Published online Dec 6, 2019. doi: 10.12998/wjcc.v7.i23.4011
Peer-review started: August 19, 2019
First decision: October 24, 2019
Revised: October 31, 2019
Accepted: November 14, 2019
Article in press: November 14, 2019
Published online: December 6, 2019
Processing time: 108 Days and 18.3 Hours
Perivascular epithelioid cell tumor (PEComa) is a rare mesenchymal neoplasm that can arise in many different organs with a broad spectrum of biological behavior, from indolent to aggressive progression. Only ten cases of gastric PEComas have been reported in the English literature, which were treated with endoscopic, laparoscopic, or open resections. Due to its rarity, the optimal surgical management and prognosis of this tumor are still uncertain.
We present a case of robotic wedge resection of a 6.5 cm bleeding lesion of the gastric fundus located 3 cm below the esophago-gastric junction in a 55-year-old man. Biopsy revealed a malignant tumor with epithelioid cells focally positive for muscle markers desmin and smooth muscle actin. In addition, histology revealed that the tumor was positive for HMB-45, melan-A (MART-1), microphthalmia transcription factor and negative for pan-cytokeratin AE1/AE3, CD34, p40, DOG-1, CD117 (c-kit), S100, CD3, CD79a, caldesmon and myogenin. These markers suggested the possibility of a PEComa. The patient underwent a diagnostic laparoscopy via the da Vinci® Si™ system and robotic wedge resection. Final pathology confirmed a malignant gastric PEComa with negative margins. At his 11-mo follow-up visit, the patient remained disease-free.
Gastric PEComa can be treated with a robotic R0 resection with acceptable postoperative and short-term oncological outcomes.
Core tip: Robot-assisted surgical resection can be considered to facilitate the surgical treatment of a gastric perivascular epithelioid cell tumor (PEComa). PEComa should be included in the differential diagnosis of gastric tumors with unclear pathology. Due to its rarity, optimum management of the primary and metastatic disease is still unknown. To date, only ten cases of gastric PEComas treated with open or laparoscopic surgery are described in the literature. We report the first malignant PEComa of the fundus treated with a robotic R0 resection. The robotic approach was safe, feasible and provided acceptable short-term oncological outcomes.
- Citation: Marano A, Maione F, Woo Y, Pellegrino L, Geretto P, Sasia D, Fortunato M, Orcioni GF, Priotto R, Fasoli R, Borghi F. Robotic wedge resection of a rare gastric perivascular epithelioid cell tumor: A case report. World J Clin Cases 2019; 7(23): 4011-4019
- URL: https://www.wjgnet.com/2307-8960/full/v7/i23/4011.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i23.4011
Perivascular epithelioid cell tumors (PEComas) represent a family of rare mesenchymal neoplasms defined by the World Health Organization in 2002. PEComas are composed of perivascular epithelioid cells (PEC) which demonstrate immunohistochemical evidence of both smooth muscle and melanocytic differentiation[1]. These tumors are histologically heterogenous and demonstrate a broad spectrum of biological behaviors. Although malignancy may be suggested by some histological characteristics[2-4], reliable markers of aggressive behavior have not yet been validated.
Clinically, PEComas have been described in various visceral and soft tissue sites[2,4,5] where gastrointestinal (GI) involvement predominantly affects the colon and the small intestine[6], but rarely the stomach[4,7-13]. Due to the rarity of stomach PEComas, clinical presentation and optimal management are still unclear. Herein, we report the first case of PEComa of the gastric fundus treated with a robotic wedge resection performed with curative intent.
A 55-year-old man presented with melena.
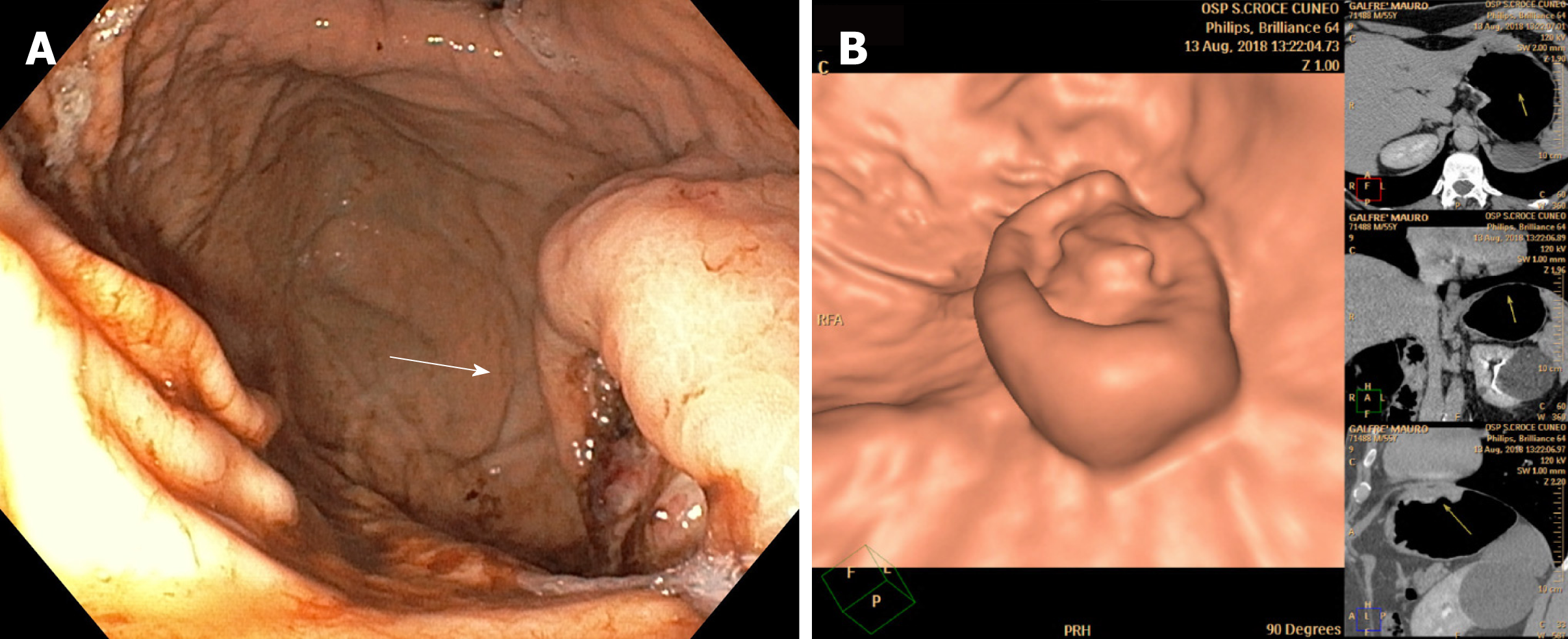
Following admission, upper GI endoscopy was performed which revealed an actively bleeding ulcerative lesion of the gastric fundus (Figure 1A). Pathologic evaluation of a biopsy of the lesion demonstrated a malignant epithelioid cell tumor with marked nuclear pleomorphism and myo-melanocytic differentiation. The possibility of a PEComa was considered and a second pathologic review confirmed this diagnosis.
The patient had no significant past medical or surgical history. He had no previous malignancy, immunosuppressive disorders, use of nonsteroidal anti-inflammatory medications, or unusual infections.
The patient did not report weight loss, decreased appetite or changes in bowel habits. He has never smoked.
Physical examination was unremarkable.
Laboratory data showed a microcytic anemia caused by iron deficiency: hemoglobin of 7.5 g/dL, hematocrit of 24.70%, mean corpuscular volume of 74.4 fl, mean corpuscular hemoglobin of 22.6 pg, mean corpuscular hemoglobin concentration of 30.4 g/dL, iron of 15 μg/dL, and ferritin of 8.0 ng/mL.
To guide management, a thorough staging work-up was performed. A virtual gastroscopy[14] identified the mass in the gastric fundus, 3 cm below the esophago-gastric junction (EGJ). On computed tomography of the chest, abdomen and pelvis, the mass had heterogeneous enhancement, measured approximately 60 mm and appeared to be attached to the left diaphragmatic crus (Figure 1B). Positron emission tomography showed high avidity exclusively at the site of the gastric lesion.
A multidisciplinary consultation recommended surgical resection and an exploratory laparoscopy via the da Vinci® Si™ system was planned.
The final diagnosis in this patient was nonmetastatic PEComa of the fundus suitable for surgery with curative intent.
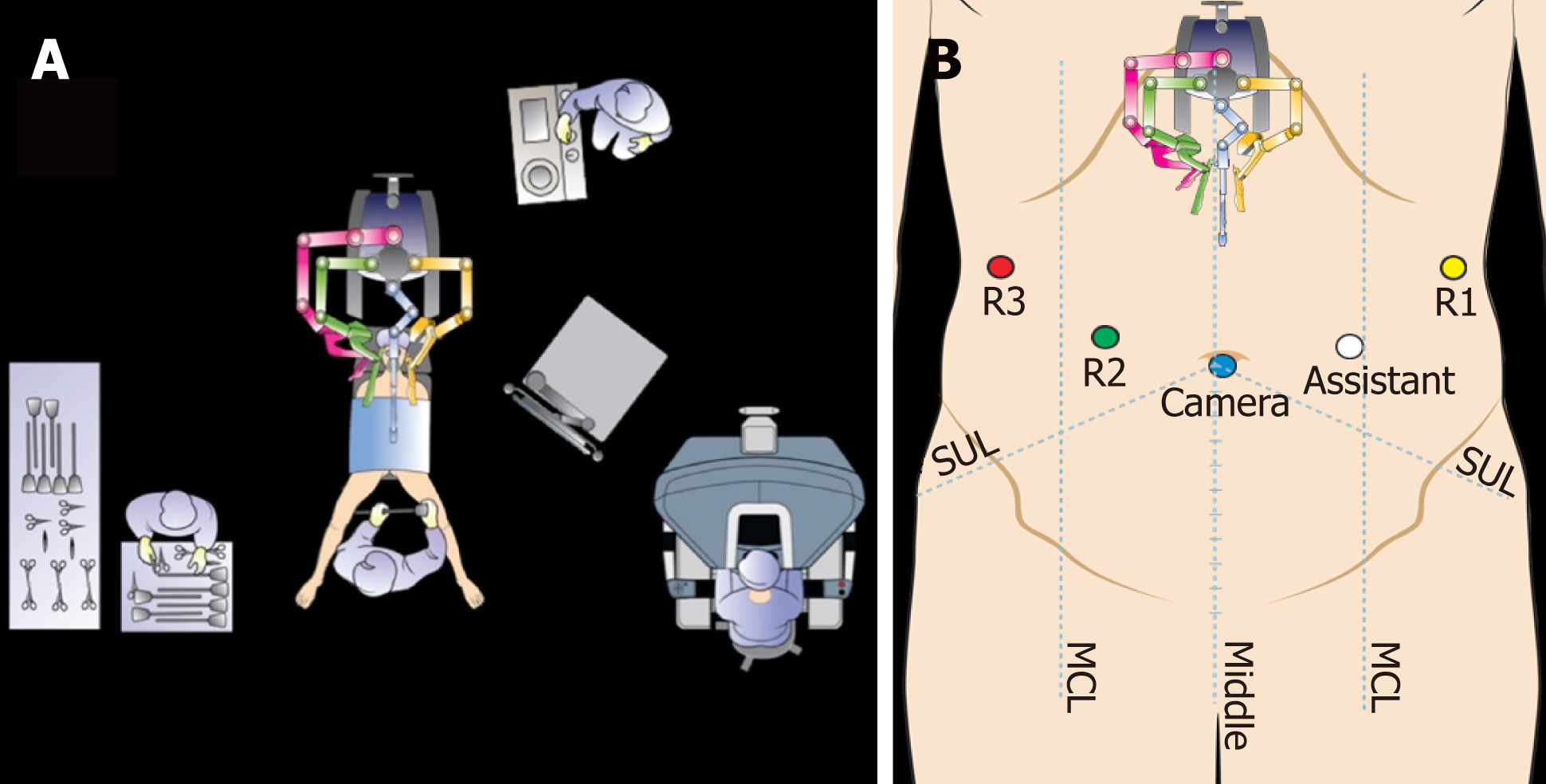
Thromboprophylaxis and cefazoline 2 g i.v. were administered 12 h and one hour before surgery, respectively. A thoracic epidural catheter for postoperative pain control was inserted just prior to induction. After induction of general anesthesia, the patient was placed in the supine position with both arms alongside the body (Figure 2A). A 12 mmHg pneumoperitoneum was established using a Veress Needle at Palmer’s Point. A 12 mm trocar was placed just below the umbilicus as the camera port for the 30° down scope; and four additional ports were inserted: two ports (8 mm diameter) in the bilateral hypochondriac regions and two further ports (8 mm and 12 mm diameter, respectively) placed at both sides of the lateral abdomen (Figure 2B).
The patient was then placed in the reverse Trendelenburg position at about 10-15°.
The abdominal cavity was explored and confirmed to be free of metastatic disease. The left lobe of the liver was then retracted towards the anterior abdominal wall using the liver-puncture method[15]. The mass was identified as a depressed area of the serosa of the stomach in the anterior wall of the proximal fundus towards the greater curvature, just below the EGJ. Once the absence of metastatic disease and the tumor location were confirmed, we docked the robot which was brought to the OR table from the head-side of the patient. The appropriate instruments were placed on each of the robotic arms under direct camera vision (arm #1: bipolar forceps; arm#2: ultrasonic shears; arm#3: fenestrated Cadiere forceps).
The robotic portion of the operation was then began with near-complete mobilization of the greater curvature of the fundus starting with division of the gastrocolic and gastrophrenic ligaments towards the upper pole of the spleen. Short gastric vessels were identified, ligated and divided proximately. The left diaphragmatic crus was found to be attached to the gastric fundus but not involved with the lesion.
Next, the pars flaccida of the lesser omentum was opened along the lesser curvature proximally up to the right side of the gastric cardia where dissection proceeded until the cardia was completely exposed.
On the basis of the intraoperative finding of disease localized to the gastric fundus without diaphragmatic or cardia involvement, we decided to perform a gastric wedge resection. First, an anterior vertical gastrotomy was carried out far away from the lesion. This allowed direct visualization of the intraluminal extent of the tumor. Using the ultrasonic shears, the tumor was excised with at least a 2 cm gross margin from the mass. We avoided any direct tumor manipulation, an advantage attributable to steady traction of the fundus by the third robotic arm. A lymph node dissection of the right paracardial region and the upper perigastric portion of the lesser curvature was performed. The specimen was removed en block with lymph nodes and bagged for extraction.
The defect left due to the resected tumor was reapproximated vertically using three stay sutures. The gastrotomy was then closed with two hemi-continuous running interlocking sutures. A second reinforcing layer was applied using interrupted sutures. The specimen was then removed through a 4 cm Pfannenstiel incision. Surgery was completed following closure of the port incisions (Video).
The total operation time was 200 min with a blood loss of 30 mL. The postoperative course was uneventful: the nasogastric tube was removed on postoperative day 1 and the patient was discharged on postoperative day 5 with good tolerance of oral intake.
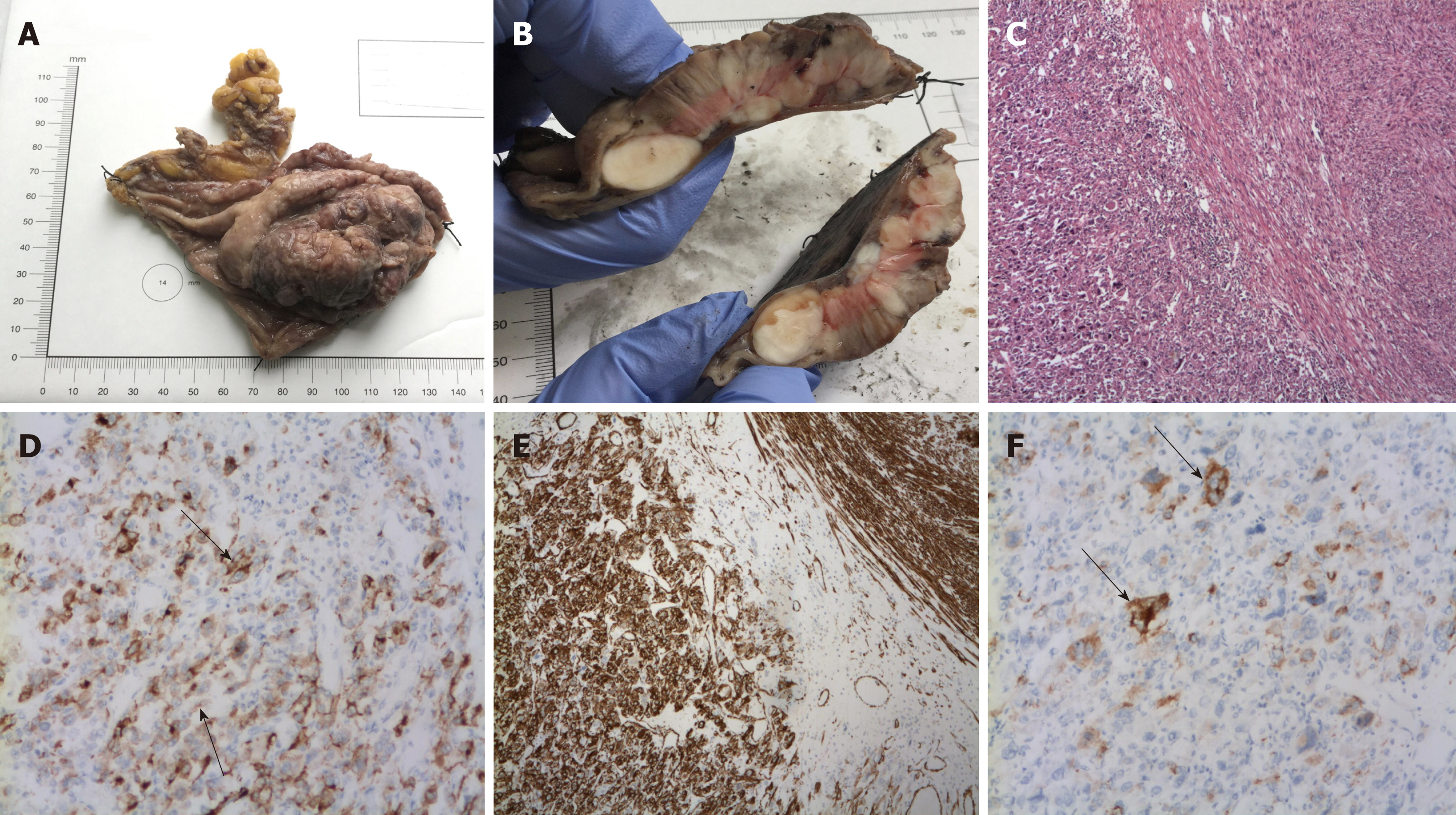
On gross examination of the removed specimen, the gastric polypoid mass measured 6.5 cm × 6 cm × 3.4 cm with at least 1 cm to the closest resection margin. Microscopically, the tumor displayed a mixture of epithelioid and spindle cell components. The mitotic count was high (63/50 high power fields-HPF) and the growth pattern was infiltrative with high nuclear grade and high cellularity. Vascular invasion and necrosis were also identified. The tumor was focally positive for smooth muscle actin, caldesmon, desmin, HMB-45 and melan-A (Mart-1), microphthalmia transcription factor (MITF) and negative for pan-cytokeratin AE1/AE3, CD34, CD31, CD117 (c-kit), S100 and myogenin (Figure 3). All these findings were consistent with the diagnosis of malignant gastric PEComa and confirmed the preoperative biopsy results. The ten lymph nodes removed during surgery were negative for metastasis.
As clear indications for adjuvant therapy have yet to be established, the medical oncologists did not recommend any further therapy and proposed surveillance follow-up. The patient was last seen 11 mo after surgery and remains disease-free.
In this article, we report the first application of the robotic system to resect a 6.5 cm malignant PEComa of the gastric fundus with a stomach-sparing R0 resection. Robotic wedge resection of the PEComa was safe, feasible and did not compromise short-term oncological outcomes.
Preoperative diagnosis with immunohistochemistry is preferred to differentiate PEComas from other uncommon tumors of the stomach with differential diagnoses including GI stromal tumors (GISTs), smooth muscle tumor, sarcomatoid-pleomorphic carcinoma, clear cell sarcoma (CCS), and melanoma (primary or metastatic).
The diagnostic challenge is due to the fact that gastric PEComa is a very rare neoplasm with only ten cases reported in the English literature[4,7-13]. Radiological imaging is not sensitive enough to distinguish PEComa from other types of gastric neoplasms due to nonspecific characteristics and a wide spectrum of different radiological aspects[16]. Histology is necessary for the diagnosis of PEComa. Microscopically, this tumor showed the most typical aspects of PEComas which included nests or sheets of epithelioid cells or spindle cells with variable clear or lightly granular eosinophilic cytoplasm. In many cases, cells have perivascular distribution and variable degrees of pleomorphism. On immunohistochemical analysis, PEComas are characterized by both positive melanocytic and muscle markers[2] with variable staining intensity and extent of tumor involvement.
Gastric PEComas are easily confused with GISTs due to their epithelioid and spindle morphology and submucosal location; in this case, positivity for melanocytic markers (HMB-45, MART-1, MITF) and negativity for GISTs markers (CD117, DOG-1) were more consistent with a diagnosis of PEComa. In addition, the morphology of leiomyosarcoma may be very similar to PEComa. Indeed, smooth muscle tumors disseminate into cytoplasmic eosinophilia, vacuoles around the nucleus, and “cigar-shaped” nuclei, while PEComas have clear to lightly eosinophilic cytoplasm, and round or ovoid nuclei. Immunohistochemical analysis allows for more accurate differentiation between these tumors. This was true in our case where the focal positivity for melanocytic markers (HMB-45, MART-1, MITF) favored PEComa. Sarcomatoid-pleomorphic carcinoma is also likely to confuse pathologists due to its pleomorphic, epithelioid, and spindle appearance. In the present case, the expression of melanocytic and muscle markers, and the lack of immunoreactivity for pan-cytokeratin AE1/AE3 helped to exclude the diagnosis of carcinoma. GI CCS always shows nests of round or epithelioid cells and mixed osteoclast-like giant cells; it also has strong reactivity for S100 protein, but is less consistent in the expression of other melanocytic markers and in most cases carries specific gene fusion, which represents the main difference between PEComa and CCS.
Finally, melanoma should always be considered when diffuse expression of melanocytic markers is present. For melanomas, the presence of a primary skin lesion is considered essential for diagnosis. Furthermore, in the case of metastatic melanoma it is important to rely on clinical history. Additionally, S100 protein is important to distinguish melanoma from PEComa as it is more frequently positive in melanoma even if some PEComas express a weak and focal S100 positivity. The present case was negative for S100 protein, focally strong and uniformly positive for smooth muscle actin, focally positive for desmin, caldesmon, HMB-45, MART-1, and MITF. These findings excluded melanoma as a diagnosis.
PEComas show a broad spectrum of malignancy and lack reliable criteria for biological behavior[17]. Little is known about their prognosis. However, in 2005 one study[2] found that tumor size > 5 cm, mitotic index > 1/50 HPF, infiltrative growth pattern, marked hypercellularity, pleomorphism, necrosis and nuclear atypia were associated with local recurrence or metastasis. However, the study by Folpe involved PEComas from different anatomic sites and did not focus on GI PEComas. Thus, we cannot predict how these criteria could be applied for GI PEComas and more specifically for gastric PEComas. Some years later, Fadare et al[18] suggested that the only characteristics related to aggressive behavior are mitotic count > 1/10 HPF and/or coagulative necrosis. Additionally, the study suggested that atypia should be considered as an indication of uncertain malignant potential, while tumor size and lymph node involvement are not considered worrisome features. In 2013 Fu et al[19] proposed that infiltrating growth pattern and coagulative necrosis should be considered more important factors than hypercellularity, high mitosis, and regional lymph node involvement in order to define the malignancy of PEComas because they better represent the aggressiveness of this tumor. In the same year, Doyle et al[4] examined 35 cases of GI PEComas and proposed the following findings as reliable histologic predictors of malignancy: marked nuclear aypia, diffuse pleomorphism and ≥ 2 mitoses per 10 HPF. According to the criteria by Folpe et al[2] and Doyle et al[4], the current case can be classified as being malignant with a high risk of recurrence (tumor size > 5 cm, infiltrative growth pattern, high nuclear grade and marked hypercellularity, mitotic index > 1/50 HPF and vascular invasion).
A review of the English literature on gastric PEComas yielded ten cases and are presented in Table 1. Patient demographics provide little insight into PEComas. There is no sex predominance in gastric PEComas in contrast to PEComas in other sites, which were reported more often in females[4]. The age distribution is broad, from 39 to 74 years and none of the reported gastric PEComas were associated with tuberous sclerosis complex. The most common anatomic site was the pyloric antrum (4 cases), followed by the gastric body (3 cases) and fundus (1 case). A high nuclear grade was present in the majority of patients (4/6) and necrosis was identified in four of seven cases. In general, the median mitotic rate was high. Regional lymph node metastases are usually not reported and it is not clear whether the surgical resection included an additional lymphectomy or lymph node sampling. Two patients presented with metastasis at the time of diagnosis and another patient with a 4 cm lesion of the upper body of the stomach, which was treated with endoscopic submucosal dissection (ESD), developed liver metastasis at 6 mo. The remaining 7 patients had follow-up periods ranging from 6 mo to 7 years with no recurrences. Interestingly, we observed that none of the patients who underwent surgical resection even with unfavorable prognostic factors such as high nuclear grade and high mitotic rate developed metastases, unlike PEComas that were endoscopically treated. Although additional factors such as infiltrative growth pattern and the presence of coagulative necrosis seem to be prognostic of poor outcomes, the small number of cases does not allow us to draw any conclusions regarding the prognostic criteria of gastric PEComas.
| Ref., yr | No of cases | Age (yr), sex | Site of the lesion | Size (cm) | Treatment | Malignant criteria (Folpe’s classification[2]) | IHC | Follow up | |||||||
| Infiltrative growth pattern | Nuclear grade | Necrosis | Mitotic activity | Vascular invasion | HMB-45 | Melan-A | SMA | Desmin | |||||||
| Mitteldorf et al[7], 2010 | 1 | 71, F | Antrum | 3 | Partial gastrectomy | - | Moderate | - | Low (1/50 HPF) | - | - | + | + | + | DF at 19 mo |
| Waters et al[8], 2012 | 1 | 42, M | Pylorus | 10 | Distal gastrectomy | NR | NR | NR | NR | NR | NR | + | NR | + | Liver met at diagnosis, death after 3 mo |
| Doyle et al[4], 2013 | 2 | NR | NR | NR | Surgical resection | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Wilson et al[9], 2013 | 1 | 74, F | Body | 0.5 | No surgery | NR | NR | NR | NR | NR | NR | NR | + | + | Multiorgan met at diagno-sis |
| Yamada et al[10], 2015 | 1 | 39, M | Body-lesser curvature | 7.3 | Lap wedge resection | + | High | + | High (> 2/50 HPF) | +/- | + | + | + | + | DF at 6 mo |
| Kumar et al[11], 2015 | 1 | 48, F | Antrumgreater curvature | 11.5 | Open distal gastrectomy | NR | High | + | High (20/10 HPF) | NR | - | + | + | NR | NR |
| Shin et al[12], 2017 | 2 | 62, F | Antrum | 4.2 | Lap wedge resection | - | Low | - | Low (1/50 HPF) | - | + | - | + | + | DF at 8 mo |
| 67, M | Fundus below the EGJ | 5 | Subtotal gastrectomy | - | High | - | High (45/50 HPF) | NR | - | + | + | - | DF at 7 yr | ||
| Toya et al[13], 2017 | 1 | 47, M | Upper body | 4 | ESD | + | High | + | High (> 1/50 HPF) | NR | + | + | + | + | Liver met at 6 mo |
| Current case | 1 | 55, M | Fundus- below the EGJ | 6.5 | Robotic wedge resection | + | High | + | High (63/50 HPF) | + | + | - | NR | + | DF at 11 mo |
The optimal surgical management and need for systemic treatment of primary and metastatic PEComas have not yet been established. According to the available literature, surgery with an R0 surgical resection of the tumor seems to be the best primary treatment option for non-metastatic PEComas with aggressive appearance. This is consistent with the recommended approach for mesenchymal tumors (e.g., GIST or sarcoma). Limited literature suggests that surgical resection with gastric wedge or gastrectomy is curative and results in disease-free survival[7,10,12]. Only one patient treated by ESD developed distant metastasis[13]. For this reason, we decided to perform an organ-sparing resection with limited peritumoral lymph node dissection. The large lesion was located in an unfavorable site just below the EGJ[20]. The robotic approach was chosen for its well-known technical advantages in procedures to remove lesions in difficult locations with the goal of stomach preservation[21]. Due to the benefits of a tremor filter, steady traction of the fundus was made possible by the third robotic arm in order to completely excise the lesion without tumor manipulation. This allowed for adherence to the oncologic “no-touch” principle for prevention of peritoneal seeding. Moreover, taking advantage of the articulating wristed capability of the robotic needle drivers, a robot-sewn suture of the gastrotomy was easily performed, simulating the same technique achieved in conventional open surgery[20]. The resection and repair of the gastrostomy site were safely and effectively performed by the robotic approach.
Postoperatively, adjuvant chemotherapy was not offered to the patient, despite many histological signs of malignancy in the resected tumor, as there are no current indications of the effectiveness of chemotherapy after complete resection of a PEComa. Recently, mammalian target of rapamycin inhibitors such as sirolimus, temsirolimus, and everolimus have shown promising results in patients with metastatic PEComa[22] and their use might be supported for a subset of PEComas that exhibit malignant behavior[23].
In conclusion, gastric PEComa is a rare entity and should be considered in the preoperative differential diagnosis of gastric tumors. According to the available literature, complete surgical removal may be the best treatment for non-metastatic PEComa and a minimally invasive resection of the tumor, including robot-assisted surgery can yield an acceptable outcome. Further studies with long-term follow-up are needed to understand more about the prognostic factors of gastric PEComa and to determine the optimal diagnostic path, treatment and follow-up for this tumor. However, standardization of treatment for PEComa will be difficult to recommend.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ahmed M, Lambrecht NW, Mohamed SY S-Editor: Dou Y L-Editor: Webster JR E-Editor: Xing YX
| 1. | Fletcher CDM, Bridge JA, Hogendoorn P, Mertens F. World Health Organization Classification Tumors of Soft Tissue and Bone. 4th edition. Lyon: IARC, 2013. . |
| 2. | Folpe AL, Mentzel T, Lehr HA, Fisher C, Balzer BL, Weiss SW. Perivascular epithelioid cell neoplasms of soft tissue and gynecologic origin: a clinicopathologic study of 26 cases and review of the literature. Am J Surg Pathol. 2005;29:1558-1575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 640] [Cited by in RCA: 636] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 3. | Bleeker JS, Quevedo JF, Folpe AL. "Malignant" perivascular epithelioid cell neoplasm: risk stratification and treatment strategies. Sarcoma. 2012;2012:541626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 135] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 4. | Doyle LA, Hornick JL, Fletcher CD. PEComa of the gastrointestinal tract: clinicopathologic study of 35 cases with evaluation of prognostic parameters. Am J Surg Pathol. 2013;37:1769-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Folpe AL, Goodman ZD, Ishak KG, Paulino AF, Taboada EM, Meehan SA, Weiss SW. Clear cell myomelanocytic tumor of the falciform ligament/ligamentum teres: a novel member of the perivascular epithelioid clear cell family of tumors with a predilection for children and young adults. Am J Surg Pathol. 2000;24:1239-1246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 182] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Chen Z, Han S, Wu J, Xiong M, Huang Y, Chen J, Yuan Y, Peng J, Song W. A systematic review: perivascular epithelioid cell tumor of gastrointestinal tract. Medicine (Baltimore). 2016;95:e3890. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Mitteldorf CA, Birolini D, da Camara-Lopes LH. A perivascular epithelioid cell tumor of the stomach: an unsuspected diagnosis. World J Gastroenterol. 2010;16:522-525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Waters PS, Mitchell DP, Murphy R, McKenna M, Waldron RP. Primary malignant gastric PEComa - Diagnostic and technical dilemmas. Int J Surg Case Rep. 2012;3:89-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Wilson J, Hartke J, Akram S. Metastatic perivascular epithelioid cell tumor of the stomach: an unusual diagnosis. Proceedings of the American College of Gastroenterology (ACG), 2013 Annual Meeting; 2013 Oct 11-16; San Diego (California). Am J Gastroenterol. 2013;108:S238. |
| 10. | Yamada S, Nabeshima A, Noguchi H, Nawata A, Nishii H, Guo X, Wang KY, Hisaoka M, Nakayama T. Coincidence between malignant perivascular epithelioid cell tumor arising in the gastric serosa and lung adenocarcinoma. World J Gastroenterol. 2015;21:1349-1356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Kumar M, Kumar V, Abrina V, Kaur S, Kumar A, Maroules M. Malignant gastric PEComa: a rare malignancy. Am J Cancer Case Rep. 2015;3:209-214. |
| 12. | Shin SA, Choi J, Moon KC, Kim WH. Perivascular Epithelioid Cell Tumor in the Stomach. J Pathol Transl Med. 2017;51:428-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Toya Y, Eizuka M, Matsumoto T. Submucosal Tumor of the Stomach With Drastic, Short-term Changes in Morphology. Gastroenterology. 2017;153:357-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Kim JH, Eun HW, Choi JH, Hong SS, Kang W, Auh YH. Diagnostic performance of virtual gastroscopy using MDCT in early gastric cancer compared with 2D axial CT: focusing on interobserver variation. AJR Am J Roentgenol. 2007;189:299-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Woo Y, Hyung WJ, Kim HI, Obama K, Son T, Noh SH. Minimizing hepatic trauma with a novel liver retraction method: a simple liver suspension using gauze suture. Surg Endosc. 2011;25:3939-3945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Tan Y, Zhang H, Xiao EH. Perivascular epithelioid cell tumour: dynamic CT, MRI and clinicopathological characteristics--analysis of 32 cases and review of the literature. Clin Radiol. 2013;68:555-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Hornick JL, Fletcher CD. PEComa: what do we know so far? Histopathology. 2006;48:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 318] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 18. | Fadare O. Perivascular epithelioid cell tumor (PEComa) of the uterus: an outcome-based clinicopathologic analysis of 41 reported cases. Adv Anat Pathol. 2008;15:63-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Fu X, Jiang JH, Gu X, Li Z. Malignant perivascular epithelioid cell tumor of mesentery with lymph node involvement: a case report and review of literature. Diagn Pathol. 2013;8:60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Zhao J, Wang G, Jiang Z, Jiang C, Liu J, Zhou J, Li J. Robotic Gastrotomy With Intracorporeal Suture for Patients With Gastric Gastrointestinal Stromal Tumors Located at Cardia and Subcardiac Region. Surg Laparosc Endosc Percutan Tech. 2018;28:e1-e7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, Caravaglios G. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 749] [Cited by in RCA: 771] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 22. | National Comprehensive Cancer Network. National Comprehensive Cancer Network (NCCN) Guidelines Soft Tissue Sarcoma. Available from: URL: https://www.nccn.org/professionals/physician_gls/pdf/sarcoma.pdf. |
| 23. | Wagner AJ, Malinowska-Kolodziej I, Morgan JA, Qin W, Fletcher CD, Vena N, Ligon AH, Antonescu CR, Ramaiya NH, Demetri GD, Kwiatkowski DJ, Maki RG. Clinical activity of mTOR inhibition with sirolimus in malignant perivascular epithelioid cell tumors: targeting the pathogenic activation of mTORC1 in tumors. J Clin Oncol. 2010;28:835-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 278] [Article Influence: 18.5] [Reference Citation Analysis (0)] |