Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4226
Peer-review started: August 17, 2019
First decision: September 23, 2019
Revised: October 20, 2019
Accepted: November 19, 2019
Article in press: November 19, 2019
Published online: December 26, 2019
Processing time: 129 Days and 21.7 Hours
Branches of the lateral circumflex femoral artery (LCFA) stretch across the surgical field during a direct anterior total hip arthroplasty. It is an anatomical marker in direct anterior approach. As an important vessel around the hip joint, this vessel was ligated in most situations. Although ligation of the vascular pedicle of the LCFA is a common, traditional procedure used to decrease bleeding, the ligation of the pedicle of the vessel is tedious and time-consuming.
To explore whether this ligation is truly necessary in a direct anterior approach to total hip arthroplasty.
This single-center, single-surgeon, prospective study was performed to compare patients’ bleeding undergoing ligation of the branches of the LCFA pedicle (group A) vs those treated with electrocautery from the branches of the LCFA (group B). In both groups, the pedicles were identified in the intermuscular plane between the tensor fasciae lata and the rectus femoris muscles. In group A, the pedicles were ligated with a silk ligature. In group B, the branches coming off the LCFA were controlled with electrocautery. We compared preoperative vs postoperative changes in blood hemoglobin levels, intraoperative blood loss, operative time, rates of transfusion, re-bleeding, and hematoma between the two groups.
The reduction of hemoglobin in group A was 20.9 ± 7.0, and in group B it was 21.2 ± 4.9. There was no statistically significant difference between the two groups (P > 0.05). The actual calculated blood loss in group A was 784 ± 125 mL, and in group B it was 722 ± 153 mL. There was a trend in group A having more blood loss (P = 0.078). The estimated blood loss in group A was 344 ± 88 mL, and in group B it was 346 ± 73 mL. There was no statistically significant difference between the two groups (P = 0.883). In addition, there were no significant differences in the rates of postoperative transfusion (10% vs 6.7%, P > 0.05), postoperative hematomas (6.7% vs 13.3%, P > 0.05), or re-bleeding (13.3% vs 20%, P > 0.05) between the two groups.
Ligation of the pedicle of the LCFA has no advantage in preventing or decreasing bleeding during or after a total hip arthroplasty using the direct anterior approach. Ligation of the pedicle of the vessel is a cumbersome, unnecessary procedure and can be replaced by electrocautery control of the branches off this artery that course through the surgical field.
Core tip: Most surgeons ligate the ascending branch of the lateral circumflex femoral artery during direct anterior total hip arthroplasty, but it may not be necessary. In our study, ligation of the lateral femoral circumflex artery does not reduce bleeding in direct anterior total hip arthroplasty and can be replaced by electrocautery.
- Citation: Zhao GY, Wang YJ, Xu NW, Liu F. Dissection and ligation of the lateral circumflex femoral artery is not necessary when using the direct anterior approach for total hip arthroplasty. World J Clin Cases 2019; 7(24): 4226-4233
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4226.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4226
Hemorrhage during a total hip arthroplasty (THA) involves an expected blood loss as well as perioperative “hidden blood loss”[1-4]. Specific measures designed to minimize blood loss are important not only to decrease unnecessary bleeding, but also to promote a more rapid, functional recovery and to decrease the need for blood transfusion[5,6]. The direct anterior approach (DAA) to performing a THA utilizes an approach via the intermuscular plane, which is designed to minimize muscle damage and blood loss. Moreover, this approach is associated with accelerated postoperative recovery and low rates of dislocation.
The lateral circumflex femoral artery (LCFA) arises from the profunda femoris artery or the femoral artery and supplies blood to the inferior-medial cortex of the femoral neck and the periarticular soft tissues. In most cases, the LCFA usually divides into an ascending and a descending branch; however, in some patients, the LCFA has a third, transverse branch[7-10]. During a DAA, the ascending and transverse branches of LCFA span across the incision between the distal and the middle third of this approach. Most surgeons believe that these vessels are involved in extra blood loss and therefore believe that their ligation is necessary to minimize otherwise unnecessary bleeding[11-14]. Their control via ligation of their pedicle is a troublesome procedure for orthopedists, requiring a bit of extra time and effort to dissect the pedicle.
The aim of this study was to investigate whether ligation of the pedicle of the LCFA will decrease blood loss and lead to better surgical results compared to electrocauterization of the branches off the LCFA.
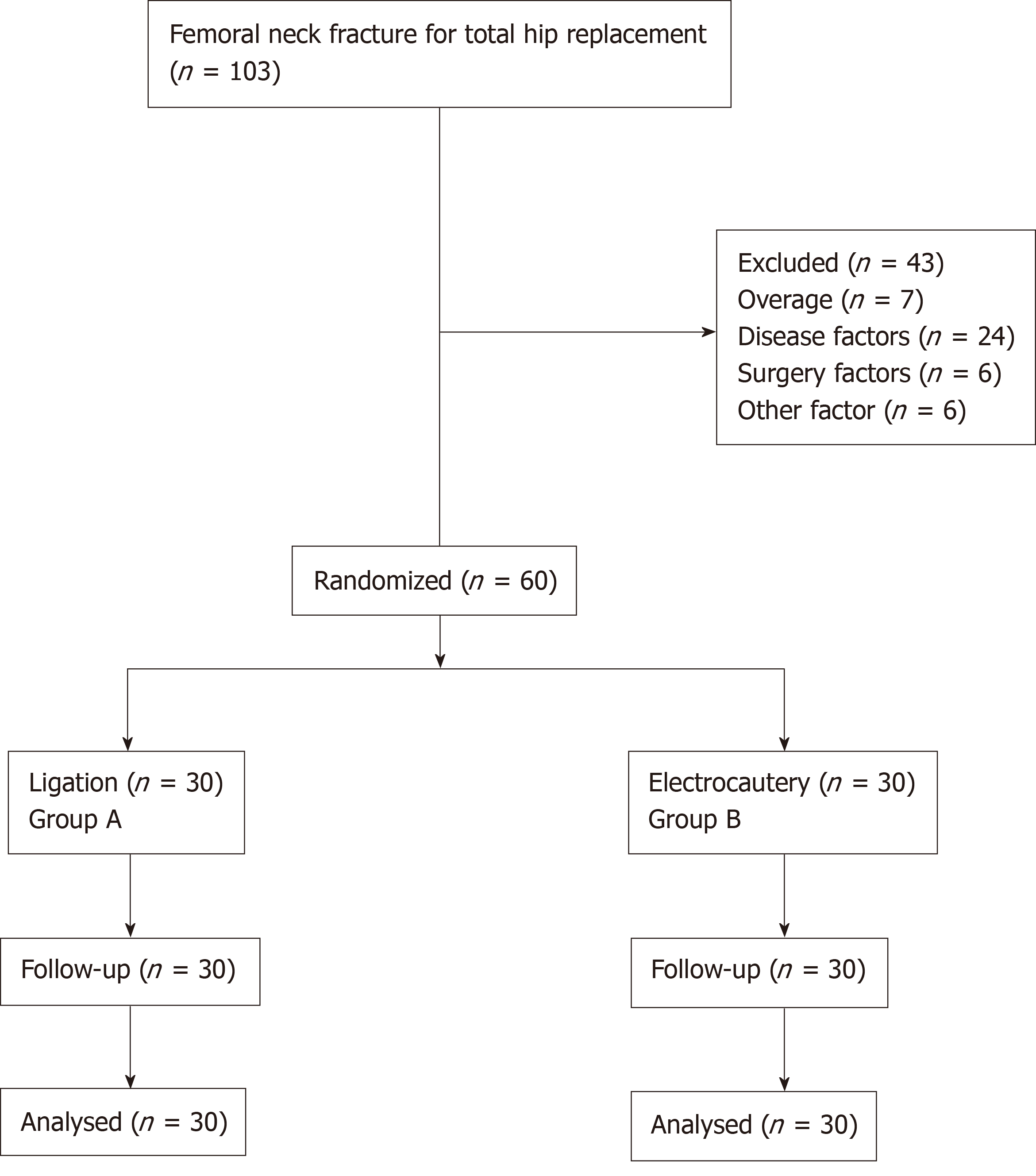
We conducted a 2-year study of 103 patients with femoral neck fractures undergoing a THA via a DAA from October 2016 to October 2018. Patients older than 90 years (n = 7) were excluded. Patients who had a history of stroke (n = 10), hepatic or renal failure (n = 3), coagulation abnormalities (n = 4), taking anticoagulants (n = 6), myocardial infarction (n = 3), previous venous thromboembolism (n = 4), and surgery lasting more than 90 min or had an unexpected condition, such as an intraoperative fracture (n = 6) were also excluded.
In the end, 60 patients were enrolled in the study, ranging in age from 52- to 87-years-old. Patients were numbered according to the order of admission. Patients with an odd number were included in group A, and patients with even number were included in group B. The patients were assigned to groups by a supervisor nurse who did not know the surgery situation. Patients who underwent ligation of the pedicle comprised Group A; those whose branches off the LCFA were treated by electrocautery comprised Group B. Approval for this study was obtained from the Institutional Review Board committees of the authors’ affiliated institutions. The patients were informed of the intraoperative vascular management and signed the informed consent after obtaining the consent. Patients were blinded of their grouping.
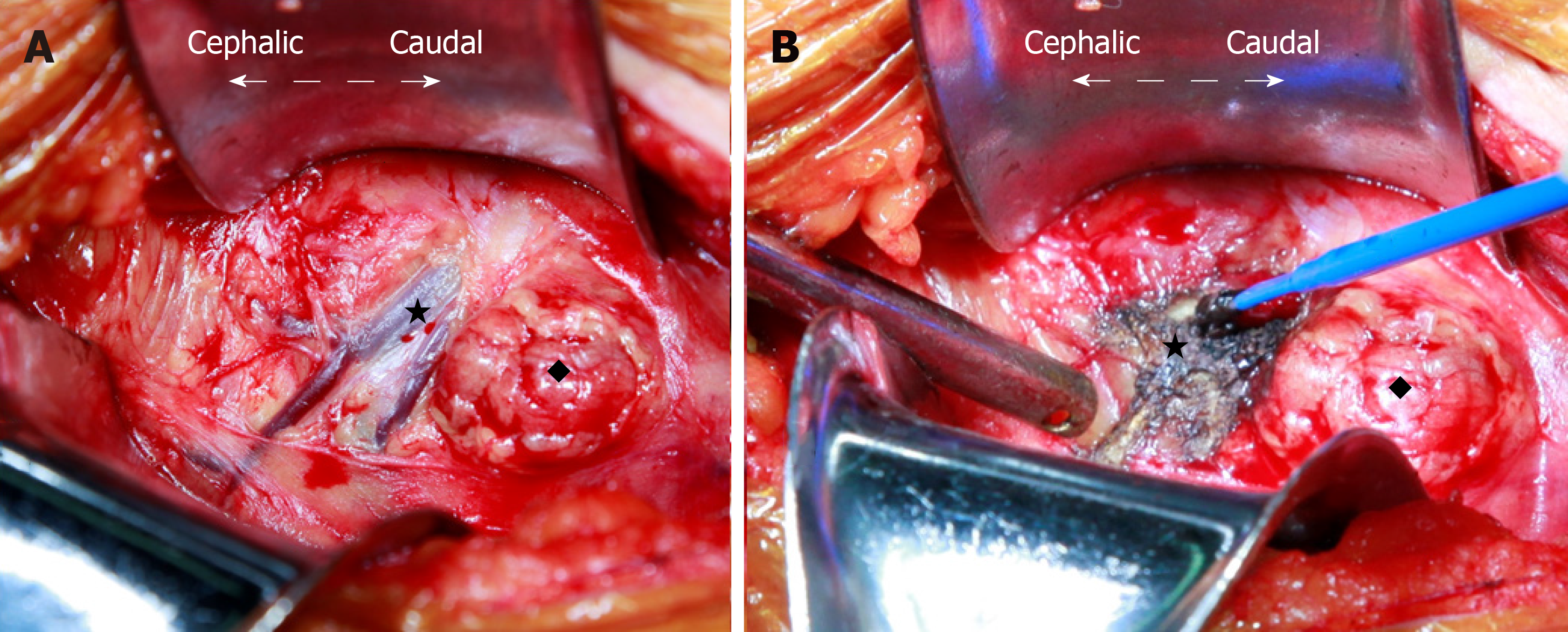
For this DAA approach, a vertical incision was made over the medial edge of the tensor fasciae lata muscle (TFLM). After the location of the TFLM was confirmed, the overlying fascia was incised and the plane between the TFLM and rectus femoris muscles was identified and dissected with retraction of the TFLM laterally. The branches of the LCFA were seen to course anterior to the underlying fat (Figure 1A). The pedicle of the LCFA in group A was ligated with silk suture material and transected; this maneuver required dissection of their pedicles deep into the wound. In group B, the branches off the LCFA were controlled with electrocautery set at a power of 55 W. Electrocautery was easily and rapidly carried out along the blood vessels, and satisfactory hemostasis was evident (Figure 1B).
All operations were performed by the same group of surgeons using the DAA. Each patient received a cementless hip stem prosthesis and a cementless acetabular cup from a single manufacturer (Waldemar Link Gmbh and Co, Hamburg, Germany). After the operation, all patients received subcutaneous injections of 4100 IU of low molecular weight heparin calcium once a day and application of mechanical intermittent pneumatic compression devices in bed twice a day (30 min each time) to prevent venous thromboembolism. All patients started to walk with a walking aid within 24 h of surgery.
We measured the decrease in hemoglobin (Hgb), estimated intraoperative blood loss, actual (calculated) blood loss, transfusion rate, re-bleeding rate, and hematoma rate. The decrease in Hgb was associated with changes in Hgb concentrations between the preoperative value and the values at 48 h postoperative. The actual blood loss was calculated using the equation: Actual blood loss = blood volume [preoperative hematocrit - postoperative hematocrit]/[mean hematocrit], where blood volume = body weight in kilograms × 70 mL/kg[15].
The estimated blood loss was determined from the anesthesia record and postoperative drainage. The indications for transfusion were Hgb < 7 g/L and/or hematocrit < 22 in patients less than 75 years of age. In contrast, patients older than 75 years with Hgb < 9 g/L were given transfusions if the clinical evaluation showed tachycardia, poor urine output, hypotension, fatigue, light-headedness, or other symptoms of acute anemia as determined by the postoperative team. The duration of the operation was determined from the anesthesia record. The relevant clinical data were collected by a single observer, who was blinded to the patient’s operative approach.
Data were recorded and collected into an Excel database (Microsoft). Statistical analysis was performed using GraphPad Prism 5. All variables were analyzed using a paired Student’s t test except the rates of transfusion, hematoma, re-bleeding, and prosthetic loosening, which were analyzed using Fisher’s exact test. Statistical significance was defined at P < 0.05. All variables were analyzed by an independent orthopedist who was not part of the operative team, was blinded to the patient groups, and who received no funding, has no competing interests, and confirmed the accuracy of the findings.
From October 2016 to October 2017, 103 patients scheduled for a primary THA with a single surgeon were screened and assessed for eligibility. Forty-three of the patients were excluded for failing to meet the selection criteria. After randomization, 60 patients (30 patients in group A; 30 patients in group B) were included in the statistical analysis of our trial (Figure 2). The patients were evenly matched in demographics (Table 1). There were no statistically significant differences in body mass index, age, or sex (all P values were > 0.05).
| Group A | Control B | t-test | P value | |
| Age (yr) | 71 (9) | 71 (9) | 0.447 | 0.657 |
| Male, n (%) | 11 (37) | 8 (27) | - | |
| BMI (kg/m2) | 24.0 (2.6) | 24.0 (2.5) | 0.092 | 0.927 |
There were no statistically significant differences in the decrease of Hgb between group A and group B (20.9 ± 7.0 g vs 21.2 ± 4.9 g, respectively; P = 0.805) and the actual calculated blood loss (784 ± 125 mL vs 722 ± 152 mL). However, there was a trend in group A towards having more blood loss (P = 0.078). However, this trend did not explain the problem, and the difference would be narrowed after the sample size increased. The estimated blood loss (344 ± 88 mL vs 346 ± 73 mL; P > 0.5) did not show significant differences. Importantly, there were no statistically significant differences between the two methods in the rate of blood transfusion, hematoma, or re-bleeding (P > 0.2 for each) (Table 2).
DAA is associated with less trauma than the posterolateral approach for THA. Because it is a less traumatic approach, finding a method to address the relevant blood vessels to prevent unnecessary bleeding during the operation is particularly important. In the posterolateral approach, the pedicle to be ligated is the medial circumflex femoral artery. Chiron et al[6] reported that ligation of the pedicle of the medial circumflex femoral artery can decrease bleeding effectively during a posterolateral approach. In the DAA, the ascending branch of LCFA is the important vessel in the surgical field and must be controlled. The LCFA originates from the profunda femoris artery or the common femoral artery. The ascending branch continues along the capsule and crosses the hip joint to supply the anterolateral capsule and thereby crosses the operative field in a DAA[16,17]. Because it is the donor and must be anastomosed by vascularized grafts in the treatment of osteonecrosis of the femoral head, the ascending branch also can be used as both a pedicle and free flap. Because the LCFA provides a less plentiful blood supply than the medial circumflex femoral artery, ligating it does not appear to have any pronounced negative effects[10,18,19].
Previous studies have described a number of surgical procedures and techniques during a DAA, but few works have focused on the treatment of this troublesome vessel[15,20-22]. Our study compared the consequences of two methods of dealing with the ascending branch of LCFA during a DAA and demonstrated that formal ligation of the ascending branch of the LCFA is unnecessary. Electrocautery is a simple and effective method to control this vessel; electrocautery can transect the vessel without causing bleeding, which simplifies the procedure. In the ligation group, there was no increased risk of re-bleeding or hematoma, suggesting that it is a relatively safe hemostatic technique and can replace the dissection of and subsequent ligation of its pedicle as a means of preventing unnecessary bleeding from the ascending branch of the LCFA.
We emphasize that our study did not include patients with coagulation disorders, hematologic disorders, or other related diseases affecting coagulation. For these patients, whether suture ligating the vessel is safe and effective still needs further verification. This study should be supplemented by a larger, randomized study to verify these preliminary conclusions.
Leaving the lateral circumflex pedicle unligated and addressing any bleeding using electrocauterization alone does not increase blood loss in the perioperative period and does not increase the incidence of postoperative hematomas in patients undergoing THA by a DAA. Although ligation did not significantly increase the operative time, it did require some additional time and effort, while offering no obvious benefit. Therefore, it is unnecessary to ligate the LCFA during a DAA.
Direct anterior approach total hip arthroplasty is widely accepted and becoming more and more popular all over the world. More orthopedists have switched from posterior to anterior approaches. Although the procedure is generally the same, no consensus has been reached on some details.
In the direct anterior approach, there are different opinions on the treatment of the ascending branch of the lateral femoral circumflex artery. The hope is that these studies will lead to a consensus on some of the details of direct anterior approach total hip arthroplasty.
Whether ligation of the ascending branch of the lateral femoral circumflex artery during direct anterior approach total hip arthroplasty is advantageous in reducing bleeding and whether this procedure is necessary.
The manuscript compared the surgical bleeding, hemoglobin reduction, hematoma rate, and other indicators of two groups that received different treatments for the ascending branch of the lateral femoral circumflex artery during direct anterior approach total hip arthroplasty.
According to the results, the ligation of the ascending branch of the lateral femoral circumflex artery was not a necessary procedure. Electrocautery is a simple and effective method. However, due to the small sample size and short follow-up time, further observation is needed to see whether there is any difference between the two treatment methods.
The intraoperative and postoperative blood loss were calculated to indirectly reflect vascular bleeding. Excision of the ascending branch of the lateral femoral artery by electrocautery did not increase bleeding. In the treatment of the ascending branch of the lateral circumflex femoral artery, cumbersome ligation can be replaced by electrocoagulation.
Ligation is unnecessary and should be replaced by electrocautery in the treatment of the lateral circumflex femoral artery during the direct anterior approach total hip arthroplasty.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Widmer KH S-Editor: Gong ZM L-Editor: Filipodia E-Editor: Liu MY
| 1. | Borgen PO, Dahl OE, Reikerås O. Blood loss in cemented THA is not reduced with postoperative versus preoperative start of thromboprophylaxis. Clin Orthop Relat Res. 2012;470:2591-2598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Bao N, Zhou L, Cong Y, Guo T, Fan W, Chang Z, Zhao J. Free fatty acids are responsible for the hidden blood loss in total hip and knee arthroplasty. Med Hypotheses. 2013;81:104-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Johansson T, Engquist M, Pettersson LG, Lisander B. Blood loss after total hip replacement: a prospective randomized study between wound compression and drainage. J Arthroplasty. 2005;20:967-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B. Hidden blood loss after total hip arthroplasty. J Arthroplasty. 2011;26:1100-1105.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 144] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 5. | Alshryda S, Mason J, Sarda P, Nargol A, Cooke N, Ahmad H, Tang S, Logishetty R, Vaghela M, McPartlin L, Hungin AP. Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total hip replacement: a randomized controlled trial (TRANX-H). J Bone Joint Surg Am. 2013;95:1969-1974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Chiron P, Murgier J, Reina N. Reduced blood loss with ligation of medial circumflex pedicle during total hip arthroplasty with minimally invasive posterior approach. Orthop Traumatol Surg Res. 2014;100:237-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Gradman WS. Bypass to the lateral circumflex femoral artery. Ann Vasc Surg. 1992;6:344-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Goel S, Arora J, Mehta V, Sharma M, Suri RK, Rath G. Unusual disposition of lateral circumflex femoral artery: Anatomical description and clinical implications. World J Clin Cases. 2015;3:85-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Vuksanovic-Bozaric A, Radojevic N, Muhovic D, Abramovic M, Radunovic M. Significance of anatomical variations of the lateral circumflex femoral artery for the tensor fasciae latae flapping. Folia Morphol (Warsz). 2015;74:389-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Zlotorowicz M, Czubak-Wrzosek M, Wrzosek P, Czubak J. The origin of the medial femoral circumflex artery, lateral femoral circumflex artery and obturator artery. Surg Radiol Anat. 2018;40:515-520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Post ZD, Orozco F, Diaz-Ledezma C, Hozack WJ, Ong A. Direct anterior approach for total hip arthroplasty: indications, technique, and results. J Am Acad Orthop Surg. 2014;22:595-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 224] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 12. | De Geest T, Vansintjan P, De Loore G. Direct anterior total hip arthroplasty: complications and early outcome in a series of 300 cases. Acta Orthop Belg. 2013;79:166-173. [PubMed] |
| 13. | Cadossi M, Sambri A, Tedesco G, Mazzotti A, Terrando S, Faldini C. Anterior Approach in Total Hip Replacement. Orthopedics. 2017;40:e553-e556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Connolly KP, Kamath AF. Direct anterior total hip arthroplasty: Literature review of variations in surgical technique. World J Orthop. 2016;7:38-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Horne PH, Olson SA. Direct anterior approach for total hip arthroplasty using the fracture table. Curr Rev Musculoskelet Med. 2011;4:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Burusapat C, Nanasilp T, Kunaphensaeng P, Ruamthanthong A. Effect of Atherosclerosis on the Lateral Circumflex Femoral Artery and Its Descending Branch: Comparative Study to Nonatherosclerotic Risk. Plast Reconstr Surg Glob Open. 2016;4:e856. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Kalhor M, Horowitz K, Gharehdaghi J, Beck M, Ganz R. Anatomic variations in femoral head circulation. Hip Int. 2012;22:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Nakano N, Lisenda L, Khanduja V. Pseudoaneurysm of a branch of the femoral circumflex artery as a complication of revision arthroscopic release of the iliopsoas tendon. SICOT J. 2017;3:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Seeley MA, Georgiadis AG, Sankar WN. Hip Vascularity: A Review of the Anatomy and Clinical Implications. J Am Acad Orthop Surg. 2016;24:515-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Manrique J, Chen AF, Heller S, Hozack WJ. Direct anterior approach for revision total hip arthroplasty. Ann Transl Med. 2014;2:100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 21. | Ochi H, Baba T, Homma Y, Matsumoto M, Watari T, Ozaki Y, Kobayashi H, Kaneko K. Total hip arthroplasty via the direct anterior approach with a dual mobility cup for displaced femoral neck fracture in patients with a high risk of dislocation. SICOT J. 2017;3:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Tamaki T, Oinuma K, Miura Y, Shiratsuchi H. Total hip arthroplasty through a direct anterior approach for fused hips. Hip Int. 2015;25:549-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |