Published online Dec 6, 2019. doi: 10.12998/wjcc.v7.i23.4130
Peer-review started: September 27, 2019
First decision: October 24, 2019
Revised: November 14, 2019
Accepted: November 20, 2019
Article in press: November 20, 2019
Published online: December 6, 2019
Processing time: 69 Days and 23.2 Hours
Herein, we report a case in whom two foreign bodies entered the upper mediastinal cavity from the cervical root and subsequently the esophagus. Surgery is the preferred treatment method, and operational procedures depend on the size and location of the foreign body relative to the mediastinal vessels. Rigid esophagoscopy combined with angle endoscopic surgery was selected to avoid surgical trauma and complications.
A 63-year-old male patient with a 6-mo old history of neck trauma presented with a black-brown foreign body in the lateral wall of the esophagus. Neck and chest computed tomography (CT) revealed that two superior mediastinal foreign bodies penetrated the esophagus diagonally. We removed two foreign bodies through an esophagoscope. Owing to the rigid working channel of esophagoscope and good exposure of endoscope, the risk of injury to the adjacent vital tissues was minimized. Postoperative comprehensive therapies, including antibiotic administration and nutritional support, resulted in a prompt postoperative recovery. Postoperative CT confirmed the absence of a residual foreign body and neck and chest infections. In addition, upper gastrointestinal angiography and gastroscopy revealed the absence of an evident esophageal perforation. The patient received an oral diet and did not experience any complication at the time of discharge from the hospital.
Rigid esophagoscopy combined with angle endoscopy is an effective, minimally invasive treatment for penetrating neck injuries.
Core tip: In this case, we report a 63-year-old male patient with a history of neck trauma who presented with a black-brown foreign body in the lateral wall of the esophagus. Neck and chest-computed tomography showed that two superior mediastinal foreign bodies penetrated the esophagus diagonally. We performed a rigid esophagoscopy combined with angle endoscopic surgery to remove the two foreign bodies. Because of a rigid working channel of the esophagoscope and good exposure of the endoscope, the risk of injury to the adjacent vital tissues was minimized.
- Citation: Wang D, Gao CB. Rigid esophagoscopy combined with angle endoscopy for treatment of superior mediastinal foreign bodies penetrating into the esophagus caused by neck trauma: A case report. World J Clin Cases 2019; 7(23): 4130-4136
- URL: https://www.wjgnet.com/2307-8960/full/v7/i23/4130.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i23.4130
Retention of a mediastinal foreign body is significantly risky, as it can induce mediastinal abscess, and a sharp foreign body may injure the blood vessels[1]. Mediastinal foreign bodies have varied sources; however, they usually originate from esophageal foreign body injuries. Neck trauma is a rare cause of foreign bodies penetrating the mediastinum. According to the divided zone of neck trauma, zone I is adjacent to the superior mediastinum, and a foreign body penetrating in zone I can penetrate into the mediastinum[2]. Owing to the complexity of the superior mediastinal anatomy and possible complications, surgeons experience difficulty in completely removing mediastinal foreign bodies. This report aims to show that rigid esophagoscopy combined with angle endoscopy surgery is an appropriate surgical strategy for the removal of mediastinal foreign bodies.
A 63-year-old male patient, a teacher, presented with swallowing difficulty lasting for a week and had a history of anterior neck trauma caused by bamboo penetration 6 mo before.
The patient had undergone debridement and extraction of a bamboo section in a primary care hospital. The wound healed without auxiliary examination and treatment (Figure 1), and the patient did not complain of subsequent discomfort. A month ago, he had abnormal sensations in his neck and heel, but no dysphagia. The laryngoscopy performed at the local county hospital did not show any abnormalities, so no other auxiliary examinations or treatments were performed.
A week ago, the patient presented with marked dysphagia and could only ingest liquid food. Gastrointestinal (GI) endoscopy revealed a dark-brown foreign body in the lateral wall of the esophagus. In the primary hospitals, attempts to remove the foreign body with a flexible GI endoscope were unsuccessful because the foreign body was embedded in the lateral wall of the esophageal mucosa, which could cause further trauma if the foreign body was forcibly removed.
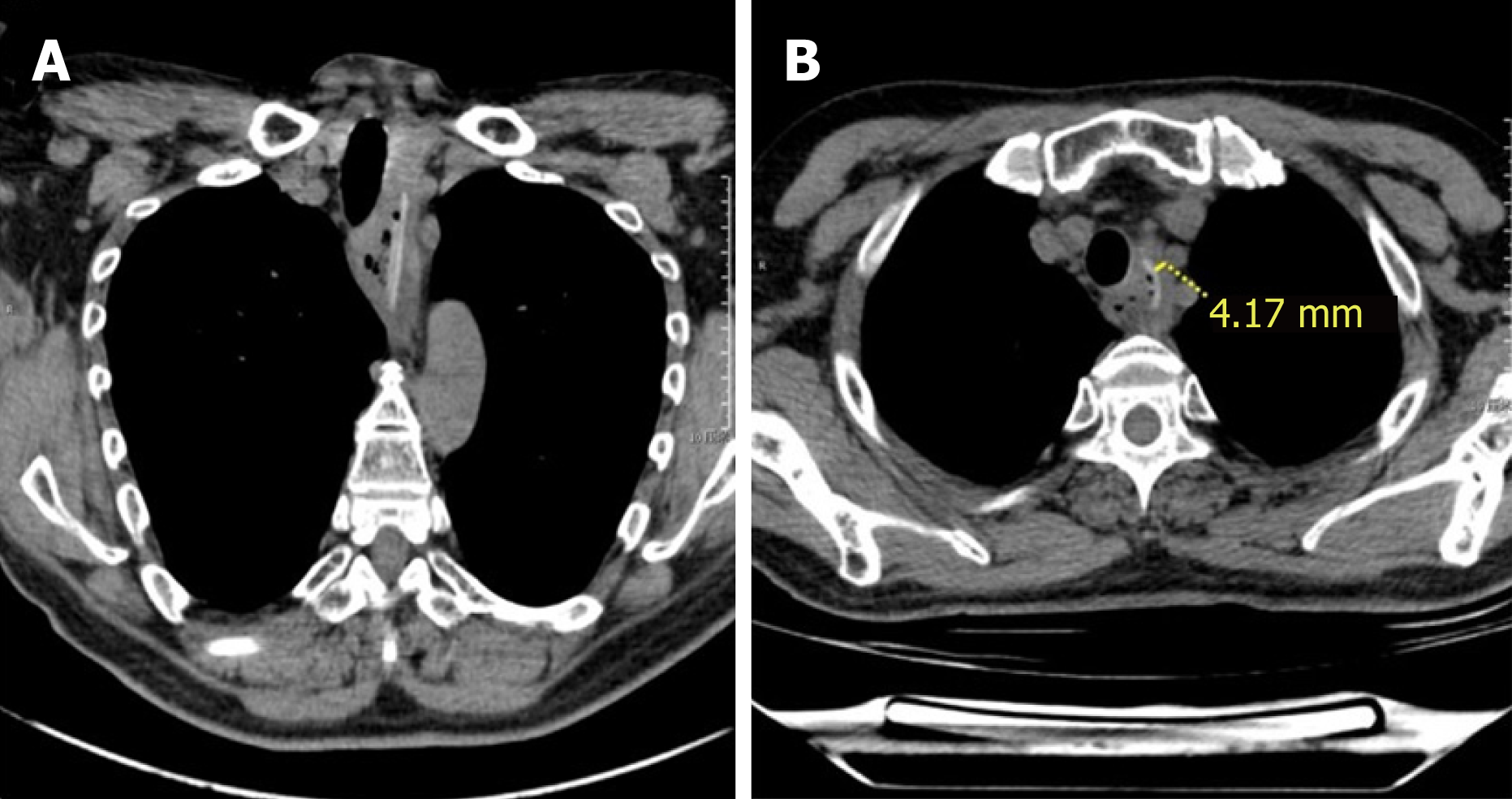
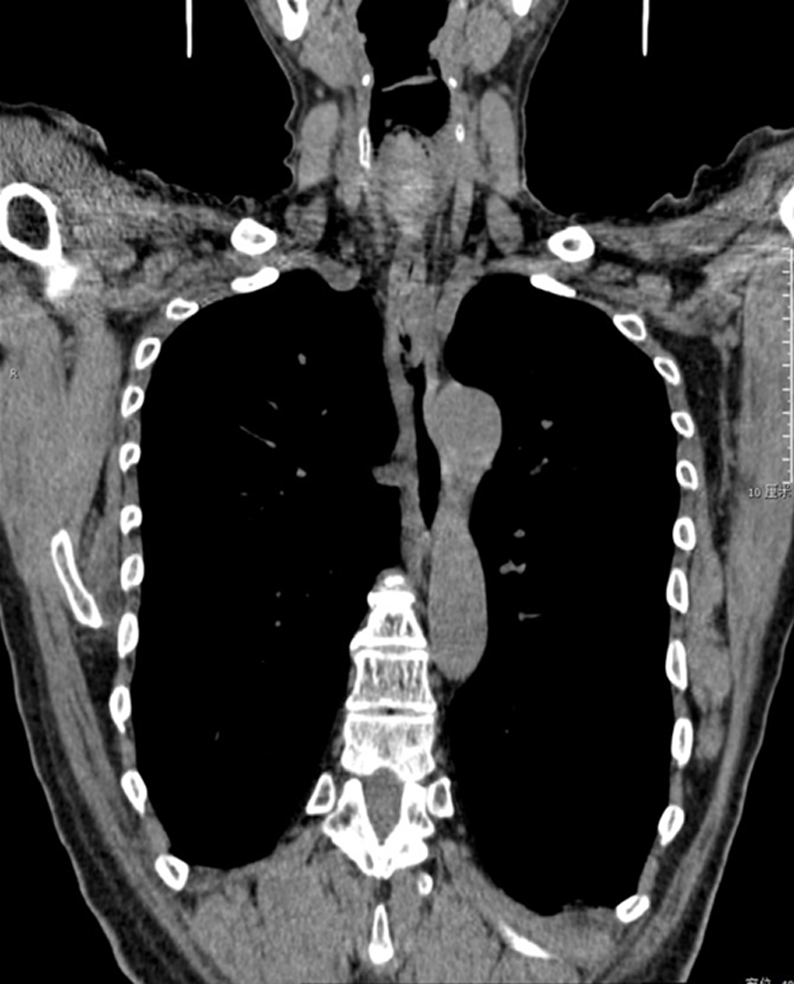
On admission, we performed neck and chest computed tomography (CT) and found that two foreign bodies had penetrated the esophagus from the superior mediastinum. In addition, each layer of the esophagus was penetrated diagonally, and the embedded foreign bodies were adjacent to the left common carotid and left subclavian arteries above the aortic arch (Figure 2A and B). The laboratory data were judged as normal after multidisciplinary discussion among the anesthesiologist, gastroenterologist, and thoracic surgeon. Rigid esophagoscopy combined with angle endoscopic surgery was performed under general anesthesia (Figure 3).
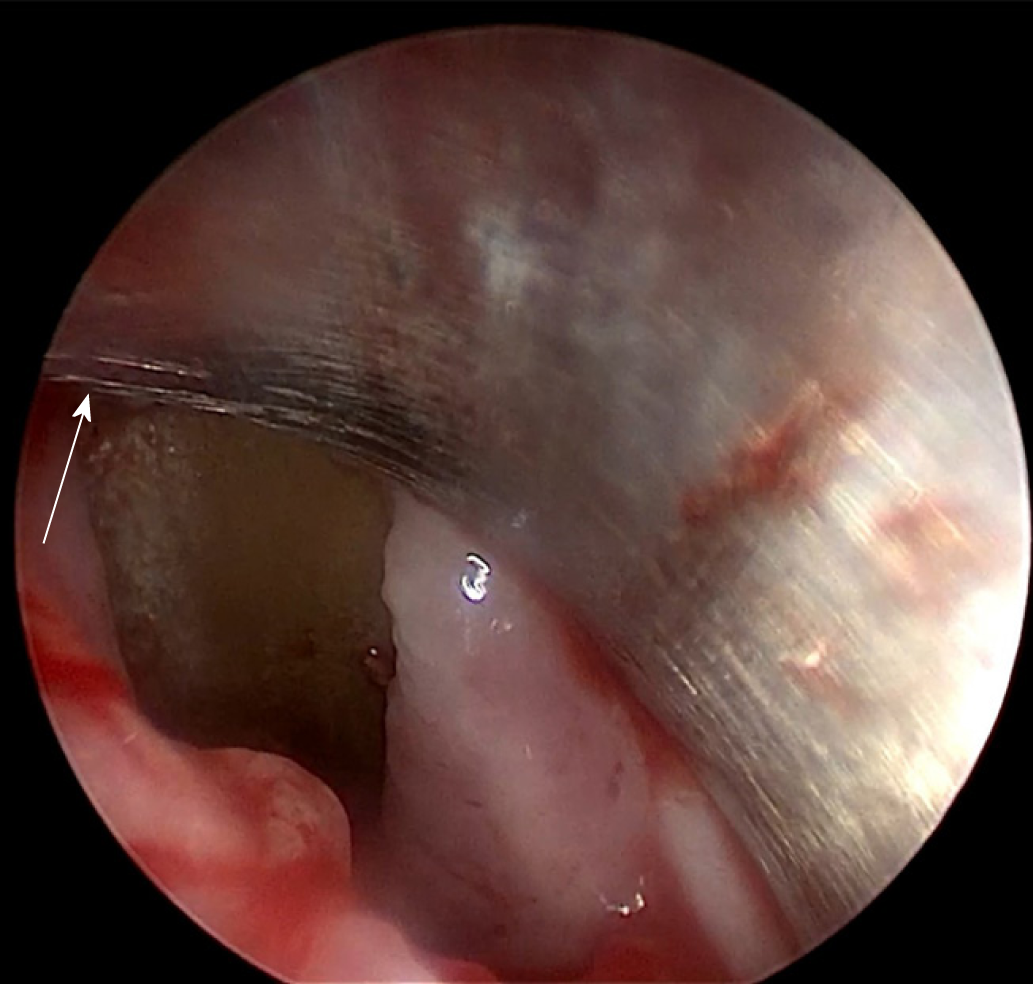
A rigid esophagoscope was inserted in the esophagus. However, because the rigid esophagoscope was significantly long, an angle ureteroscope was inserted in the rigid esophagoscope to reveal the foreign body impaction in the lateral wall of the esophagus from the esophageal mucosa 23 cm from the incisor (Figure 4).
Superior mediastinal foreign bodies, esophageal perforation, and neck trauma.
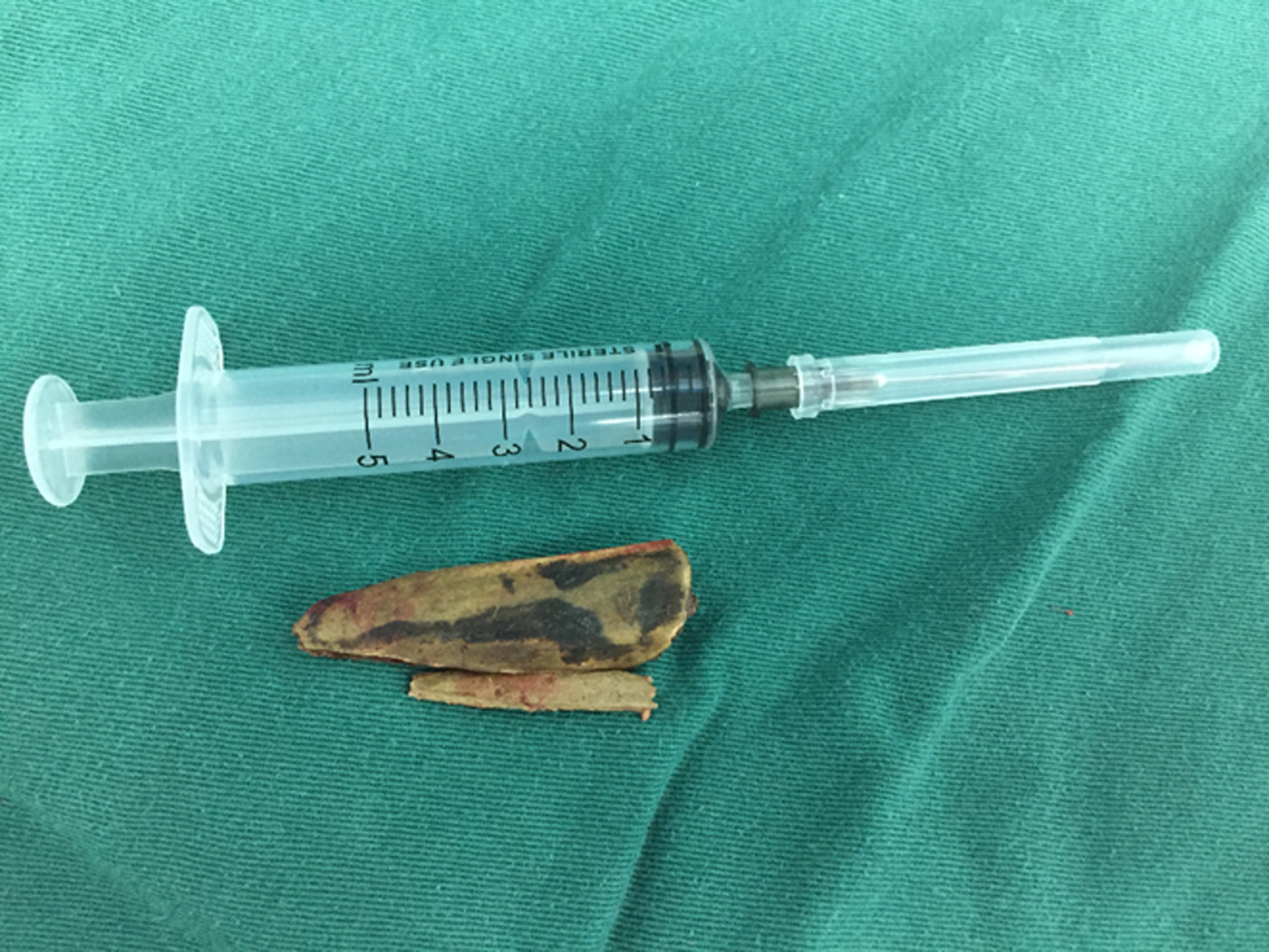
The surgery using an angle ureteroscope was performed in two main steps as follows. First, the foreign bodies were slowly moved into the esophageal lumen along the direction of the esophageal insertion and, subsequently, removed using an esophagoscope (Figure 5). After foreign body removal, angle ureteroscopy revealed no evident perforation or longitudinal laceration in the esophagus, no excessive abscess, and no vascular bleeding. A nasogastric tube was inserted. Postoperative antibiotic administration and enteral nutritional support were initiated. We performed neck and chest CT on the seventh day after the surgery and found no residual foreign body.
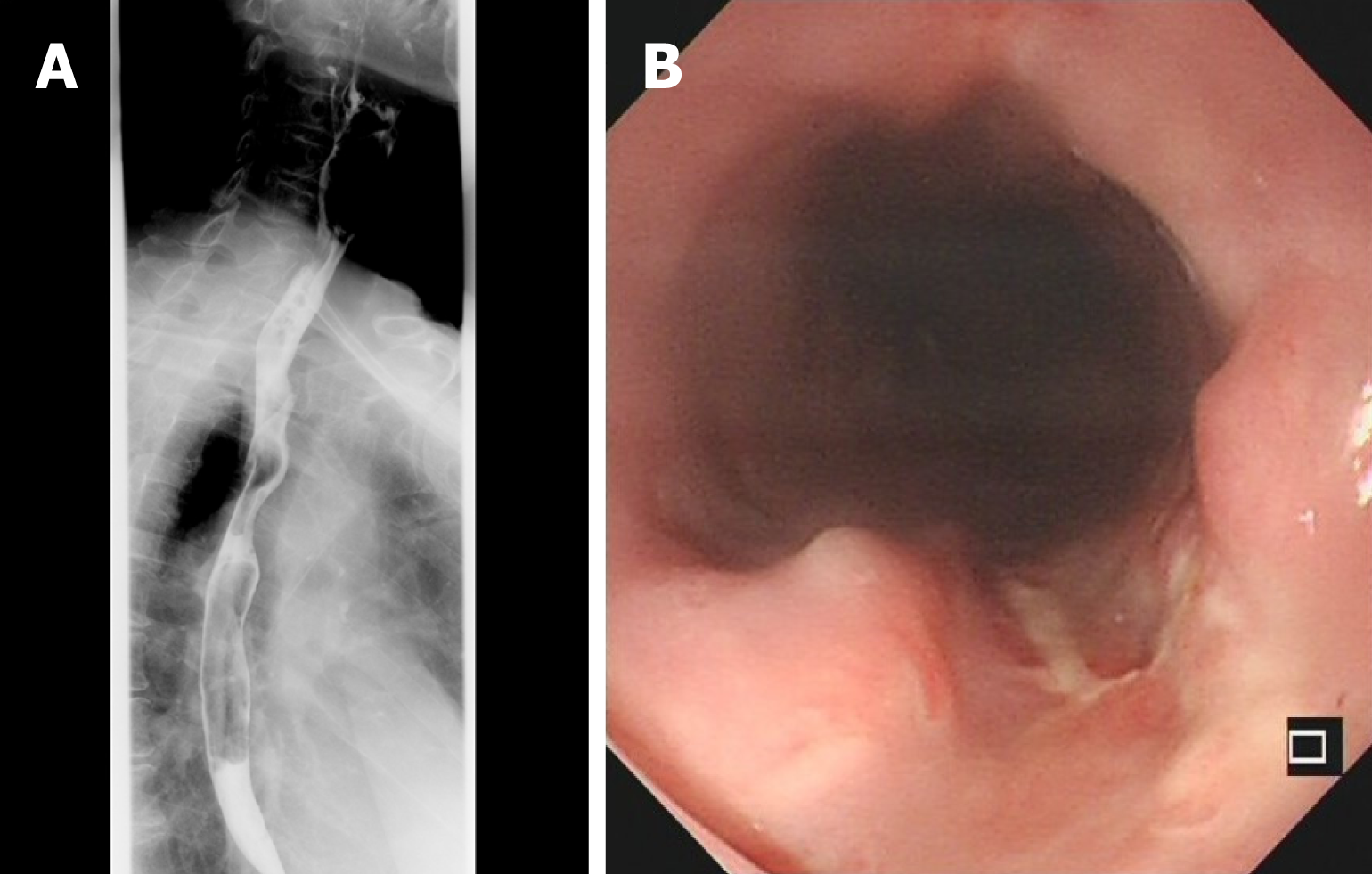
On postoperative day 14, upper GI enterography confirmed the absence of contrast agent leakage (Figure 6A). Moreover, flexible GI endoscopy revealed a superficial esophageal ulcer without evident perforation (Figure 6B); thus, subsequently, oral fluid feeding was initiated. After 2 d of oral fluid feeding, neck and chest CT revealed no periesophageal or mediastinal infections (Figure 7), and the results of all routine examinations were normal. Subsequently, routine oral feeding was initiated, and the patient was discharged with no complaints of discomfort on postoperative day 20. Follow-up flexible GI endoscopy revealed no esophageal stenosis 3 mo after the operation.
Owing to the complex anatomy of the cervical vertebral root and the high density of important blood vessels, surgery is not ideally recommended for mediastinal foreign bodies. In addition, the lack of technical expertise and incomplete debridement of the trauma zone in primary care hospitals generally result in a residual foreign body. Neck and chest CT or CT angiography should be performed to identify any vital-structure injury according to the divided zone of the neck trauma[3,4].
Foreign body retention was observed in the present patient only after debridement because no prior other auxiliary examinations were performed. As the superior mediastinum is anatomically continuous with the loose connective tissue of the neck, the foreign bodies entered the superior mediastinum with the swallowing movement, diagonally penetrated the outer membrane of the esophagus into the intraluminal layer, and were subsequently embedded in the esophagus.
Esophageal foreign bodies and neck trauma are the most common causes of foreign bodies penetrating the mediastinum and mediastinal abscesses. Foreign bodies penetrate into the mediastinum from the esophagus, and the direction of foreign body insertion is at an acute angle to the direction of the long axis of the esophagus. Hence, food and fluids tend to flow into the mediastinum, resulting in infection. In the present case, owing to the obtuse angle between the direction of the insertion and the long axis of the esophagus, retrograde flow of food and liquids into the mediastinum is difficult, resulting in no infection or abscess. With the development of thoracic surgical techniques, video-assisted thoracoscopic/mediastinoscopic surgery is the primary choice of treatment for mediastinal foreign bodies and abscess. In addition, the complication rate of the treatment is lower than that of open-heart surgery, and a series of successful cases have been reported[5,6]. However, in the present case, the foreign bodies penetrated each layer of the esophagus diagonally and were embedded in the esophagus. Moreover, because the upper ends of the foreign bodies were close to the blood vessels and the upper mediastinal space is narrow, performing mediastinoscopy was significantly difficult. Forcibly removing the foreign bodies could tear the esophagus longitudinally and damage the large blood vessels. In our patient, no abscess was found in the mediastinum and the foreign bodies entered the esophageal cavity along the direction of the esophageal insertion. By using an angular endoscope, the foreign body was completely inserted in the direction of entry into the esophagus and safely removed from the esophageal cavity. Therefore, for this case, the above-mentioned method was the best choice, and the trauma caused by the rigid esophagoscope was smaller than that caused by the mediastinoscope. To promote esophageal healing, postoperative treatment was mainly based on antibiotic administration and gastrointestinal nutritional support. Many factors are believed to be associated with esophageal perforation healing, such as the perforation site, malnutrition, sepsis, pulmonary comorbidities, and length of perforation[7-9]. Recently, treatments for esophageal perforation mainly include conservative and surgical methods. Appropriate treatment must be chosen according to the situation of the patient. Currently, conservative treatment is the best treatment in most cases (endoscopic clipping, stenting, antibiotic administration, or endoscopic vacuum therapy)[10-12]. In the present case, as each layer of the esophagus was penetrated diagonally and the foreign bodies were embedded in the esophagus, the layers of the esophagus may have adhered to each other after foreign body removal. Thus, no obvious perforation was observed in the esophagus. Maybe the perforation had healed, and we did not observe it. In the absence of an evident mediastinal infection, we chose conservative treatment and gastrointestinal nutritional support combined with adequate doses of broad-spectrum antibiotics to enhance the healing of the esophageal perforation.
Although mediastinal foreign body penetration following neck trauma is extremely rare, it can be prevented if the neck trauma is treated effectively and promptly. To the best of our knowledge, rigid esophagoscopy combined with angle endoscopy is an appropriate treatment strategy for mediastinal foreign body invasion in the esophagus. Therefore, the standard treatment for penetrating neck injuries must be performed in cases similar to the present one. We believe that rigid esophagoscopy combined with angle endoscopy is an effective, minimally invasive treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hourneaux de Moura DT S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 388] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 2. | Roon AJ, Christensen N. Evaluation and treatment of penetrating cervical injuries. J Trauma. 1979;19:391-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 151] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Kasbekar AV, Combellack EJ, Derbyshire SG, Swift AC. Penetrating neck trauma and the need for surgical exploration: six-year experience within a regional trauma centre. J Laryngol Otol. 2017;131:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Teixeira F, Menegozzo CA, Netto SD, Poggeti RS, Collet E Silva Fde S, Birolini D, Bernini Cde O, Utiyama EM. Safety in selective surgical exploration in penetrating neck trauma. World J Emerg Surg. 2016;11:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Davies B, Black E, Vaughan R. Thoracoscopic drainage of and foreign body removal from a posterior mediastinal abscess. Eur J Cardiothorac Surg. 2004;25:897-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Wang J, Wu WB, Chen L, Zhu Q. Video-mediastinoscopy assisted fish bone extraction and superior Medistinal abscess debridement. J Cardiothorac Surg. 2018;13:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Bhatia P, Fortin D, Inculet RI, Malthaner RA. Current concepts in the management of esophageal perforations: A twenty-seven years Canadian experience. Ann Thorac Surg. 2011;92:209-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 8. | Cho JS, Kim YD, Kim JW, I HS, Kim MS. Thoracoscopic primary esophageal repair in patients with Boerhaave's syndrome. Ann Thorac Surg. 2011;91:1552-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Huang Y, Lu T, Liu Y, Zhan C, Ge D, Tan L, Wang Q. Surgical management and prognostic factors in esophageal perforation caused by foreign body. Esophagus. 2019;16:188-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Infante M, Valente M, Andreani S, Catanese C, Dal Fante M, Pizzetti P, Giudice G, Basilico M, Spinelli P, Ravasi G. Conservative management of esophageal leaks by transluminal endoscopic drainage of the mediastinum or pleural space. Surgery. 1996;119:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Mokbel KM, Khafagy YW. Single flap with three pedicles, bone paté and split-thickness skin graft for immediate mastoid obliteration after canal wall down mastoidectomy. Eur Arch Otorhinolaryngol. 2012;269:2037-2041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | De Moura DTH, De Moura BFBH, Manfredi MA, Hathorn KE, Bazarbashi AN, Ribeiro IB, de Moura EGH, Thompson CC. Role of endoscopic vacuum therapy in the management of gastrointestinal transmural defects. World J Gastrointest Endosc. 2019;11:329-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 110] [Cited by in RCA: 86] [Article Influence: 14.3] [Reference Citation Analysis (6)] |