Published online Dec 6, 2019. doi: 10.12998/wjcc.v7.i23.4157
Peer-review started: September 5, 2019
First decision: October 24, 2019
Revised: November 1, 2019
Accepted: November 14, 2019
Article in press: November 14, 2019
Published online: December 6, 2019
Processing time: 91 Days and 24 Hours
Endoscopic ultrasound (EUS)-guided drainage is the optimal method for treatment of pancreatic fluid collections (PFCs), and is associated with ease, safety, and efficiency. Bleeding is one of the main procedure-related complications, and often requires surgery or radiologic interventions. Indeed, endoscopic management of this complication is limited.
A 42-year-old man presented for evaluation of abdominal pain and distention for approximately 2 wk. Abdominal computed tomography revealed a pancreatic pseudocyst located in the tail of the pancreas. EUS-guided pancreatic pseudocyst was performed. After stent placement, massive bleeding was noted from the fistula. Finally, hemostasis was successfully achieved using hemostatic forceps within the fistula.
Bleeding vessel grasp and coagulation may represent a successful treatment for a fistula hemorrhage during EUS-guided drainage for a PFC, which may be tried before application of balloon or stent compression.
Core tip: We report the successful management of massive fistula bleeding during endoscopic ultrasound-guided pancreatic pseudocyst drainage using hemostatic forceps within the fistula, which proved the efficiency of this method.
- Citation: Ge N, Sun SY. Management of massive fistula bleeding after endoscopic ultrasound-guided pancreatic pseudocyst drainage using hemostatic forceps: A case report. World J Clin Cases 2019; 7(23): 4157-4162
- URL: https://www.wjgnet.com/2307-8960/full/v7/i23/4157.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i23.4157
Endoscopic ultrasound (EUS)-guided drainage is the optimal method for the treatment of pancreatic fluid collections (PFCs), and is associated with ease, safety, and efficiency[1-5]. Bleeding is one of the main procedure-related complications; the incidence is low but difficult to manage and often requires surgery or radiologic-guided embolization[6]. Herein we report the successful management of massive fistula bleeding during EUS-guided pancreatic pseudocyst drainage using hemostatic forceps.
A 42-year-old man presented for evaluation of abdominal pain and distention for approximately 2 wk.
The patient has a long-term history of alcohol consumption.
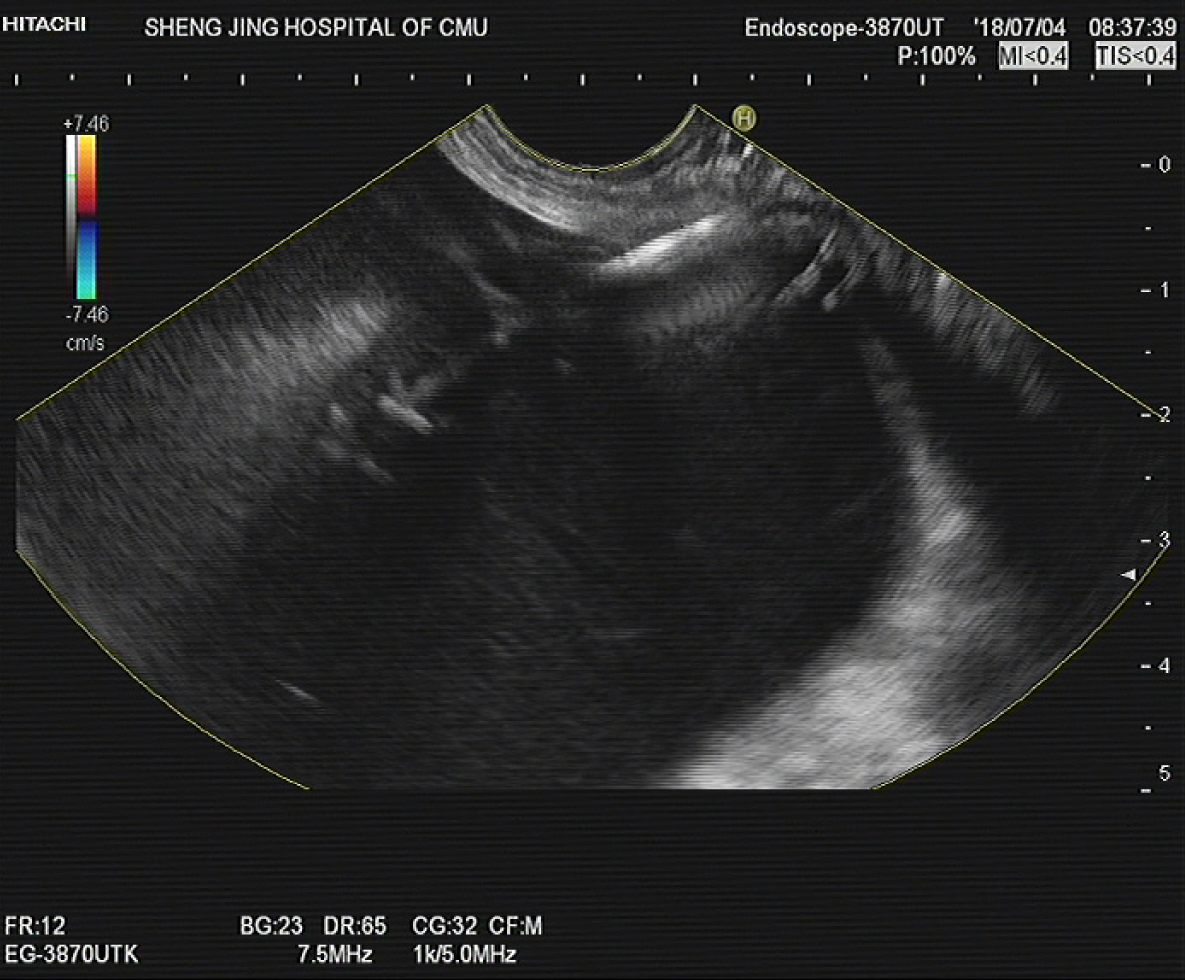
Abdominal computed tomography (CT) revealed atrophy of the pancreatic parenchyma and dilation of the main pancreatic duct with multiple stones. A pancreatic pseudocyst was located in the tail of the pancreas, measuring 9.8 cm × 8.0 cm. Varicose veins were also found around the fundus of the stomach (Figure 1).
Pancreatic pseudocyst.
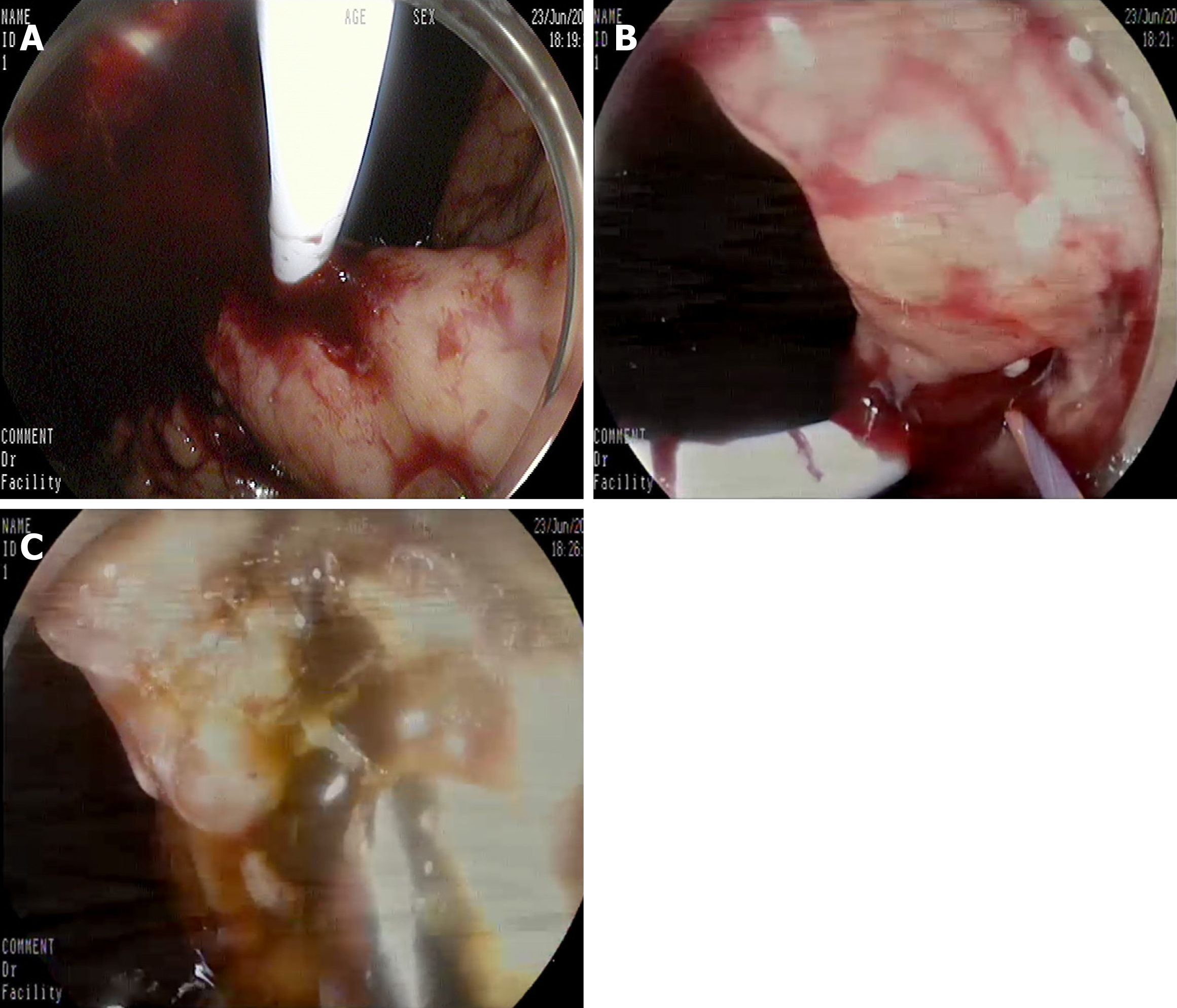
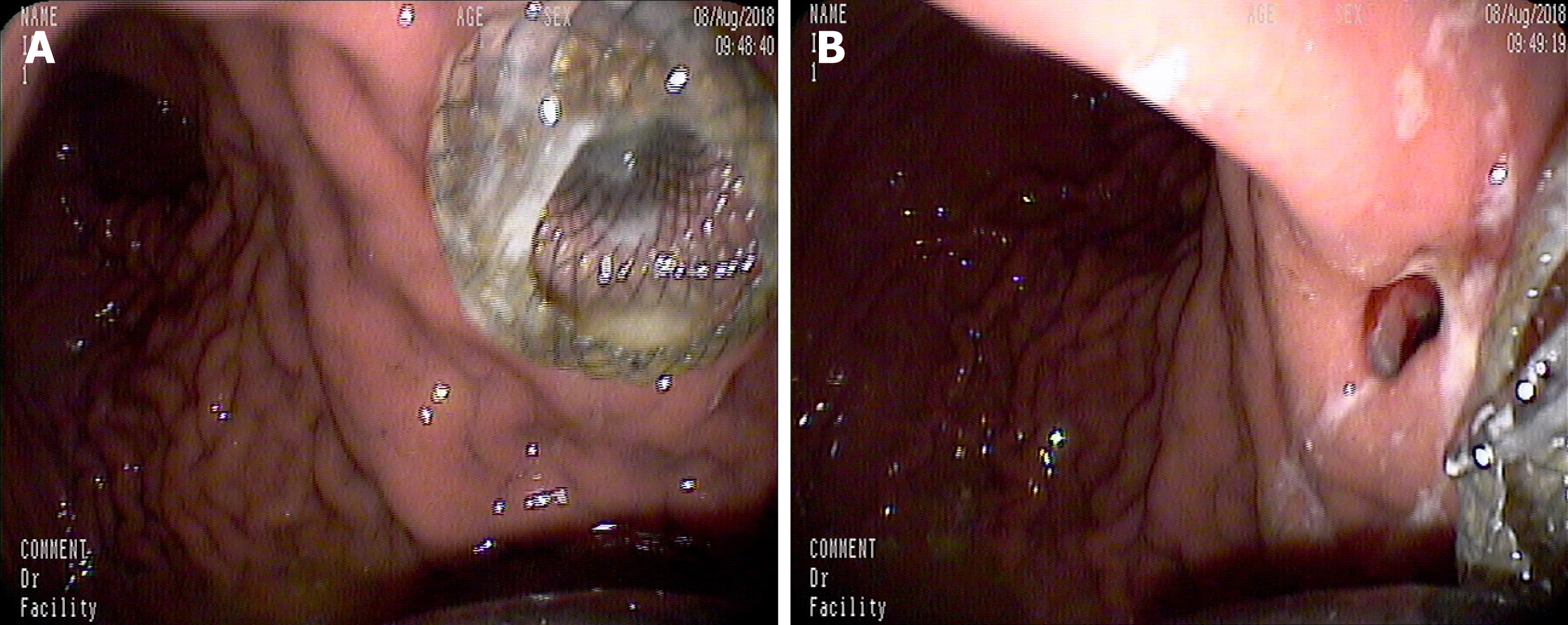
An EUS-guided cyst-gastrostomy was performed. A longitudinal echoendoscope (PENTAXEG3870UT; Pentax Corporation, Takyo, Japan) with a 3.8-mm working channel accessible to a 10 Fr stent was used. Color Doppler was used to identify and avoid interposing vessels during puncture. An EchoTip Ultra endoscopic ultrasound needle (19-gauge; Boston Scientific Corp., United States) was introduced via the working channel of the echoendoscope, and the PFC was punctured under EUS guidance (Figure 2). A brown cystic fluid sample was aspirated and sent to determine the amylase level, as well as for other biochemical analyses. A guidewire (0.035 inch/480 mm; Boston Scientific, United States) was inserted into the cystic cavity. A cystotome (10 Fr; Wilson-Cook Medic, United States) was delivered to the dilated needle path and followed with a 10-mm balloon dilator. A 10-Fr plastic double-pigtail stent (Wilson-Cook Medic) was placed. After the stent placement, massive bleeding was noted from the fistula (Figure 3A). Under EUS, the site of bleeding was difficult to locate and blood began to fill the stomach cavity. We withdrew the EUS and introduced a gastrointestinal endoscope (3.2-mm working channel; Pentax Corporation) with a transparent cap attached. The bleeding vessel was viewed within the fistula (Figure 3B). Hemostatic forceps were introduced and the vessel was grasped until the bleeding stopped, then high-frequency electrocoagulation was performed. Hemostasis was successfully achieved (Figure 3C). A lumen-apposing metal stent (12 mm/25 mm, 16 mm/35 mm; Micro-Tech/Nan Jing Co., Ltd., China) was placed for the pancreatic pseudocyst drainage.
After the procedure, the patient remained hemodynamically stable, received standard care and antibiotics, and had no drop in hemoglobin during a 3-day hospital stay. A follow-up abdominal CT scan 1 month later showed almost complete resolution of the PFC (Figure 4), and the stent was removed (Figure 5).
Ultrasound-guided drainage is the first-line modality for drainage of symptomatic PFCs. The overall clinical success rate is 90.5%-100%; the adverse effect rate is 98.0%-23.8%, mainly including hemorrhage, perforation, secondary infection, and stent migration[7-11]. Procedure-related bleeding reportedly occurs in 1%-2% of cases during EUS-guided drainage of PFCs. The use of EUS may help to reduce the risk of bleeding by visualizing intervened vessels. One prospective study reported a 13% bleeding rate with conventional endoscopic drainage, compared to no bleeding with EUS-guided interventions[12]; however, even with EUS guidance, bleeding remains an important adverse event[13]. Varadarajulu et al[7] also reported that bleeding occurred in a patient with underlying acquired factor VIII inhibitors. Also, straight biliary fully-covered self-expandable metal stent possibly increases the risk of delayed bleeding, in which case endoscopic intervention may be limited. Stent erosion of the gastric wall can occur during esophagogastroduodenoscopy. Collateral vessel bleeding can also occur during fistula creation and is often successfully managed conservatively. The bleeding caused by splenic artery pseudoaneurysms are often life-threatening[6]. In our case, the vessel injury during puncture, which was missed during EUS scanning, was the cause of bleeding.
As reported, there are three endoscopic interventions to manage bleeding during the procedure, as follows: (1) Fistula bleeding can be compressed by a balloon dilator, which is effective when the bleeding is not severe[14]; (2) A fully-covered self-expandable metal stent is delivered directly to continuously compress the fistula; and (3) Wang et al[14] reported using a bi-flanged self-expandable metal stent to stop bleeding in the needle path by external compression at the puncture site from stent expansion. In our case, the needle path was dilated using a 1-cm balloon, which permitted clear visualization of the needle path and identification of the bleeding vessel. If the needle path was not fully dilated, the bleeding vessel would not be detected and a fully covered metal stent may be considered. In our case, the bleeding vessel was ruptured and direct hemostasis was considered before balloon or stent compression.
In conclusion, bleeding vessel grasp and coagulation may represent a successful treatment for a fistula hemorrhage during EUS-guided drainage for a PFC, which may be tried before application of balloon or stent compression.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Castro-Fernandez M, Lowenberg M S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Adler DG. Single-operator experience with a 20-mm diameter lumen apposing metal stent to treat patients with large pancreatic fluid collections from pancreatic necrosis. Endosc Ultrasound. 2018;7:422-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Adler DG, Shah J, Nieto J, Binmoeller K, Bhat Y, Taylor LJ, Siddiqui AA. Placement of lumen-apposing metal stents to drain pseudocysts and walled-off pancreatic necrosis can be safely performed on an outpatient basis: A multicenter study. Endosc Ultrasound. 2019;8:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Caillol F, Godat S, Turrini O, Zemmour C, Bories E, Pesenti C, Ratone JP, Ewald J, Delpero JR, Giovannini M. Fluid collection after partial pancreatectomy: EUS drainage and long-term follow-up. Endosc Ultrasound. 2019;8:91-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Li L, Cristofaro S, Qu C, Liang S, Li X, Cai Q. EUS-guided drainage of pancreatic fluid collection with a Hot AXIOS stent in a patient with pancreatitis following distal pancreatectomy (with video). Endosc Ultrasound. 2018;7:347-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Bang JY, Varadarajulu S. Stent Tracker app: Novel method to track patients with indwelling lumen-apposing metal stents. Endosc Ultrasound. 2018;7:69-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Lang GD, Fritz C, Bhat T, Das KK, Murad FM, Early DS, Edmundowicz SA, Kushnir VM, Mullady DK. EUS-guided drainage of peripancreatic fluid collections with lumen-apposing metal stents and plastic double-pigtail stents: comparison of efficacy and adverse event rates. Gastrointest Endosc. 2018;87:150-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 107] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 7. | Varadarajulu S, Christein JD, Wilcox CM. Frequency of complications during EUS-guided drainage of pancreatic fluid collections in 148 consecutive patients. J Gastroenterol Hepatol. 2011;26:1504-1508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 8. | Saul A, Ramirez Luna MA, Chan C, Uscanga L, Valdovinos Andraca F, Hernandez Calleros J, Elizondo J, Tellez Avila F. EUS-guided drainage of pancreatic pseudocysts offers similar success and complications compared to surgical treatment but with a lower cost. Surg Endosc. 2016;30:1459-1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Siddiqui AA, Adler DG, Nieto J, Shah JN, Binmoeller KF, Kane S, Yan L, Laique SN, Kowalski T, Loren DE, Taylor LJ, Munigala S, Bhat YM. EUS-guided drainage of peripancreatic fluid collections and necrosis by using a novel lumen-apposing stent: a large retrospective, multicenter U.S. experience (with videos). Gastrointest Endosc. 2016;83:699-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 214] [Article Influence: 23.8] [Reference Citation Analysis (1)] |
| 10. | Chen Y, Zhu H, Jin Z, Li Z, Du Y. An unusual complication of cardia occlusion with lumen-apposing metal stent therapy for pancreatic pseudocyst. Endosc Ultrasound. 2018;7:61-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Rana SS, Gupta R, Kang M, Sharma V, Sharma R, Gorsi U, Bhasin DK. Percutaneous catheter drainage followed by endoscopic transluminal drainage/necrosectomy for treatment of infected pancreatic necrosis in early phase of illness. Endosc Ultrasound. 2018;7:41-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Varadarajulu S, Christein JD, Tamhane A, Drelichman ER, Wilcox CM. Prospective randomized trial comparing EUS and EGD for transmural drainage of pancreatic pseudocysts (with videos). Gastrointest Endosc. 2008;68:1102-1111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 278] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 13. | Siddiqui AA, Kowalski TE, Loren DE, Khalid A, Soomro A, Mazhar SM, Isby L, Kahaleh M, Karia K, Yoo J, Ofosu A, Ng B, Sharaiha RZ. Fully covered self-expanding metal stents versus lumen-apposing fully covered self-expanding metal stent versus plastic stents for endoscopic drainage of pancreatic walled-off necrosis: clinical outcomes and success. Gastrointest Endosc. 2017;85:758-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 222] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 14. | Wang BH, Xie LT, Zhao QY, Ying HJ, Jiang TA. Balloon dilator controls massive bleeding during endoscopic ultrasound-guided drainage for pancreatic pseudocyst: A case report and review of literature. World J Clin Cases. 2018;6:459-465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |