Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4196
Peer-review started: September 8, 2019
First decision: November 11, 2019
Revised: November 24, 2019
Accepted: November 27, 2019
Article in press: November 27, 2019
Published online: December 26, 2019
Processing time: 108 Days and 8.5 Hours
Knee osteoarthritis is the most prevalent form of osteoarthritis and is becoming the main reason for progressive pain in knee joints. Arthroscopy combined with unicondylar knee arthroplasty (UKA) is one of the effective methods for the treatment of severe unicompartmental knee arthritis. This surgical approach gives us the capacity to explore all the articular cavities and plays a vital role in UKA patient selection. However, some scholars think that the surgical procedure is traumatic and may increase the rate of surgical infection, and its clinical efficacy needs further study.
To compare the clinical effect of arthroscopy combined with UKA and UKA alone for patients suffering from unicompartmental osteoarthritis (OA).
A retrospective study was conducted on patients who were diagnosed with unicompartmental OA (Kellgren–Laurence grade ≥ III) and underwent UKA between October 2012 and November 2006. The patients were followed at 3, 6, and 12 mo and every 2 years thereafter. During each follow-up, the radiographic materials, the range of motion of knee and hospital for special surgery (HSS) score, knee society score and knee function score as recorded, and the modes and time of failure and revision details were collected as well.
Data on 104 patients (118 knees), including 54 patients (60 knees) in the arthroscopy combined with UKA group (group A) and 51 (58 knees) in UKA alone group (group B) were collected during an average follow-up duration of 7.25 years, excluding the cases who were lost to follow-up. At the final follow-up, 3 (5.0%) of 60 knees in group A compared with 4 (6.9%) of 58 knees in group B failed and converted to total knee arthroplasty, with no statistically significant difference between the two groups (P = 0.933). The percentage of patients receiving blood transfusion was 40% in group A, significantly lower than that in group B (67.2%; P = 0.003). Total volume of blood transfusion in group A was also significantly lower than that of group B (P = 0.001). Both groups improved significantly after operation in clinical symptoms and functions. HSS score, knee society score, and knee function score increased significantly at the latest follow-up compared to pre-operation in group A, from 59.6 ± 10.9 to 82.7 ± 9.3 (mean difference [MD], 23.2; 95%CI: 19.3-27.0; P = 0.000), 47.3 ± 6.3 to 76.2 ± 13.1 (MD, 28.9; 95%CI: 25.1-32.7; P = 0.000), and 57.5 ± 6.3 to 75.1 ± 19.6 (MD, 17.5; 95% CI: 12.1-23.0; P = 0.000); and in group B, from 59.3 ± 15.6 to 84.3 ± 10.1 (MD, 23.7; 95%CI: 18.9-28.5; P = 0.000), 49.1 ± 9.2 to 75.1 ± 13.2 (MD, 24.7; 95%CI: 19.9-29.5; P = 0.000), and 59.3 ± 9.0 to 77.4 ± 13.8 (MD, 17.2; 95%CI: 12.8-21.6; P = 0.000).
Arthroscopy combined with UKA and UKA alone both provide benefits in clinical symptom improvement and alignment correction. Arthroscopy combined with UKA does not increase the infection probability and surgical complications, and has an advantage in reducing the total volume of blood transfusion and the percentage of patients receiving blood transfusion.
Core tip: The aim of this study was to compare the clinical effects of arthroscopy combined with unicondylar knee arthroplasty (UKA) and UKA alone for patients suffering from unicompartmental osteoarthritis during an average follow-up duration of 7.25 years. The hospital for special surgery score, knee society score, knee function score, femoral-tibial angle, and hip-knee-ankle angle increased significantly at the latest follow-up compared to pre-operation in both groups. The percentage of patients receiving blood transfusion (P = 0.003) and the total volume of blood transfusion (P = 0.001) were both significantly lower in the arthroscopy combined with UKA group than in the UKA alone group. Arthroscopic surgery has a unique advantage with regard to patient selection and a curative effect on cartilage degeneration in the lateral compartment.
- Citation: Wang HR, Li ZL, Li J, Wang YX, Zhao ZD, Li W. Arthroscopy combined with unicondylar knee arthroplasty for treatment of isolated unicompartmental knee arthritis: A long-term comparison. World J Clin Cases 2019; 7(24): 4196-4207
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4196.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4196
Knee osteoarthritis (KOA) is the most prevalent form of osteoarthritis (OA) and is becoming the main reason for progressive pain in knee joints[1-3]. Severe KOA needs knee arthroplasty[4,5]. However, in patients who received total knee arthroplasty (TKA), around 5%-20% suffered from unicompartmental OA[6]. For these patients, unicondylar knee arthroplasty (UKA) can provide a better clinical curative effect and quicker recovery than TKA[7,8].
The indications for UKA are determined according to clinical symptoms, physical examination, and radiographic information[9-11]. With the development of prosthesis designs and surgery techniques, the indications for UKA are not as strict as before[12,13]. Thompson et al[14] conducted a retrospective study including 229 knees and found that younger patients had better results than older patients and body mass index (BMI) had no direct association with failure rate. It is justified to broaden classic UKA indications owing to the study performed by von Knoch et al[15]. The main reasons for failure in UKA includes the defects on prosthesis design, a lack of experience in surgical techniques, the progression of arthritis, and inadequate patient selection[16]. Emerson et al reported that progression of arthritis in the lateral compartment resulted in a 90% failure rate in UKA[17]. Identifying the injury degree of articular cartilage, meniscus, and anterior cruciate ligament (ACL) can help to improve the clinical curative effects of UKA and lengthen prosthesis longevity.
Applying arthroscopic surgery combined with UKA gives us the capacity to explore all the articular cavities and makes up for the defect of the operation that limits one to a single compartment of UKA, which plays a vital role in UKA patient selection[18]. For patients affected by Outerbridge III or IV cartilage degeneration in patellofemoral joint or lateral compartment newly found through arthroscopic surgery, arthroscopic debridement or TKA could be a better option[19]. Cleaning the damaged cartilage and smoothing the bone surface in the lateral compartment through arthroscopic technique can also improve the clinical curative effects of UKA.
The purpose of this study was to describe the effectiveness of arthroscopy combined with UKA for the treatment of unicompartmental OA as opposed to UKA alone. We hypothesized that arthroscopy combined with UKA can provide better relief in clinical symptoms and alignment and reduce the revision rate simultaneously.
We retrospectively studied 131 knees in 117 patients from November 2006 to October 2012, using either arthroscopy combined with UKA (group A) or UKA alone (group B) for medial unicompartmental OA. The prosthesis selection included the fix-bearing design (Link) and the mobile-bearing design (Oxford; Biomet). Surgeries were conducted by two different surgeons who had more than 10 years of experience. The inclusion criteria were as follows: (1) A clear diagnosis of medial compartmental KOA with Kellgren-Lawrence (K-L) grade III or greater based on radiographic information; (2) Regular articular cartilage coverage or Outerbridge grade I or II in the lateral compartment and a normal status on patellofemoral joint according to clinical tests and radiographs; (3) A varus deformity no more than 10° as well as a flexion contracture less than 15°; (4) A range of motion (ROM) more than 90°; (5) Inefficient and normal function of the ACL and collateral ligaments based on clinical tests and magnetic resonance imaging (MRI); and (6) The willingness to participate in the study and the possibility to be investigated by phone or email to share their health resources with us. The contraindications included rheumatoid arthritis, severe chondrocalcinosis, and a clinically symptomatic patellofemoral joint.
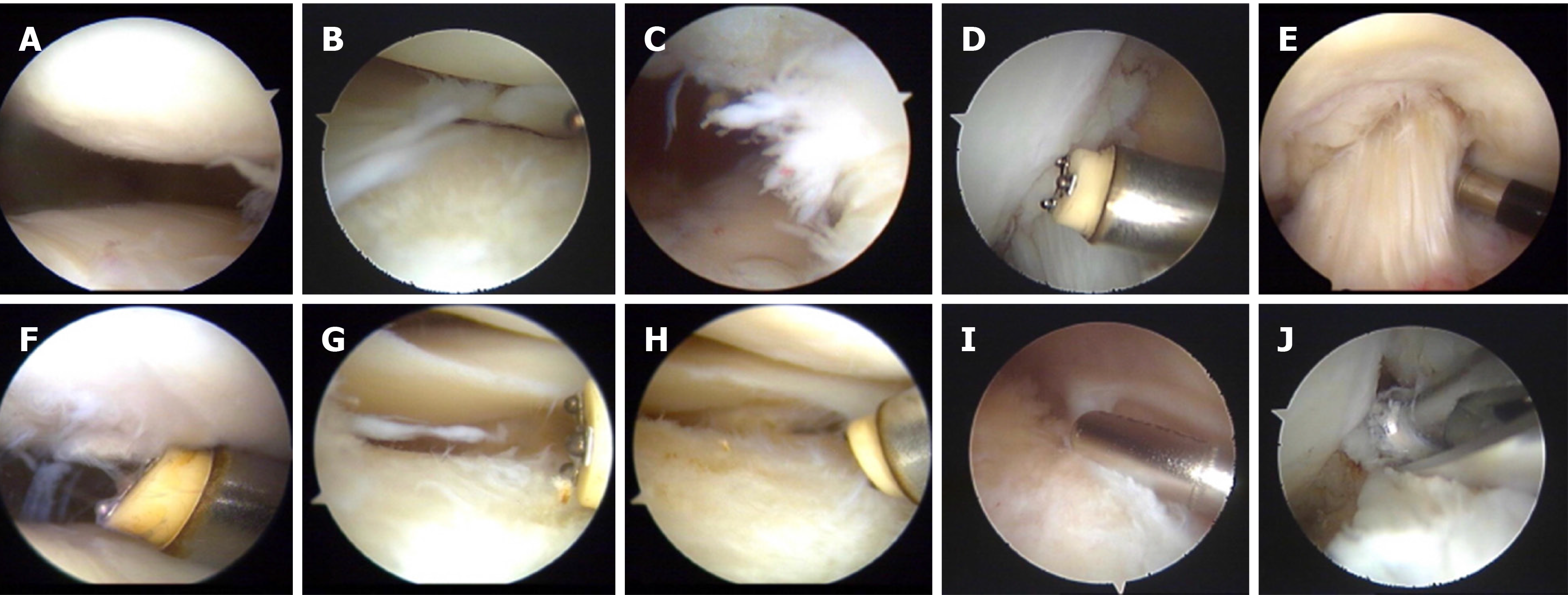
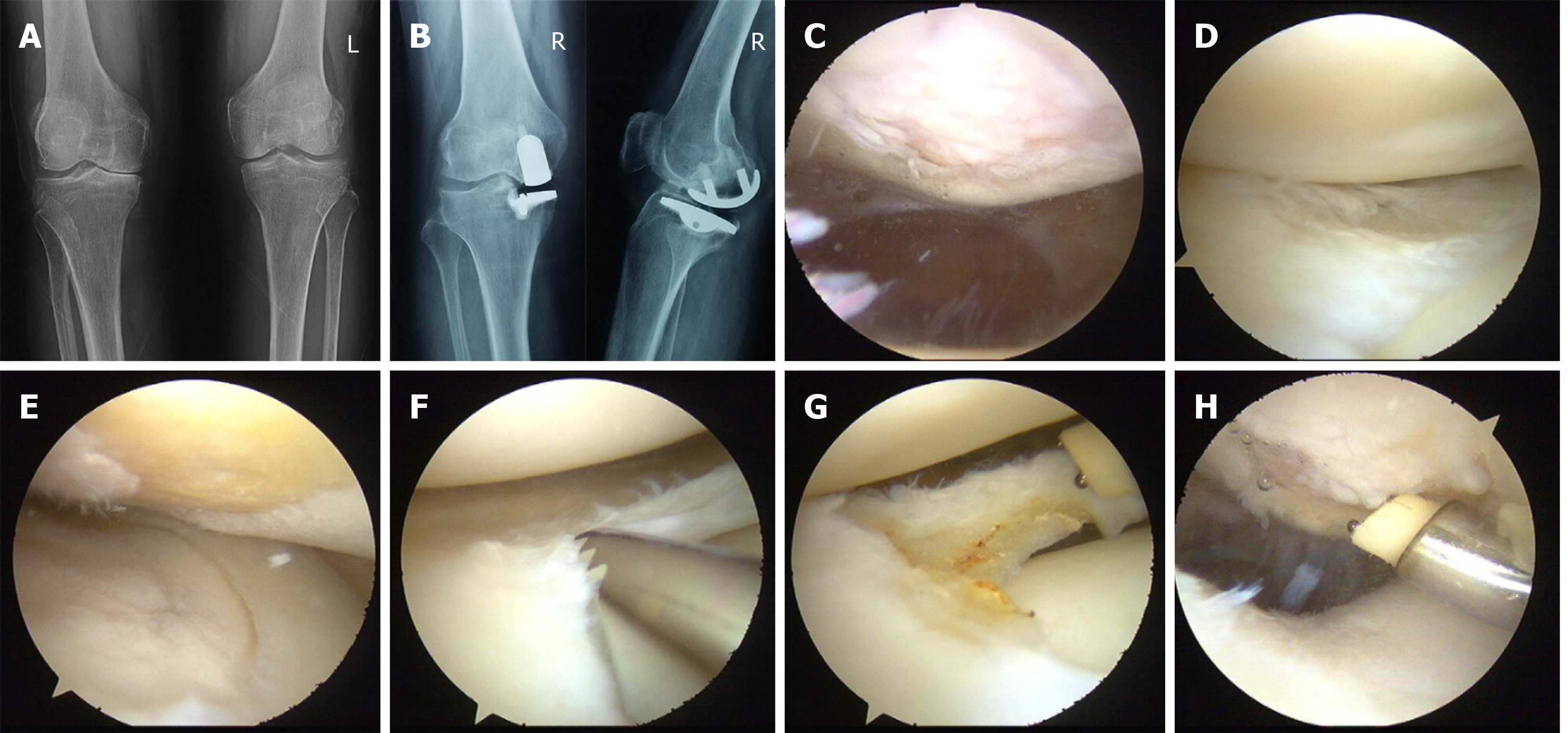
The decision of whether or not to add arthroscopic surgery before UKA was determined according to the patients’ characteristics and surgeons’ preferences. Arthroscopic exploration would be necessary if the radiographic information failed to show the explicit image of ACL or the unreplaced compartment. Every compartment of the articular joint was successively examined (Figure 1A-D), and the tension of the ACL and posterior cruciate ligament was judged with a clasp (Figure 1E). The options for UKA, TKA, or arthroscopic debridement alone were determined according to the cartilage of each compartment. As for the patients who met the criteria of UKA, the arthroscopic operation included synovium excision, cleaning the damaged cartilage, smoothing the bone surface in the lateral compartment through abrasive drilling, and trimming the lateral meniscus with wear or degeneration to make it smooth and slope-shaped (Figure 1F-J).
Minimally invasive surgery (MIS) was adapted for UKA surgery[20]. The drainage tube was kept for 24-48 h and removed when the total draining volume was less than 50 mL. The patients were allowed to start quadriceps femoris muscle and ankle active contraction immediately after the operation. Passive knee contraction on continuous passive motion began 1 d later. Patients were recommended to start partial weight bearing with crutches 3 d after the operation and gradually returned to full weight bearing over the course of 1 wk.
The inpatient information we collected included hospitalization time, hemorrhage during operation, the total volume of blood transfusion, the percentage of patients receiving blood transfusion, and the percentage of patients developing complications after the operation. All patients were assessed preoperatively and at 3, 6, and 12 mo after operation and every 2 years thereafter, including clinical symptoms and radiographic resources, either by phone or physical examination upon return to the clinic. The clinical outcomes were recorded by hospital for special surgery (HSS) score, knee society score, knee function score, and ROM. Radiographic information, including long-leg pictures as well as anterior-posterior and lateral pictures, was evaluated by femoral-tibial angle (FTA) and hip-knee-ankle angle (HKA). The angle between the two mechanical axes represented HKA and was defined as the mechanical axis of the lower limb; the angle between the two anatomy axes represented FTA and was defined as the anatomy axis of the lower limb. According to the Kennedy classification[21], we drew a line from the center of the femur head to the midpoint of the superior articular surface of the talus and judged which part of the tibial plateau the line went through to evaluate the alignment deformity at the latest follow-up. We defined the valgus in area 3, the varus in area 0 or 1, and the alignment correction in area 2 or C. Any type of revision or conversion to TKA was considered a failure, and we used the Kaplan-Meier curve to compare the survival rates.
In this study, continuous data such as age and BMI were normally distributed and are described as the mean ± SD. Inter-group comparisons were performed using the independent sample t-test. Continuous data such as height, body weight, follow-up time, hospitalization time, intraoperative bleeding, and total blood transfusion did not follow a normal distribution and are described by medians (lower quartile and upper quartile). The Mann-Whitney nonparametric test was used for comparison between groups. The paired sample t-test was used to compare paired data including preoperative and postoperative HSS scores, knee society scores, function scores, ROM, HKAs, and FTAs.
With regard to the proportionality data, the Kennedy and White classification, the side, and blood transfusion rates were consistent with the theoretical number (T) ≥ 5 and the total sample size (n) ≥ 40. The test was performed using Pearson’s χ2. Gender, etiology, and postoperative complication rates were in accordance with T < 5 but T ≥ 1 and were tested with a chi-square corrected for continuity.
The Kaplan-Meier curve and log-rank test were used to compare the survivor rates. The analyses were implemented with SPSS software (version 19.0; SPSS Inc., Chicago, IL, United States). P values < 0.05 were considered to indicate a significant difference.
Of all the 117 patients, 104 (118 knees) met the criteria and were followed continuously until the last. Fifty-four patients (60 knees) in group A and 51 patients (58 knees) in group B were included in the study. One patient underwent UKA surgery on both legs. However, arthroscopy was used before the left leg replacement and no arthroscopic surgery was performed on the right leg. The basic characteristics of the patients are shown in Table 1. There was no significant between-group difference in numbers, age, sex, side, BMI, etiology, or follow-up time.
| Characteristic | Group A | Group B | t/Z/X2 | P |
| Number of UKA | 60 | 58 | 0.416 | 0.519 |
| Bilateral surgeries | 6 | 7 | ||
| Age (yr) | 61.2 ± 8.4 | 63.0 ± 8.1 | 1.169 | 0.245 |
| Gender (Male/Female) | 12/48 | 19/39 | 2.478 | 0.115 |
| Side (Left/Right) | 21/39 | 27/31 | 1.631 | 0.212 |
| Height (cm) | 160 (156-163) | 160 (156-167) | 1.190 | 0.234 |
| Weight (kg) | 69.0 (63.0-75.8) | 70.0 (64.5-78.3) | 0.989 | 0.323 |
| Body mass index (kg/m²) | 27.1 ± 3.2 | 27.2 ± 3.5 | 0.167 | 0.868 |
| Etiology (OA/Post-traumatic arthritis) | 57/3 | 55/3 | 0.142 | 0.766 |
| Follow-up period (yr) | 7.08 (6.42-7.83) | 7.08 (6.42-7.83) | 0.100 | 0.921 |
The inpatient information is shown in Table 2. The percentage of patients receiving blood transfusion was 40% in group A, significantly lower than that in group B (67.2%; P = 0.003). The total volume of blood transfusion in group A was also significantly lower than that in group B (P = 0.001). One patient in group A had severe pain in the upper abdomen, and another experienced paroxysmal atrial fibrillation the day after operation (P = 0.491). Both patients recovered and achieved stable condition after symptomatic and supportive treatment.
| Group A | Group B | Z/X2 | P | |
| Hospitalization time (d) | 12.0 (11.0-14.75) | 10.5 (9.0-13.3) | 2.246 | 0.025 |
| Hemorrhage during operation (mL) | 100 (50-100) | 50 (50-100) | 1.484 | 0.138 |
| Total volume of blood transfusion (mL) | 0 (0-350) | 350 (0-565) | 3.325 | 0.001 |
| Percentage of patients receiving blood transfusion (%) | 40 | 67.2 | 8.795 | 0.003 |
| Percentage of patients developing complications after operation (%) | 1.7 | 1.7 | 0.475 | 0.491 |
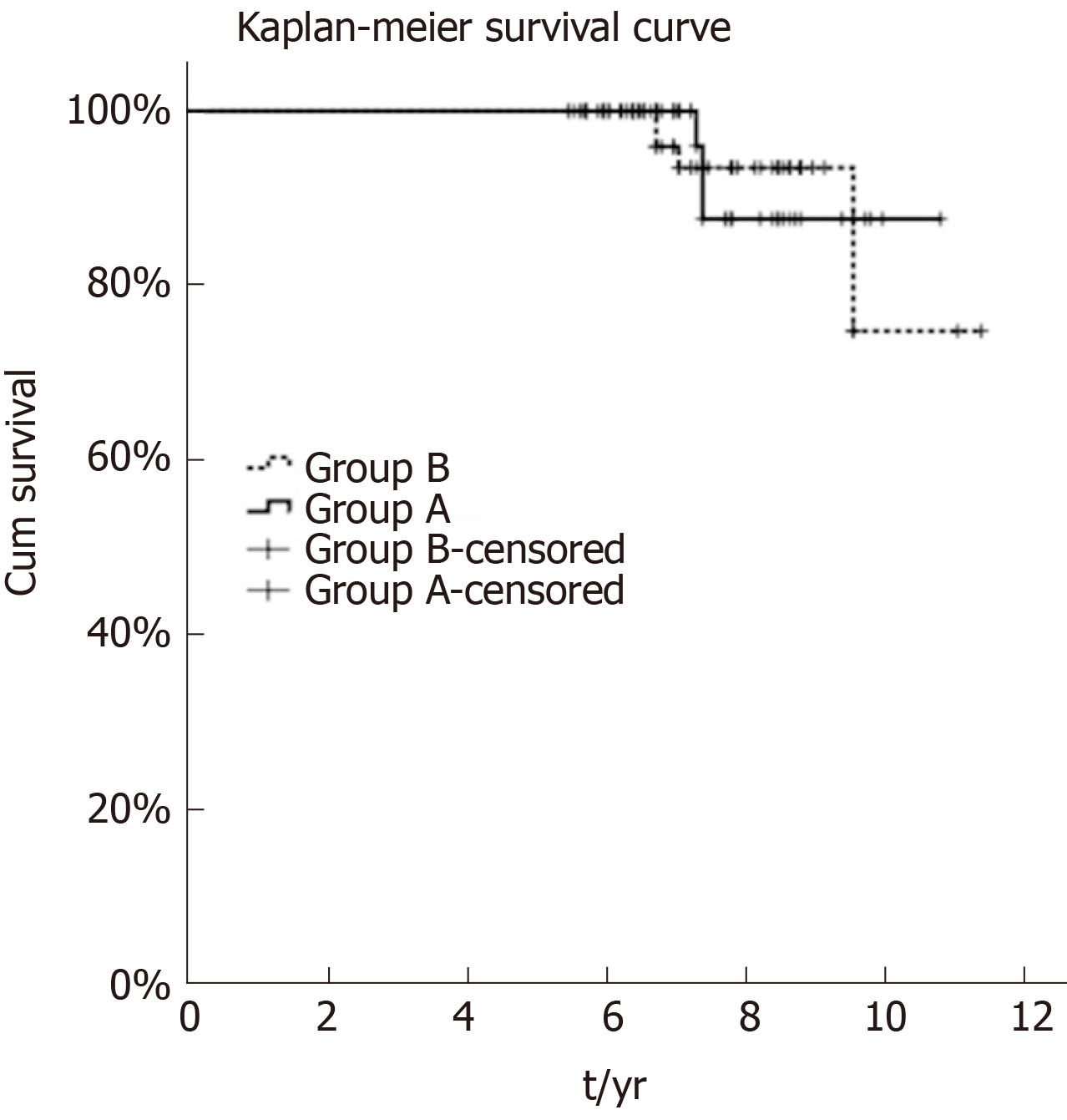
At the last follow-up, three patients in group A received revision with a survivorship of 95%, and four in group B received revision with a survivorship of 93.1%. The outcome showed no statistically significant difference for unicompartmental OA patients receiving the two measures (χ2 = 0.007, P = 0.933). The Kaplan-Meier survival curve is shown in Figure 2. All these patients converted to TKA after failure because of the progression of arthritis, aseptic loosening, and bearing dislocation. The revision detail is shown in Table 3.
| Group | Number of of knees | Mean time to revision (yr) | Follow-up years |
| Group A | |||
| Progression of arthritis | 2 | 6.92 | 7.42 |
| Aseptic loosening | 1 | 6.33 | 7.33 |
| Group B | |||
| Progression of arthritis | 3 | 6.33 | 6.86 |
| Bearing dislocation | 1 | 1 | 9.58 |
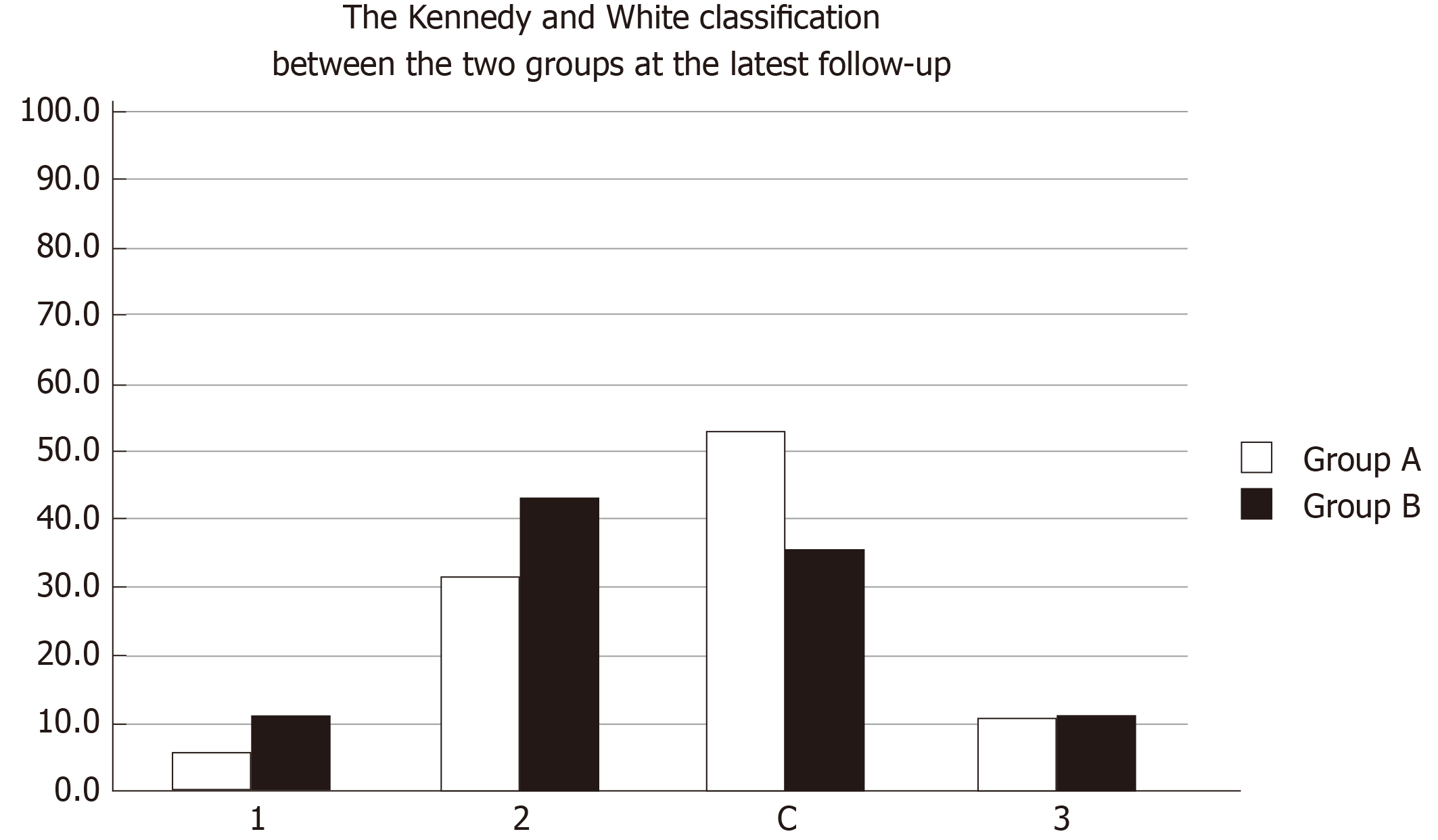
The outcome scores and the radiographic comparison are shown in Table 4. Both groups improved significantly, after operation, in clinical symptoms and functions. However, there was no significant difference between the two groups at the final follow-up in HSS score [mean difference (MD), -1.6; 95%CI: -5.2-2.1; P = 0.392], knee society score (MD, 1.0; 95%CI: -3.9-6.0; P = 0.676), or knee function score (MD, -2.3; 95%CI: -8.7-4.0; P = 0.471). At the last follow-up, the mean FTA was 175.2° ± 2.5° in group A and 175.0° ± 3.7° in group B with no significant difference (MD, 0.2; 95%CI: -1.0-1.4; P = 0.770). The average HKA was closer to 180° in group A but with no significant difference between the two groups (MD, 0.2; 95%CI: -1.0-1.4; P = 0.759). We found more knees getting alignment correction at the last follow-up with a percentage of 84.2% in group A and 77.8% in group B with no significant difference (P = 0.387) according to the Kennedy and White classification (Figure 3).
| Group | Pre-operation | Last follow-up | mean difference (95%CI) | P |
| Group A | ||||
| HSS score | 59.6 ± 10.9 | 82.7 ± 9.3 | 23.2 (19.3-27.0) | 0.000 |
| Knee society score | 47.3 ± 6.3 | 76.2 ± 13.1 | 28.9 (25.1-32.7) | 0.000 |
| Knee function score | 57.5 ± 6.3 | 75.1 ± 19.6 | 17.5 (12.1-23.0) | 0.000 |
| FTA | 179.9 ± 3.5 | 175.2 ± 2.5 | 4.7 (3.5-5.8) | 0.000 |
| HKA | 175.1 ± 2.8 | 176.7 ± 3.1 | 1.6 (0.4-2.7) | 0.008 |
| ROM | 121.5 ± 8.2 | 129.1 ± 11.5 | 7.6 (4.1-11.2) | 0.000 |
| Group B | ||||
| HSS score | 59.3 ± 15.6 | 84.3 ± 10.1 | 23.7 (18.9-28.5) | 0.000 |
| Knee society score | 49.1 ± 9.2 | 75.1 ± 13.2 | 24.7 (19.9-29.5) | 0.000 |
| Knee function score | 59.3 ± 9.0 | 77.4 ± 13.8 | 17.2 (12.8-21.6) | 0.000 |
| FTA | 181.5 ± 5.0 | 175.0 ± 3.7 | 6.2 (4.5-7.8) | 0.000 |
| HKA | 173.9 ± 3.7 | 176.5 ± 3.2 | 2.5 (1.0-4.0) | 0.001 |
| ROM | 116.1 ± 17.3 | 131.1 ± 14.1 | 14.2 (8.7-19.7) | 0.000 |
KOA is a very common chronic arthropathy whose pathogenesis is uncertain, featured as articular cartilage and bone beneath cartilage damage as well as osteophyte proliferation[1,22]. UKA is an effective method for unicompartmental OA[7,8]. UKA in a patient can provide smaller incisions, less trauma and hemorrhage, better conservation of bone stock for revision, better kinematic recovery, and quicker recovery than TKA[23-25]. Reservation of the lateral compartment and ACL results in better proprioception[26-28].
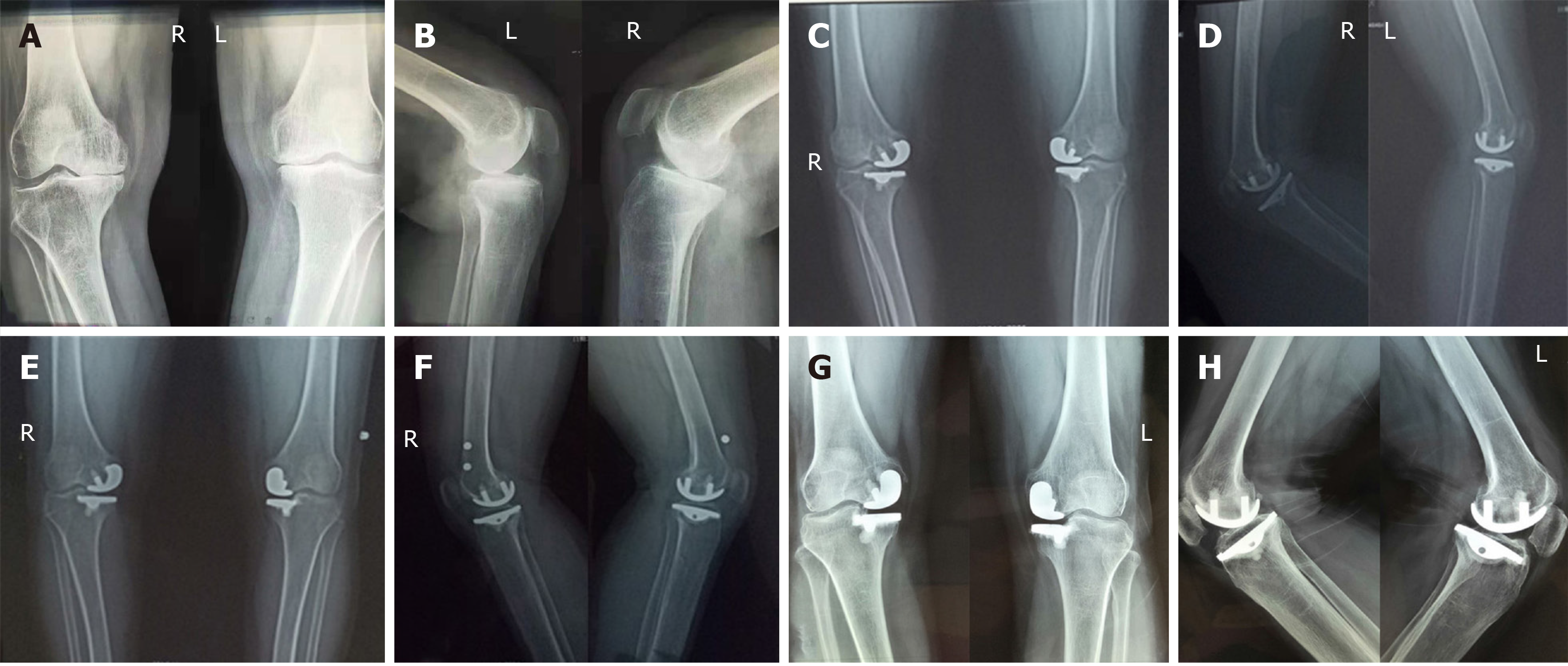
In our study, the average survivor rate of UKA was 95% in group A and 93.1% in group B. It is worth noting that several patients developed severe pain symptoms several years after surgery, and X-rays showed partial loosening of the prosthesis (Figure 4). Out of fear of pain from replacement surgery or other personal reasons, this complaint of the patients has not been treated for the next step. However, because of the small sample size, the contribution of arthroscopic debridement to survivor rate needs further study. Sebastien et al reported a total survivorship of 85.9% in a 20-year retrospective study, and the revision details included progression of arthritis (36.4%), aseptic loosening (22.7%), polyethylene wear (18.2%), and bearing dislocation (13.6%)[29]. Their study did not use the treatment of arthroscopy, which may result in a higher rate of revision than our study, while they did include more patients and longer viewing times. The leading reason for revision was the progression of arthritis, which shows that the diagnoses of the patients were incomplete[30-32]. The wear particle of the component also contributed to this progression[2,30,33]. Therefore, strict patient selection is the key to the effect of operation and the survival rate of the prosthesis for UKA[9,10].
Regarding inpatient information, the percentage of patients receiving blood transfusion was 40% in group A, significantly lower than that in group B (67.2%; χ2 = 8.795, P = 0.003). The total volume of blood transfusion in group A was also significantly lower than that in group B (Z = 3.325, P = 0.001). There was no significant difference between the two groups in hemorrhage during operation. The results showed that arthroscopy combined with UKA did not increase surgical trauma, infection probability, or surgical complications but provided an advantage in reducing the total volume of blood transfusion and the percentage of patients receiving blood transfusion.
At the last follow-up, there was no significant difference between the two groups in HSS score, knee society score, or knee function score. Both groups improved significantly after the operation, which suggests that these two surgical methods provide notable improvement in clinical symptoms and function and thus improve life quality.
At the last follow-up, the mean FTA and HKA showed no significant difference (P = 0.770; P = 0.759). More knees got alignment correction with no significant difference (P = 0.933) according to the Kennedy and White classification[21]. Perkins and Gunckle reported 40 UKA samples and found that the revision rate increased 7 times for varus over 2° or valgus over 6° after operation[34]. Parmaksizoğlu et al[35] studied 38 UKA patients who experienced fine recovery in clinical symptoms and function with an average varus over 1.5°. Controversy remains around the force line correction of UKA. We consider better correction when the force line crosses the joint center or there is slight varus because the excess valgus could lead to progression of arthritis in the lateral compartment while the over-varus would load more pressure on the prosthesis, which could improve the incidence of aseptic loosening and pad wearing.
With the development of surgical techniques and the deeper research in KOA, the indications for UKA are not as strict as before. Cartilage degeneration in the patellofemoral joint and lateral compartment is no longer contraindications of UKA[12,13]. For patients suffering from Outerbridge I or II cartilage degeneration in the patellofemoral joint or lateral compartment as well as an injury in the lateral meniscus, performing arthroscopic surgery before UKA is necessary. Moreover, excision of the synovial membrane, removal of the corpus liberum, and brisement of the patellar retinaculum through arthroscopy could reduce synovitis, cartilage wearing, and pain in the patellofemoral joint (Figure 5). For patients affected by severe cartilage degeneration newly found through arthroscopic surgery, arthroscopic debridement or TKA could be the substitution, which also avoids the limitation of patient selection based only on physical examination and radiographic information.
Of the 54 patients who received arthroscopic operations, 39 had cartilage degeneration at various levels in the patellofemoral joint, 12 had meniscus injury in the lateral compartment, and 27 suffered from cartilage degeneration on the lateral tibial plateau. Most of the patients experienced good recovery after arthroscopic operation, which included trimming the meniscus and articular cartilage and smoothing the bone surface. One failed case suffered from Outerbridge IV cartilage injury on the lateral femoral condyle and Outerbridge I cartilage injury on the lateral tibial plateau and had a survival time of 6.33 years. He accepted TKA on the other leg in 2017, owing to the abuse of his non-UKA leg and acceleration of the progression of arthritis.
The crucial part of UKA is to judge the functional integrity of the ACL, and an ACL-deficient knee should be considered a contraindication[36-38]. For ACL-deficient patients who undergo UKA, the leading reason for revision is aseptic loosening[39,40]. However, most KOA patients had varying degrees of ACL damage. Lee et al studied 107 KOA patients through physical examination and found that 41 (39%) had ACL injury[41]. There is also controversy around the diagnosis of chronic ACL damage using MRI. According to knee prosthesis research conducted by Sharp et al[33], 33% of patients had ACL defects while only 13% of treatments changed to TKA during operation. One explanation for the inaccuracy of MRI could be that MRI provides only imaging diagnosis, which fails to show functional integrity. Meanwhile, the ACL of KOA patients is relaxed and lacks strass during MRI because of cartilage loss. This problem can be solved using the arthroscopic technique. During arthroscopic surgery before UKA, the tension of the ACL can be precisely evaluated. Compared to the MIS incision of UKA, the magnifying image during arthroscopic surgery provides better visualization to judge the blood supply and synovial membrane of the ACL. In our study, no patients in group A had a deficiency or lack of tension in the ACL.
Other advantages of arthroscopic surgery combined with UKA are as follows. First, although arthroscopic surgery increases operation time, infection probability and surgical complications do not increase. In our long-term study, neither infection cases nor surgical complications were found. Second, arthroscopic operation has the same operative position as UKA. Third, the risk of anesthesia and infection can be reduced compared to staged operation.
There remain some limitations in our study. Our study was a single-center retrospective study, which is less persuasive than multiple-center studies. Randomization was not adopted when grouping. Also, the option of receiving arthroscopic surgery was based on operators’ preference. Lastly, the radiographs were not reviewed by multiple observers, which could result in observer error.
In conclusion, this study shows that arthroscopic surgery combined with UKA and UKA alone both provide benefits in patients’ clinical symptom improvement and alignment correction. Also, arthroscopy combined with UKA does not increase infection probability or surgical complications, and has an advantage in reducing the total volume of blood transfusion and the percentage of patients receiving blood transfusion. Arthroscopic surgery has its unique advantage with regard to patient selection and a curative effect on cartilage degeneration in the lateral compartment.
Knee osteoarthritis is the most prevalent form of osteoarthritis and is becoming the main reason for progressive pain in knee joints. Arthroscopy combined with unicondylar knee arthroplasty (UKA) is one of the effective methods for the treatment of severe unicompartmental knee arthritis. This surgical approach gives us the capacity to explore all the articular cavities and plays a vital role in UKA patient selection. However, some scholars think that this surgical procedure is traumatic and may increase the rate of surgical infection, and its clinical efficacy needs further study.
We aimed to compare the clinical effects of arthroscopy combined with UKA and UKA alone for patients suffering from unicompartmental knee osteoarthritis (OA).
To further clarify the clinical efficacy, postoperative infection rate, and trauma of arthroscopy combined with UKA in patients with unicompartmental OA.
A retrospective study was conducted after selecting patients who were diagnosed with unicompartmental OA and underwent UKA between October 2012 and November 2006. The condition of each compartment was evaluated under arthroscopy, and whether or not to perform the UKA was determined according to the situation of the knee compartments. Minimally invasive surgery was adapted for UKA surgery. Patients were followed at 3, 6, and 12 mo and every 2 years thereafter. During each follow-up, the radiographic materials, the range of motion (ROM) of knee, the hospital for special surgery (HSS) score, knee society score, and knee function score as recorded, and the modes and time of failure and revision details were collected as well.
Data of 104 patients (118 knees), including 54 patients (60 knees) in the arthroscopy combined with UKA group (group A) and 51 patients (58 knees) in the UKA alone group (group B) was collected at an average follow-up time of 7.25 years. There were no significant differences in the number, age, gender, side, body mass index, etiology, or follow-up between the two groups. At the final follow-up, 3 (5.0%) of 60 knees in group A compared with 4 (6.9%) of 58 knees in group B failed and converted to total knee arthroplasty (TKA), with no statistically significant difference between the two groups (P = 0.933). The percentage of patients receiving blood transfusion was 40% in group A, significantly lower than that in group B (67.2%; P = 0.003). Total volume of blood transfusion in group A was also significantly lower than that of group B (P = 0.001). Both groups improved significantly after operation in clinical symptoms and functions. HSS score, knee society score, and knee function score increased significantly at the latest follow-up compared to pre-operation in group A, from 59.6 ± 10.9 to 82.7 ± 9.3 (P = 0.000), 47.3 ± 6.3 to 76.2 ± 13.1 (P = 0.000) and 57.5 ± 6.3 to 75.1 ± 19.6 (P = 0.000); and in group B, from 59.3 ± 15.6 to 84.3 ± 10.1 (P = 0.000), 49.1 ± 9.2 to 75.1 ± 13.2 (P = 0.000), and 59.3 ± 9.0 to 77.4 ± 13.8 (P = 0.000). There were no significant differences in the scores or angles between the groups at the last follow-up. As to the force line, 84.2% of patients in group A were corrected to normal, which was higher than that in group B (77.8%), although there was no statistical difference between the two groups (P = 0.387).
Arthroscopy combined with UKA and UKA alone both provide benefits in clinical symptom improvement and alignment correction. Arthroscopy combined with UKA does not increase the infection probability and surgical complications, and has an advantage in reducing the total volume of blood transfusion and the percentage of patients receiving blood transfusion. Arthroscopic surgery has a unique advantage with regard to patient selection and a curative effect on cartilage degeneration in the lateral compartment.
This study is a clinical follow-up study limited to a single center. We will conduct a multi-center large-scale clinical follow-up study and expand the case number. Through arthroscopic surgery, the surgery plan for patients who do not meet the UKA indications changes to arthroscopic joint cavity cleaning or TKA. Next, we will also collect clinical data from these patients and follow them to further verify the advantages of arthroscopy combined with UKA with regard to patient selection.
We thank Xiang-Zheng Su and Chun-Hui Liu for their contribution to analysis and interpretation of the data.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shih B, Shantha Kumara MC S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Ma YJ
| 1. | Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee Osteoarthritis: A Primer. Perm J. 2017;21:16-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 210] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 2. | Tang X, Wang S, Zhan S, Niu J, Tao K, Zhang Y, Lin J. The Prevalence of Symptomatic Knee Osteoarthritis in China: Results From the China Health and Retirement Longitudinal Study. Arthritis Rheumatol. 2016;68:648-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 307] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 3. | Wallace IJ, Worthington S, Felson DT, Jurmain RD, Wren KT, Maijanen H, Woods RJ, Lieberman DE. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci USA. 2017;114:9332-9336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 637] [Article Influence: 79.6] [Reference Citation Analysis (0)] |
| 4. | Masaracchio M, Hanney WJ, Liu X, Kolber M, Kirker K. Timing of rehabilitation on length of stay and cost in patients with hip or knee joint arthroplasty: A systematic review with meta-analysis. PLoS One. 2017;12:e0178295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 5. | Wodowski AJ, Swigler CW, Liu H, Nord KM, Toy PC, Mihalko WM. Proprioception and Knee Arthroplasty: A Literature Review. Orthop Clin North Am. 2016;47:301-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Satku K. Unicompartmental knee arthroplasty: is it a step in the right direction?--Surgical options for osteoarthritis of the knee. Singapore Med J. 2003;44:554-556. [PubMed] |
| 7. | Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br. 2006;88:54-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 185] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | Clark M, Campbell DG, Kiss G, Dobson PJ, Lewis PL. Reintervention after mobile-bearing Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2010;468:576-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71:145-150. [PubMed] |
| 10. | Lorbach O, Pape D, Mosser P, Kohn D, Anagnostakos K. [Medial unicondylar knee replacement]. Orthopade. 2014;43:875-876, 878-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Yamabe E, Ueno T, Miyagi R, Watanabe A, Guenzi C, Yoshioka H. Study of surgical indication for knee arthroplasty by cartilage analysis in three compartments using data from Osteoarthritis Initiative (OAI). BMC Musculoskelet Disord. 2013;14:194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Berend KR, Lombardi AV, Morris MJ, Hurst JM, Kavolus JJ. Does preoperative patellofemoral joint state affect medial unicompartmental arthroplasty survival? Orthopedics. 2011;34:e494-e496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | van der List JP, McDonald LS, Pearle AD. Systematic review of medial versus lateral survivorship in unicompartmental knee arthroplasty. Knee. 2015;22:454-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 14. | Thompson SA, Liabaud B, Nellans KW, Geller JA. Factors associated with poor outcomes following unicompartmental knee arthroplasty: redefining the "classic" indications for surgery. J Arthroplasty. 2013;28:1561-1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | von Knoch F, Munzinger U. [Modern unicondylar knee arthroplasty. Tips and tricks]. Orthopade. 2014;43:414-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Springer BD, Scott RD, Thornhill TS. Conversion of failed unicompartmental knee arthroplasty to TKA. Clin Orthop Relat Res. 2006;446:214-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 75] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 17. | Emerson RH, Higgins LL. Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg Am. 2008;90:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 130] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 18. | Lakra A, Murtaugh T, Geller JA, Macaulay W, Shah RP. Simultaneous ipsilateral knee arthroscopy and unicondylar knee arthroplasty is effective for bicompartmental symptoms. J Orthop. 2017;14:507-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Karim AR, Cherian JJ, Jauregui JJ, Pierce T, Mont MA. Osteonecrosis of the knee: review. Ann Transl Med. 2015;3:6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 50] [Reference Citation Analysis (0)] |
| 20. | Müller PE, Pellengahr C, Witt M, Kircher J, Refior HJ, Jansson V. Influence of minimally invasive surgery on implant positioning and the functional outcome for medial unicompartmental knee arthroplasty. J Arthroplasty. 2004;19:296-301. [PubMed] |
| 21. | Kennedy WR, White RP. Unicompartmental arthroplasty of the knee. Postoperative alignment and its influence on overall results. Clin Orthop Relat Res. 1987;278-285. [PubMed] |
| 22. | Xu Q, Chen B, Wang Y, Wang X, Han D, Ding D, Zheng Y, Cao Y, Zhan H, Zhou Y. The Effectiveness of Manual Therapy for Relieving Pain, Stiffness, and Dysfunction in Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Pain Physician. 2017;20:229-243. [PubMed] |
| 23. | Akizuki S, Mueller JK, Horiuchi H, Matsunaga D, Shibakawa A, Komistek RD. In vivo determination of kinematics for subjects having a Zimmer Unicompartmental High Flex Knee System. J Arthroplasty. 2009;24:963-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Jeer PJ, Cossey AJ, Keene GC. Haemoglobin levels following unicompartmental knee arthroplasty: influence of transfusion practice and surgical approach. Knee. 2005;12:358-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW; Oxford Hip and Knee Group. Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty. 2001;16:970-976. [PubMed] |
| 26. | Baumann F, Bahadin Ö, Krutsch W, Zellner J, Nerlich M, Angele P, Tibesku CO. Proprioception after bicruciate-retaining total knee arthroplasty is comparable to unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25:1697-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 27. | Isaac SM, Barker KL, Danial IN, Beard DJ, Dodd CA, Murray DW. Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompartmental arthroplasty. Knee. 2007;14:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 28. | Wautier D, Thienpont E. Changes in anteroposterior stability and proprioception after different types of knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25:1792-1800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Parratte S, Pauly V, Aubaniac JM, Argenson JN. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2012;470:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Inoue A, Arai Y, Nakagawa S, Inoue H, Yamazoe S, Kubo T. Comparison of Alignment Correction Angles Between Fixed-Bearing and Mobile-Bearing UKA. J Arthroplasty. 2016;31:142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Kumar V, Pandit HG, Liddle AD, Borror W, Jenkins C, Mellon SJ, Hamilton TW, Athanasou N, Dodd CA, Murray DW. Comparison of outcomes after UKA in patients with and without chondrocalcinosis: a matched cohort study. Knee Surg Sports Traumatol Arthrosc. 2017;25:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Pandit H, Mancuso F, Jenkins C, Jackson WFM, Price AJ, Dodd CAF, Murray DW. Lateral unicompartmental knee replacement for the treatment of arthritis progression after medial unicompartmental replacement. Knee Surg Sports Traumatol Arthrosc. 2017;25:669-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 33. | Sharpe I, Tyrrell PN, White SH. Magnetic resonance imaging assessment for unicompartmental knee replacement: a limited role. Knee. 2001;8:213-218. [PubMed] |
| 34. | Perkins TR, Gunckle W. Unicompartmental knee arthroplasty: 3- to 10-year results in a community hospital setting. J Arthroplasty. 2002;17:293-297. [PubMed] |
| 35. | Parmaksizoğlu AS, Kabukçuoğlu Y, Ozkaya U, Bilgili F, Aslan A. Short-term results of the Oxford phase 3 unicompartmental knee arthroplasty for medial arthritis. Acta Orthop Traumatol Turc. 2010;44:135-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 36. | Mancuso F, Dodd CA, Murray DW, Pandit H. Medial unicompartmental knee arthroplasty in the ACL-deficient knee. J Orthop Traumatol. 2016;17:267-275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 37. | Plancher KD, Dunn AS, Petterson SC. The anterior cruciate ligament-deficient knee and unicompartmental arthritis. Clin Sports Med. 2014;33:43-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 38. | Suggs JF, Li G, Park SE, Sultan PG, Rubash HE, Freiberg AA. Knee biomechanics after UKA and its relation to the ACL--a robotic investigation. J Orthop Res. 2006;24:588-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 39. | Citak M, Bosscher MR, Citak M, Musahl V, Pearle AD, Suero EM. Anterior cruciate ligament reconstruction after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1683-1688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 40. | Engh GA, Ammeen DJ. Unicondylar arthroplasty in knees with deficient anterior cruciate ligaments. Clin Orthop Relat Res. 2014;472:73-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 41. | Lee GC, Cushner FD, Vigoritta V, Scuderi GR, Insall JN, Scott WN. Evaluation of the anterior cruciate ligament integrity and degenerative arthritic patterns in patients undergoing total knee arthroplasty. J Arthroplasty. 2005;20:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |