near the area where the ramus clavicularis of the sternocleidomastoid muscle attaches to the clavicle). The reason for selecting these three points is that they are all used as central venous puncture sites[9]. Each patient took the supine position, and the patient’s head was rotated 30° to the left from midline. The probe was gently pressed against the neck and the center of the probe was positioned at the measurement point in short axis scanning. The following indicators of IJV and CCA was measured before and after LMA placement: (1) At the high, middle, and low points, the horizontal diameter of the CCA and the overlap length of the IJV and CCA, respectively, were measured; and (2) At the middle point, using ultrasound-simulated needle puncture direction (the probe was 30° above the coronal plane, and pointed to the ipsilateral nipple direction), whether the simulated puncture needle crossed the IJV or CCA was recorded. Using Doppler to measure the cross-sectional area and blood flow velocity of IJV, each indicator was measured three times and averaged, and the pressure of the cuff of the LMA was 60 cmH2O.
The main indicator was the overlap index (OI), which has been proposed to represent the percent of overlap of the IJV and CCA[11]. The OI was derived from the ratio of the overlap length of the IJV to the horizontal diameter of the CCA. The formula for calculation is as follows: OI = [overlap (mm)/CCA diameter (mm)] × 100[11]. The secondary indicators included the proportion of ultrasound-simulated needle crossing the IJV and CCA before and after placement of the LMA, and the cross-sectional area and blood flow velocity of the IJV before and after placement of the LMA.
Continuous variables were analyzed with the independent samples t-test, variance analysis with repeated measures, Mann-Whitney U test, the Kruskal-Wallis rank sum test, or the Wilcoxon paired rank-sum test. Categorical variables were analyzed with chi-square analysis, continuity correction χ2 test, or Fisher’s exact test. Statistical analyses were performed with SPSS 14.0 (SPSS Inc, Chicago, IL, United States). All tests were two-sided, and P < 0.05 was considered statistically significant. With Bonferroni correction adjusting for testing three genera, the α-threshold 0.0167 (0.05/3) was applied to determine whether the association was significant.
From November 5, 2013 to June 24, 2014, a total of 102 patients participated in the study. After LMA placement, 1 patient in group 2 and 1 patient in group 3 failed to do ultrasound examination, so 100 patients were included in the final analysis: 32 patients in group 1, 39 patients in group 2, and 29 patients in group 3. The last case was completed on June 24, 2014. The baseline demographics and characteristics were comparable among the three groups (Table 1).
| Group 1, n = 32 | Group 2, n = 39 | Group 3, n = 29 | P value | |
| Gender, Male/Female | 2/30 | 6/33 | 5/24 | 0.342 |
| Age in yr | 50 ± 16 | 49 ± 15 | 49 ± 16 | 0.932 |
| Height in cm | 163 ± 5 | 164 ± 6 | 163 ± 7 | 0.626 |
| BMI in kg/m2 | 23 ± 3 | 23 ± 3 | 23 ± 3 | 0.754 |
| ASA, I/II | 17/15 | 26/13 | 18/11 | 0.503 |
| LMA size, 3/4/5 | 4/27/1 | 3/35/1 | 5/23/1 | 0.807 |
Among the three groups, the OI increased significantly after placement of LMA at the three points (P < 0.01) except for group 2 at the low point. Among the three groups, there was significant difference at the high point after LMA insertion (P < 0.01), in group 2 and group 3 the OI was lower than that in group 1 (P < 0.0167). There was no significant difference among the three groups at the middle and low points (Table 2).
| Group 1, n = 32 | Group 2, n = 39 | Group 3, n = 29 | P value | |
| High point | ||||
| Before LMA | 21.7 (6.5, 61.5) | 23.4 (0, 51.6) | 25.7 (12.2, 60.2) | 0.712 |
| After LMA | 100 (100, 100)d | 72.1 (40.0, 100)ad | 100 (69.0, 100)ad | 0.000 |
| Middle point | ||||
| Before LMA | 52.8 (29.1, 82.7) | 44.8 (18.5, 65.9) | 40.3 (19.6, 100) | 0.624 |
| After LMA | 100 (100, 100)d | 100 (100, 100)d | 100 (100, 100)d | 0.318 |
| Low point | ||||
| Before LMA | 26.2 (0.0, 97.8) | 41.0 (11.5, 94.5) | 30.3 (0, 100) | 0.465 |
| After LMA | 67.8 (18.5, 100)d | 56.3 (12.1, 100) | 54.7 (22.5, 100)d | 0.993 |
At the middle point, after LMA insertion, the proportion of simulated needle path based on the landmark technique crossing the IJV significantly decreased in all three groups (P < 0.05). The proportion of simulated needle crossing the CCA or both the IJV and CCA significantly increased in group 1 and group 2 (P < 0.05), which increased with no statistical significance in group 3. Among the groups, there was a significant difference regarding the proportion of simulated needle path crossing the IJV after LMA insertion, which was higher in group 2 than that in group 3 (P < 0.0167), and there was no other significant difference (Table 3).
| Group 1, n = 32 | Group 2, n = 39 | Group 3, n = 29 | P value | |
| IJV | ||||
| Before LMA | 31 (96.9) | 38 (97.4) | 24 (82.8) | 0.059 |
| After LMA | 24 (75.0)d | 31 (79.5)ad | 15 (51.7)d | 0.036 |
| CCA | ||||
| Before LMA | 6 (18.8) | 8 (20.5) | 7 (24.1) | 0.871 |
| After LMA | 19 (59.4)d | 17 (43.6)d | 13 (44.8) | 0.361 |
| IJV and CCA | ||||
| Before LMA | 6 (18.8) | 7 (17.9) | 3 (10.3) | 0.613 |
| After LMA | 17 (53.1)d | 16 (41.0)d | 9 (31.0) | 0.215 |
After LMA insertion, the cross-sectional area of the IJV significantly increased (P < 0.01), while the blood flow velocity significantly decreased (P < 0.01). There was no significant difference among the three groups (Table 4).
Since the introduction of the LMA into wide clinical practice, there has been great expansion in its clinical applications including cardiopulmonary resuscitation, cardiac anesthesia, and in cases of potentially unstable cervical spines[12-15]. IJV cannulation may be required in such cases, which rely on anatomical landmarks to indicate the likely position of the vein. With the popularity of LMA in clinical anesthesia and the need of intraoperative IJV catheterization, the impact of placement of LMA on the main blood vessels of the neck has attracted more and more attention. The change of anatomy may result in difficulty in catheterization of IJV based on the landmark technique.
A study showed that when the patient was placed in the neutral position, after placement of the LMA there was no significant lateral displacement of the IJV or CCA and there was no significant overlap between the IJV and CCA[16]. When performing IJV catheterization, the head was rotated 30° to the left from midline, while the study showed that the overlap between the IJV and CCA increased when the head was 30° to the left[17]. Placement of the LMA causes change in the structure of the neck. A radiological study about the relationship between the LMA and structures of the larynx showed that when the cuff was inflated, the thyroid, arytenoid, and cartilage moved anteriorly and tissues overlying the larynx bulged slightly[18]. Since the low point is farther from the larynx, we expected that placement of the LMA at the low point may have a smaller effect on the OI. In the past, Takeyama et al[9] showed that after placement of the LMA-Classic™, overlapping of the IJV and CCA increased at the high and middle points of the IJV, while at the lower point, the position of the vessels remained unaffected. In our study, the results showed that after placement of the Guardian LMA, the OI significantly increased at both the high and the middle points, which did not increase statistically at the low point. However, after placement of the Supreme or I-gel LMA, the OI significantly increased at all the high, middle and low points. At the high point, Supreme LMA showed a greater impact on the OI than the Guardian and I-gel LMA, while at the middle and low points, there was no significant difference among the different types of LMA regarding the influence on OI. The difference in structure of the three types of LMA may explain the change.
Previous studies have shown that when using the central landmark to catheterize the IJV after a ProSeal™ LMA placement, medial deviation of the central landmark should be considered, and after placement of the ProSeal™ LMA, the central landmark does not offer a good success rate at the first puncture attempt[8]. In our study, at the middle point, using ultrasound-simulated needle puncture direction based on the central landmark, the results also showed that the success rate of IJV puncture after placement of Supreme, Guardian and I-gel was significantly reduced. Among the three different types of LMA, the success rate of IJV puncture decreased more than that in the Guardian LMA. Arterial puncture is a common complication in the operation of IJV catheterization. In a previous study, the incidence of arterial puncture during IJV catheterization without LMA was 2%-17%[19]. After placement of the Proseal LMA, the incidence of arterial puncture was significantly increased to 31.4%[8]. However, there are few studies on the incidence of arterial puncture during IJV catheterization after placement of other types of LMA. Our study observed the rate of arterial puncture after placement of the three types of LMA. The results showed that the incidence of arterial puncture was significantly increased after placement of Supreme and Guardian LMA, which was 59.4% and 43.6% respectively; and not significantly increased after placement of I-gel LMA, which was also as high as 44.8%. One possible reason why the IJV cannulation success rate is lower and CCA puncture rate is higher in patients with LMA insertion is that the IJV overlaps with the CCA after LMA insertion and cuff inflation. Therefore, during IJV puncture at high or middle or low points, ultrasound guidance is advisable to avoid arterial puncture after placement of the LMA, no matter what type of LMA is used.
Placement of LMA can affect blood flow of IJV and cause congestion. Colbert et al[20] showed that inflation of the cuff on the LMA resulted in a decrease in carotid bulb cross-sectional area which resulted in a decrease in blood flow. The results of our study showed that the placement of Supreme, Guardian and I-gel LMA resulted in significant increase in cross-sectional area and significant decrease in blood flow velocity of the IJV, and there was no significant difference between three types of LMA. The result means that congestion of the IJV can exist when the LMA is inserted.
This study had potential limitations. First, we simulated the needle path, as we did not consider it ethical s to achieve our study goals by actually passing a needle instead of simulating the needle path, because most patients observed in our study did not need catheterization of IJV for the operation, and most catheterizations of IJV in our department have been assisted by the use of ultrasound for several years. Second, we measured the cross-sectional area and blood flow velocity of the IJV when the pressure of the cuff was 60 cm H2O; however, we did not measure the cross-sectional area and blood flow velocity of the IJV when the pressure of the cuff was higher or just above airway leak pressure. Third, the potential for inaccuracies in the 1-2 mm range to influence our results cannot be completely eliminated.
In conclusion, the results of this study showed that placement of Supreme, Guardian and I-gel LMA can increase the OI, reduce the success rate of IJV puncture, increase the incidence of arterial puncture, and cause congestion of IJV. Type of LMA did not influence the difficulty of IJV puncture. Therefore when LMA is used, ultrasound is recommended to guide the IJV puncture.
Since the introduction of the laryngeal mask airway (LMA) into wide clinical practice, there has been a great expansion in its clinical applications, and IJV cannulation may be required in such cases, which rely on anatomical landmarks to indicate the likely position of the vein. In recent years, the impact of placement of LMA on the main blood vessels of the neck has attracted more and more attention.
In clinical anesthesia using LMA for airway management, central venous catheterization via the IJV might be required in some patients. However, placement of the LMA may cause a change in the anatomy of the surrounding structures, especially the position relation of the IJV and common carotid artery (CCA). These anatomical changes may lead to failure of the catheterization of IJV based on the landmark technique. In addition, placement of the LMA may also cause venous congestion. However, there are few studies on the influence of placement of LMA or type of LMA on the position of the IJV and CCA, and the changes in blood flow of IJV.
To investigate the effect of placement of different types of LMA (Supreme LMA, Guardian LMA, I-gel LMA) on the position and blood flow of the right IJV.
This was a prospective randomized controlled trial. A total of 102 patients aged 18-75 years who were scheduled to undergo laparoscopic abdominal surgery with general anesthesia were randomly assigned to three groups: the Supreme LMA group (group 1), the Guardian LMA group (group 2), and the I-gel LMA group (group 3). The main indicator was the OI of IJV and CCA at the high, middle and low points before and after the placement of the LMA. The second indicators were the proportion of the ultrasound-simulated needle cross the IJV and CCA, the cross-sectional area and blood flow velocity of the IJV before and after the placement of the LMA at the middle point.
The OI increased significantly after placement of the LMA in the three groups at the three points (P < 0.01) except group 2 at the low point. In group 2 and group 3, the OI was lower than that in group 1 after LMA insertion at the high point (P < 0.0167). At the middle point, after LMA insertion, the proportion of the simulated needle cross the IJV significantly decreased in all the three groups (P < 0.05), and the proportion in group 2 was higher than that in group 3 (P < 0.0167). The proportion of the simulated needle cross the CCA or both the IJV and CCA significantly increased in group 1 and group 2 (P < 0.05), which increased with no statistical significance in group 3. After the LMA insertion, the cross-sectional area of the IJV significantly increased, while the blood flow velocity significantly decreased (P < 0.01). There was no significant difference between the three groups.
The placement of Supreme, Guardian and I-gel LMA can increase OI, reduce the success rate of IJV puncture, increase the incidence of arterial puncture, and cause congestion of IJV. Type of LMA did not influence the difficulty of IJV puncture. Therefore when LMA is used, ultrasound is recommended to guide the IJV puncture.
With the popularity of LMA for the management of clinical anesthesia, we should pay more attention to the influence of the LMA on the position and blood flow of the IJV. The best type and proper pressure of the cuff of the LMA, which cause minor effects on the position and blood flow of the IJV, should be the subject of further investigations.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Asselah T, Salami A S-Editor: Wang JL L-Editor: Filipodia E-Editor: Qi LL
| 1. | Dumas GA, Bryant AS, Ibey J, Long JA, Vicinanzo MG, Boyd GL. Safety Comparison of Laryngeal Mask Use With Endotracheal Intubation in Patients Undergoing Dacryocystorhinostomy Surgery. Ophthalmic Plast Reconstr Surg. 2018;34:324-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Kang SH, Park M. Comparison of early postoperative recovery between laryngeal mask airway and endotracheal tube in laparoscopic cholecystectomy: A randomized trial. Medicine (Baltimore). 2019;98:e16022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Ludeña JA, Bellas JJA, Rementeria RA, Muñoz Alameda LE. Assessment of awake i-gel™ insertion for fiberoptic-guided intubation in patients with predicted difficult airway: A prospective, observational study. J Anaesthesiol Clin Pharmacol. 2018;34:490-495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Drew T, Khan W, McCaul C. The effect of i-gel® insertion on the accuracy of cricothyroid membrane identification in adult females: a prospective observational study. Br J Anaesth. 2019;123:392-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Miller KA, Nagler J. Advances in Emergent Airway Management in Pediatrics. Emerg Med Clin North Am. 2019;37:473-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Thomsen JLD, Nørskov AK, Rosenstock CV. Supraglottic airway devices in difficult airway management: a retrospective cohort study of 658,104 general anaesthetics registered in the Danish Anaesthesia Database. Anaesthesia. 2019;74:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | English IC, Frew RM, Pigott JF, Zaki M. Percutaneous catheterisation of the internal jugular vein. Anaesthesia. 1969;24:521-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 121] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Tseng KY, Tsai CJ, Wu SH, Lu DV, Hsu HT, Lu IC, Chu KS. Accuracy of the central landmark for catheterization of the right internal jugular vein after placement of the ProSeal laryngeal mask airway. Acta Anaesthesiol Taiwan. 2009;47:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Takeyama K, Kobayashi H, Suzuki T. Optimal puncture site of the right internal jugular vein after laryngeal mask airway placement. Anesthesiology. 2005;103:1136-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Lenoir RJ. Venous congestion of the neck; its relation to laryngeal mask cuff pressures. Br J Anaesth. 2004;93:476-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Sulek CA, Gravenstein N, Blackshear RH, Weiss L. Head rotation during internal jugular vein cannulation and the risk of carotid artery puncture. Anesth Analg. 1996;82:125-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | White A, Sinclair M, Pillai R. Laryngeal mask airway for coronary artery bypass grafting. Anaesthesia. 1991;46:234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Pennant JH, Pace NA, Gajraj NM. Role of the laryngeal mask airway in the immobile cervical spine. J Clin Anesth. 1993;5:226-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 53] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Martens P. The use of the laryngeal mask airway by nurses during cardiopulmonary resuscitation. Anaesthesia. 1994;49:731-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Samarkandi AH, Seraj MA, el Dawlatly A, Mastan M, Bakhamees HB. The role of laryngeal mask airway in cardiopulmonary resuscitation. Resuscitation. 1994;28:103-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Nandwani N, Fairfield MC, Krarup K, Thompson J. The effect of laryngeal mask airway insertion on the position of the internal jugular vein. Anaesthesia. 1997;52:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Troianos CA, Kuwik RJ, Pasqual JR, Lim AJ, Odasso DP. Internal jugular vein and carotid artery anatomic relation as determined by ultrasonography. Anesthesiology. 1996;85:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 143] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Nandi PR, Nunn JF, Charlesworth CH, Taylor SJ. Radiological study of the Laryngeal Mask. Eur J Anaesthesiol Suppl. 1991;4:33-39. [PubMed] |
| 19. | Domino KB, Bowdle TA, Posner KL, Spitellie PH, Lee LA, Cheney FW. Injuries and liability related to central vascular catheters: a closed claims analysis. Anesthesiology. 2004;100:1411-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 154] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 20. | Colbert SA, O'Hanlon DM, Flanagan F, Page R, Moriarty DC. The laryngeal mask airway reduces blood flow in the common carotid artery bulb. Can J Anaesth. 1998;45:23-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |