Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3904
Peer-review started: August 19, 2019
First decision: September 23, 2019
Revised: October 13, 2019
Accepted: October 30, 2019
Article in press: October 30, 2019
Published online: November 26, 2019
Processing time: 98 Days and 15 Hours
Endophthalmitis caused by Enterococci is rare, and cases involving vancomycin-resistant enterococci are even rarer. We report the first case of Enterococcus casseliflavus endophthalmitis associated with injury caused by a pig. We also review reported cases of exogenous endophthalmitis caused by Enterococcus casseliflavus and discuss the clinical management and prognosis of this disease.
A 43-year-old man with no previous visual problems complained of endophthalmitis in his left eye following injury caused by a pig. Visual acuity was light perception and B-ultrasonography revealed vitreous opacities with retinal detachment. He was treated with intravitreal vancomycin and ceftazidime after refusing vitrectomy. However, the vitreous opacities and retinal detachment deteriorated and he underwent vitrectomy 5 d post-injury. Intraoperatively, advanced rhegmatogenous and tractional retinal detachment with proliferative vitreoretinopathy were observed. On postoperative day 5, vitreous cultures grew Gram-positive cocci identified as Enterococcus casseliflavus. A 2-wk course of intravenous ampicillin and dexamethasone was commenced. On postoperative day 14, visual acuity improved to hand movement. At 6 mo post-injury, visual acuity improved to 20/667, but optic atrophy was present.
Systemic administration of linezolid in the treatment of Enterococcus casseliflavus endophthalmitis can improve visual acuity. However, intravitreal amikacin should be considered despite concerns of toxicity when oral linezolid fails to prompt improvement.
Core tip: The emergence of vancomycin-resistant enterococci endophthalmitis is of grave concern. To date, four cases of Enterococcus casseliflavus endophthalmitis have been reported in the literature. We describe the first case of Enterococcus casseliflavus endophthalmitis associated with injury caused by a pig and the treatment regimen. In addition, we review the literature and discuss the clinical management and prognosis of this disease.
- Citation: Bao QD, Liu TX, Xie M, Tian X. Exogenous endophthalmitis caused by Enterococcus casseliflavus: A case report. World J Clin Cases 2019; 7(22): 3904-3911
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3904.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3904
Exogenous endophthalmitis is often caused by penetrating eyeball injury, endophthalmic surgery, and penetrating bacteria of a corneal ulcer. The emergence of vancomycin-resistant enterococci (VRE) endophthalmitis is of grave concern. We report the first case of Enterococcus casseliflavus endophthalmitis associated with injury caused by a pig. On examination, the patient did not have an entry site for the bacterium. Bacterial endophthalmitis is difficult to treat, as virulent bacteria can damage the eye tissue in a short time, and infectious endophthalmitis often leads to loss of vision and even atrophy of the eyeball if not treated in time. If infection can be controlled in time, it may partly restore patient vision. Therefore, if endophthalmitis is suspected, effective treatment should be given as soon as possible[1]. In addition, we also reviewed reported cases of exogenous endophthalmitis caused by Enterococcus casseliflavus and their clinical management and prognosis.
A healthy 43-year-old man presented with sudden swelling and pain in his left eye for one day, accompanied by visual impairment.
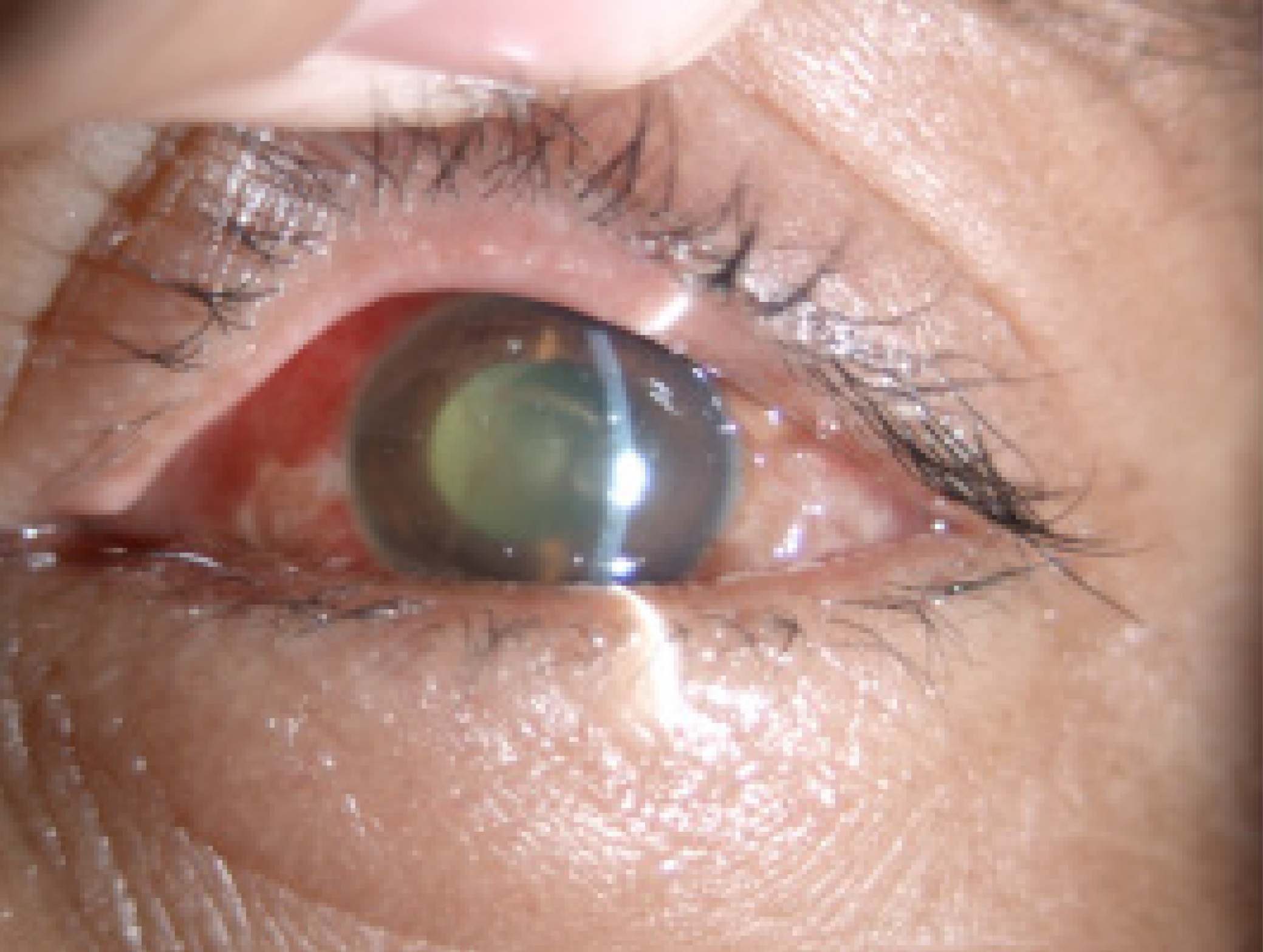
One day earlier while on his pig farm (Figure 1), he received a facial injury caused by a pig’s tail. Approximately 6 h later, his left eye became painful, and 13 h after the initial injury he noted redness in the conjunctiva. He was taken to hospital the following day.
He had no history of systemic diseases, surgery, recent bacterial or viral infections, and no previous visual disorders. No iatrogenic operations had been performed in the previous year.
Following examination, it was found that his vision was 20/20 OD and light perception was OS. There were no abnormal extraocular movements and skin abrasions on his forehead. The left eye slit lamp examination showed a + 2 conjunctival chemical reaction and + 2 corneal edema without epithelial defects. The anterior chamber showed a fibrinoid response, accompanied by a 2 mm decrease intraocular pressure. Exudates had formed a film over the exposed surface of the anterior lens capsule in the pupillary area, resulting in an occluded pupil. His vitreous cavity was filled with purulent debris and the fundus could not be seen.
The total number of leukocytes was 15 × 109/L. No abnormalities in biochemical tests, chest X-ray films and electrocardiography were observed.
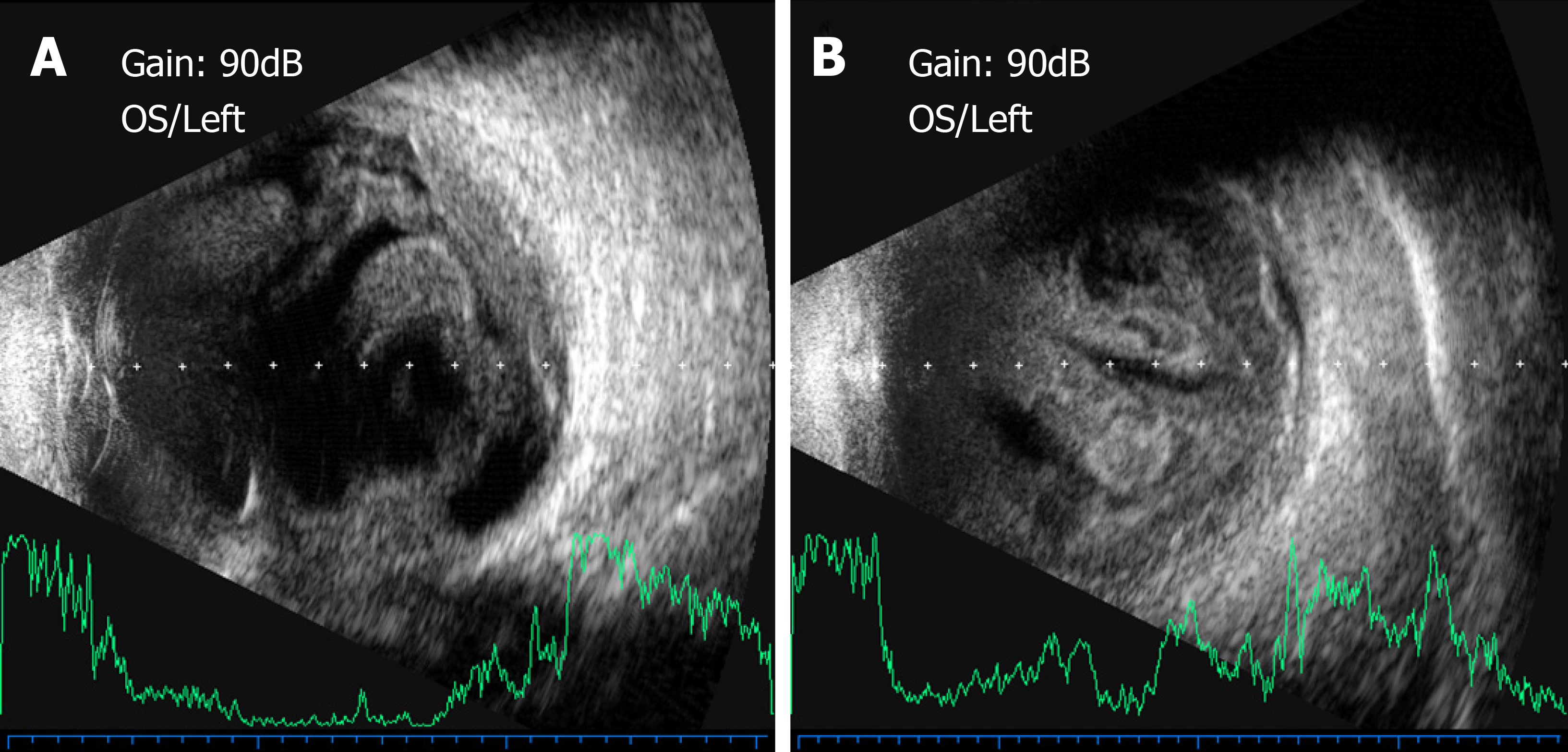
Contact B-ultrasonography revealed vitreous opacities with retinal detachment (Figure 2A).
Exogenous endophthalmitis.
The patient refused to undergo vitrectomy. A vitreous specimen was examined by microbiological methods. At the same time, the patient was given intravitreal vancomycin 1 mg/0.1 mL and ceftazidime 2 mg/0.1 mL, plus intravenous cefuroxime sodium 2500 mg and dexamethasone 10 mg were administered. Topical 0.3% tobramycin and 0.1% dexamethasone were applied every 3 h, 1% atropine and 0.3% gatifloxacin twice a day, and 0.5% pranoprofen every 6 h.
Vitreous cultures were typically negative. Anterior segment inflammation decreased (Figure 3), but vitreous opacities and retinal detachment deteriorated (Figure 2B). The patient underwent left pars plana lensectomy, vitrectomy, peripheral iridectomy and silicone oil tamponade 5 d after the injury. During the operation, compact hyaluronitis and vasculitis had occurred in the short period between the injury and the operation, which covered the optic disc and blood vessels. After the vitreous debris was removed, advanced rhegmatogenous and tractional retinal detachment with proliferative vitreoretinopathy were found obscuring a retinal tear 3PD in size. On postoperative day 5, Gram-positive Enterococcus casseliflavus was grown in culture, which was sensitive to linezolid, ampicillin, streptomycin, gentamicin, tetracycline and penicillin, but resistant to vancomycin. Therefore ampicillin was injected intravenously at 2 g/4 h and dexamethasone 600 mg/d for 2 wk.
On postoperative day 14, visual acuity in the left eye improved to hand movement. At 6 mo post-injury, visual acuity improved to 20/667 (aphakic correction), but optic atrophy occurred.
Enterococcus casseliflavus is commonly found in the gastrointestinal tract of livestock, and in soil and plants[2]. It is rarely associated with human infection. An exhaustive review of the literature showed that there are only 4 previously reported cases of microbiologically proven exogenous endophthalmitis caused by Enterococcus casseliflavus and this is the 5th such case[2-5]. The salient clinical findings in these cases are summarized in Table 1.
| NO. | Author/Yr | Age/Sex | Cause of injury | Time interval between injury and symptoms | Eye | Visual acuity | Presenting feature | Time interval between injury and vitrectomy | Treatment | Laboratory diagnosis | Disease progression | Outcome |
| 1 | Khurana et al[2], 2009 | 37/M | A horse tail injury | 24 h | Left | PL | +2 conjunctival chemosis, +2 corneal edema, intact corneal epithelium, 1-mm hypopyon, dense vitritis | 24 h | Vitrectomy; Intravitreal hydrochloride and ceftazidime | Vitreous; cultures | On post-operative day 7: The patient’s pain and anterior segment inflammation resolved. On post-operative day 21: Cataract and vitreous debris. On post-operative day 56: Vitrectomy; Retinal detachment with proliferative vitreoretinopathy | PL |
| 2 | Berenger et al[3], 2015 | 6/M | High-velocity water stream trauma | 2 h | Left | Not reported | Intact corneal epithelium, severe anterior chamber inflammation, miosis and inferior hypopyon, vitreous opacities | 26 h | Vitrectomy; Intravitreal hydrochloride and ceftazidime; Topical therapy: moxifloxacin, prednisolone, homatropine; Ciprofloxacin (PO); Vancomycin (IV) | Mass spectrometry | On post-operative min 45: Vitrectomy; Intravitreal ampicillin and amikacin; Topical therapy: gentamicin and prednisolone; ampicillin, linezolid (IV). On post-operative day 7: Outer cortical vitreous separation. Over time, the vitreous cavity and anterior segment cleared | 20/70 |
| 3 | Nguyen et al[4], 2017 | 6/M | An object projected from a lawn mower | Immediately | Left | HM | 2 + conjunctival chemosis, chemosis temporally, irregular iris, 4 + anterior chamber cells,1 mm layered hypopyon, 1.5 mm hyphema | 27 h | Vitrectomy; Intravitreal hydrochloride and ceftazidime; Subconjunctival injection: dexamethasone; Topical therapy: atropine, prednisolone acetate and moxifloxacin; Cephalexin (PO) | Vitreous cultures | On post-operative day 5: Topical therapy: tobramycin and linezolid;Linezolid (PO); On post-operative day 17: Vitrectomy; Intravitreal amikacin; On post-operative day 77: Phacoemulsification with intraocular lens placement and maculasparing retinal detachment | 20/40 |
| 4 | Low et al[5], 2015 | 54/M | Metallic intraocular foreign body | Immediately | Left | HM | Conjunctival chemosis, corneal edema, inferonasal corneoscleral laceration with iris prolapse. The anterior chamber was shallow with a fibrinous reaction, 1.6-mm hypopyon | 72 h | Vitrectomy; Intravitreal vancomycin and ceftazidime; Topical therapy: cefazolin, gentamicin, and atropine | Amoxicillin, linezolid, gentamicin (IV), amoxicillin (PO) | 6/90 | |
| 5 | Present case | 47/M | 6 h | Left | PL | +2 conjunctival chemosis, +2 corneal edema, intact corneal epithelium, 2-mm hypopyon, vitreous opacities, retinal detachment | 120 h | Vitrectomy; Intravitreal hydrochloride and ceftazidime; Topical therapy: Tobramycin, dexamethasone, atropine, gatifloxacin, pranoprofen, dexamethasone (IV) | Vitreous cultures | Intravenous dexamethasone (IV); On post-operative day 2: optic atrophy | 20/667 |
Four previously healthy men presented with endophthalmitis of the left eye following outdoor activities. The affected left eye had direct or indirect contact with the gastrointestinal tract of livestock, soil or plants. Typical endophthalmitis symptoms can develop within a few hours to 1 d after injury. However, on slit-lamp examinations, three of the five cases had no entry site for the bacterium. Cataract, retinal detachment and other complications occurred in all 5 cases after vitrectomy. Patients with timely vitrectomy, systemic administration of linezolid and intravitreal amikacin had better visual acuity.
In the present case, the injury caused by the pig may have introduced the pathogen. Enterococcus casseliflavus is a common strain found on pig farms[6] and the environment in the patient’s farm was extremely harsh, leading to a high risk of infection. There was a chemical reaction in the conjunctiva, but slit lamp examination showed no obvious perforation. Damage caused by the pig’s tail may have led to a self-sealing microperforation of the cornea or conjunctiva, which may explain how bacteria entered the eye. Similar case reports have been reported previously[3,7,8].
It is reported that 15% to 40% of patients with exogenous endophthalmitis have visual acuity of 0.5 or more[1]. The poor vision in our patient was due to the failure to perform timely vitrectomy. Vitrectomy is one of the preferred treatments for endophthalmitis, as it has the following advantages: Can clear vitreous infection, remove vitreous opacity, allows collection of intraocular specimens for culture, and better distribution of antibiotics in the vitreous cavity[9]. However, our patient had no obvious pain symptoms and refused the operation, which caused irreparable damage.
Etiological examination is inefficient and interdisciplinary cooperation is poor in exogenous endophthalmitis. The present case did not demonstrate the importance of interdisciplinary medical care, and failed to initiate early and appropriate antimicrobial treatment using laboratory technology. It has been found that the negative rate of endophthalmitis bacterial culture is up to 30%[10]. The combination of genetic diagnosis and polymerase chain reaction (PCR) detection can improve the detection rate of pathogens[11]. Due to its high specificity and sensitivity, PCR has been used to confidently exclude pathogens, which is unique. However, PCR is easily contaminated in the laboratory; thus, it is currently only used to detect targeted microorganisms. The toxigenicity of cultured strains can be tested for drug sensitivity. Bacterial culture and molecular diagnostic tests should be carried out simultaneously to complement each other. Combining the use of an automated blood culture system with matrix-assisted laser desorption/ionization-time of flight mass spectrometry methodology, 45 strains of bacteria were isolated from vitreous specimens after acute endophthalmitis surgery, of which 96% were identified[12].
Poor use of antibiotics in this disease can result in treatment failure, for example, ampicillin has poor penetration into the vitreous fluid. Studies have shown that ampicillin levels in vitreous fluid are about 2-log lower than those in serum following intravenous injection[13]. There is concern regarding the use of aminoglycosides as they can cause retinal infarction. However, intravitreal injection of amikacin can reduce the incidence of macular infarction[14]. In cases of traumatic exogenous vancomycin-resistant enterococcus endophthalmitis, intravitreal amikacin led to a good visual outcome.
Following rapid vitrectomy, it is important to understand the entry of antibiotics into the vitreous space to guide treatment. The treatment of endophthalmitis caused by Enterococcus casseliflavus is challenging, the ability of local and systemic antibiotics to enter the vitreous space is poor due to a reduced choice of antibiotics. Linezolid penetrates the vitreous chamber when administered orally or intravenously, the concentration of linezolid in the vitreous cavity was higher than the minimum inhibitory concentration of most enterococci[15]. When linezolid was used systemically, the intravitreal concentration was higher than the lowest inhibitory concentration for VRE, and linezolid resistance in Enterococcus is rare. In the case of VRE endophthalmitis, intravitreal amikacin should be considered in the vitreous cavity as oral linezolid can produce toxicity and cannot quickly relieve symptoms.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ahmed M, Kakaei F, Nowak MS S-Editor: Dou Y L-Editor: Webster JR E-Editor: Liu MY
| 1. | Vaziri K, Schwartz SG, Kishor K, Flynn HW. Endophthalmitis: state of the art. Clin Ophthalmol. 2015;9:95-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 2. | Khurana RN, Leder HA, Nguyen QD, Do DV. Enterococcus casseliflavus endophthalmitis associated with a horse tail injury. Arch Ophthalmol. 2009;127:1551-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Berenger BM, Kulkarni S, Hinz BJ, Forgie SE. Exogenous endophthalmitis caused by Enterococcus casseliflavus: A case report and discussion regarding treatment of intraocular infection with vancomycin-resistant enterococci. Can J Infect Dis Med Microbiol. 2015;26:330-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Nguyen J, Hartnett ME. Successful management of post-traumatic vancomycin-resistant enterococcus endophthalmitis. Am J Ophthalmol Case Rep. 2017;5:117-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Low JR, Teoh CS, Chien JM, Huang EH. Enterococcus casseliflavus endophthalmitis due to metallic intraocular foreign body. Eye (Lond). 2015;29:840-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Kühn I, Iversen A, Burman LG, Olsson-Liljequist B, Franklin A, Finn M, Aarestrup F, Seyfarth AM, Blanch AR, Vilanova X, Taylor H, Caplin J, Moreno MA, Dominguez L, Herrero IA, Möllby R. Comparison of enterococcal populations in animals, humans, and the environment--a European study. Int J Food Microbiol. 2003;88:133-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 99] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Al-Khatib TK, Al-Khulaidi NA. Traumatic subconjunctival crystalline lens. Dislocation by the tail of a cow. Saudi Med J. 2004;25:2018-2019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Chaddah MR, Ahluwalia BK. A rare intraocular foreign body; hair from buffaloe's tail. J All India Ophthalmol Soc. 1968;16:251-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 9. | Flynn HW, Scott IU. Legacy of the endophthalmitis vitrectomy study. Arch Ophthalmol. 2008;126:559-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19:227-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 260] [Cited by in RCA: 336] [Article Influence: 28.0] [Reference Citation Analysis (1)] |
| 11. | Faigenbaum SJ, Boyle GL, Prywes AS, Abel R, Leopold IH. Intraocular penetrating of amoxicillin. Am J Ophthalmol. 1976;82:598-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Mailhac A, Durand H, Boisset S, Maubon D, Berger F, Maurin M, Chiquet C, Bidart M. MALDI-TOF mass spectrometry for rapid diagnosis of postoperative endophthalmitis. J Proteomics. 2017;152:150-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Röber H, Göring W, Sous H, Reim M. Concentration of ampicillin in the vitreous after cryocoagulation. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1977;204:275-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | D'Amico DJ, Caspers-Velu L, Libert J, Shanks E, Schrooyen M, Hanninen LA, Kenyon KR. Comparative toxicity of intravitreal aminoglycoside antibiotics. Am J Ophthalmol. 1985;100:264-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 72] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Horcajada JP, Atienza R, Sarasa M, Soy D, Adán A, Mensa J. Pharmacokinetics of linezolid in human non-inflamed vitreous after systemic administration. J Antimicrob Chemother. 2009;63:550-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |